Programme Implementation Plan: 2009 -10
advertisement

Programme Implementation Plan: 2009 -10
State Health Society
State Rural Health Mission
Department of Health & Family Welfare
Government of Chhattisgarh
Table of Contents
Table of Contents .................................................................................................................................................... ii
INTRODUCTION ................................................................................................................................................... 1
Background............................................................................................................................................................. 1
Demographic and Health Profile of Chhattisgarh ................................................................................................. 1
Structure of Chhattisgarh Public Health System .................................................................................................... 2
The Health Infrastructure Situation ........................................................................................................................ 4
Health Workforce Status of Chhattisgarh ............................................................................................................... 5
Other Challenges .................................................................................................................................................... 5
Poor Socio-economic status ............................................................................................................................... 5
Difficult Geographic Location ............................................................................................................................ 5
Vision and Goals for the Health Sector .................................................................................................................. 6
National Rural Health Mission ............................................................................................................................... 6
Objectives of NRHM ........................................................................................................................................... 6
Systemic Inputs ....................................................................................................................................................... 7
Governance Reforms .......................................................................................................................................... 7
Introduction of Commissioner System ................................................................................................................ 7
Strengthening of Directorates ............................................................................................................................. 8
Filling up Positions of Joint Directors and Deputy Directors ............................................................................ 8
Filling up vacancies of State Programme Management Unit (SPMU) ............................................................... 8
Filling up Positions at District and lower levels ................................................................................................ 8
Devolution of Powers to Block Medical Officers................................................................................................ 8
Electronic Procurement and Funds Transfer ..................................................................................................... 8
Revision of Essential Drug List .......................................................................................................................... 9
Integrated Health Equipment Management System ............................................................................................ 9
Summary of Health Sector Achievements ............................................................................................................. 10
Comparison of Key trends under NFHS-2 and NFHS-3: ................................................................................. 11
Winner of the 4th JRD Tata Memorial awards 2008 ........................................................................................ 12
Selection of the Best Performing State ............................................................................................................. 13
Raising Medical Education Levels: .................................................................................................................. 20
Mainstreaming of Indian Systems of Medicine: ................................................................................................ 20
Control of Food & Drugs: ................................................................................................................................ 20
Situational Analysis: ............................................................................................................................................. 23
Programme Experience: ....................................................................................................................................... 25
Addressing Gaps in Infrastructure – Sanction of Facilities against Norms: .................................................... 25
Creation of Buildings: ...................................................................................................................................... 25
Human Resource Situation: .............................................................................................................................. 26
NRHM PIP 2009-10: Chhattisgarh
ii
Operationalisation of FRUs & improving institutional delivery situation: ...................................................... 29
Medically Underserved Areas: ......................................................................................................................... 31
Behaviour Change Communication: ................................................................................................................ 31
Community Level Care: The Mitanin Programme: .......................................................................................... 32
Provision of Quality Services and Better Management of facilities: ................................................................ 33
Baal Hruday Suraksha Yojana: ........................................................................................................................ 33
PRI Involvement in Health: .............................................................................................................................. 34
Urban health systems: ...................................................................................................................................... 34
Programmatic and Financial Management Issues: .......................................................................................... 35
Technical Assistance: ....................................................................................................................................... 36
Major state-specific UNICEF initiatives in Chhattisgarh are: ......................................................................... 37
Technical Assistance from RRC ........................................................................................................................ 38
Technical Assistance from Micronutrient Initiative.......................................................................................... 38
Technical Assistance from CARE ..................................................................................................................... 39
Mainstreaming of AYUSH .................................................................................................................................... 40
Status of AYUSH Institutions in Comparison with Allopathic Set up ............................................................... 40
AYUSH Interventions under mainstreaming in Chhattisgarh: ......................................................................... 41
Co-location of 85 AYUSH dispensaries in PHC\CHC after launching of NRHM ............................................ 43
Availability of Medicines in Co-Located Centres ............................................................................................. 44
Constraints Faced: ........................................................................................................................................... 44
Support of AYUSH Medical officers in National Health Programmes ............................................................. 44
Capacity building as a part of mainstreaming ................................................................................................. 44
Training of AYUSH physicians: .................................................................................................................... 44
Training of Mitanin for AYUSH Mainstreaming: ......................................................................................... 45
Proposals Submitted during 2008-09 Under Central Government Scheme: .................................................... 45
Proposals under NRHM for Mainstreaming Ayush 2008-09............................................................................ 45
Other AYUSH interventions under NRHM in Chhattisgarh ............................................................................. 46
Financial situation, estimated expenses & balance up to march 2008 (in details) .............................................. 48
Physical and Financial Report ............................................................................................................................. 70
Part A- RCH II Flexi-pool .................................................................................................................................... 78
Summary ............................................................................................................................................................... 78
Maternal Health ........................................................................................................................................... 92
Child Health: ................................................................................................................................................ 92
Family Planning ........................................................................................................................................... 93
Adolescent Health: ....................................................................................................................................... 93
Urban RCH ................................................................................................................................................... 93
Tribal RCH ................................................................................................................................................... 93
NRHM PIP 2009-10: Chhattisgarh
iii
RCH interventions for Vulnerable ................................................................................................................ 93
Maintaining Sex Ratio- ................................................................................................................................. 93
Infection Management in facilities ............................................................................................................... 93
Health Management Information System...................................................................................................... 93
BCC programmes for RCH ........................................................................................................................... 94
Training and Capacity Building for RCH..................................................................................................... 94
Effective RCH Programme Management...................................................................................................... 94
Process of Plan Preparation ................................................................................................................................ 97
Background and Current Status ........................................................................................................................... 97
Situation Analysis ............................................................................................................................................. 97
Progress and Lessons Learnt ............................................................................................................................ 97
RCH-II Programme Objectives, Strategies and Activities: .................................................................................. 97
Vision Statement ............................................................................................................................................... 97
Maternal Health ................................................................................................................................................... 98
Introduction: ..................................................................................................................................................... 98
Objectives ......................................................................................................................................................... 98
Interventions ..................................................................................................................................................... 99
Accredited Social Health Activist (ASHA) .......................................................................................................... 100
Objectives: ...................................................................................................................................................... 100
Strategies: ....................................................................................................................................................... 101
Achievements of Year 2008-09: ...................................................................................................................... 102
FOGSI............................................................................................................................................................. 105
Activities for Year 2009 -10:............................................................................................................................... 105
FRU Operationalisation: ................................................................................................................................ 105
Blood Storage Facility:............................................................................................................................... 105
Multi skilling of the Medical Officers: ............................................................................................................ 106
FOGSI: ........................................................................................................................................................... 106
Indemnity Insurance for the Multi Skilled MOs .............................................................................................. 106
Staff Appointment: .......................................................................................................................................... 107
Incentivisation: ............................................................................................................................................... 107
Operationalisation of 24 hour PHCs .............................................................................................................. 109
Activities: ........................................................................................................................................................ 109
Incentivisation for service providers: ............................................................................................................. 109
Appointment of ANMs: ................................................................................................................................... 109
Training of ANMs on Skilled Attendance at Birth: ......................................................................................... 110
Incentives for ANMs: ...................................................................................................................................... 110
Janani Suraksha Yojana: .................................................................................................................................... 110
NRHM PIP 2009-10: Chhattisgarh
iv
Progress so far: .............................................................................................................................................. 111
Interventions: .................................................................................................................................................. 112
Addressing first delay: ................................................................................................................................ 112
Addressing second delay: ........................................................................................................................... 112
Addressing third delay:............................................................................................................................... 112
Strategy: ......................................................................................................................................................... 113
Accreditation of private Facilities: ................................................................................................................. 114
New Intervention- JSY Helpline: Extending Help to the deserved: ................................................................ 115
Application for JSY beneficiaries: .................................................................................................................. 116
New initiative:................................................................................................................................................. 116
Maternal and infant death auditing committee: ............................................................................................. 116
Chiranjeevi Yojana ............................................................................................................................................. 117
Expected Outcomes......................................................................................................................................... 118
Reducing the ‘iron gap’ - improving distribution and compliance of IFA tablets among pregnant women to
control maternal anaemia................................................................................................................................... 118
Implementation Strategy:................................................................................................................................ 119
Broad Area of Activities for improving distribution and compliance of IFA tablets among pregnant mothers in
4 districts: ....................................................................................................................................................... 119
Budget Estimate:............................................................................................................................................. 120
Other Strategies on Maternal Health- ANC kits for pregnant women in disease-prone areas: ......................... 121
Preventing Post partum Haemorrhage in rural areas in institutional settings: ............................................. 121
Procurement of RTI/ STI kits: ......................................................................................................................... 122
Family Planning: ................................................................................................................................................ 124
Objectives: ...................................................................................................................................................... 124
Strategies: ....................................................................................................................................................... 126
Activities: ........................................................................................................................................................ 127
Private Partnership on Family Planning Process .............................................................................................. 127
Budget Estimation: ......................................................................................................................................... 127
Establishment of State Family Welfare Bureau: ................................................................................................. 129
Budget Estimation: ......................................................................................................................................... 129
Adolescent Reproductive Sexual Health in Chhattisgarh ................................................................................... 129
Objectives: -.................................................................................................................................................... 130
Strategies: ....................................................................................................................................................... 130
Activities: ........................................................................................................................................................ 131
Implementation of PNDT Act.............................................................................................................................. 134
Current Situation: ........................................................................................................................................... 134
Strategies: ....................................................................................................................................................... 134
Activities: ........................................................................................................................................................ 134
NRHM PIP 2009-10: Chhattisgarh
v
Training: ............................................................................................................................................................. 135
Maternal Health: ............................................................................................................................................ 135
Family planning: ............................................................................................................................................ 139
Adolescent Health: ......................................................................................................................................... 139
Laparoscopic sterilization training (LTT) ...................................................................................................... 139
TOT for district level trainers at state level: .................................................................................................. 140
Other Training Proposal from SIHFW: (Details annexed) ............................................................................ 141
Child Health ....................................................................................................................................................... 142
Objectives: ...................................................................................................................................................... 142
Strategies: ....................................................................................................................................................... 142
Activities: ........................................................................................................................................................ 143
Child Friendly Health Facility Accreditation: ................................................................................................... 143
Integrated Management of Neonatal and Childhood Illnesses (IMNCI) practice in institutional delivery ........ 144
Facility Based Newborn Care (FBNC) ............................................................................................................... 145
Integrated bi – annual maternal and child health month (Sishu Sanraksaan Maah) ......................................... 146
Operational strategy ....................................................................................................................................... 147
Micronutrient Initiative: ............................................................................................................................. 148
UNICEF: .................................................................................................................................................... 149
School Health Programme- “Swasth Pathshala Yojana” .................................................................................. 150
Introduction: ................................................................................................................................................... 150
Primary, middle and secondary schools:........................................................................................................ 150
Middle schools:............................................................................................................................................... 151
The Strategies for Swasth Pathshala Yojana: ................................................................................................. 151
Care of children with Severe or Acute Malnutrition - Baal Suposhan Yojana ................................................... 152
Background: ................................................................................................................................................... 152
Operational strategy: ..................................................................................................................................... 152
Swagath’ Package for Mothers and Newborns for institutional deliveries (A package of services for mothers and
newborns) ........................................................................................................................................................... 154
Introduction .................................................................................................................................................... 154
Rationale......................................................................................................................................................... 154
Objectives: ...................................................................................................................................................... 155
Implementation Strategy:................................................................................................................................ 155
Areas of support: ............................................................................................................................................ 156
Budget Estimate:............................................................................................................................................. 156
Management of Diarrhoea with ORS and Zinc: ................................................................................................. 157
Community-based Trial Demonstrates Longer-term Benefits of Zinc: ........................................................... 158
Suggested Points for scaling up Zinc and Lo ORS in Chhattisgarh. .............................................................. 158
NRHM PIP 2009-10: Chhattisgarh
vi
Support by Stakeholders for Scaling up revised diarrhoea management program ........................................ 160
Name of the Stakeholders ........................................................................................................................... 160
Suggested areas of Support by different Stakeholders: .................................................................................. 160
Implementation Strategy:................................................................................................................................ 161
Broad Area of Activities for scaling up Revised Diarrhoea Management Program ...................................... 162
Scaling up revised diarrhoea management (Zinc + Lo ORS) in all districts of Chhattisgarh (2009-10) ....... 162
Home Based Neonatal Child Care (HBNCC) ..................................................................................................... 164
Project Phasing: ............................................................................................................................................. 164
Current Status ................................................................................................................................................. 164
Area to be covered under HBNCC Phase I: ................................................................................................... 165
Selection of blocks: ..................................................................................................................................... 165
Kanker district: Blocks: .............................................................................................................................. 165
Raipur district: Blocks:............................................................................................................................... 165
Bastar district: Blocks: ............................................................................................................................... 165
Objective ......................................................................................................................................................... 165
Strategy ........................................................................................................................................................... 166
Operational Activities with Objective ............................................................................................................. 168
Selection of Mitanins .................................................................................................................................. 168
Incentives to Mitanin for HBNC home visits Interface with local Public health functionaries: ................. 168
Programme Management Structure............................................................................................................ 169
Base line and annual surveys: .................................................................................................................... 169
Operational Challenges .................................................................................................................................. 169
SEARCH, Gadchiroli role .............................................................................................................................. 171
Timeline for different activities in Phase I: .................................................................................................... 171
Crèches in district hospitals: .............................................................................................................................. 173
Objective to provide crèches facility in the districts hospitals ....................................................................... 173
Strategies ........................................................................................................................................................ 174
Budget requirements for one district hospital ................................................................................................ 174
Urban RCH ......................................................................................................................................................... 174
Urban health systems: .................................................................................................................................... 174
Objectives: ...................................................................................................................................................... 174
Strategies: ....................................................................................................................................................... 174
Progress So far: .............................................................................................................................................. 175
Strategies: ....................................................................................................................................................... 175
Activities: ........................................................................................................................................................ 177
Budget Requirements: ..................................................................................................................................... 178
Infrastructure: ................................................................................................................................................ 178
NRHM PIP 2009-10: Chhattisgarh
vii
Implementation of IMEP and quality assurance cell .......................................................................................... 178
Institutional Strengthening ............................................................................................................................. 179
Strengthening of BCC/IEC ................................................................................................................................. 179
Current Status ................................................................................................................................................. 179
Objectives ....................................................................................................................................................... 181
Strategies ........................................................................................................................................................ 181
Activities ......................................................................................................................................................... 182
Indicators ........................................................................................................................................................ 183
Programme Management: .................................................................................................................................. 185
Equity/Gender..................................................................................................................................................... 190
Financial management ....................................................................................................................................... 191
Convergence/Coordination................................................................................................................................. 191
MNGO / FNGO Programme in Chhattisgarh: ................................................................................................... 192
Establishment of procurement cell ..................................................................................................................... 193
District and Block Plans ..................................................................................................................................... 193
Definition of Roles of Each Levels .................................................................................................................. 193
Synergy with other NRHM Components ......................................................................................................... 194
PART B: SPECIAL INITIATIVES UNDER NRHM ............................................................................................ 196
Introduction: ....................................................................................................................................................... 196
Outcomes for Disease Control Programmes .................................................................................................. 197
Sub-centres: .................................................................................................................................................... 197
PHCs: ............................................................................................................................................................. 197
CHCs: ............................................................................................................................................................. 198
District Hospitals: .......................................................................................................................................... 198
Reduction of child malnutrition levels ............................................................................................................ 198
Filling the HR Gaps ........................................................................................................................................ 199
Decentralisation of health services and increased public participation in all health services ....................... 199
Professionalization of Management: .............................................................................................................. 199
Jeevan Deep Samitis: Making PHCs and CHCs fully functional ....................................................................... 200
Situation Analysis: .......................................................................................................................................... 200
Objectives: ...................................................................................................................................................... 200
Key Operational Elements:............................................................................................................................. 200
Strengthening Routine Sub-centre functioning ................................................................................................... 203
ISO Certification................................................................................................................................................. 203
Assistant Auxiliary Nurse Midwives: .................................................................................................................. 205
Support for Sub centres and PHCs Infrastructure .............................................................................................. 206
Appointment of Hospital Management Professionals for Public Health Facilities for Technical Assistance: ... 206
NRHM PIP 2009-10: Chhattisgarh
viii
Augmentation of Clinical Human Resources through developing ANMs from upgraded Nursing Training
Facilities: An Alternative Approach ........................................................................Error! Bookmark not defined.
The proposed study for development of Alternative Nursing Staff ......................Error! Bookmark not defined.
Training of LHVs: Lady Health Visitor (LHV) Cadre ........................................................................................ 211
Tribal Health ...................................................................................................................................................... 211
Filling Gaps in Rural Medical Services: ............................................................................................................ 211
Utilising the ongoing Three Year Medical Training Programme in the State. ............................................... 211
Reservation for candidates from tribal areas for Nursing and ANM courses: ............................................... 213
Closing Residential Gaps: .................................................................................................................................. 213
Distribution of Insecticide treated bed nets for families in high-risk tribal areas: ............................................ 214
Support in creation of Rural Medical Corps in difficult (conflict) areas in Chhattisgarh.................................. 215
The perks and payments.................................................................................................................................. 216
Quantification of the Allowances and Other Perks ........................................................................................ 217
Recruitment policy .......................................................................................................................................... 217
Career scopes ................................................................................................................................................. 218
Golden Handshake Offer: ............................................................................................................................... 218
Fund for Chhattisgarh Rural Medical Corps ................................................................................................. 218
Strengthening the Mitanin Programme under ASHA: ........................................................................................ 219
Current Situation ............................................................................................................................................ 219
Plan for the Mitanin Programme: .................................................................................................................. 222
Ongoing operational activities with objectives ........................................................................................... 222
The new operational activities with objective ............................................................................................. 224
Indicators: ...................................................................................................................................................... 226
Institutional Mechanism: ................................................................................................................................ 227
Budget Estimate:............................................................................................................................................. 227
Mobile Medical Unit:- ........................................................................................................................................ 229
Bal Hruday Raksha Yojana: Chief Ministers’ Child Heart Protection Scheme ................................................. 231
Strengthening the Village Health & Sanitation Committee ................................................................................ 232
Current Status: ............................................................................................................................................... 232
The achievements of the Mass Social Mobilisation Campaign “Gram Swasthya Niyojan Abhiyan” are as
follows:- .......................................................................................................................................................... 233
Operational objectives: .................................................................................................................................. 238
Strategies: - .................................................................................................................................................... 238
Activities: -...................................................................................................................................................... 238
Main Indicators: - ........................................................................................................................................... 240
Institutional Mechanism: ................................................................................................................................ 240
Monitoring and Evaluation................................................................................................................................. 241
Health Management Information System ........................................................................................................... 241
NRHM PIP 2009-10: Chhattisgarh
ix
Documentation Management Solution and Digitization Services ...................................................................... 243
Professional Health Management/Training of BMHOs and Reorientation of CMHO ....................................... 243
Current Status of trainings conducted: ........................................................................................................... 243
The training curriculum .................................................................................................................................. 245
First round of training:................................................................................................................................... 245
Second round of training ................................................................................................................................ 245
Third round of training- could be optional- or only at state level. ................................................................. 246
Community-Based Monitoring of Health Services ............................................................................................. 247
Current Status: ............................................................................................................................................... 247
Objectives ....................................................................................................................................................... 249
Key Strategic action........................................................................................................................................ 249
Activities ......................................................................................................................................................... 250
Indicators ........................................................................................................................................................ 251
Budget for implementing Community based Monitoring in 3 new districts .................................................... 252
The State Level Resource Support: The SHRC ................................................................................................... 256
Sickle Cell Anaemia: (Detection, management and prevention of sickle cell anaemia in Chhattisgarh) ........... 258
Introduction: ................................................................................................................................................... 258
Prevalence: ..................................................................................................................................................... 259
The Present Scenario:..................................................................................................................................... 259
Objectives ....................................................................................................................................................... 260
Strategies and activities .................................................................................................................................. 260
Prevention: ..................................................................................................................................................... 260
Surveillance and counselling centre: .............................................................................................................. 261
AYUSH component under NRHM for 2009-10 ................................................................................................... 262
Flexible fund for AYUSH Deep Samiti for monitoring ................................................................................... 263
Essential medicine for AYUSH centres in rural, remote and tribal areas .................................................. 264
Additional manpower for AYUSH units in CHC and PHC ............................................................................. 264
Telephone Connection for AYUSH district hospitals: .................................................................................... 265
Essential maternal and child health training for AYUSH doctors .................................................................. 265
Public health management training for AYUSH MOs .................................................................................... 266
National level consultative workshop for AYUSH mainstreaming ................................................................. 266
AYUSH training for ANMs and Anganwadi workers...................................................................................... 267
Training of paramedical staffs for AYUSH ..................................................................................................... 268
Supporting AYUSH cell in SHRC: .................................................................................................................. 269
Consultancy for developing an action plan for AYUSH epidemic management ............................................. 270
Support to maternity and child wards in government Ayurveda Colleges ...................................................... 270
AYUSHDEEP Samiti ...................................................................................................................................... 270
NRHM PIP 2009-10: Chhattisgarh
x
AYUSH melas in Block and District head quarters ........................................................................................ 271
AYURVEDGRAM ........................................................................................................................................... 271
AYUSH Component under NRHM for 2009-10 .............................................................................................. 272
Third Party Monitoring ...................................................................................................................................... 272
Filling up vacancies and Human Resource management ................................................................................... 275
Special initiative: Establishment of Snakebite Case Management Unit in district hospital ............................... 276
Capacity Building and Mobilization of PRI for local Health Planning: ............................................................ 277
Current Status: ............................................................................................................................................... 277
Programme Management ................................................................................................................................... 278
Chhattisgarh Health Equipment Management System ....................................................................................... 279
Introduction: ................................................................................................................................................... 279
Activity:........................................................................................................................................................... 279
Training: ......................................................................................................................................................... 279
Budget estimation: .......................................................................................................................................... 280
PART C – PIP ON IMMUNIZATION ................................................................................................................. 281
Reported and evaluation coverage: .................................................................................................................... 281
Outbreaks reported and outbreaks investigated in the last year .................................................................... 282
Assessment of critical bottlenecks for full coverage ....................................................................................... 282
Utilization / Adequate Coverage: ................................................................................................................... 282
Objective: ....................................................................................................................................................... 282
Action Plan and Budget for 2009-10: ............................................................................................................. 283
PART D: NATIONAL DISEASE CONTROL PROGRAMMES ........................................................................... 289
Revised National Tuberculosis Programme ....................................................................................................... 289
Situation analysis & epidemiological parameters for Chhattisgarh .............................................................. 289
Activities in RNTCP ........................................................................................................................................ 291
Monitoring & Evaluation ............................................................................................................................... 291
National Vector Borne Disease Control Programme ......................................................................................... 292
Situational analysis with epidemiological parameters: .................................................................................. 292
Epidemiological Situation of Malaria in Chhattisgarh State ......................................................................... 294
Burden of vector-borne diseases: ............................................................................................................... 294
Activities ......................................................................................................................................................... 294
Proposed Interventions in Relation to the Objectives and Strategies ............................................................. 295
Integrated Vector Control Management ......................................................................................................... 295
Monitoring and evaluation ............................................................................................................................. 299
Filariasis: ........................................................................................................................................................... 300
Mass Drug Administration – 2007: ................................................................................................................ 300
Proposed activities for Lymphatic Filariasis elimination: ............................................................................. 301
NRHM PIP 2009-10: Chhattisgarh
xi
Monitoring And Evaluation: ........................................................................................................................... 302
Budget Summary: ........................................................................................................................................... 302
Leprosy Eradication ........................................................................................................................................... 310
Situational Analysis with epidemiological Parameters .................................................................................. 310
Prevalence ...................................................................................................................................................... 312
Grade I disability among new cases ............................................................................................................... 312
Reconstructive Surgery ................................................................................................................................... 312
Analysis of BLAC (BLOCK LEPROSY AWARENESS CAMPAIGN) since 2004 ............................................ 313
Constraints:- ................................................................................................................................................... 315
Activities: ........................................................................................................................................................ 315
Monitoring and evaluation ............................................................................................................................. 316
Budget Summary for Leprosy programme ...................................................................................................... 316
Urban Leprosy Control Programme............................................................................................................... 319
Supervision, Monitoring and Review .............................................................................................................. 320
National Blindness Control Programme ............................................................................................................ 321
Situation analysis with epidemiological parameters in CG ............................................................................ 321
Activities: ........................................................................................................................................................ 322
Monitoring and Evaluation: ........................................................................................................................... 325
Monitoring and Evaluation team .................................................................................................................... 325
Integrated Disease Surveillance Project ............................................................................................................ 327
Situation analysis with epidemiological parameters: ..................................................................................... 327
Out breaks reported in the year 2008-09 under IDSP .................................................................................... 328
Activities at the state level will include: ......................................................................................................... 330
Monitoring and evaluation of programme will be done based on following Indicators ................................. 330
National Iodine Deficiency Disorders Control Programme (NIID) ................................................................... 337
Situation Analysis: .......................................................................................................................................... 337
Activities: ........................................................................................................................................................ 337
Monitoring of Programme .............................................................................................................................. 338
PART E: CONVERGENCE ................................................................................................................................ 339
Introduction: ....................................................................................................................................................... 339
Prevention of Anaemia among children and adolescents: .................................................................................. 339
Referral of sick Newborn, Young child and malnourished children with complications. ................................... 340
Timely initiation of Complementary Feeding- .................................................................................................... 340
Integrated Health, Nutrition, Immunisation and Development card for children and mothers: ........................ 340
AYUSH Orientation ............................................................................................................................................ 340
Bal Suposhan Yojana- ........................................................................................................................................ 340
Swasth Pathshala Yojana: .................................................................................................................................. 340
NRHM PIP 2009-10: Chhattisgarh
xii
Monthly village health and nutrition Melas: ...................................................................................................... 340
Involvement of Total Sanitation Campaign in quality of health services– ......................................................... 341
Budget Requirements: ..................................................................................................................................... 341
Provisional NRHM PIP 2009-10: to be submitted to GoI- at a glance ..................Error! Bookmark not defined.
NRHM PIP 2009-10: Chhattisgarh
xiii
INTRODUCTION
Background
Chhattisgarh carved out of Madhya Pradesh came into being on 1 November 2000 as the
26th State of the Union. It fulfils the long-cherished demand of the tribal people for having
their own state. The state of Chhattisgarh has an area of 1, 35,191 sq. km. with 18 districts
(two of them, Bijapur and Narayanpur being created recently), 146 blocks, and 20308
villages.
It is one of the few landlocked states of the country. Uttar Pradesh and Bihar bind the State
in north, in the east it is bound by Orissa, in the south by Andhra Pradesh and in the west by
Madhya Pradesh and Maharashtra. A large part of the state comes under Vindhyachal range
that divides the Indian subcontinent into two. The middle part of the state is mostly plane
land while both the northern and southern parts are largely plateau area covered with dense
forest. Mahanadi and Narmada are the principal rivers of the state. The main crop of the
state is paddy which is cultivated only once in a year due to dependency on rain.
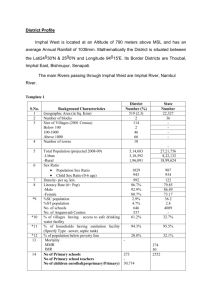
Demographic and Health Profile of Chhattisgarh
It has a population of 20.83 million (Census 2001) and population density of 154 per sq. km.,
one of the less densely populated states in India (as against the national average of 312).
This is because a large portion of the state (44%) is covered with lush green forests
sheltering large number of tribal populations (32% of overall state populations) and 12% of
Scheduled caste populations. Other Backward Caste (OBC) population totals to 45%.
Therefore, overall 89 % population of the state is disadvantaged in different ways, drawing
special attention from the centre for their upliftment based on Social Justice.
The decadal growth rate of the state is not available as the state is less than a decade in
existing (against 21.54% for the country). However, the population of the state is growing at
a slower rate than the national rate.
Table 1.1: Demographic Profile of Chhattisgarh
S. No.
Item
Chhattisgarh
India
1
Total population (Census 2001) (in millions)
20.83
1028.61
2
Decadal Growth (Census 2001) (%)
NA
21.54
3
Crude Birth Rate (SRS Oct -2008)
26.5
23.1
4
Crude Death Rate (SRS Oct -2008)
8.1
7.4
NRHM PIP 2009-10: Chhattisgarh
Page 1
5
Total Fertility Rate (SRS 2006)
3.4
2.9
6
Infant Mortality Rate (SRS Oct -2008)
59
55
7
Neonatal Mortality Rate ( NFHS III)
63.5
48.5
8
Maternal Mortality Ratio (SRS 2001 - 2003)
379
301
9
Perinatal Mortality Rate (SRS 2005)
44
301
10
Sex Ratio (Census 2001)
989
933
11
Population below Poverty line (%)
41
26.1
12
Schedule Caste population (in millions)
2.42
166.64
13
Schedule Tribe population (in millions)
6.62
84.33
14
Female Literacy Rate (Census 2001) (%)
51.9
53.7
The Total Fertility Rate of the State is 3.4 a little high above the national level of 2.9. The
Infant Mortality Rate for the state has come down currently to 59 from previous figure of 79
at the time of formation of the state. This is a major achievement for the state considering the
fact that any reduction in IMR requires synergistic efforts from several departments and
improvement in social status. The Maternal Mortality Ratio of 379 (SRS 2001- 03) is slightly
higher than the National average (see the table below). The Sex Ratio in the State is 989 a
favourable one, compared to 933 for the country. Comparative figures of major health and
demographic indicators are as follows:
Table 1.2: Administrative Profile of Chhattisgarh
Administrative Units
Number
No. of districts
18
No. of blocks
146
No. of Gram Panchayats
9193
No. of Villages
20308
Structure of Chhattisgarh Public Health System
NRHM PIP 2009-10: Chhattisgarh
Page 2
NRHM PIP 2009-10: Chhattisgarh
Page 2
The Hon’ble Chief Minister is the premier for the overall public health system of
Chhattisgarh Health System. The Department of Health & Family Welfare is under the
portfolio for the State Health Minister. However, the executive decisions pass through the
chain of Chief Secretary and Secretary Health.
There are five main directors under the direct control of the Health Secretary. The Director,
SHRC in his additional technical support to the Department of Health and Family Welfare.
Mission Director, NRHM is the principal authority for the tasks related to the mission. The
Director undertakes the PIP formulation and subsequent execution of the plans with wellconcerted and coordinated support from several other departments besides health. The State
Programme Management Unit, District Programme Management Units, Block Programme
Management Units are the executive chain for successful implementation of the PIP plans.
Director AYUSH looks after the activities, including planning, implementation, monitoring
and evaluation of the programmes related to Indian systems of medicine such as Ayurveda
Yoga, Unani, Siddha and Homeopathy.
Director Health & Family Welfare is concerned with the state health and family welfare
programmes.
Director Medical Education and Training is concerned with the medical education and
training activities across the state.
Director SHRC provides additional technical inputs for planning, policy formation, strategy
execution, monitoring, and evaluation of the plans. Moreover, SHRC is involved in the
nurturing and development of 60000 cadres Mitanin (Community Health Volunteers)
Programme.
The Directors are supported by several Joint Directors and Deputy Directors in effective and
smooth functioning of the overall health systems.
The Chief Medical & Health Officers are in charge of the District Health Systems, while the
Civil Surgeons are responsible for proper functioning of the district hospitals. The DPMU
supports the functioning of the CMHOs while the BPMUs support the activities of the Block
Medical
Officers
in
implementation
of
NRHM
activities.
NRHM PIP 2009-10: Chhattisgarh
Page 3
The Health Infrastructure Situation
The overall health infrastructure of the state has been quite poor when the state received its
own independent status. Until recently, there was only one medical college for modern
medicine in the state at Raipur. Similarly, the number of sub centres, primary health centres or
community health centres were way below the requirement, keeping in mind that the state is
one of the sparsely populated with very remote and difficult to reach terrain with almost half of
its land covered with dense forests.
The state is also having presence of large number of indigenous practitioners in the form of
Ayurveda, Unani, Siddha and other systems along with Homoeopathy.
Table 1.3: Health Infrastructure of Chhattisgarh
Health Institution
Number (2007)
Number (2008)
Medical College
3
3
District Hospitals
14
14
Community Health Centre
113
137
Primary Health Centre
659
721
Sub-centre
4164
4758
Ayurvedic Hospitals
6
6
Ayurvedic Dispensaries
633
634
Unani Hospitals
0
0
Unani Dispensaries
6
6
Homeopathic Hospitals
0
0
Homeopathic Dispensary
52
52
(Source: RHS Bulletin, March 2007, M/O Health & F.W., GOI)
Continued efforts by the successive governments with support from NRHM and European
Union and similar other development partners’ organisations have helped to improve the
status to some extent. However, very few of the institutions would match the Indian Public
Health Standards (IPHS) norm.
Table 1.4: Gap filling of infrastructure in C.G. 2008-09 and 2009-10
Institution
State Budget
European Union Partnership NRHM
PHC
111
16
NRHM PIP 2009-10: Chhattisgarh
(of
earlier
year
in 0
Page 4
progress)
Health Sub Centre
250
290 (118 + 172 of earlier year 11
(
Naxalite
in progress)
affected areas )
AYUSH wing in CHCs
0
39
0
Drugs store centre
0
0
Nursing College
1
1 State
16 Districts
32 CHC
0
ANM Training Centre
3 Staff setup
4 (Building construction)
10 (Up gradation of
infrastructure )
Male Health Worker 1 Staff setup
Training Centre
2 ( Building Construction)
Residential
quarters 0
for health staff
in
PHCs
150 ( Building construction )
1 ( Tribal district )
199 ( Naxalite
affected 2 districts)
Health Workforce Status of Chhattisgarh
The health workforce situation of the state is still in real dearth. The state is lacking in almost
every category of health workforce. Worse still, the number of available nurses, doctors,
specialists and super specialists are below the requisite level. The condition is further
worsened by the fact that the state is yet to develop sufficient number of institutions for meeting
this
demand-supply
gap
in
human
resource
for
health
services.
Other Challenges
Poor Socio-economic status
The state is one of the poorest states of the country deserving to be included into the 18 EAG
states. There is pervasive poverty, hunger, malnutrition combined with poor water and
sanitation services. Endemicity of malaria (9% of India’s Malaria burden), leprosy, and
continued political conflict adds to the woe further.
Difficult Geographic Location
With large portion of the state either covered with forests or having plateau area with poor
connectivity and transport systems is a major problem for referral services.
NRHM PIP 2009-10: Chhattisgarh
Page 5
Vision and Goals for the Health Sector
The Government of Chhattisgarh is committed to achieve the level of mental, physical and
social well-being of its citizens through empowerment of local communities, framing of equity
and gender sensitive policies, reduction of poverty, provision of comprehensive healthcare
services. The Vision 2020 document of the state is in line with the Millennium Development
Goals.
The state will be guided by the principles of transparency, accountability, community
involvement, both the public, private, NGOs, to create a society allowing people to live their
life to the fullest, fulfilling their social responsibilities and contributing to national progress.
National Rural Health Mission
The National Rural Health Mission is a much welcome step for the state. It, along with support
from European Union, fills the gaps left unattended or underserved by the State due to
availability of limited resources. Mission’s aims to provide universal access to equitable,
affordable and quality health care that is accountable and responsive to the needs of the
people, reduction of child and maternal deaths as well as population stabilization, gender and
demographic balance is in line with the States Vision 2020 document.
Objectives of NRHM
Reduction of the IMR from the current 61 to 30 by the year 2012
Reduction of MMR from current 379 to about 100 by the year 2012
An increase of CPR to 65% by the year 2008 and reduction of total fertility rate to 2.1
and net reproduction rate to 1.0 by the year 2010
Achieving IPHS norms of service delivery in all sub-centres, PHCs and CHCs and
district hospitals by the year 2012
Making maternal health, child health and adolescent health care facilities, safe
abortion services and management of reproductive tract infections easily
accessible to all
Addressing the health issues in vulnerable communities like tribal population, urban
slum population, people living in conflict areas etc.
Effective outcomes on all disease control programmes
Making Community level first contact care as well as necessary referral supports
available to all
Reduction of child malnutrition levels
NRHM PIP 2009-10: Chhattisgarh
Page 6
Ensuring effective Coordination within the health department as well as ensuring
coordination with all sectors and programmes, which are determinants of good
health
Resolving the issue of finding skilled personnel to serve in medically underserved areas
through implementation of an improved health human resource development policy
and through appropriate public private and public civil society partnerships
Decentralisation of health services and increased public participation in all health
services and health management
Professionalization of management at all levels
Initiating community based monitoring and feedback system in order to improve the
quality of public health interventions through triangulation of monitoring
Mainstreaming of AYUSH systems
Improving Medical Education along with tertiary level health care facilities in the state
The Mission envisages achieving these targets in a manner that is affordable to the community
and equitable in distribution based on the varying needs of different strata of the population.
The Mission aims to bring about a change in the health sector that is gender sensitive, taking
care of the marginalised and vulnerable sections of the society, and people friendly.
Systemic Inputs
Governance Reforms
Empowerment of Panchayati Raj Institutions and Improved Efficiency of Health systems are
two cornerstones of National Rural Health Mission. The mission document envisages setting up
a platform for involving the Panchayati Raj institutions and community in the management of
primary health programmes and infrastructure; train and enhance capacity of Panchayati Raj
Institutions (PRIs) to own, control and manage public health services. Further, it counsels to
strengthen existing PHCs through better staffing and human resource development policy,
clear quality standards, better community support and an untied fund to enable the local
management committee to achieve these standards. Integrating vertical Health and Family
Welfare programmes at State, District and Block levels is another dimension of this mission.
To achieve all these aspirations the State must have possess a core group of team leaders. They
will be involved in supervising, mentoring and regulatory activities. Without such dedicated
team leaders, delegation, devolution of powers and responsibilities will result in poor planning
and implementation at lower levels. Chhattisgarh initiated several reforms in view of the above
objectives. Some of the important ones are briefly described below.
Introduction of Commissioner System
NRHM PIP 2009-10: Chhattisgarh
Page 7
One of the key efforts of the state is appointment of a Health Commissioner at state level. The
Commissioner will supervise and coordinate the activities of three state level Directors, viz.
Directors of Family Welfare, Health Services and Health Training.
Strengthening of Directorates
To improve the efficiency of the system at state level, three Directors have been appointed, viz.
Directors of Family Welfare, Health Services and Health Training. Through this, each of the
divisions shared heavy workload that previously bogged down the system, resulting in delay in
plan implementation, poor planning and other administrative bottlenecks. The Director of
Health Training has been especially created to take care of the ensuing heavy load of training
and capacity building efforts in near future.
Filling up Positions of Joint Directors and Deputy Directors
Five Joint Directors and Deputy Directors have been selected from the public health officials.
They are supporting the Directors in integration of efforts, coordination among health
divisions and with other departments.
Filling up vacancies of State Programme Management Unit (SPMU)
To improve the functioning of the NRHM wing of the health sector, one state programme
manager, one state finance manager, 5 state level consultant and 6 district programme
managers have been appointed with support from National Health System Resource Centre
(NHSRC).
Filling up Positions at District and lower levels
After formation of the state in 2000, many districts were without any Chief Medical and Health
Officers. This hampered planning, implementation and monitoring activity at grass root levels.
In addition, many of the CHCs, PHCs etc. were running without adequate work force. The state
took initiatives to have one CMHO and one DHO at each of the 16 districts. Similarly, 250
specialists, 354 MPWs, 161 LHVs have been appointed at grass root levels. However, it is still
inadequate and the state will take similar measures to reduce the demand supply gap.
Similarly, seven-district account manager, eight district data assistants, one hundred and forty
six block programme manager and data assistants were appointed by State Health Resource
Centre, Raipur.
Devolution of Powers to Block Medical Officers
This is a bold step taken by the State. The Block Medical Officers have been given the power of
Drawing and Disbursal Officer. Through this measure, more decentralized decisions making
on health activities and quick fund release and utilization have been materialized. This effort
will bear fruits after sometime and then it is likely to be held as key step in decentralised
planning and implementation process.
Electronic Procurement and Funds Transfer
NRHM PIP 2009-10: Chhattisgarh
Page 8
Establishment of electronic procurement and electronic funds transfer are signal events in
health sector reform of the state. E-tendering and procurement of equipments, drugs and such
other items will help to promote transparency, speediness with simultaneous involvement of
vendors from across the nation. So far, e-tendering has been adopted for Health Management
Information System, selection of Insurance Company for Rashtriya Swasthya Bima Yojana,
Medical Mobile Units, Drug & Equipment procurement.
Revision of Essential Drug List
Rational use of drugs is a burning issue dogging the nation. To overcome the issue
Chhattisgarh had formulated an “Essential Drug List” in 2002. However, the drug industry is
a rapidly evolving industry and needs constant updating. Thus, an initiative was taken with
assistance from State Health Resource Centre, Medical Colleges and select Peripheral Medical
Officers to revise this list. The revised essential drug list, in year 2007, contains total 350
drugs and consumables and it has been endorsed by the Government.
Integrated Health Equipment Management System
Health sector is mainly a service sector with 60 – 65 % of the cost going for remuneration.
However, 25 – 30 % of the cost is spent on drugs and equipments. Therefore, this area offers
an opportunity to undertake measures for cost containment. Keeping this in mind, the
Chhattisgarh Health Equipment Management System has been created as a part of an
integrated inventory management system. There are one State Cell and two regional workshops
under this system. This system is taking care of rationalized procurement, immediate repair of
small equipments, supervising the annual maintenance contract for costly equipments.
Moreover, this system is undertaking capacity building measures to improve the skills and
knowledge of different cadres of technicians in preventive maintenance and repair.
NRHM PIP 2009-10: Chhattisgarh
Page 9
Summary of Health Sector Achievements
After the state formation, health sector reforms in the state have been given a major thrust and
the state has achieved stupendous success in bettering basic health indicators, in ensuring
quality health services and in improving the public health infrastructure. The rural infant
mortality rate has registered a major decline during this period. In 2003, the Rural IMR was
77 per 1000 live births whereas presently it is 62, which is equal to the national average. The
growth has also been tremendous in the health services scenario. The Comparison of National
Family Health Survey-2 during formation of the state and the NFHS-3 with the very recent
status gives a testimony to this growth.
The IMR scene : Growth in Chhattisgarh 2000-2008:
A comparison with India and Madhya Pradesh, the mother state
72
77
6162
59
61
62
55
NRHM PIP 2009-10: Chhattisgarh
Page 10
Infant deaths per 1000 live births
Trend of IMR in Chhattisgarh
Rural
100
95
Mitanin Programme Started
Urban
90
Mitanin Programme Scaled up
88
85
80
Total
All Mitanins in action
79
77
77
73
70
70
65
63
62
61
61
60
60
Goal as per CG
Health &
Population
policy
61
59
58
55
52
51
50
49
52
50
49
> 80% pediatricians in urban areas
40
30
30
2000
2001
2002
2003
2004
2005
2006
2007
2008
2009
2010
2011
2012
2013
2014
2015
Reference year
IMR source: SRS
Comparison of Key trends under NFHS-2 and NFHS-3:
Trends in Contrceptive Prevalance
Rate
Percentage of women who received
ANC
54
52
53
89
50
48
57
46
44
45
42
40
Chhat t isgarh
NFHS-2
NFHS-2
NFHS-3
Percentage of children age 12-23
months received BCG+3 Polio+3
DPT+Measles
60
49
40
20
22
0
Pecentage of Children Got all 3 Polio
Vaccines
90
80
70
60
50
40
30
85
57
NFHS-2
NFHS-2
NFHS-3
NFHS-3
NFHS-3
NRHM PIP 2009-10: Chhattisgarh
Page 11
It could also be seen that the health service indicators like Contraception prevalence rate,
women receiving ANC, Children receiving full immunisation has improved in a much visible
manner and malnourishment among children has decreased. An independent evaluation done
by UNICEF and the District Level Household Surveys also project a very good improvement of
health services in the state. One of the major community level achievements marked is the
growth in breastfeeding- the colostrums feeding, early initiation of breastfeeding as well as
exclusive breastfeeding- that has extreme potential in reducing the neonatal mortality. This
was the result of comprehensive community level health education drives that the state
government was able to gear up through various measures like folk art based communication
programmes followed by good service delivery together by health department staff and
Mitanins. Another achievement has been the reduction of malnourishment among children
below 3 years- credit of this goes to the interdepartmental coordination that was key agenda of
the government.
Tendencies in Breast Feeding in Chhattisgarh
Children age bel ow 3 years who are
underweight (%)
100%
DLHS 2002 - 04
CES 2006
90%
80%
70%
70
60
60%
61
52
50
50%
40
40%
30%
20%
10%
0%
Initiation in 24
hours
Colostrum
feeding
Exclusive
breastfeeding
Winner of the 4th JRD Tata Memorial awards 2008
Population Foundation of India instituted JRD TATA Memorial Award to recognize the efforts
made by the state and districts on Population and Reproductive Health Programmes. Till date,
there were three awards in three different years-1997, 1999 and 2002. The 4th JRD TATA
Memorial Award 2008 was bagged by Chhattisgarh. The award ceremony was recently held at
New Delhi, on 9th of January 2009.
The 4th JRD Tata Memorial awards for excellence in reproductive health & population
programmes for the year 2008 is won by Chhattisgarh. The State with a score of 115.8 ranked
first among the bigger states, followed by Rajasthan & Andhra Pradesh with scores of 103.5 &
100.6 respectively.
Chhattisgarh has made significant strides in developing an educational and health
infrastructure and transport and communication networks. These advances had a significant
impact on the socio-economic and demographic status of the state. Chhattisgarh ranks
favourably in many of the indices used to determine the performance of reproductive and child
health programmes in the states. Chhattisgarh has made improvement in almost all the
indicators considered for the 4th JRD Tata Memorial award. Full immunization for the state
improved from 20.0 in 1998-99 to 48.7 in 2005-06. Similarly, for at least three ANC visits, the
NRHM PIP 2009-10: Chhattisgarh
Page 12
figure got a boost from 33.2 in 1998-99 to 54.2 in 2005-06. The state has also shown
improvement, in safe delivery, children underweight and infant mortality rate.
Selection of the Best Performing State
Step 1: At first step, as it has been followed by UNDP for Human Development Index (HDI)
each variable was converted into an index ranging from 0 to 100. The index was computed as:
For positive indicators (like use of family planning and utilization of ANC):
Index =
(State value - Minimum Value)
x 100
(Maximum value - Minimum value)
For negative indicators (like TFR and IMR):
Index =
(Maximum value – State value)
(Maximum value - Minimum value)
x 100
Step 2:Secondly, a composite index was computed for base year and final year based on these
fourteen indices. This composite index is the simple average of fourteen indices.
Step 3: Thirdly, a score was obtained for each state by combining the recent levels and changes
over the base and final years in the composite index in the ratio of 1:4.
After final ranking of the nineteen bigger states (population of 10 million and above) on the
basis of composite index, Chhattisgarh emerged as the best state and among the ten smaller
states (population of less than 10 million) Sikkim emerged as the best state. Chhattisgarh got a
high score among all the bigger states in the composite index as the change was observed to be
the highest among all the 19 bigger states. Similarly, among 10 smaller states, Sikkim emerged
as the winner state, as the change in between the base year and the final year for Sikkim was
observed to be the highest.
Methodology: The selection of the states for the state level award 2008 has been done based on
14 indicators, for which data were compiled from various published sources. These indicators
were finalized based on recommendations of the Technical Advisory Committee. These
indicators have a strong bearing on reproductive health, gender equity, family planning and
fertility levels of the population.
Table 1.5: Source of Indicators
Sl. No.
Indicator
Source
1
Women(20-24 years) married before age 18
NFHS II & III
2
CPR (Contraceptive Prevalence Rate) –any
NFHS II & III
methods
3
Full Immunization
NFHS II & III
4
TFR(Total Fertility Rate)
NFHS II & III
NRHM PIP 2009-10: Chhattisgarh
Page 13
5
At least 3 ANC(Ante-natal checkups) visits
NFHS II & III
6
Safe Delivery
NFHS II & III
7
% Children underweight(weight for age)
NFHS II & III
8
IMR (Infant Mortality Rate)
SRS (Sample Registration System),
1999 and 2005
9
Under Five Mortality Rate (Male/Female
Indirect Estimates, Census 2001
Ratio)
10
Child Sex Ratio(0-6 years)
Census, 1991 and 2001
11
Girls School Attendance Rate (6-14 years)
Census, 1991 and 2001
12
Female Youth (15-24 years) Literacy Rate
Census, 1991 and 2001
13
Literacy Rate (7 and more years)
Census, 1991 and 2001
14
National
Human
Development
Planned Expenditure on Social Sector,1997
Report,2001 and Statistical Abstract
and 2004
India,2001
NRHM PIP 2009-10: Chhattisgarh
Page 14
Indicators, and Ranking of States for the 4th JRD Tata Memorial Awards
Table 1.6: Index Values for Base and Final Years and Ranking:
State
Rank
of
NFHS
III
Composite
Composite
index
(U5 index,
excluded),
NFHS II
NFHS III
Rank
of
NFHS
II
Change
Rank
(NFHSIII- Change
II)
(NFHS
III-II)
4*Change Rank of 4* Final Final
Change
Index Rank
(NFHS IIIII)
Chhattisgarh 61.8
19
58.9
45.4
24
13.5
1
54.0
1
115.8
1
Sikkim
73.5
5
71.5
61.9
12
9.6
5
38.3
5
111.8
2
Uttarakhand
66.4
15
63.8
53.8
19
9.9
3
39.7
3
106.1
3
Rajasthan
51.0
26
50.8
37.7
27
13.1
2
52.5
2
103.5
4
Manipur
70.7
9
70.3
62.8
9
7.5
11
30.0
11
100.8
5
Andhra
Pradesh
68.9
11
66.5
58.5
13
7.9
9
31.8
9
100.6
6
Tamil Nadu
78.6
3
77.5
72.2
5
5.2
17
21.0
17
99.6
7
16
65.2
57.7
16
7.5
12
30.0
12
95.9
8
14
64.7
57.9
15
6.8
13
27.4
13
94.6
9
8
69.4
63.6
8
5.7
15
23.0
15
94.5
10
Jammu
Kashmir
Composite
index,
NFHS III
& 66.0
West Bengal
67.2
Maharashtra 71.6
NRHM PIP 2009-10: Chhattisgarh
Page 15
Apart from above, the state was able to record major achievements in disease control - like:
NFHS-2
NFHS-3
Yaws - Disease of the underdeveloped areas- has been eliminated from the state and it
is marching towards eradication. There were 15 identified cases of Yaws were
there in the state in 2003, whereas within a year, this was brought down to zero.
The Chhattisgarh efforts on this has been highly appreciated by World Health
Organisation and our officials are now been invited to support the Yaws operations
in countries like Indonesia.
The Polio scene has also been controlled very well during this period. During the
initial days of the state, a threat of polio was prevalent as some cases were
reported in the state during that time. With effective surveillance systems,
management and immunisation initiatives, the disease have been prevented as
much as possible and “no case” has been reported till date.
Leprosy is another disease, which is reaching the elimination stage. In 2003, the
prevalence rate was 7.20 per 10000 populations, which have been brought down to
1.99 through persistent efforts. In 6 out of 16 districts, national goal of less than 1
prevalence rate has been achieved and the remaining districts are moving quickly
to achieve this.
Towards achieving better impact of TB control programme, the first step that the State
adopted was to expand the programme to cover all 16 districts whereas it was
covering only 4 districts earlier.
In Malaria control, the major achievement is the very efficient level of control in
malaria epidemics- this is despite the fact that the state is highly endemic if
compared to any other state of the country. The death tally, which was 98 during
the period 2000-03, has been brought down to 15 in the last 3 years. The Annual
Parasite Incidence, which was 10.6 in 2003, has been brought down to 5.6 as result
of the dedication rendered by the Health Department. Still, three of the southern
districts where API is high are under high focus.
Towards Controlling HIV/AIDS , the awareness programmes as well as voluntary
counselling/testing has been optimised. Effective target intervention as well as
blood transfusion facilities has been achieved as well as the state was able to
successfully negotiate for making ARV treatment available for the state which was
not available till 2004. 52 Integrated counselling and treatment centres and 33
STD clinics initiated. Initiation of state of the art model blood bank and the
constitution of state blood transfusion council are also notable achievements.
The Scenario of Blindness control has improved to one of the best programmes of the
country during this period. We could initiate a Public Private Partnership also, in
the area of advanced eye care, with MGM Eye Institute, Raipur.
NRHM PIP 2009-10: Chhattisgarh
Page 16
In order to make advanced health care facilities, especially cardiac surgery, available
to the people, the MoU with Escorts hospital was renewed with more pro-poor
clauses and conditions. Similarly, a new 100 bedded cancer hospital is coming up
in Raipur as a joint venture with Vedanta.
A special programme to control Sickle Cell Anaemia , a specific disease prevalent in the
state is also being run. Operational research, mass screening and counselling as
well as other measures initiated where support from Red Cross society is also
availed.
An Integrated Disease Surveillance Programme has been launched in order to sharpen
the operations related to disease control initiatives.
The Reproductive & Child Health Programme as well as National Immunisation
Programme also has been implemented by the state with utmost priority. Under
Janani Suraksha Yojana, the institutional delivery level has gone up which was
about 16% earlier and further major hike is expected during this year.
All these achievements are results of better planning, of optimum use of technical
efficiency and of bringing together all stakeholders. The government has taken
major initiatives to improve the community participation in health, quality of health
care services as well as adequate health infrastructure and manpower provisions.
An innovative institutional model has been set up in the form of state-civil society
joint initiative, the State Health Resource Centre to shape the reform processes
and to initiate them wherever it is necessary. Some initiatives that the state took are
widely appreciated, like:
Optimising the Community Level Measures – The Mitanin Programme : The Mitanin
Scheme of community based health services, what began as very small community
level project has become a model and path paver scheme for the entire country.
The scheme has undergone a major expansion during the last few years to a
massive coverage of more than 60000 Mitanins or voluntary health activists who
are giving their voluntary services in every hamlet and in every nook and corner of
the state. They have undergone 10 rounds of trainings including the one on
integrated management of neonatal and childhood illnesses and giving first level
curative care using Mukhyamantri Dawa Peti Scheme. The Mitanin Scheme has
been grown to such a level during this period that it influenced the design of ASHA
(Accredited Social Health Activist) scheme under the National Rural Health
Mission launched by Government of India.
Improving Performance of the Hospitals - The Jeevan Deep Approach : In order to
improve the quality of management of the government run hospitals and to change
the perceptions of general community about the poor quality of services in
government hospitals, a pioneering hospital reform scheme called the Jeevan Deep
Scheme has been put in place in the state. Under this novel scheme a more
responsive, more representative, more people oriented and more target centric
hospital management committees called Jeevan Deep Samitis have been created for
NRHM PIP 2009-10: Chhattisgarh
Page 17
every level of government hospitals upto the PHC. These committees will also have
the power to recommend disciplinary action against non-performing officials.
Under this scheme, every hospital in the state will be graded based on its service
quality and best hospitals will be given Jeevan Deep gold stars, silver stars and
bronze stars respectively. The best hospital in every district will get Rs. 2 Lakhs as
reward for good services. Chhattisgarh is the pioneer state to have launched such a
peoples friendly target oriented scheme. It will be a marked departure from the old
Rogi Kalyan Samitis, which were running the hospitals earlier. Korba, Ambikapur
and Durg are Silver Star hospitals. The Korba District Hospital has been certified
for ISO 9001:2000.
Developing FRU facilities and bridging specialist gaps: the Equip Initiative : In terms
of closing the gaps in infrastructure, skilled manpower and equipment in parallel to
addressing quality and adequacy of utilization of services, a new block by block
approach has been adopted by the state. This approach goes by the acronym
“EQUIP”-Enhancing QUality in Primary health care- and it focuses on reduction
of maternal mortality as the quality index around which health services are
rationalized. 32 blocks each has been taken up in the first two years and the entire
state is planned to be covered in another 3 years. So as to address the specialist
gaps, an innovative training programme for multiskilling doctors, particularly in
EmOC and Anaesthesia, has been designed which has been replicated nationally
now. These trainings are conducted in 3 top medical institutions of the state and so
far 96 MBBS doctors has been built capacities to impart EmOC services as well as
anaesthesia. A training on essential neonatal care and some other disciplines are
also started very recently. This way the FRU service provision has been marked a
much better status in the state if compared to past- We would like to note that these
facilities are now becoming available even in some of those facilities situated in
conflict-ridden areas of the state.
Placing Health into Panchayats Agenda- The Swasth Panchayat Scheme : This is a
programme to support local health planning and to enhance PRI role in health. An
indicator based health & human development index has been prepared for all
Panchayats of the state that is hamlet centred so as to capture even the intrapanchayat variations. At present, the HHDI is ready for 9141 Panchayats out of
9820 Panchayats in the state. Hon’ble Chief Minister of the state has declared an
award for two top Panchayats of each block based on this index and also
provisions are made to support weaker Panchayats identified under this process.
The Programme is now in the second year of implementation.
Reaching out to the people in every corner- The Mobile Medical Units : Chhattisgarh is
a tribal state where 44 % of the area is covered with forests. Reaching out to the
far-flung corners of the state for providing health services is major challenge. In
order to overcome this challenge and to provide uninterrupted health services in
tribal blocks, as many as 74 mobile medical units have been operationalised in the
state. They are providing valuable services in the haat bazaars of tribal blocks in
the state.
NRHM PIP 2009-10: Chhattisgarh
Page 18
Other than these major innovations, other milestones achieved by the state can be summarised
as:
Formation of State Health Mission and Driving towards the NRHM Goals: Moving
towards health for the poor, a state health mission has been constituted under
NRHM, Chaired by the Hon. Chief Minister. State, District, and Block programme
Management Units are supporting the mission activities at respective levels.
Decentralised planning and management of resources to address local needs has
become a reality.
Visions and Policies: Taking all stakeholders on board, the State health & Population
policy has been prepared and this shall be notified soon. In addition, Vision-2020
for health sector has been adopted. A new act for regulation of clinical
establishments under private sector is drafted and awaiting approval.
Major Infrastructure Expansion: The state has taken historical initiatives to expand the
health delivery infrastructure in the state. Inadequate infrastructure being a major
gap faced by the department, filling this has been accorded highest priority. The
inadequacy in number of facilities has been met during this period by sanctioning
health facilities: apart from all districts sanctioned of district hospitals, 17 new
Community Health Centres, 200 new Primary Health Centres and 874 new sub
centres has been sanctioned. By this, the state has achieved population norms
except in the case of CHCs. In terms of filling the building gaps, 26 CHCs, 39
PHCs and 201 sub centre buildings are under construction. During the last 3
years, Rs 20 Lakhs per block allocations are made under various schemes for
refurbishment of available buildings in all 146 blocks. The major focus under the
European Union State Partnership is infrastructure development.
Creation of the State Institute of Health & Family Welfare: A Human Resource
Development policy for health has been adopted and SIHFW has been created to
take forward the implementation of this policy. A state of the art building for
SIHFW has been completed and the institution has given adequate manpower and
logistical support in terms of achieving its goals. It is aimed that the capacity and
motivation gaps among the field force be addressed through systematic planning
and implementation of training programmes initiated by SIHFW.
Sanction of staff setup for the health department: Every level of department from
bottom up is provided with adequate manpower provisions under this.
Recruitment of Medical officers through PSC: For the first time after state formation,
449 doctors have been appointed through Public Service Commission, though only
250 of them has joined the services.
Successful Negotiation for European Union Assistance: The state was able to get 174
crores assistance for the health sector improvements in the state.
NRHM PIP 2009-10: Chhattisgarh
Page 19
Raising Medical Education Levels:
In the area of medical education, a promising scene has been created. One more medical
college has been opened in Jagadalpur and another one for the northern part of the state is
under consideration. The existing Medical College of Raipur has been given all necessary
technological inputs as well as institutional support so as to develop it as a state-of the art
medical institute of the area. Rapid allocations and steps have been made for the completion of
the new building for Dental College. An attractive land policy is at the final stage in order to
motivate non-governmental players to start new medical/nursing colleges and super speciality
clinics. A Medical University to lead entire medical education arena within the state was also
realised this year.
Mainstreaming of Indian Systems of Medicine:
The Indian Systems of Medicine has been given top priority by the state. Initially the Raipur
Ayurveda College was declared as a model Ayurvedic College with maximum funding and
logistic support ended up ultimately as an Ayurvedic University. Pharmacy as well as drug
testing facility for Ayurveda is available in quite a few states of the country as on now, and
Chhattisgarh is one among them. Panchakarma therapy centres and speciality clinics have
been started in a number of Allopathic health facilities so as to provide choice for the
community. As many as 86 Primary Health Centres and Ayurvedic Dispensaries have been
merged. All 60000 Mitanins are being trained on household herbal remedies. “AyurvedGram"
concept has been developed to popularise Ayurveda based lifestyle practices.
Control of Food & Drugs:
Achievements are many in the area of Food and Drugs Control also. A state of the art Drug
Testing Laboratory is waiting inauguration at the heart of Raipur city where it was necessary
to sent food/drug samples to external laboratories for getting the sample tests done. In addition
to this, mobile laboratories have been made operational in order to make collecting samples
from remote and village areas possible. Smoking and tobacco use has been banned in public
places.
Table 1.7: Comparative chart on health-showing growth on various interventional areas
Area
Status 2003
Status 2008
Purpose/Achievements
Policies and Programmes
Health and Population Policy Nil
Finalised, awaiting Policy Governance
approval
HRD Policy
Nil
Notified
Drug policy
Nil
Finalised, awaiting Towards rational drug use
approval
NRHM PIP 2009-10: Chhattisgarh
Planned HR Development
Page 20
Policy
for
Medically Nil
Underserved Areas
Under Preparation Reaching the unreached
Delegation
and Upto
decentralisation of powers
District
Upto Block
Grassroots governance
Mainstreaming of AYUSH
Not done
Achieved
Holistic approach
Yaws Control (No. of cases)
15
0
Towards Elimination
Polio Control (No. of cases)
2
0
Towards elimination
Leprosy Control (Prevalence 7.2
Rate)
1.99
72.36 % reduction
TB
Control
Covered)
16
100 % coverage
60092
100 % coverage of rural
areas
(District 4
Mitanin Programme (No. of Nil
Mitanins)
Medical Facilities in public sector
No. of Medical Colleges
2
3
1
No. of District Hospitals
9
15
6
No. of 100 bedded Civil 8
Hospitals
16
8
No. of Community Health 114
Centres
129
15
No. of Functional
Referral Units
First 0
64
64
Health 512
727
215
4728
910
No. of Posts sanctioned of 1455
medical officers
1737
282
No. of Posts sanctioned of 247
Specialists
637
390
No. Doctors promoted as 0
250
250
No. of
Centres
Primary
No. of Primary Health Sub 3818
centres
Manpower
NRHM PIP 2009-10: Chhattisgarh
Page 21
specialists
Doctors sanctioned for a 1
PHC
2
2 times
Doctors sanctioned for CHC
8
2 times
448
448
4
Selection of Doctors through 0
PSC
Completion of Buildings
New District hospital
0
6
6
New CHCs
0
36
36
New PHCs
0
73
73
New Sub centres
0
203
203
Budget outlay for Health 235.23
Department
crores
485.7 crores
Almost 2 times
Assistance Under Sanjeevani 2.49 crores
Kosh
13.29 crores
Almost 5 times
Assistance Less than 50 More than
crores
crores
300 Almost 3 times
Fund Allocations
External
Mobilised
Inpatient dietary allocations 8.00 Rs
per head
16.00 Rs
2 times hike
Additional Untied Funds per 0
District Hospital pa
5.0 Lakhs
5.0 Lakhs for 16 facilities
Additional Untied Funds per 0
CHC pa
2.0 Lakhs
2.0 Lakhs
facilities
for
117
Additional Untied Funds per 0
PHC pa
0.5 Lakhs
0.5 Lakhs
facilities
for
517
Additional Untied funds per 0
Sub centre
0.18 Lakhs
0.18 Lakhs
facilities
for
4692
NRHM PIP 2009-10: Chhattisgarh
Page 22
Situational Analysis:
The state's current demographic and health profile is given in the table below against the
status of prior years:
Table 1.8: Demographic profile -State versus India
Indicator
India
Chhattisgarh
2000
2008
2000
2008
Population in million
1027**
10286.1
20.79**
208.333
Population Share (%)
100
NA
2.02**
NA
Population Density
324
312
154**
154
Female Literacy Rate 2001 (%)
54.28**
52.4**
Rise in Female Literacy Rate since 1991 (% 15**
points)
Sex Ratio
24.88**
933**
Tribal Population (%) (SC + ST population. NA
given in brackets (%)
933
990**
989
NA
43%**
43.4
Table 1.9: Health profile of State
Indicators
India
Chhattisgarh
2000
2005
2008
2000
2005
2008
*IMR Total
68
58
55
79
63
59
*IMR Rural
74
64
61
95
65
61
*IMR Urban
44
40
37
49
52
49
*Birth Rate Total
25.8
23.8
23.1
26.7
27.2
26.5
*Birth Rate Rural
27.6
25.6
24.7
29.2
29.0
28.0
*Birth Rate Urban
20.7
19.1
18.6
22.8
20.0
19.9
*Death Rate Total
8.5
7.6
7.4
9.6
8.1
8.5
*Death Rate Rural
9.3
8.1
8.0
11.2
8.4
8.5
*Death Rate Urban
6.3
6.0
6.0
7.1
6.9
6.5
*Natural Growth rate- total
17.3
16.3
15.7
17.1
19.1
18.4
NRHM PIP 2009-10: Chhattisgarh
Page 23
*Natural growth rate- rural
18.3
17.5
16.8
18.1
20.6
19.5
*Natural growth rate- urban
14.4
13.1
12.7
15.7
13.1
13.1
Note: * SRS data (Report Oct – 2008), ** Census data
Data over the last five years. These cover the basic health indicator along with key social
determinants like malnutrition, Literacy and population dynamics in the state. A brief analysis
of these is presented below, with a comparison of the change that has taken place year by year
at locally and nationally. This comparison will show that, despite of the numerous limitations,
Chhattisgarh is continually recording considerable positive growth in the field of Health and
development, but still its long to reach parity to the level where the nation stands or some of
the better performing states stand.
Table 1.10: Progress of Chhattisgarh in terms of selected vital health indicators
Positive Indicators
Chhattisgarh
DLHS 2* DLHS 3**
Change
Proportion (%) of mothers who had at least 3 ante- 44.4
natal care visits for their last birth
51.2
6.8
Institutional Delivery
18.1
18.1
00
Proportion (%) of births assisted by health personnel
11.1
14.1
3.0
Proportion (%) of children below 3 years who were 29.5
breastfed within an hour of birth
50.1
20.6
Proportion(%) of children below one year who are
breastfed within 24 hours of birth*
Proportion (%) of children who are exclusively NA
breastfed for 5 months
78.3
Proportion (%) of children 12-23 months fully 56.9
immunized
59.6
2.7
Proportion (%) of children 12-23 months who have 66.7
received measles immunization
69.7
3.0
Proportion (%) of children 12-23 months vitamin A in 32.4
last 6 months
65.1
32.7
Proportion (%) of children with diarrhoea in last 2 41.7
weeks who received ORS
36.6
-5.1
Proportion (%) of children with ARI in last 2 weeks 63.3
who were seen by an health facility
68.1
4.8
Source*- DLHS 2, ** DLHS 3
NRHM PIP 2009-10: Chhattisgarh
Page 24
Looking for indicators of community level action, we find few indicators are not dependent on
supply side action. Of these breastfeeding in the first hour, which theoretically can lead by
itself to a decrease of 13% in infant mortality (Reference), is one of the most sensitive and
exclusive breast-feeding is another. ORS use in diarrhoea is a third. Breastfeeding initiation is
dramatically improved as per UNICEF evaluation– to 87.3% mothers feeding the colostrums,
50.1 % children breastfed in the first one hour (DLHS 3). That would mean that most mothers
in Chhattisgarh breast-feed within the first few hours – but not necessarily in the first hour.
One of the major thrust in the Mitanin Programme after the neonatal and child survival
training is to improve this further.
In exclusive breast feeding the figure is 78.3 by NFHS 3. However, in ORS usage the figure
decreased 41.7 in NFHS 2 to 36.6 in DLHS 3. The improvement in institutional delivery has
also been tremendous. Part of it could be attributed to JSY, but a major credit shall also go to
the community mobilisation and education, where demand for the entitled services could be
generated well.
One more fact the state has taken into account is about the trends in IMR. There was a 4-point
increase in rural IMR from 2004 to 2005. But now in 2008, the IMR has dropped down by 3
points (from 58 to 55, SRS data), which indicates that various programmes through community
intervention, with institutional support, are showing an ongoing positive trend.
Programme Experience:
Addressing Gaps in Infrastructure – Sanction of Facilities against Norms:
There has been a creation of 876 new sub-centres, 200 new PHCs, and 16 CHCs in this period.
This has brought up the creation of public health facilities to what has been stated as required
as per national norms. Currently, the state has 4758 sanctioned sub centres and 721 PHCs,
which meets the current national norms. In the case of CHCs, we have 137 and meeting almost
one CHC per block- though, it needs more CHCs to meet the national norms. On the other
hand, the requirement of district hospitals has been met except for 4 districts where the existing
district hospitals have been upgraded as hospitals under teaching institutions.
Creation of Buildings:
There has been acceleration in creation of buildings also. Taking funds from various sources –
47 CHC buildings have been built to norms and funds are available for another 82 buildings
(from SIP, state funds, and NRHM). At least we can reach the minimum infrastructure needed
for the creation of functional FRUs immediately for these CHCs, though it may take some more
time to meet IPHS norms in all. The enormous gap in sub centre buildings of over 2800 sub
centres has also been reduced to 1932 by this year through pooling funds from various sources.
Given the fact that we are to move towards two ANM sub-centres and institutional delivery at
every sub-centre, this still continues as a challenge. In PHCs, also, there is a substantial gap of
382 that need to be built- this includes the newly sanctioned ones. Other than health facilities,
we need a district training centre in 12 districts and an office for the chief medical officer and
district health society in 14. (the current data needs to be collected for the district action plan)
NRHM PIP 2009-10: Chhattisgarh
Page 25
To address human resource gap in future state has plan to start 15 New Nursing College
attached with District Hospital which will produce Total 750 student / Yr. Along with this 10
ANM school attached with District hospital and Vocation training 10 + 2 and ANM dual
certificate course will start soon . More than 50 percent of the assistance availed under EUState Partnership Programme has been allocated for addressing infrastructure gaps which
shall be used in tribal and sc dominant areas. For rest of the areas, further possibilities needs
to be explored.
Facility
Year 2002-03
Sanctioned
with own buildings
Sanctioned
With own buildings
Sanctioned
With own buildings
Sanctioned
With own buildings /
under construction
Actual Gaps
Sanctioned
Table 1.11: Current Infrastructure Situation:
Sub
centres
3818
1458
3818
1458
4692
1853
4694
3983
711
4728
PHC
513
327
516
327
717
400
707
465
242
721
CHC
114
34
116
34
133
70
136
100
37
137
00
17
Civil
Hospital
Year
04
2003- Year 2006-07
17
17
Year 2007-08
17
Year
200809
District
Hospital
6
6
15
9
16
13
18
17
1
17
Medical
College
01
01
01
01
01
01
03
03
00
03
Dental
College
--
--
01
01
01
01
01
01
00
01
Human Resource Situation:
The state has shown considerable growth in filling the human resource gap as well. The new
staff setup has been sanctioned to match the requirement of new situation and permissions have
been given to fill the gaps. The crunch on this as on today has been to get adequate number of
doctors and paramedics. Timely promotion of various cadres of staff like from medical officers
to specialists to administrative cadre as well as of paramedical staff and other workers to next
level of seniority continued to be a problem and this has been given sufficient attention very
NRHM PIP 2009-10: Chhattisgarh
Page 26
recently. Almost all due promotions except that of the top order has been completed- 161
ANMs to LHVs, 354 MPW (m) to Supervisors, 16 Nursing sisters to matrons, 250 MOs to
Specialists, 15 Senior Medial Officer/Specialists to DHOs, 8 DHOs to CMHOs. Similarly, posts
of 1200 doctors, 162 staff nurses, 150 radiographers, have been advertised very recently. This
way, the workforce situation indicates a growth, though still there are major gaps to fill. The
numerical situation on this is as following:
Table 1.12: Workforce status
Post
Sanctioned Regular
Existing Staff
Vacant Contractual Total
Staff/ Ad hoc Existing
Vacant
Posts
Director
3
0
3
1
1
3
Joint
Director
6
3
3
0
3 (only two 3
working,
as one is
DHS i/c)
Joint
Director
Finance
1
1
0
0
0
Deputy
Director
9
0
9
12 (Ad hoc 12
from regular
Staff)
-3
CMHO
16
5
11
11
16
0
DHO
16
16
0
0
16
0
BMO
146
0
146
129
129
17
Medical
officer
2147
1109
1038
369
1407
Specialist
701
248
453
-----
-----
453
Staff Nurse
935
866
69
00
866
-8
ANM
5653
4984
495
156
5140
770
MPW (m)
4784
2514
2270
0
2514
2270
Radiographer 153
99
54
00
99
Lab
Technician
357
374
00
357
0
(MBBS
+AYUSH)
731
NRHM PIP 2009-10: Chhattisgarh
Page 27
Ophthalmic
Assistants
620
167
453
00
167
Pharmacist
(Grade 2)
974
614
360
00
614
Dresser
936
630
306
00
630
Male
supervisor
872
722
150
00
722
Nursing
Sister
185
39
146
00
39
L.H.V.
1034
749
285
00
749
H.A
398
225
176
00
225
Table 1.13: Progress on training and skill development front
S.
No
Type of Training Year 2003-04
institution
Government
Year 2008-09
Private
Total
Government
Private
Total
1.
State Health and 0
Family
Welfare
Training Centre
0
0
1
0
1
2.
B.
Sc.
College
Nursing 1
0
1
1
25
26
3.
General
Nursing 2
Training Centre
4
6
4
4
8
4.
M.P.W ( Female )
7
1
8
10
1
11
5.
M.P.W ( Male)
3
0
3
5
2
7
The major problem faced by the state was lack of an adequate state level facility for conducting
the state level trainings to prepare the trainers team. Looking at this, a Human Resource
Policy was adopted and The SIHFW was conceptualised. Though the SIHFW got constructed
and inaugurated with state of the art facilities, lack of training faculty and experts continues to
be the major role limiting factor and this has affected the capacity building initiatives at the
state level. Many of the training initiatives that were planned in last year could not be initiated
in want of this. However, necessary steps are being initiated to overcome these problems.
The training materials needed for multi-skilling medical and paramedical staff got prepared.
So far, about 95 doctors each have completed the training on multi-skilling for EmOC and
NRHM PIP 2009-10: Chhattisgarh
Page 28
anaesthesia and the course has been further expanded adding other specialities needed for the
FRU functions. The material for nationally guided training programmes is also in place. An
evaluation of anaesthesia short-term course was conducted by Government of India, which has
pointed out a number of shortcomings in the course management- that are being addressed one
by one.
For IMNCI training, the state level resource persons are trained under the UNICEF
coordinated national level training programme but the next level of trainings could not be
initiated except in the case of Rajnandgaon district. The paediatrics faculty from the Raipur
medical college also was trained on IMNCI. To monitor the ongoing training activities,
technical consultants are being posted at SIHFW.
For Adolescent Health, ARSH training is yet to be initiated. Pilot activity is being initiated in 2
districts on this as well as in ARSH clinics.
On training of ASHA under NRHM, more than 58000 Mitanins have completed initial 10th
rounds of trainings and the training rounds 11, 12, to be started.
At Panchayat level, training on Health & Human Development Index has been revised and
further training of Panchayat functionaries and community conducted. A detailed guideline on
VHSC functions prepared and the training is ready to be rolled across the state, in year 200809 totals 18322 VHSC formed against and 15326 VHSC A/C opened against the target of
20639, out of that for 14236 funds has been released.
Towards facility development, orientation on assessment of facility performance has been given
under Jeevandeep Scheme. The gap on how to formulate facility development plan, how to
coordinate with Jeevan Deep Samitis on improving the infrastructure and service quality has
slowly been addressed. In the year of 2008-09 out of 894-facility total, 861 Jeevan Deep
Samitis formed and money has been released to all the newly formed Jeevan deep Samitis.
ISO certification of Korba hospital. The Korba District hospital is the first ever in India to be
accredited with ISO certification.
Operationalisation of FRUs & improving institutional delivery situation:
With a goal adopted on becoming a site of 24-hour institutional delivery/basic emergency care
and skilled birth assistance and manpower planning being implemented, 76 out of a planned
96 PHCs have started to function providing 24 institutional delivery and basic emergency
obstetric care. Further, almost all 129 CHCs have become functional as 24-hour sites for Basic
emergency obstetric care and for Institutional deliveries.
Still, we realise that the achievements in institutional delivery needs improvement particularly
when schemes like Janani Suraksha Yojana are operational. Newly upgraded facilities are yet
to reach the desired level of performance on this and more than half of CHCs also have to
improve on this. At the PHCs also, though we have succeeded them to initiate institutional
deliveries, there is a major need of improving their achievement levels. As far as Sub-Centres
are concerned, at present only one fourth( DLHS ) of them have adequate space for
institutional delivery and even in these achieving institutional delivery has been difficult due to
NRHM PIP 2009-10: Chhattisgarh
Page 29
inability to make referral arrangements. One of the major achievements, job description of
ANM has been prepared for the level of Sub Centre and PHC, daft has been send for final
approval. This year we are planning to achieve this by adopting one ANM per panchayat
strategy: being the state have almost 2 times of panchayats in number, if compared to Sub
centres.
The long-term goal regarding CHCs is to reach IPHS standards – incorporating both the
concept of FRU and CEmONC centres. Of this, we began work on 32 centres to be developed
as FRUs and of these, 21 centres have now initiated Emergency Obstetric Care services and 28
have initiated basic emergency obstetric care services. Due to various reasons, we are still not
able to expand this number- alternative approaches are being planned this year as part of
Jeevandeep facility development plans with focus to FRU designated facilities. In another set of
32 CHCs which was taken under phase 2 FRU development during last year, doctors have
completed short term specialist skill training in select institutes for Emergency Obstetric Care
and anaesthesia. New batch nomination has been invited form block level to start next multi
skilling batch.
Pt
JNM
Medical
College,
Raipur
Chhattisgarh
Institute of
Medical
Sciences,
Bilaspur
JLN
Hospital and
Research
Centre,
Bhilai
Total
No.
Trained
Table 1.14: Status of multi-skill training
EmOC
LSAS
EmOC
LSAS
EmOC
LSAS
EmOC
LSAS
Phase I 4
Batch I
5
5
5
4
5
13
15
28
Phase II 2
Batch II
6
6
3
4
4
12
13
25
Total
11
11
8
8
9
25
28
53
Phase II 2
Batch I
3
6
3
4
3
12
9
21
Phase II 1
Batch II
4
3
5
5
3
9
11
20
Total
3
7
9
8
9
6
21
20
41
Grand
Total
9
18
20
16
17
15
46
49
95
Batch
6
Grand
Total
The evaluation conducted by Government of India has recommended a number of measures to
improve the multi-skill training in Anaesthesia. From this year, the EmOC training shall be
held by FOGSI in designated training institutes. The MOU has been signed and the first phase
of instalment has been already transferred to GOGSI.
NRHM PIP 2009-10: Chhattisgarh
Page 30
So far, the FRU operationalisation is concerned, measures are being taken to post those
trained doctors to FRUs back. The recent GTZ survey report also points towards a number of
measures to be adopted towards materialising the functional FRU. We are taking this as the
key task of coming year.
Medically Underserved Areas:
Chhattisgarh is a state with high forest cover and many of these areas are conflict-affected,
underserved areas are high where doctors are not available to work and lack of adequacy in
other staff also. Currently the major strategy that is able to contribute towards outreach in
these areas is the Mobile Medical Units, where 74 MMUs are operational.
A package for medically underserved areas with special incentives and promotional support
for doctors is drafted and a pilot proposal on this is this is submitted for approval as part of
this PIP. This comprises a block headquarter based health department colony, transport
facilities to peripheries, insurance schemes and family support for education etc. In addition to
this, a special strategy for areas in conflict situation is also envisaged, as many areas within
Dantewada and similar districts are facing such a situation. Filling medical officer gaps by
placing Ayurvedic doctors has been adopted as a strategy in these areas and a special training
package is being developed for these doctors so that they can handle almost all those cases that
an MBBS doctor can manage at the PHC level (Total no of Ayurvedic doctor in PHC level). An
additional compensation package is being approved for these doctors. We are also planning to
deploy the diploma holders in modern and holistic medicine trained in the state as part of a 3year medical course in rural PHCs this year (Total no of 3-year medical course appointed and
process) .
Another major intervention planned this year for the difficult area is the Rural Medical Corpsthis envisages a number of initiatives to the doctors and other health staff a number of benefits
over and above the salary, including a health worker’s colony, insurance support and study
support for kin. Similarly, we are proposing to post the 3-year medical diploma holders in
rural PHCs with a special incentive for difficult areas. Similarly, we are proposing more staff
nurse positions on contract in order to operationalise the 24 x 7 PHCs and CHCs with focus to
difficult areas total no of 3-year medical diploma holder in system).
Behaviour Change Communication:
A well-planned IEC/BCC strategy and implementation framework is in place and District Level
IEC plans have been made. This year our focus was to make programmes based on this. The
basic constraint here was to reinforce the need to understand the importance of IEC/BCC
planning for locale specific and outcome based BCC programmes. The state lacks a rigorous
planning unit that conceptualises and strategizes the programmes and an implementing team
that realises these programmes to the expected levels. We are planning for adding this as part
of this PIP.
Currently, the key strategy adopted by the state is folk art based on Kalajathas, wall writings,
printed posters and handouts, TV/Radio interventions etc- In HIV-AIDS control, some
innovative strategies were adopted. It has been found that the current state level centralisation
NRHM PIP 2009-10: Chhattisgarh
Page 31
of this needs to be shifted to local level strategies, for which a policy has been formulated. This
year, we are also planning to have specific focus on IEC areas for each month.
A BCC kit was developed for the Mitanins during the current year, which is shall act as an
interventional tool for raising the right demands at right platforms as well as to improve
community roles in health.
Community Level Care: The Mitanin Programme:
The Mitanin Programme continues to give very good demand side inputs for health services. In
this year total 46149Mitanin has been trained in for Neonatal and child survival for 5 days
(10th round training), 59489 Mitanin trained for 3 days training.
Table 1.15: Mitanins and their training status
District
Trained
Mitanins
Essential
Neonatal
Care given
on
First
Day
Essential
intervention
for
prevention/cure of
common
Childhood diseases
Support
during
immunization
day
Percentage
of
active
mitanins
Dantewada
3414
2630
2695
2499
76.4
Bastar
5167
4760
4954
4562
92.1
Kanker
2776
2397
2520
2398
87.8
Dhamtari
1627
1354
1439
1492
87.8
Mahasamund 2007
1883
1995
1995
97.5
Raipur
6691
5705
6207
5928
88.9
Durg
5062
4240
4586
4671
88.9
Rajnandgaon
3740
2215
3223
2848
73.9
Kawardha
1633
1274
1447
1351
83.1
Bilaspur
4204
3804
3721
2327
78.1
Janjgir/
Champa
3586
2629
3381
3163
85.3
Korba
2274
750
2267
1980
73.2
Raigarh
3731
3277
3270
3307
88.0
Jashpur
3185
2361
2920
2305
79.4
Sarguja
8259
4978
6839
5730
70.8
NRHM PIP 2009-10: Chhattisgarh
Page 32
Koriya
2133
1892
2090
2030
94.0
Total
59489
46149
53554
48586
83.1
Key weakness under the programme is continuing to be the weaker referral response at the
health facilities. This is being addressed through an intervention called Mitanin Helpdesk.
Currently all the 136 CHC, and district hospital have Mitanin help desk to provide support and
to facilitate CSY. (Total no of Mitanin help desk). Lesser technical understanding at the
Mitanin level was another problem, which is improving after the rigorous training under
Neonatal and Child Survival training based on audio-visuals, video and patient reviews, based
on IMNCI and HBNC principles. Mitanin-Anganwadi convergence has improved and this has
been envisaged to be further improved through the BCC kit intervention, which is common for
AWW and Mitanins. The role being played by the Mitanins and the programme team in the
SWASTH Panchayat index generation and planning has also been remarkable and they are
expected to anchor the social mobilisation initiatives under the Village Health & Sanitation
Committee initiatives.
Provision of Quality Services and Better Management of facilities:
Jeevan Deep Hospital Development Programme, run by the state as improved Rogi Kalyan
Samitis, got inbuilt components for assessment and grading of facility performance and quality,
annual plans for betterment of the facility using available funds and special grants,
Accreditation standards that lead towards a roadmap to IPHS, and Award/Reward schemes.
The scheme was launched in 2005-06 and the interventions at district levels are showing good
trends and block level interventions were initiated very recently. At the district level, 3 of the
hospitals were accredited as Jeevandeep Golden Star Hospital and 2 of them were accredited
as Bronze star hospitals.( Korba hospital ISO Certification ) We could organise a national
level award giving ceremony for this in order to boost the motivation of good performers. The
district level quality assessment that was taken place as part of the Jeevan Deep Scheme was
an eye opener for many of the hospitals and it gave them an insight of how to look at solutions
side for many of the critical gaps. With this scheme and other inputs through various
programmes, the facility level outputs are expected to be improved. Currently we are getting
ready for second year evaluation of district hospitals and moving towards the completion of the
first year evaluation of CHCs. So far, we are not able to organise adequate technical support
for facilities below district levels, which shall be addressed this year. In addition, we are
planning
Baal Hruday Suraksha Yojana:
1. Started on 15th July 2008
2. Institution involved – Apollo S.R. Hospital, Bhilai, Ram Krishna Care Hospital, Raipur,
Escort Heart Centre, Raipur , Apollo Hospital , Bilaspur ,
3. Total payment: Rs. 57, 11,920 only.
Table 1.16: Achievements under Baal Hruday Suraksha Yojana
NRHM PIP 2009-10: Chhattisgarh
Page 33
Total registration
Referred case
Total No of patient treated
445
310
85
PRI Involvement in Health:
In 2005-06, a specific programme to improve panchayat role in health was initiated by the
state under RCH/NRHM called the Swasth Panchayat Scheme. This derived an indicator based
status presentation of each and every panchayat on health using a unique tool called
Panchayat Health & human Development Index followed by planning by Panchayats to
overcome the issues identified as part of the indexing. In 2006, this process was initiated in
more than 90% of the Panchayats of the state. One more important feature of this initiative is
that there is an award for best Panchayats as well as a special focus planned on weaker
Panchayats in a block, which has already been operationalised. Another benefit is that the
intra-panchayat and inter-Panchayat variations could be assessed as part of this so that each
Panchayats can have sufficient insights on various health issues in terms of improving them.
The programme has now entered into rigorous planning phase in all Panchayats, expecting
formulation of actionable village health plan at all panchayat level. The introduction of Village
Health & Sanitation Committees this year has strengthened this further- we have achieved
almost 100% in formation of the VHSCs- a detailed operational guideline was prepared and
disseminated on this, which is widely appreciated. Our focus is to orient the VHSCs through a
massive campaign and to ensure micro health planning, which is going to materialise very
soon. In 2007-08, we have completed the second round of massive data collection on hamlet
based HHDI and better performing Panchayats on Health in 132 out of 146 has been identified
and awarded. The weaker Panchayats in all these blocks were identified as well. Overall, the
programme has touched 9300-gram panchayats HHDI assessment. Prior to this, a major
mobilisation campaign was conducted to orient the panchayat heads and a hand book on
health related development programmes in the form of panchayat diary was provided to them
with Unicef support. Around 20000 PRI functionaries were sensitised under this. Panchayat
Health Planning was initiated in about 1000 Panchayats so far and more than 300 plans have
been finalised from them. Many of the panchayats are allocating their own resources for health
amenities and interventions, is a very good indicator of impact of this initiative. Still, we note
that the data quality in HHDI survey was not upto mark in some of the HHDI parameters- we
are attributing this to lack of proper orientation due to the massive character of this community
based data collection.
Urban health systems:
The state has four major cities with more than a laky population amongst which, Raipur, Durg,
Bilaspur and Korba are the highly populated and growing. The growth of these cities is
tremendous after Chhattisgarh has become a state. Migration to these cities from village sides
is high, and development of these cities is leaving behind a large number of new health
challenges to be handled. The populations here are largely served by private providers. The
growth of urban slums is the most challenging feature in terms of health services provision
where affordability levels are very low and public systems are must. The strategies planned to
address this were to set up urban health centres per thousand populations for the poor
NRHM PIP 2009-10: Chhattisgarh
Page 34
population particularly leaving in the slums, peer education programme for the urban
vulnerable and community health workers per thousand populations. The implementation of
these strategies is at the very early stage and this needs to be strengthened.
Last year, 2 of the districts have completed the urban mapping and in one district, selection of
Mitanins for the slum areas is complete in Durg district. Lack of proper guidelines and
operational manuals, the districts are facing some problem in taking this programme forward.
Lack of proper health systems in these area and improper coordination with urban local bodies
are some of the other role limiting factors. However, this year we are going to focus on this
system related issues. The introduction of Urban Health Mission shall further enhance this.
One of the prime agenda for SHRC in the coming year will be to scale up the urban community
interventions for health.
Programmatic and Financial Management Issues:
Management of programmes under NRHM – both programmatic and financial - has improved
largely during these three years but it still has major room to improve. The financial flow from
state to district and peripheries has tremendously improved in this period after the adoption of
electronic transfer mechanisms. Coordination between state and district structures has made
perfective, reporting mechanisms were streamlined, training on financial management was
successfully organised, guidelines on financial management was properly disseminated and
followed, the lacunae as pointed out in past reviews were resolved one by one- these are the
overall achievements of the year. Nevertheless, some of the problems like that of qualified
manpower for these purposes at the state and district levels still exist. Lack of fully manned and
functional PMUs is a major problem faced by many of the districts even now- the filling of
vacancies could not be done so far- decision to fill these vacancies are taken and this is going
for selection procedures very soon. The Block PMU has been decided to be set up but the
selection procedures yet need to be initiated. The HR situation within the PMUs is an area
identified for further interventions this year (appointment of DADA, BADA, and DDA).
Stability within the PMU structures at both state and district levels changed in those units
where the PMU members are either trying for, or had higher career opportunities. In case
these positions become vacant, a temporary instability in those units would need timely
attention. The role clarity at the state and district level structures continues as another area
with major scope of improvement, where some of the confusions still need to be resolved. So
far, the meetings of the state health society and mission are concerned, we could do one
meeting so far of the Society General Body, but meeting of the mission was called twice but this
is yet to be materialised. Functioning of Health Directorates and Mission Directorate also
were being strengthened in parallel, but this is also at a stage where further focus is needed.
In a recent national level review, it has been found that the organisational aspects of the state
PMU needs to be further improved and the state is initiating adequate measures to overcome
this. The state programme management unit is limited to the three staff hired centrally and
placed here where the state accounts manager position was recently filled and the rest of the
expansion under the NRHM secretariat is yet to happen. In order to address the gaps in human
resource management, this year we are planning to appoint an HR agency to look after these
issues timely. This would be attained through NHSRC support.
Table 1.17: Workforce situation of programme management units
NRHM PIP 2009-10: Chhattisgarh
Page 35
S.
no
Position
Sanctioned
Filled*
Gaps Remark
1
State Programme Manager
1
1
0
2
State Finance Manager
1
1
0
3
State Accounts Manager
1
1
0
4
IEC Consultant
1
1
0
5
State
Consultant
Procurement expert
1
0
1
To be re-advertised.
6
State
Consultant
Demography expert
1
0
1
To be advertise
7
State consultant
expert
1
1
0
Selection & appointment
process done.
8
State HMIS Consultant
1
1
0
-do-
9
State
ConsultantMonitoring/Evaluation
1
0
1
-To be re-advertise
10
DPMs
16
15
1
Selection for vacant posts
completed.
11
DAM
16
10
6
Selection for vacant posts
completed.
12
Data Assistant
16
8
8
Selection for vacant posts
completed
13
BPM
146
0
146
Selection for vacant posts
completed
14
BADA
146
0
146
Selection for vacant posts
completed
Training
Note: *Position filled up to November 2008
Technical Assistance:
The State Health Resource Centre (SHRC) is the key agency to provide technical assistance in
the state, which plays a key role in design, planning and functional support to the state health
mission and society, other than UNICEF. The Regional Resource Centre for RCH, the
Micronutrient Initiative and CINI, CARE are also providing some assistance in select areas
where their programmes are concerned. Another technical support envisaged was for the EU
partnership but this has not yet been materialised. In addition, in the area of training and BCC,
the SIHFW is being built up and this is not fully functional as the faculty appointment is not
complete yet.
NRHM PIP 2009-10: Chhattisgarh
Page 36
The key technical inputs to the NRHM come from the State Health Resource Centre. An
autonomous body especially set up for health sector reforms in the state, the SHRC got a team
of experts in almost all walks of Public Health. They give implementation support too, for all
the community based health programmes like the Mitanin Programme, the Swasth Panchayat
initiatives, Village Health & Sanitation Committee operationalisation, The Jeevan Deep
Hospital Reforms programme etc. They do play coordinating role in the capacity building
initiatives like the multiskilling training of medical officers for FRU operationalisation,
professionalization of health management through PHRN fast-track training programme etc.
SHRC act as the coordinating unit for design & planning of NRHM initiatives, supported by
other technical agencies. Apart from NRHM planning, it plays critical role in the ongoing
European Union State Partnership Programme as well. The convergence initiatives with
Department of Panchayat, Education, ICDS etc are also been coordinated by SHRC. The state
government has requested the SHRC to set up an AYUSH technical wing as well, in order to
push up the mainstreaming of AYUSH systems. Other than this, the SHRC supports the state in
preparation of acts, policies etc related to health like role under their role as additional
technical capacity to the health department- like the Health & Population Policy, Revision of
Essential Drug List, Clinical Establishments Act, Medical University Act, VHSC Guidelines
etc.
Another Technical Assistance agency in the state is UNICEF, with a Major objective of
reduction in infant and maternal deaths. TOTAL BUDGET supported in financial year is 200708: USD 1,057,000 (INR 4, 20, 15,750). Key contribution of UNICEF has been:
Popularization of institutional deliveries to ensure reach at least 50 percent
Roll out of IMNCI throughout the state to ensure recognition and referral of sick
neonates locally supported by Mitanin.
Facilitate the Creation of sick newborn care units at district hospitals.
Promotion of Zinc based ORS.
Strengthen health and nutrition days in order to promote full coverage of Immunization.
Major state-specific UNICEF initiatives in Chhattisgarh are:
Facility survey with GIS based mapping of all the Government health facility.
To facilitate JSY help line.
To put up the bottleneck analysis of the state and capacity building on technique useful
for the district health plan.
Support a child survival cell at SIHFW for capacity building and monitoring support.
To support the Mitanin programme in IMNCI based training.
To support IMNCI training programme for Medical Officers.
NRHM PIP 2009-10: Chhattisgarh
Page 37
A touch screen for health awareness ‘Sishu Sanraksak Kiosk’ will be provided to
district hospitals that have Mitanin help desk.
To provide technical support on integrated BCC kit plan, Hepatitis B promotion.
To support the ‘Sishu Sanraksaan Maah’
Neonatal Intensive Care Units (NICUs) will be established in eligible district hospitals.
To promote and distribute the bed nets to pregnant women of the tribal district.
Rajnandgaon will continue to be a focus district for UNICEF and support major health
initiatives.
In Dantewada, ambulances will be procured and supplied for referral to prevent
maternal and child deaths.
Collaboration will be made with professional bodies like IAP, IMA, NNF, and FOGSI
etc to achieve the goals.
Technical Assistance from RRC
Another Technical Assistance agency is Regional Resource Centre run by Population
Foundation of India, where the roles of RRC in the state are as follows: To facilitate for the implementation of RCH-II activities by MNGOs/FNGOs under
NRHM at the unserved and underserved areas.
To act as the technical supporting agency for MNGOs and SNGOs of the state
To build the capacity of MNGOs for the implementation of the activities through
training programmes, seminars, workshops etc.
To facilitate the State and District Health Societies for the implementation of the
MNGO & SNGOs scheme.
To validate and monitor the activities of the MNGOs and SNGOs in cooperation with
the district and state health authorities
To associate with such activities those are aiming for the reduction of IMR and MMR.
To document and facilitate for the replication of best practicing centres in the state and
to record the case studies in the field of RCH.
To assist the state and district health authorities in the implementation of RCH or
related activities under NRHM.
Technical Assistance from Micronutrient Initiative
NRHM PIP 2009-10: Chhattisgarh
Page 38
The Micronutrient Initiative-CINI collaboration gives technical support in biannual vitamin-a
supplementation to be held as a comprehensive child-protection campaign called Sishu
Sanraksaan Maah. They do take up all the activities right from the planning, mobilisation,
training and monitoring of this campaign with UNICEF Support.
Technical Assistance from CARE
Yet another technical input is from CARE, through the child health and nutrition project named
Integrated Nutrition and health program, INHP is in its third phase, and this is the main
project of CARE in the state. As per request of the government of India, this phase of the
project is focused on replication of best practices to non-CARE supported districts and to
phase-out from earlier program Blocks. For last five years, this project was implemented in 10
out of the 16 districts in the state and hence currently being replicated to the six non-CARE
districts. Objectives of this project are to:
- Reduce infant mortality rate and
- Reduce childhood malnutrition.
The main approach is to improve quality of implementation of ICDS and RCH programs, by
building capacities of functionaries of these programs and by enhancing convergence between
the two programs at all levels. Working on the demand generation side, this project also
focuses in capacitating community representatives, (both PRI leaders as well as members of
community based organizations like SHGs, Mahatari Panchayats etc). Key technical
interventions focused are:
- Home based newborn care practices,
- Infant and young child feeding practices and
- Childhood immunization including Vitamin A supplementation
Enhancing capacities of ICDS and RCH functionaries on these technical areas and
emphasizing on home-contacts of Anganwadi Worker to undertake inter-personal
communication, through strengthening ICDS supervisory system are being predominantly
focused. Improving management systems of ICDS at block and district level as well as
promoting convergence with RCH at the block and district level with engagement of district
collectors are being attempted. INHP has a team of 17 program officers and 10 local NGO
partners in the districts and there are ten state based team members for all programs of CARE
in the state. Approximate annual budget for this project in the state is about one million USD.
The new HIV mainstreaming project, in support of NACP III, is being initiated in three districts
of Raipur, Durg and Korba. This project will have a three-member team supported by
management team at the state level. Further details of this project are being worked out
currently. One of the recent efforts is to promote evidence based program planning and
implementation by district RCH societies, as part of which two of the districts were facilitated
to undertake population based survey of critical RCH indicators. This information will be used
for prioritizing focus areas for the district planning process. CARE is also supporting ICDS in
NRHM PIP 2009-10: Chhattisgarh
Page 39
developing of state PIP and district annual plans for World Bank supported ICDS IV project in
nine districts of the state.
Mainstreaming of AYUSH
The National Health Policy (1983) visualized an important role for the AYUSH practitioners in
the delivery of health services. In order to give focused attention to the development and
optimal utilization of this branch of medicine and to ensure that AYUSH practitioners are
brought under the regular health system .This intervention is expected to provide
complementary system of care along with practitioners of modern systems of medicine. This
policy has laid down a set of goals for AYUSH system.
The Government of Chhattisgarh has also given equal status and fairer chance of development
of AYUSH to its full potential in providing health care. Mainstreaming AYUSH institutions and
practitioners with modern systems of medicine in Chhattisgarh has been major priority, so that
people have access to complementary systems of care. Utilizing human resources of AYUSH in
the national health programmes, with the ultimate aim of enhancing the outreach of AYUSH
health care in an accessible, acceptable, affordable, and quality manner is visualized. The
department of AYUSH has reasserted on mainstreaming component with constant efforts and
activities in coordination with modern system of medicine coordination.
Status of AYUSH Institutions in Comparison with Allopathic Set up
The mainstream health provides services at district, block and village level as primary,
secondary and tertiary level of services. The AYUSH health care set up in Chhattisgarh is a
large cadre of health care institutions at primary and tertiary level. The primary institutions of
AYUSH are District Ayurveda Hospitals, which cater OPD, IPD and special health care
services under AYUSH. The services at block level are deficient with no utilization of
manpower at the block levels to provide services and lack of block level coordination and
monitoring.
The department of AYUSH in Chhattisgarh aims at the identification and conservation of rare
and extinct herbs. With the motto of testing the herbs for their potency and toxicity, the
Department of AYUSH has established a Drug testing and Research laboratory in Government
Ayurveda College. So far, 65 drugs are tested for Authenticity.
Table 1.18: comparative AYUSH vs. Allopathic service deliver facilities
Allopathic Health Care Delivery facilities Numbers AYUSH Facilities
Numbers
Medical college hospitals
3
Ayurveda college hospitals
1
District Hospitals
18
District Ayurveda Hospitals
6
CHC
133
Health facility at block level
0
PHC
727
AYUSH Dispensaries
692(Total)
Sub Centre
4692
Ayurveda Dispensaries
634
NRHM PIP 2009-10: Chhattisgarh
Page 40
Homeopathy Dispensaries
52
Unani Dispensaries
6
Drug testing and Research Centre
0
Drug testing and Research Centre 1
Pharmacy
0
Ayurvedic pharmacy
1
The educational institutions under AYUSH in Chhattisgarh are not sufficient to provide
AYUSH education to young aspirants. The AYUSH institutions in Chhattisgarh need to be
increased, So that the State can produce quality professionals to serve in AYUSH heath
services in Chhattisgarh. The Allopathic institutions in the state are three and these are
established in Bilaspur, Raipur and Jagadalpur. The AYUSH educational institutions in
Chhattisgarh are one Ayurveda college in Raipur with the capacity of 55 students and there is
deficiency of Homeopathy, Unani, Naturopathy and Yoga Government educational institutions
in Chhattisgarh.
Table 1.19: comparative AYUSH vs. Allopathic education facilities
Educational
Institutions Nos.
Under Allopathic Health Care Available
Delivery System
Educational
Institutions Nos.
Under AYUSH Health Available
Care Delivery System
Medical college
Ayurveda Medical college
1
Homeopathy college
0
Unani college
0
3
Naturopathy
college
and
Yoga 0
Table 1.20: Status of Ayush Health Care Providers in Chhattisgarh
Deficit
Sanctione
d
In place
Deficit
Sanctione
d
In place
Deficit
Sanctione
d
In place
Deficit
Auxiliary Workers
In place
Swasthya
Sanctione
d
Mahila
Karyakarta
Deficit
Dispensary Attendant
In place
Compounders
Sanctione
d
Doctors
1016
526
490
667
456
211
759
529
230
76
54
22
692
573
119
112
41
71
52
26
26
0
0
0
0
0
0
0
0
0
26
6
20
6
1
5
0
0
0
0
0
0
0
0
0
1154
573
581
725
483
242
759
529
230
76
54
22
692
573
119
AYUSH Interventions under mainstreaming in Chhattisgarh:
Establishment
NRHM PIP 2009-10: Chhattisgarh
Page 41
15 AYUSH wings in District Hospitals,
22 Specialized therapy centre in CHC
24 AYUSH specialty clinics in PHC
357 AYUSH OPD in PHC & 42 AYUSH OPD in CHC
Districts
AYUSH Wings
Functional
Gaps
Specialized
Therapy
Centres/
Speciality
Clinics
Functional
Gaps
Table 1.21: Present status of AYUSH wings, specialized therapy centre and speciality clinic
Kawardha
1
0
1
2
0
2
Janjgir Champa
2
2
0
1
-
1
Koriya
1
0
1
2
0
2
Raipur
1
0
1
2
0
2
Surguja
1
0
1
3
0
3
Korba
1
0
1
1
0
1
Raigarh
1
0
1
2
0
2
Dhamtari
1
0
1
4
0
4
Mahasamund
1
0
1
2
0
2
Durg
1
1
0
2
1
1
Kanker
1
0
1
4
0
4
Jashpur
1
0
1
3
0
3
Rajnandgaon
1
1
0
4
0
4
Bastar
-
-
-
2
2
Dantewada
1
0
1
6
0
6
Bilaspur
-
-
-
6
0
6
Total
15
4
11
46
1
45
At present out of 15 AYUSH wings, only 4 AYUSH wings (1in Durg, 2 in Janjgir and 1 in
Rajnandgaon) are fully operational. Out of 24 specialized therapy centres, only one in Durg is
NRHM PIP 2009-10: Chhattisgarh
Page 42
functional and 22 special clinics established nothing is functional. The major constraint faced
is of less or no space allocation in Allopathic centres.
Co-location of 85 AYUSH dispensaries in PHC\CHC after launching of NRHM
As a primary initiative, 85 centres are collocated in PHC\CHC and in rest 613 centres AYUSH
facilities are planned to be co-located in a systematic manner. Mainstreaming activities in
Chhattisgarh have been initiated from the year2007.Collocation of AYUSH dispensaries in
PHC or CHC building has been undertaken in a planned manner.85 such dispensaries were
selected which were placed near PHC\CHC and efforts were taken for collocation. Where
AYUSH dispensaries were in a good status with best infrastructure the PHC’s were collocated
in AYUSH Dispensaries. Eight dispensaries (Khatti, Pantora, Urba, Nagpur bazaar,
Karpavand, Bainur, Gangalur and Faraspal) were identified in total 85 which had good
infrastructure were PHC was merged.
Table 1.22: Present Status of Co-located Centres:
Districts
Colocated
centres
in CHC
Co-located
Co-located Fully
centres in centres in Function
PHC
Ayush
al
Dispensari
es
Doctors Compound Dispensa
in place ers in place ry
attendant
s
in
place
Raipur
0
7
0
7
6
3
6
Mahasamun
d
0
2
1
2
1
3
2
Korba
1
4
0
3
4
4
5
Dhamtari
0
3
0
3
0
1
1
Bilaspur
5
7
0
3
12
10
8
Janjgir
Champa
1
3
1
3
5
4
4
Rajnandgao
n
0
3
0
1
1
3
2
Kawardha
0
1
0
1
1
1
0
Raigarh
0
3
1
3
4
2
4
Jashpur
0
1
0
1
1
1
1
Surguja
1
22
0
6
23
20
22
Koriya
0
5
1
2
5
6
6
Dantewada
2
0
2
3
4
2
3
Durg
1
10
0
7
11
6
5
NRHM PIP 2009-10: Chhattisgarh
Page 43
Bastar
0
0
2
2
2
2
2
Availability of Medicines in Co-Located Centres
Under NRHM the provision of essential medicine for the collocated centres as Rs 25000/- is
provided to the collocated centres. The other required medicines are fulfilled by the department
of AYUSH as per the demands placed by the Ayurveda medical officers annually.
Constraints Faced:
Space allocated is not sufficient to the standards for collocation in the PHC\CHC.
No space provision for collocation of AYUSH dispensaries in the PHC\CHC as the
existing space in the PHC is less.
No proper space allocation for CSIDC (nodal agency for construction of AYUSH
centres in mainstream health).CSIDC has agreed for new construction of AYUSH
dispensary in the PHC, which is attached to existing building.
Minimum space requirement for development of Ayush wing, speciality centres and
speciality clinic as per the central government guideline as charted out is deficient
in PHC and CHC for starting the AYUSH units in allopathic wings.
Support of AYUSH Medical officers in National Health Programmes
The major input of AYUSH physicians in National Health programmes in Chhattisgarh helps in
implementation of National programmes. The AYUSH physician provides continuous support
to all the programmes run by the Government - encouraging mothers to immunize their child,
formation of malaria slides, counselling and encouraging the couples for family planning. A
target is set for achievement in family planning. Supporting all the other programmes and
active participation of AYUSH physicians is present in Chhattisgarh from the day of its
inception and the activities have been strengthened from the NRHM period by capacity
building of AYUSH physicians in national programmes.
Capacity building as a part of mainstreaming
Training of AYUSH physicians:
The training of Integration of AYUSH physicians in Mainstream Health is initiated, till
now 60 AYUSH physicians have been trained. Another TOT training under NRHM
has been undertaken for Mainstreaming AYUSH in Delhi 3 physicians have been
trained under this programme.
Essential maternal Health and Child survival : As further expansion of service delivery
of AYUSH physicians in national programmes a training programme of AYUSH
physicians has been designed for 2008-09 Maternal and Child health considering
the high Maternal and infant mortality in Chhattisgarh. To monitor this effectively,
the AYUSH directorate and Directorate of Health services are keeping track of this
NRHM PIP 2009-10: Chhattisgarh
Page 44
and monitoring report is brought out regularly. The targets set are all the Medical
officers of Dispensaries and District Ayurveda medical officers.
Training of Mitanin for AYUSH Mainstreaming:
Training of 60,000 Mitanin on AYUSH module “Jadi buti lae kar lae illaj” as a means of
propagation and utilization of Herbal combinations for common ailments by Mitanins.
Proposals Submitted during 2008-09 Under Central Government Scheme:
Development of Drug testing and Research Laboratory: For the infrastructural
development and man power, the Department has proposed a fund of 50 lakhs and the
sanctioned amount is 37.60 lakhs
For the procurement of new machinery for the Ayurvedic Pharmacy which produces
herbal combinations as per the demands of Ayurvedic Dispensaries and District
Ayurveda Hospitals. The amount demanded for this year was 120 lakh and sanctioned
amount is 68.61 sanctioned
Development of Model college: For the development of Government Ayurveda college as
model college with best infrastructure and facilities. No amount was sanctioned for the
same
Table 1.23: Proposal for infrastructure development of AYUSH
Schemes for 2008-09
Proposed
Sanctioned by
Amount For the the Government
Scheme
(in (in lakhs)
lakhs)
Centrally sponsored scheme for development of Drug 50
testing Laboratory
37.6
Centrally sponsored scheme for development of Ayush 300
Institutions
0
Central Scheme for development of Ayurvedic Pharmacy
68.61
Central Scheme for
programmes of AYUSH
CME/ROTp
and
120
Exchange 3.75
3.75
Centrally sponsored scheme for development of Hospitals 1052
and Dispensaries
625.2
Proposal for Essential Drugs under NRHM flexi pool
162.5
162.5
Proposals under NRHM for Mainstreaming Ayush 2008-09
NRHM PIP 2009-10: Chhattisgarh
Page 45
Essential Maternal Health and Child Survival Training of AYUSH Doctors : The AYUSH
Doctors play a critical role in the Delivery of health services .In difficult tribal
areas they have been posted in mainstream health facility wherever facility
Allopathic doctors are not available. Similarly, 85 AYUSH dispensaries are
collocated in mainstream health facilities. Therefore, rigours training of AYUSH
physicians as skilled birth attendants with the management of neonatal and
childhood disorders are essential. The plan for training the AYUSH physicians has
been initiated. With a target of 360 physicians to be trained.
AYURVEDGRAM : Propagation of AYUSH based preventive, promotive and curative
principles in the selected villages by IEC and Health Melas. The health status of
the villages needs to be improved by the AYUSH principles. Conduction of
conceptualization work shop for expert participants. Due to non-availability of
funds, this workshop was not conducted.
AYUSHDEEP SAMITI : Reform based hospital management in the AYUSH health care
facilities. The major objectives of the scheme are facility development as well as
management and untied fund for up gradation of facilities. Dissemination of
guidelines, registration of AYUSHDEEP committee and initial training. Formed
guidelines are disseminated with registration of 12 Districts for AYUSH DEEP
Samiti and others are in progress of registration.
INTEGRATED EPIDEMIC CELL : Disease surveillance and epidemic control strategy is
developed by AYUSH. The epidemic control will be worked out through AYUSH
principles. The process of integrated epidemic cell formation is initiated by
recruitment of Technical consultant.
FORMATION OF MATERNITY AND CHILD WARD IN AYURVEDIC COLLEGE : The special
maternal health and child health training of the existing batch of BAMS students
in order to be professionally skilled. To improve institutional deliveries in Raipur
and managing complicated deliveries the maternal and child ward is initiated. As a
part of this scheme, the Technical consultants of the maternal health and child
health are recruited by the Department with the ongoing process of recruitment of
supporting staff with the fund release of 13.40 lakh.
AYUSH TECHNICAL ASSISTANCE: to improve the AYUSH Medical education, for
improving the planning skills and improving the quality of health care services the
department of AYUSH has placed two technical consultants to provide valuable
inputs in planning and administration.
AYUSH MELAS AT BLOCK AND DISTRICT LEVEL : To popularize and promote the
services under the AYUSH system of medicine and improving the outreach to the
patients. Conduction of melas at blocks quarterly and District biannually was
planned. Due to non-availability of funds, the scheme was not launched as desired.
Other AYUSH interventions under NRHM in Chhattisgarh
NRHM PIP 2009-10: Chhattisgarh
Page 46
Another innovative approach developed by the state is AyurvedGram Yojana, where
one potential panchayat under all the blocks have been adopted to develop public
awareness and action on these issues. At present 121 out of 86 development blocks
have been identified for this programme. This programme is meant to disseminate
promotive, preventive and curative principles of Ayurveda in the villages with the
help of Health Melas and promotive IEC, which will add a remarkable change in
community outreach of AYUSH facilities. As a major initiative 25 villages have
been selected as pilot project for propagation of Ayurvedic health principles in
2007-08.In 2009-10 further same 25 villages with another 50 villages can be
selected for pilot project.
The state medicinal plant board has been constituted functionalized since 2003.
Chhattisgarh has a large diversity of herbal flora, which has made Chhattisgarh
the herbal state. The State medicinal plant board and Directorate AYUSH work in
close coordination for conservation, promotion, collection and production of herbs.
Memorandum of understanding of Department of AYUSH (DTL) with Vanoushadi
board for testing existing Herbal flora is a new initiative under taken by
Department of AYUSH. Under Ayurvedgram Scheme understanding with
Department of Forest for plantation of herbs in the selected villages.
NRHM PIP 2009-10: Chhattisgarh
Page 47
Financial situation, estimated expenses & balance up to march 2008 (in details)
Table 1.24: Financial Status upto March 2008
S.No
1
PARTICULARS
2
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
RCH - Phase - I
i
24HRs delivery Programme
-5.36
3.60
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-5.36
3.60
-1.77
0.00
-1.77
ii
Computer Assistance
0.00
-0.43
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.43
-0.43
0.00
-0.43
iii
Public Private Partnership
0.00
50.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
50.00
50.00
0.00
50.00
iv
Community Incentive
Scheme
0.00
10.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
10.00
10.00
0.00
10.00
v
Contractual Appointments
0.00
398.07
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
398.07
398.07
0.00
398.07
vi
Dai Training
0.67
0.66
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.67
0.66
1.33
0.00
1.33
vii
EAG
1.35
44.40
0.00
0.00
0.00
0.00
0.00
0.00
0.00
1.35
44.40
45.75
0.00
45.75
viii
FRU Civil Works*
-82.47
5.22
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-82.47
5.22
-77.25
0.00
-77.25
ix
FRU
10.04
3.26
0.00
0.00
0.00
0.00
0.00
0.00
0.00
10.04
3.26
13.30
0.00
13.30
x
Cold Chain Handlers
Training
-0.02
0.54
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.02
0.54
0.53
0.00
0.53
NRHM PIP 2009-10: Chhattisgarh
Page 48
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
xi
Cold Chain Maintenance I
-0.80
4.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.80
4.01
3.21
0.00
3.21
xii
Cold Chain Maintenance II
0.25
1.61
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.25
1.61
1.86
0.00
1.86
xiii
Implementation of PNDT
Act
0.04
0.69
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.04
0.69
0.72
0.00
0.72
xiv
Indtra Dhanush III
0.00
0.01
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.01
0.01
0.00
0.01
xv
IST SST Training'
-6.20
0.15
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-6.20
0.15
-6.05
0.00
-6.05
xvi
Laparoscopy Maintenance
0.00
-129.42
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-129.42
-129.42
0.00
-129.42
xvii
Laparoscopy AMRC
0.00
1.86
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
1.86
1.86
0.00
1.86
xviii
Major Civil Works
10.03
9.60
0.00
0.00
0.00
0.00
0.00
0.00
0.00
10.03
9.60
19.63
0.00
19.63
xix
Mobility Support
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
xx
NGO Activities
0.00
60.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
60.00
60.00
0.00
60.00
xxi
NGO Support Activities
0.00
0.05
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.05
0.05
0.00
0.05
xxii
Population Commission
0.00
19.90
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
19.90
19.90
0.00
19.90
xxiii
IEC Activities (RCH- I)
4.35
13.68
0.00
0.00
0.00
0.00
0.00
0.00
0.00
4.35
13.68
18.03
0.00
18.03
NRHM PIP 2009-10: Chhattisgarh
Page 49
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
xxiv
Contractual Salary
(ANM,SN,LT)
0.00
-352.54
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-352.54
-352.54
0.00
-352.54
xxv
Printing of Formats (RCHI)
0.00
-36.53
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-36.53
-36.53
0.00
-36.53
xxvi
Purchase of Inverters
(RCH - I)
0.00
-29.47
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-29.47
-29.47
0.00
-29.47
xxvii
RCH Camp Arrangement
-1.69
4.03
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-1.69
4.03
2.34
0.00
2.34
xxviii
Referral Transport
5.19
21.68
0.00
0.00
0.00
0.00
0.00
0.00
0.00
5.19
21.68
26.87
0.00
26.87
xxix
Repair & Renovation state
office
0.00
5.12
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
5.12
5.12
0.00
5.12
xxx
Review Meeting and
Mobility & Support
0.82
0.37
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.82
0.37
1.19
0.00
1.19
xxxi
Scova Staff
0.00
3.40
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
3.40
3.40
0.00
3.40
xxxii
Training of SST & IST
NIHFW
0.00
0.94
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.94
0.94
0.00
0.94
xxxiii
Refund from District
0.00
168.12
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
168.12
168.12
0.00
168.12
xxxiv
ANM Training
0.03
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.03
0.00
0.03
0.00
0.03
NRHM PIP 2009-10: Chhattisgarh
Page 50
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
xxxv
NSVT Training
0.53
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.53
0.00
0.53
0.00
0.53
xxxvi
Ayurvedic & Homoeopathic
0.00
0.18
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.18
0.18
0.00
0.18
xxxvii
Lok Kala Jatha
-4.10
0.04
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-4.10
0.04
-4.06
0.00
-4.06
xxxviii
ISM & H
0.24
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.24
0.00
0.24
0.00
0.24
xxxix
Swasthya Mela
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
xxxx
Misc. Fund
521.08
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
521.08
0.00
521.08
0.00
521.08
xxxxi
Creda
-0.50
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.50
0.00
-0.50
0.00
-0.50
xxxxii
Vande Matram
-0.03
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.03
0.00
-0.03
0.00
-0.03
xxxxiii
NMBS
6.62
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
6.62
0.00
6.62
0.00
6.62
xxxxiv
Opening Difference
0.04
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.04
0.00
0.04
0.00
0.04
xxxxv
Catup round
-0.95
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-0.95
0.00
-0.95
0.00
-0.95
xxxxvi
Sterilisation Compensation
0.39
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.39
0.00
0.39
0.00
0.39
xxxxvii
M.P. Govt
0.12
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.12
0.00
0.12
0.00
0.12
xxxxviii
Minor Civil Work
0.31
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.31
0.00
0.31
0.00
0.31
NRHM PIP 2009-10: Chhattisgarh
Page 51
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
D.H.S.
S.H.S.
3
4
5
Total RCH - Phase - I
459.98
282.80
PART A - RCH Flexi Pool
0.00
1
MATERNAL HEALTH
0.00
i
Operationalise FRUs
ii
Operationalisation 24 x 7
of 200 New PHC
iii
Operationalise Sub-centres
iv
RCH Camp in Hat Bazaar
(non)
51.76
-42.39
0.00
0.00
0.00
0.00
11.74
0.00
11.74
40.02
-42.39
v
RCH Camp in Hat Bazaar
41.00
-75.67
0.00
0.00
0.00
0.00
0.00
0.00
0.00
41.00
vi
Janani Suraksha Yojana
467.56
-2057.60
0.00
0.00
0.00
1740.00
1282.28
0.00
1282.28
2
CHILD HEALTH
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Care of Sick Children and
Severe Malnutrition
0.00
0.00
0.00
0.00
0.00
0.00
0.09
ii
Facility Based Newborn
Care Unit (SHCU)
0.00
0.00
0.00
0.00
0.00
81.75
0.00
1
2
106.77
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
Closing / Unspent
Balance as on
31.12.08
-200.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
0.00
0.00
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
0.00
0.00
459.98
282.80
742.77
0.00
742.77
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
23.00
-23.00
24.74
-132.04
0.52
-0.52
-2.37
0.00
-2.37
-75.67
-34.66
7.53
-42.20
925.28
-2057.60
-1132.32
2390.00
-3522.32
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.09
-0.09
0.00
-0.09
0.00
-0.09
0.00
0.00
81.75
0.00
81.75
0.00
81.75
14.07
0.00
14.07
92.70
Page 52
-200.00
-107.30
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
3
FAMILY PLANNING
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Family Planning Operation
608.80
-1469.21
0.00
0.00
0.00
1291.34
248.10
0.00
248.10
1652.03
-1469.21
182.83
243.72
-60.89
ii
NSV Camp
135.78
-117.72
0.00
0.00
0.00
0.00
2.94
0.00
2.94
132.84
-117.72
15.12
6.30
8.82
iii
Dissemination of manuals
on sterilisation standards
& quality assurance of
sterilisation services
0.00
0.00
0.00
0.00
0.00
0.00
6.28
0.00
6.28
-6.28
0.00
-6.28
2.57
-8.85
iv
Compensation for female
sterilisation
0.00
0.00
0.00
0.00
0.00
0.00
183.77
0.00
183.77
-183.77
0.00
-183.77
102.84
-286.61
v
Compensation for male
sterilisation
0.00
0.00
0.00
0.00
0.00
0.00
3.50
0.00
3.50
-3.50
0.00
-3.50
0.00
-3.50
vi
I.U.C.D. Camp & Incentive
0.00
0.00
0.00
0.00
0.00
30.60
0.00
0.00
0.00
30.60
0.00
30.60
3.93
26.67
4
ADOLESCENT
REPRODUCTIVE AND
SEXUAL HEALTH / ARSH
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Adolescent Health Program
0.00
5.84
0.00
0.00
0.00
0.00
10.66
0.00
10.66
-10.66
5.84
-4.82
0.00
-4.82
ii
Adolescent health District
Level
90.83
-39.88
0.00
0.00
0.00
0.00
0.00
0.00
0.00
90.83
-39.88
50.95
27.54
23.41
NRHM PIP 2009-10: Chhattisgarh
Page 53
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
iii
Adolescent Health District
Level
31.18
-172.71
0.00
0.00
0.00
0.00
0.00
0.00
0.00
31.18
-172.71
-141.53
0.00
-141.53
5
URBAN RCH
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Urban Health Programme
185.14
8.03
0.00
0.00
0.00
0.00
5.03
0.00
5.03
180.11
8.03
188.14
36.65
151.49
6
TRIBAL RCH
0.00
0.00
0.00
0.00
0.00
0.00
0.62
0.00
0.62
-0.62
0.00
-0.62
1.00
-1.62
7
VULNERABLE GROUPS
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8
INNOVATIONS/ PPP/
NGO
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
PNDT Programme
1.27
29.86
0.00
0.00
0.00
0.00
0.20
0.00
0.20
1.08
29.86
30.94
0.60
30.33
ii
Public Private Partnerships
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
iii
NGO Programme
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
iv
Other innovations( if any)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
v
NGO Participation in
service
38.50
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
38.50
0.00
38.50
0.00
38.50
9
INFRASTRUCTURE &
HUMAN RESOURCES
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 54
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
10
Contractual Staff &
Services
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Contractual staff Salary
(ANM)
17.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
17.00
0.00
17.00
196.17
-179.17
ii
Laboratory Technicians
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
iii
Staff Nurses
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
iv
Specialists (Anaesthetists,
Paediatricians, Ob/Gyn,
Surgeons, Physicians)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
v
Others - Computer
Assistants/ BCC Coordinator/ ASHA Link
Worker etc
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
vi
Incentive/ Awards etc. to
ASHA Link worker/ SN/
MOs etc.
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
11
Major civil works (New
constructions/
extensions/additions)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 55
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
i
Major civil works for
operationalisation of FRUS
0.00
0.00
0.00
0.00
0.00
0.00
26.12
0.00
26.12
-26.12
0.00
-26.12
0.56
-26.68
ii
Major civil works for
operationalisation of 24
hour services at PHCs
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
12
Minor civil works
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Minor civil works for
operationalisation of FRUs
0.00
0.00
0.00
0.00
0.00
0.00
4.80
0.00
4.80
-4.80
0.00
-4.80
5.60
-10.40
ii
Minor civil works for
operationalisation of 24
hour services at PHCs
0.00
0.00
0.00
0.00
0.00
0.00
9.17
0.00
9.17
-9.17
0.00
-9.17
0.00
-9.17
iii
Renovation of CHC
/PHC/SC
0.00
12.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
12.00
12.00
0.00
12.00
13
Operationalise Infection
Management &
Environment Plan at health
facilities
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
14
Other Activities (RCH-I
Civil Works)
0.00
0.00
0.00
0.00
0.00
0.00
1.70
0.00
1.70
-1.70
0.00
-1.70
7.74
-9.44
15
INSTITUTIONAL
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 56
S.No
1
PARTICULARS
2
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
STRENGTHENING
i
Monitoring & Evaluation /
HMIS
15.62
1.00
0.00
45.00
0.00
0.00
3.62
0.00
48.62
12.00
-44.00
-32.00
47.09
-79.10
ii
Sub Centre Rent and
Contingencies
0.00
0.00
0.00
0.00
0.00
0.00
0.20
0.00
0.20
-0.20
0.00
-0.20
15.11
-15.31
16
TRAINING
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Training Activities
0.00
26.67
0.00
0.00
0.00
0.00
3.69
0.00
3.69
-3.69
26.67
22.98
35.00
-12.02
17
Strengthening of Training
Institutions
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
18
Development of training
packages
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Training of paramedicals
131.10
-85.48
0.00
0.00
0.00
0.00
0.00
0.00
0.00
131.10
-85.48
45.62
0.00
45.62
19
Maternal Health Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Training in EmOC (FOGSI,
Mumbai)
0.00
0.00
0.00
0.00
46.73
0.00
0.00
0.00
46.73
0.00
-46.73
-46.73
41.71
-88.44
20
IMEP Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
21
Child Health Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 57
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
i
Training Nodal Funding
60.02
21.75
0.00
0.00
0.00
0.00
0.00
0.00
0.00
60.02
21.75
81.77
4.94
76.83
22
Family Planning Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
6.09
-6.09
i
LTT Training
0.00
0.00
0.00
0.00
0.00
6.09
0.00
0.00
0.00
6.09
0.00
6.09
0.00
6.09
ii
IUD Insertion Training
0.00
0.00
0.00
0.00
0.00
0.00
3.69
0.00
3.69
-3.69
0.00
-3.69
0.00
-3.69
iii
I.U.C.D. Training
8.79
-9.07
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8.79
-9.07
-0.29
0.00
-0.29
23
ARSH Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
2.70
-2.70
24
Programme Management
Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
4.04
-4.04
25
BCC / IEC
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Behaviour Change
Communication and IEC
0.00
-313.05
0.00
5.79
0.00
29.20
0.00
0.00
5.79
29.20
-318.84
-289.64
0.50
-290.14
ii
IEC Activities (RCH- I)
0.00
-302.96
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-302.96
-302.96
0.00
-302.96
iii
NSVT IEC Activities
0.00
-64.62
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-64.62
-64.62
0.00
-64.62
iv
Printing of Books Mitanin
0.00
-23.17
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
-23.17
-23.17
0.00
-23.17
26
Strengthening of BCC/IEC
Bureaus
(state and
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 58
S.No
1
PARTICULARS
2
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
district levels)
i
Mobile dispensary and IEC
8.24
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8.24
0.00
8.24
0.30
7.94
ii
Malaria Care for pregnant
Woman
0.00
0.42
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.42
0.42
0.00
0.42
27
Development of State
BCC/IEC strategy
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
28
Implementation of
BCC/IEC strategy
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
29
PROCUREMENT
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Mitanin Education and
equipments
349.42
-744.43
0.00
0.00
0.00
0.00
0.00
0.00
0.00
349.42
-744.43
-395.01
0.00
-395.01
ii
Medicine Supply for PHC /
Sc
11.80
41.04
0.00
0.00
0.00
0.00
88.76
0.00
88.76
-76.96
41.04
-35.92
14.00
-49.92
iii
ANM Kit, Kit A,B & PHC
Kit
432.68
-1324.20
0.00
0.00
0.00
0.00
0.00
0.00
0.00
432.68
-1324.20
-891.51
100.64
-992.15
30
PROGRAMME
MANAGEMENT
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 59
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
i
Salary of DPMUs
9.62
-70.59
0.00
0.00
0.00
182.34
52.08
0.00
52.08
139.88
-70.59
69.29
20.54
48.75
ii
Contractual Salary
(SPMU)
0.00
158.19
0.00
8.32
0.00
0.00
0.00
0.00
8.32
0.00
149.87
149.87
5.25
144.62
31
OTHER
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Infrastructure Renovation
310.85
-0.10
0.00
0.00
0.00
0.00
0.00
0.00
0.00
310.85
-0.10
310.75
0.00
310.75
ii
Strengthening routine SHC
113.20
52.17
0.00
0.00
0.00
0.00
0.00
0.00
0.00
113.20
52.17
165.37
0.00
165.37
iii
UNTIED Fund Dist.
Hospital
265.87
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
265.87
0.00
265.87
0.00
265.87
iv
Incentive for 24 hour PHC
7.80
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
7.80
0.00
7.80
0.00
7.80
v
Strengthening SIHFW
0.00
1.18
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
1.18
1.18
0.00
1.18
vi
Contingencies
0.00
-37.01
0.00
14.50
0.00
0.00
0.00
0.00
14.50
0.00
-51.52
-51.52
5.86
-57.38
vii
Improving CHC PHC
Performance
0.00
48.96
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
48.96
48.96
0.00
48.96
viii
Initiative to MO serving in
under Service
0.00
50.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
50.00
50.00
0.00
50.00
ix
Grant Received from GOI
0.00
3576.00
4280.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
7856.00
7856.00
0.00
7856.00
NRHM PIP 2009-10: Chhattisgarh
Page 60
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
TOTAL PART - A
3500.60
-3116.74
PART - "B"
0.00
1
ASHA
i
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
4280.00
73.62
46.73
3361.31
1963.12
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
Mitanin Selection &
Training programme
0.00
629.27
0.00
0.00
ii
Selection & Training of
ASHA
0.00
0.00
0.00
iii
Procurement of ASHA
Drug Kit
15.33
2.93
2
Untied Funds
0.00
i
UNTIED Fund CHC
ii
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
0.00
2083.47
4898.80
1042.91
5941.71
3384.77
2556.94
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
400.00
400.00
148.30
0.00
548.30
251.70
229.27
480.98
25.94
455.04
0.00
0.00
0.00
221.00
0.00
221.00
-221.00
0.00
-221.00
161.21
-382.21
0.00
269.57
0.00
0.00
2.00
0.00
271.57
13.33
-266.64
-253.31
5.00
-258.31
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
4.49
0.00
4.49
-4.49
0.00
-4.49
0.00
-4.49
UNTIED Fund SHC
349.73
-420.92
0.00
0.00
0.00
0.00
27.20
0.00
27.20
322.53
-420.92
-98.39
490.50
-588.89
iii
Untied Fund PHC
164.34
-143.05
0.00
0.00
0.00
0.00
17.78
0.00
17.78
146.56
-143.05
3.51
25.00
-21.49
iv
Untied fund for Adolescent
counselling clinic
0.00
0.00
0.00
0.00
0.00
3.99
0.00
0.00
0.00
3.99
0.00
3.99
0.00
3.99
v
Fund for V.W.H.S.C.
1578.10
-2011.00
0.00
0.00
0.00
146.00
29.50
0.00
29.50
1694.60
-2011.00
-316.40
0.00
-316.40
1
2
NRHM PIP 2009-10: Chhattisgarh
Page 61
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
3
Hospital Strengthening
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Up gradation of DH to
IPHs
0.00
320.00
0.00
0.00
0.00
0.00
13.71
0.00
13.71
-13.71
320.00
306.29
57.26
249.03
ii
Sub Centres
0.00
0.00
0.00
0.00
0.00
0.00
0.06
0.00
0.06
-0.06
0.00
-0.06
1.50
-1.56
iii
Strengthening of District
and Su-divisional Hospitals
0.00
0.00
0.00
0.00
0.00
0.00
5.51
0.00
5.51
-5.51
0.00
-5.51
18.00
-23.51
4
Annual Maintenance
Grants
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Annual Maintenance grant
for PHC
88.20
0.00
0.00
0.00
0.00
0.00
4.84
0.00
4.84
83.36
0.00
83.36
19.50
63.86
ii
Annual Maintenance for
Leprosy
0.00
0.00
0.00
0.00
0.00
33.00
0.00
0.00
0.00
33.00
0.00
33.00
3.45
29.55
5
New Constructions/
Renovation and Setting up
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
PHCs
0.00
0.00
0.00
0.00
0.00
0.00
8.95
0.00
8.95
-8.95
0.00
-8.95
15.22
-24.17
ii
SHCs/Sub Centres
0.00
0.00
0.00
0.00
0.00
0.00
4.39
0.00
4.39
-4.39
0.00
-4.39
1.91
-6.30
6
Corpus Grants to
HMS/RKS
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
NRHM PIP 2009-10: Chhattisgarh
Page 62
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
i
District Hospitals
0.00
0.00
0.00
0.00
0.00
20.00
5.00
0.00
5.00
15.00
0.00
15.00
6.69
8.31
ii
CHCs
0.00
0.00
0.00
0.00
0.00
33.00
29.33
0.00
29.33
3.67
0.00
3.67
7.50
-3.83
iii
PHCs
0.00
0.00
0.00
0.00
0.00
76.50
35.38
0.00
35.38
41.12
0.00
41.12
12.00
29.12
iv
Other or if not bifurcated
as above
0.00
0.00
0.00
0.00
0.00
2.00
1.00
0.00
1.00
1.00
0.00
1.00
478.00
-477.00
v
Jeevan deep Samiti (Dh,
CHC, PHC)
403.55
-144.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
403.55
-144.00
259.55
0.00
259.55
7
District Action Plans
(Including Block, Village)
66.48
-49.98
0.00
0.00
0.00
0.00
2.83
0.00
2.83
63.65
-49.98
13.67
5.00
8.67
8
Panchayati Raj Initiative
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Constitution and
Orientation of Community
leader & of
VHSC,SHC,PHC,CHC etc
0.00
0.00
0.00
0.00
0.00
0.00
0.10
0.00
0.10
-0.10
0.00
-0.10
0.00
-0.10
9
Mainstreaming of AYUSH
0.00
0.00
0.00
0.00
0.00
0.00
0.50
0.00
0.50
-0.50
0.00
-0.50
0.40
-0.90
10
IEC-BCC NRHM
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Health & Swasthya Mela
0.00
88.63
0.00
0.00
0.00
0.00
7.38
0.00
7.38
-7.38
88.63
81.25
15.21
66.04
NRHM PIP 2009-10: Chhattisgarh
Page 63
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
11
Mobile Medical Units
(Including recurring
expenditures)
0.00
721.92
0.00
34.92
0.00
0.00
0.00
0.00
34.92
0.00
687.00
687.00
675.00
12.00
12
Referral Transport
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
13
School Health Programme
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
14
Additional Contractual
Staff (Selection, Training,
Remuneration)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
15
PPP/ NGOs
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Rural Medical Assistant
0.00
0.00
0.00
0.00
0.00
144.40
0.00
0.00
0.00
144.40
0.00
144.40
0.00
144.40
16
Training
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Nursing Training
(Strengthening of Existing
Training
Institutions/Nursing
School)
109.05
-85.00
0.00
0.00
0.00
0.00
2.62
0.00
2.62
106.43
-85.00
21.43
0.00
21.43
17
Training and Capacity
Building Under NRHM
0.00
0.00
0.00
0.00
0.00
0.00
1.81
0.00
1.81
-1.81
0.00
-1.81
0.00
-1.81
NRHM PIP 2009-10: Chhattisgarh
Page 64
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
i
Other training and capacity
building programmes
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8.73
-8.73
18
Incentives Schemes
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
ii
Incentives to Medical
Officers (PHCs)
0.00
0.00
0.00
0.00
0.00
0.00
0.06
0.00
0.06
-0.06
0.00
-0.06
1.98
-2.04
19
Planning, Implementation
and Monitoring
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
4.03
-4.03
20
Procurements
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Procurement of Drugs/
NRHM Drug Kit
0.00
1239.06
0.00
0.00
0.00
0.00
7.34
0.00
7.34
-7.34
1239.06
1231.72
134.67
1097.04
ii
Procurement of Equipment
0.00
0.00
0.00
0.00
0.00
0.00
3.26
0.00
3.26
-3.26
0.00
-3.26
35.00
-38.26
21
PNDT Activities
0.00
0.00
0.00
0.00
0.00
0.00
0.13
0.00
0.13
-0.13
0.00
-0.13
0.22
-0.35
22
Regional drugs warehouses
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
23
New Initiatives/ Strategic
Interventions (As per State
health policy)/ Innovation/
Projects (Telemedicine,
Hepatitis, Mental Health,
Nutrition Programme for
0.00
0.00
0.00
0.00
0.00
0.00
0.12
0.00
0.12
-0.12
0.00
-0.12
0.62
-0.74
NRHM PIP 2009-10: Chhattisgarh
Page 65
S.No
1
PARTICULARS
2
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
Pregnant Women,
Neonatal) NRHM Helpline)
as per need (Block/ District
Action Plans)
24
Health Insurance Scheme
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
25
Research, Studies, Analysis
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
26
State level health resources
centre(SHSRC)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Strengthening SHRC
0.00
293.86
0.00
0.00
38.09
0.00
16.57
0.00
54.66
-16.57
255.77
239.20
1.83
237.37
27
Support Services
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Other Support Programmes
0.00
0.00
0.00
0.00
0.00
0.00
44.56
0.00
44.56
-44.56
0.00
-44.56
123.10
-167.66
28
NRHM Management Costs/
Contingencies
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Block Programme
Management Cost
0.00
100.00
0.00
0.00
0.00
93.16
17.84
0.00
17.84
75.32
100.00
175.32
57.33
117.99
ii
District level
0.00
0.00
0.00
0.00
0.00
0.00
6.54
0.00
6.54
-6.54
0.00
-6.54
2.80
-9.34
iii
State level
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
3.00
-3.00
NRHM PIP 2009-10: Chhattisgarh
Page 66
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
iv
Audit Fees
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
v
Concurrent Audit system
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
vi
Other Management
expenses
0.00
0.00
0.00
0.00
0.00
0.00
7.11
0.00
7.11
-7.11
0.00
-7.11
10.60
-17.71
vii
Telephone and Mobile
phone, Contingencies
expenses
0.00
0.00
0.00
0.00
0.00
0.00
0.26
0.00
0.26
-0.26
0.00
-0.26
2.15
-2.41
viii
Mobility Support to
BMO/MO/Others
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.30
-0.30
29
Other Expenditures (Power
Backup, Convergence etc)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
11.92
-11.92
i
Operationalisation of FRU
to IPHs
0.00
104.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
104.00
104.00
0.00
104.00
ii
Nursing College Building
(DME)
0.00
0.00
0.00
0.00
150.00
0.00
0.00
0.00
150.00
0.00
-150.00
-150.00
0.00
-150.00
iii
Naxal effected area
(Dantewada and Bijapur)
0.00
0.00
0.00
0.00
0.00
441.00
0.00
0.00
0.00
441.00
0.00
441.00
0.00
441.00
iv
Bal Hruday Suraksha
Yojana
0.00
0.00
0.00
0.00
300.00
0.00
0.00
0.00
300.00
0.00
-300.00
-300.00
0.00
-300.00
NRHM PIP 2009-10: Chhattisgarh
Page 67
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
v
Trauma Centre
0.00
0.00
0.00
47.08
0.00
0.00
0.00
0.00
47.08
0.00
-47.08
-47.08
0.00
-47.08
vi
IPH Gandhinagar
0.00
0.00
0.00
0.00
2.70
0.00
0.00
0.00
2.70
0.00
-2.70
-2.70
0.00
-2.70
vii
Contingencies
0.00
0.00
0.00
23.06
0.00
0.00
0.00
0.00
23.06
0.00
-23.06
-23.06
0.00
-23.06
viii
Grant Received from GOI
0.00
5432.90
3389.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
8821.90
8821.90
0.00
8821.90
TOTAL PART -B
2774.79
6078.61
3389.00
374.63
890.79
1393.05
677.46
0.00
1942.87
3490.39
8202.20
11692.58
2422.57
9270.01
PART - "C"
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Immunisation Activities
196.21
39.95
0.00
0.00
0.00
408.61
37.82
0.00
37.82
567.01
39.95
606.96
205.10
401.86
ii
Cold chain maintenance
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
iii
Pulse Polio operating costs
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
TOTAL PART -C
196.21
39.95
0.00
0.00
0.00
408.61
37.82
0.00
37.82
567.01
39.95
606.96
205.10
401.86
OTHERs
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
i
Bank Interest Fund
0.00
317.86
72.15
0.00
0.00
0.00
0.00
0.00
0.00
0.00
390.01
390.01
0.00
390.01
ii
MNGO Preparatory Grant
0.00
232.50
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
232.50
232.50
0.00
232.50
iii
Pulse Polio
-1.04
29.41
671.00
0.00
0.00
663.15
158.14
0.00
158.14
503.97
700.41
1204.37
663.15
541.22
NRHM PIP 2009-10: Chhattisgarh
Page 68
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
D.H.S.
S.H.S.
GIA
Received
from
GOI
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
Closing / Unspent
Balance as on
31.12.08
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
vi
Construction of (40+78)
Sub centre (SIP)
48.47
2.50
0.00
0.00
0.00
0.00
0.00
0.00
0.00
48.47
2.50
50.97
0.00
50.97
v
PMU Training NIHFW
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
vi
Special IEC for FWP and
RCH
0.00
205.60
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
205.60
205.60
0.00
205.60
vii
Fund for Data Collection
from Unicef
0.00
0.37
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.37
0.37
0.00
0.37
viii
Sishu Sanraksaan Maah
(Unicef)
0.41
-5.31
0.00
0.00
0.00
9.20
0.00
0.00
0.00
9.61
-5.31
4.30
0.00
4.30
xi
European Union State
Partnership
0.00
512.90
0.00
0.00
100.00
0.00
0.00
0.00
100.00
0.00
412.90
412.90
5.00
407.90
x
European Union (Bal
Hruday Suraksha Yojana)
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
xi
European Union (Dist
Hospital Korba for ISO)
0.00
0.00
0.00
0.00
0.00
7.00
0.00
0.00
0.00
7.00
0.00
7.00
0.00
7.00
xii
Ayush Dispensaries
(Released to Ayush)
0.00
162.50
0.00
0.00
44.88
0.00
0.00
0.00
44.88
0.00
117.62
117.62
0.00
117.62
xiii
State Contribution
0.00
1200.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
0.00
1200.00
1200.00
0.00
1200.00
NRHM PIP 2009-10: Chhattisgarh
Page 69
S.No
PARTICULARS
Unspent Balance as
on 1st April 08
GIA
Received
from
GOI
D.H.S.
S.H.S.
3
4
5
Total
47.84
2658.32
TOTAL (A+B+C)
6979.42
5942.95
1
2
Expenses
at State
Level
Funds to District
Total
Expenditure
(6+7+9)
Release
to State
level
others
Release
to the
District
Expenditure
District
Refund
from
District
6
7
8
9
10
743.15
0.00
144.88
679.35
158.14
8412.15
448.25
1082.40
5842.33
2836.54
Closing / Unspent
Balance as on
31.12.08
Closing /
Unspent
Balance
as on
31.12.08
Estimated
Expenses
Jan 09 to
March 09
Estimated
Balance
as on
31st
March
2009
D.H.S.
(3+8-910)
S.H.S.
(4+5-67+10)
11
12
13
14
15
16
0.00
303.02
569.05
3256.60
3825.64
668.15
3157.49
0.00
4367.18
9985.22
12824.45
22809.67
6680.59
16129.08
Physical and Financial Report
Table 1.25: Physical and financial progress
Sl
No.
Programme Head
Key Activities Proposed
Maternal Health
b) Blood storage facility
Work in progress
c) operationalise 24hr PHC
5 as per GTZ report and the IPHS.
However, on call basis there are 418 PHCs
(as per districts report) are catering
service.
lack of staff nurse continue
as the major hurdle- to
address this year
d)
operationalise
Safe
Abortion service in FRUs
16 Master Trainer trained
Training of trainees to be
started soon
NRHM PIP 2009-10: Chhattisgarh
Total
Layout
Physical Achievement as on 31 Dec 2008
Page 70
remarks, if any
e) operationalise RTI/ STI
services
Training ongoing at district level
To be completed by July
2009
Referral Transport Linkages
– second referral for JSY
Money yet to be received from GoI
Yet to
District
JSY
Home delivery – 46138
Out of 3487 lakh, 14crore23 lakh is already
disbursed to district.
Inst. delivery- 67781
be
released
to
Total- 113919
ANC Kit
women
2
Child Health
For
Pregnant
With UNICEF Support
IMNCI in three district
Training completed by SIHFW in
coordination with UNICEF for 3 District.
Facility Based New Born
Care at 12 Dist Hospital
4 SNCU plan has been finalised and SNCU at Durg is almost
submitted, Rajnandgaon, Durg, Bastar, and completed.
Raigarh.
Home Based New Born Care
57,730 Mitanin trained
School Health Program
School health card is under process.
NRHM PIP 2009-10: Chhattisgarh
Page 71
3
Family Planning
Care of Children with
Severe or Acute Mal
nutrition Baal Suposhan
Yojana
Training of paediatrics and staff nurses In
coordination
completed at 8 districts hospitals, UNICEF and BPNI.
Dantewada, Dhamtari, Raipur, and
Mahasamund. Kawardha, Bilaspur, Janjgir
Champa and Raigarh.
Management of Diarrhoea
and Micronutrient.
MOU is prepared
Neonatal and Child Survival
Initiatives under Mitanin
Programme
Navajat
Swagath Bheit
Welcome kits finalised and under printing,
Guidelines and feedback systems finalised
Wage Compensation
Sterilization
Activities ongoing- cases upto February 08
To be optimised by March
Activities ongoing- cases upto February 08
To be optimised by March
for
NSV Camps approach
with
4
Adolescent Reproductive Untied fund for Adolescent
/Sexual Health Initiative
Counselling clinic
Training ongoing except in few districts- Training is slow than
ARSH clinics being started in 2 district on a expected, in want of proper
pilot basis
training facilities
5
Urban Health
Urban Mitanin/Urban Post
2 districts completed mapping and urban To be completed by June
mitanins got selected in 1 district
2009
6
Tribal Health
RCH camps at Tribal Blocks
Plans made by CMHOs
7
Intervention
for
Vulnerable groups
the Emergency fund for conflict
areas
NRHM PIP 2009-10: Chhattisgarh
To be completed by April
2009
Funds yet to be received from GoI
Page 72
8
Implementation
PNDT act
of
the Implementation of the PNDT
act
Activity ongoing
9
Implementation of IMEP Implementation of IMEP
and quality assurance cell and quality assurance cell
Activity ongoing
10
Institutional Strengthening
BCC
Activities like printing and dissemination of
Health Calendar and Diary, JSY messages
in PDS rice bags, Organising various
health days complete
11
Training Activities
FRU Multiskill training
2 batches of training complete in the year,
third batch ready to start
Training of Doctors on
essential PHC level service
more than 100 doctors trained
To be complete by July
2009
SBA training
More than 300 trained
Training to be completed
within 6 months
IMNCI training
Mitanin training completed.
Training
of
Doctors
laparoscopic sterilisation.
Fund released to DHS Bilaspur.
EMOC training
46 lakh released to FOGSI for EMOC Training yet to be started.
training.
NRHM PIP 2009-10: Chhattisgarh
some clarity regarding the
guidelines particularly on
the use of incinerator need
to be addressed
Page 73
Training on
installation
IUD
380A
Training of Master Trainer completed, TOT for other district will
district level training of field worker in be initiated soon.
Raipur is started.
Programme
Unit
Management
SPMU/ DPMU and Blok PMU established , Need relaxation in norms
rest vacancy will be filled immediately
for BPMU.
NRHM Part B
1
Jeevan Deep Samiti
Improvement
institutions.
of
Health
DH-15/15
CHC-129/136
PHC- 695/721 --
2
Untied fund to Strengthen
Routine Sub Health Centre
Fund allocated to 4694 Sub health Centre
3
Mitanin Programme
Mitanins trained in :- Swasthya Panchayat
yojana- 58189
Sehat, Poshan, Social security- 58430
Ayush- Jadi Buti le kare Ilaj- 57340
Nischaya -Pregnancy test kit- 30000
4
Trauma Care Centres in Establishment of trauma
National Highways
care and ambulance. For
emergency care.
10 ambulances realised to district. 10
ambulance under process Trauma care
centre yet to establish
5
Mobile Medical Unit
16 MMU is finalized with Medisfare
Es
NRHM PIP 2009-10: Chhattisgarh
Page 74
Training
indicated
of
ANMs
6
Bal Hruday
Yojana
Suraksha
7
Untied fund for village
Health and Sanitation
committee
18322 VHSC formed, 16 653 account Process under Panchayat
opened and fund released to 14236 VHSC
leadership
8
Monitoring
Evaluation-HMIS
State level training on web based data To be held in Feb. 09.
management completed, training for the
district level and below is planned.
9
Village and Panchayat
level capability Building
9300 panchayat prepared hamlet based
HHDI.
more
than
20000
PRI
representatives oriented
10
Alternative
Clinical
Human
Resource
Development
through
Nurse
Practitioner
Programme
and
improving Nurse Training
Facilities
Programme to be started in Raipur Nursing
college.
11
Induction Training of
BMHOs and re orientation
of CMHOs on Health
Programme
administration
and
Management
Yet to initiate
and
NRHM PIP 2009-10: Chhattisgarh
85 children have been operated and 445
registered.
Waiting for the promotion
process to complete
Page 75
12
Professional on Health
Management- the PHRN
390 health professional trained on PHRN will be complete by June
first track training.
2009
13
Closing Residential Gap
Money Released to districts – construction
to be initiated soon
14
Telephone
PHCs
15
SHRC strengthening
All agreed activities complete
16
Block
Programme Establishment of block level
Management Unit
programme management
63 BPM and 76 BADA appointed.
for
SHC
/ Tele
communication
established at PHC and
CHC
NRHM PIP 2009-10: Chhattisgarh
Out of target, 5500 telephone connection
4400 telephone connection established.
Page 76
The Project Implementation Plan for the year 2009-10 has the following components:o Part A: Reproductive and Child Health priority areas under RCH-II flexible pool.
o Part B: The Cross cutting Health Sector Priorities & Special Initiatives under NRHM
Flexible Pool
o Part C: The specific activity plan for Universal Immunisation Programme.
o Part D: National Disease Control Programmes
o Part E: Plan for Convergence with various Health as well as other Sector Programmes
However, the projected need for coming year, including the plans for available balance with
the state comes over and above the available envelop for Part A & B. We hope the GoI shall
allocate funds according to the need projected by the state, looking at the objective situation.
The overall budget requirement for 2009 – 10 is as projected below:
Table 1.26: Summary of outlay for 2009 – 10
NRHM Total Outlay 2009 – 10
PART -A
1,21,05,06,019
PART -B
1,55,51,53,400
PART -C
9,66,52,688
PART -D
46,55,41,207
PART -E
TOTAL (Part A to Part E)
-
3,32,78,53,314
Infrastructure and maintenance(Central Govt. Scheme)
88,80,00,000
Special accommodation/Residential Facilities at naxalite affected
area, recommended by Ministry of Tribal GoI
66,00,00,000
GRAND TOTAL
NRHM PIP 2009-10: Chhattisgarh
4,87,58,53,314
Page 77
Part A- RCH II Flexi-pool
Summary
The state of Chhattisgarh, amongst the newly formed 3 states of India about 7 years back, is on
the process of collecting all possible resources, planning and innovating for achieving the
desired goals and objectives of better health and health services provision. From the last 3
years of implementation of RCH-II and the past inputs from RCH-SIP, similar programmes,
and I and through improved community involvement through interventions like Mitanin
Programme, it has been able to record some remarkable improvements in some of the critical
health indicators like IMR and some of the community level practices and behaviours. The fact
that the health background of the state is not very sound, the infrastructure situation is very
weak, major gaps are there in critical manpower availability, and the skill gaps in available
personnel are high, the state has to strive forward in terms of achieving its health goals. The
detailed situation analysis has been presented as part of the introduction of the NRHM
comprehensive PIP.
Table 2.1: Status and Targets for next two years
RCH II Chhattisgarh
GOAL
Current
status
(year
source)
India
Target
2008& 09
200910
201011
Current
status
(year
source)
Target
2008& 09
200910
MMR
379
(SRS 01-03)
300
<200
301
(SRS 01-03)
200
<100
IMR
61
(SRS 2007)
<55
<40
57
(SRS 2007)
45
<30
TFR
2.62
(NFHS 3)
2.2
2.1
2.68
(NFHS 3)
2.3
2.1
201011
Table 2.2: Status and Goals on RCH Outcomes
RCH Outcomes
Current Status
Target
(specify year & source)
08 – 09
09–10
10-11
Maternal Health
% of pregnant women receiving full ANC coverage (3 ANC checks, 2 TT injections & 100 IFA
Tablets)
Overall
78 % (DLHS 3)
NRHM PIP 2009-10: Chhattisgarh
80%
95%
100%
Page 78
SC/ST
% of pregnant women age 15-49 who are anaemic
Overall
58.0% (NFHS-3)
60%
55%
50%
SC/ST
% of births assisted by a doctor/nurse/LHV/ANM/other health personnel
Overall
44.3% (NFHS-3)
60%
65%
70%
27.2% (CES 2006)
40%
50%
60%
SC/ST
% of institutional births
Overall
SC/ST
% of mothers who received post partum care from a doctor/ nurse/ LHV/ ANM/ other health
personnel within 2 days of delivery for their last birth
Overall
25.3% (NFHS-3)
50%
75%
80%
50%
60%
70%
95%
95%
SC/ST
Child Health
% of neonates who were breastfed within one hour of life
Overall
50.1.%(DLHS 2008)
SC/ST
% of infants who were breastfed exclusively till 6 months of age
Overall
82.0% (NFHS-3)
95%
SC/ST
% of infants receiving complementary feeds apart from breast feeding at 6 months
Overall
54.5% (NFHS-3)
75%
70%
80%
80%
100%
100%
50%
30%
30%
SC/ST
% of children 12-23 months of age fully immunized
Overall
59.3% (CES 2006)
SC/ST
% of children 6-35 months of age who are anaemic
Overall
81% (NFHS-3)
SC/ST
% of children under 5 years age who have received all nine doses of Vitamin A
Overall
44% (UNICEF Study)
70%
85%
95%
SC/ST
% of children under 3 years with diarrhoea in the last 2 weeks who received ORS
Overall
42.0% (NFHS 3)
NRHM PIP 2009-10: Chhattisgarh
80%
100%
100%
Page 79
SC/ST
% of children under 3 years age who are underweight
Overall
52.1% (NFHS-3)
45%
45%
40%
50%
55%
60%
SC/ST
Family Planning
Contraceptive prevalence rate (any modern method)
Overall
49.7% (DLHS 3)
SC/ST
Contraceptive prevalence rate (limiting methods)
Male Sterilization
1.8%(DLHS 3)
3.50%
5.00%
8.00%
Female Sterilization
41.3%(DLHS 3)
42%
45%
50%
Contraceptive prevalence rate (spacing methods)
Oral Pills
1.7%(DLHS 3)
2%
5%
7%
IUDs
0.6%(DLHS 3)
1%
3%
5%
Condoms
1.6%(DLHS-3)
3%
5%
8%
10%
12%
15%
12%
15%
20%
Unmet need for spacing methods among eligible couples
Overall
9.1 %(DLHS 3)
SC/ST
Unmet need for terminal methods among eligible couples
Overall
11.8 %(NFHS-3)
SC/ST
NRHM PIP 2009-10: Chhattisgarh
Page 80
Table 2.3: Status and Goals of RCH intermediate indicators
RCH Intermediate / MOU Indicator
Current Status
Target
(year, source)
2009-10 (quarter-wise)
Q1
Q2
Q3
09–10
10–11
710
710
Q4
Infrastructure
No. and % PHCs upgraded to provide 24X7 72 (District
RCH services
08)
Report 350
360
No. and % of health facilities upgraded to FRUs, fulfilling the minimal criteria per the FRU guidelines (at least 3 critical criteria)
a. District Hospitals
11
1
2
2
1
17
17
b. Sub-district Hospitals
0
c. CHCs
12
12
12
12
16
64
96
d. Block PHCs
0
0
0
0
0
0
0
No. and % of functional Sub-Centres (ANM 4725/5495
(NRHM 0
is posted and working out of the facility)
dist report 08)
5
5
6
4741
4741
No. and % of sampled FRUs following 100% (NRHM dist 100 %
agreed infection control and health care report 08)
waste disposal procedures
100 %
100 %
100 %
100 %
100 %
No. and % of health facilities that have
operationalised IMEP guidelines
100 %
100 %
100 %
100 %
100 %
NRHM PIP 2009-10: Chhattisgarh
100 %
Page 81
Human Resources
No. and % of ANM positions filled (against 4984/5653
(NRHM 4180
required)
dist report 08)
Ist ANM
4741
II nd AMN
400
No. and % of specialist positions filled at 37 Anaesthetist, 45 40%
FRUs (against required)
Gynaecologist(NRHM
dist report 08)
4180
4180
0
600
40%
60%
4692
4692
4692
4741
4741
1000
2344
60%
80%
100%
Anaesthetist - 37
15
12
64
96
Gynaecologist - 45
10
10
64
96
0
18/18
18/18
Programme Management
No. and % of state and districts having full
time programme managers for RCH with
financial & administrative powers delegated 16/18
No. and % of sampled state and district All district by CMHO
programme managers whose performance
MD/ Director
was reviewed during the past 6 months
NRHM PIP 2009-10: Chhattisgarh
2
0
0
All district All
All
All district All
by CMHO district by district by by CMHO
district
CMHO
CMHO
by
CMHO
Page 82
All
district
by
CMHO
% of district action plans ready-
100% (NRHM dist 100%
report 08)
(NRHM
dist report
08)
100%
(NRHM
dist
report
08)
100%
(NRHM
dist
report
08)
100%
(NRHM
dist report
08)
100%
(NRHM
dist
report
08)
100%
(NRHM
dist
report
08)
% of sampled districts that are 3 district selected not
implementing M&E triangulation involving started
community
3 dist
3 dist
3 dist
8 district
16
district
SPMU in place with 100 % staff
No
Yes
No. and % DPMU staff in place
30/48 (NRHM
report 08)
48/48
(NRHM
dist
report
08)
48/48
48/48
48/48
48/48
100%
100%
dist 48/48
(NRHM
dist report
08)
If project If project
continue continue
Financial Management
% of districts reporting quarterly financial 87.5% (14/16)
performance in time
87.5%
100%
Logistics / Procurement
NRHM PIP 2009-10: Chhattisgarh
Page 83
100%
100%
% of district not having at least one month
stock of
Measles vaccine
OCP
EC Pills
Surgical Gloves
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
25
25
25
155
150
15
30
30
Training
No. and % of Medical Officers trained in
SBA
55
Life-saving anaesthesia skills
53
EmOC
41
12
12
12
12
48
48
RTI/STI
452/800
50
50
50
50
200
200
MTP using MVA
50
50
50
150
150
MTP using other methods
50
50
50
150
150
20
20
20
80
90
IMNCI
25
15
18 Doctors trained as 20
Master
Trainers
(Unicef, 08)
Facility Based Newborn care
NRHM PIP 2009-10: Chhattisgarh
Page 84
Care of sick
malnutrition
children
and
severe 3 paediatrician + 8 0
Staff Nurse trained by
UNICEF
4
8
4
NSV
67/167 (NRHM
report 08)
30
30
30
100
100
Laparoscopic sterilisation
26 Doctors
5
5
5
10
25
25
Minilap
95 Doctors
25
25
25
25
100
100
IUD insertion
38 doctors
50
50
50
50
200
100
ARSH
All doctors
0
0
0
0
0
0
ANM
1300/1400
25
25
25
25
100
100
LHV
300/600
0
30
30
30
90
100
Staff nurse
183/200
0
17
0
0
17
100
200
200
200
200
800
1500
50
50
50
50
200
400
40
40
40
40
160
--
To be checked with UNICEF
dist 10
IMEP
No. and % Staff trained in SBA
No. and % Staff trained in IMNCI
ANM
LHV
280 By UNICEF
Staff Nurses
NRHM PIP 2009-10: Chhattisgarh
Page 85
ANM
0
No. and % of staff nurses trained in Facility None
Based Newborn Care
40
40
40
40
160/ 866
No. and % of ASHAs trained in Home Based 57000/60000
Newborn Care
0
0
0
0
0
200
No. and % Staff trained in IUD insertion
ANM
233
0
0
0
0
4622
0
LHV
41
0
0
0
0
749
0
Staff nurse
38
0
0
0
0
866
0
None
1000
1000
1000
1000
4000
100
100
100
100
200
200
200
200
No. and % of staff trained in ARSH
ANM
LHV
Staff nurse
9
Programme Managers
No. and % of state and district programme None
managers trained on IMEP
NRHM PIP 2009-10: Chhattisgarh
Page 86
800
No. and % of health personnel who have None
undergone
Contraceptive
Update/ISD
Training
to
Maternal Health
% of ANC registrations in first trimester of 60 %
pregnancy
60%
65%
70%
75%
80%
90%
% of 24 hrs PHCs conducting minimum of 27/310
(8.70%) 0
10 deliveries/month
(NRHM dist report
08)
110
110
113
360
360
No and % of CEmONC centres conducting 19 (NRHM District 10
Caesarean Sections
Report)
10
10
10
40
60
0
0
0
0
100%
100%
0
0
0
0
100%
100%
90
90
90
360
721
No. and % of health facilities providing RTI/STI services
a. DHs
100%
b. SDHs
NA
c. CHCs
100%
d. PHCs
230
out of 721 90
(NRHM dist report
08)
No. and % of health facilities providing MTP services
NRHM PIP 2009-10: Chhattisgarh
Page 87
a. DHs
100%
0
0
0
0
100%
100%
b. SDHs
NA
c. CHCs
32/136
25
25
25
29
104
0
d. PHCs
7/721
0
0
0
0
7
7
0
0
0
0
0
0
20
10
11
100%
100%
No. of districts where Referral Transport All
services are functional
No. and % of planned RCH outreach camps
held
No. and % of planned Monthly Village 49% (NRHM
Health and Nutrition Days held
report 08)
dist 10
Child Health
No. of districts where IMNCI logistics are 3 out of16
supplied regularly
0
2
0
2
7dist
10dist
No. and % of health facilities with at least 21 out of 32 FRUs
one provider trained in Facility Based
Newborn Care
5
5
5
5
41
60
No. and % of sampled outreach session 100%
where AD syringe use and safe disposal are
followed
100%
100%
100%
100%
100%
100%
No. of districts and schools where School 0 District
Health Programme is implemented
4
4
4
4
16
16
NRHM PIP 2009-10: Chhattisgarh
Page 88
Family Planning
No. and % of health facilities providing Female Sterilization services
a. DHs
17/18
0
1
O
o
18/18
18/18
b. SDHs
NA
c. CHCs
115/136
5
5
5
6
136
136
d. PHCs
None
0
0
0
0
0
0
0
2
0
0
18/18
18/18
No. and % of health facilities providing Male Sterilization services
a. DHs
16/18
b. SDHs
NA
c. CHCs
106 / 136 (NRHM dist 0
report 08)
10
10
7
136
136
d. PHCs
23/721
Report)
0
0
0
23
23
(District 0
No. and % of health facilities providing IUD insertion services
a. CHCs
137
0
0
0
0
100%
100%
b. PHCs
711
0
10
0
0
100%
100%
c. Sub centres
4741
100%
100%
100%
100%
100%
100%
No. of accredited private institutions providing:
NRHM PIP 2009-10: Chhattisgarh
Page 89
a. Female sterilisation services
Not available
b. Male sterilisation services
Not available
c. IUD insertion services
Not available
% of districts with Quality Assurance 100% for sterilization
Committees (QACs)
100%
100%
100%
100%
100%
100%
% of district QACs having quarterly 100% for sterilization
meetings
100%
100%
100%
100%
100%
100%
% of planned Female Sterilisation camps
held in the quarter
80%
80%
100%
100%
% of planned NSV camps held in the quarter 464
60%
60%
80%
100%
20%
30%
40%
100%
100%
Adolescent Reproductive and Sexual Health
% of ANC registrations in first trimester of 33606
out of 20%
pregnancy for women < 19 years of age
675802 (4.9 %)
No. and % of health facilities providing ARSH services
a. FRUs
100%
100%
100%
100%
100%
100%
100%
b. CHCs
100%
100%
100%
100%
100%
100%
100%
c. PHCs
None
d. Others
None
NRHM PIP 2009-10: Chhattisgarh
Page 90
No. and % of health facilities with at least 9
one provider trained in ARSH
133
300
700
Vulnerable Groups
No. and % of district plans with specific 2/18
(Naxalite 0
activities to reach vulnerable communities
effected district )
0
0
0
2
2
Innovations/PPP/NGO
No. of districts covered under MNGO 12/18 District
scheme
0
0
0
0
12
12
No.
of
MNGO
implementation
0
0
0
0
7
7
0
2
2
0
18
18
proposals
under 7/18 District
Monitoring and Evaluation
% of districts reporting on the new MIES 14/18 District
format on time
NRHM PIP 2009-10: Chhattisgarh
Page 91
In order to achieve these goals, the state has planned various programmatic outcomes that can
lead to this. The indicators have been derived for each of the programmes to measure the
adequacy of processes as well as outcomes. The programme experience under RCH and
NRHM of last three years has been critically looked at and corrective measures adopted
wherever gaps were found to optimise the programme outputs. The current PIP is also
covering the backlog that is left behind of last year, i.e. 2008-09, for whichever activities could
not be initiated or completed. In brief, the activities proposed in the RCH-II PIP are:
Maternal Health
Operationalisation of FRUs
Operationalisation of 200 PHCs to give 24 Hour services through additional staff
nurses provision
Operationalisation of MTP Services in 32 CHCs and 96 PHCs
Operationalisation of RTI/STI Services in 32 CHCs and 96 PHCs
Strengthening Health Sub centres through additional ANMS based on Panchayats,
supportive Supervision, Health Worker Assistance System, Mobility Support for
ANMs with additional workload
Referral Transport Support for Second referrals for institutional deliveries linked with
JSY helpline- one district pilot on referral transport on call
RCH Out-reach camps in difficult areas in non-tribal areas
Monthly Village Health & Nutrition Melas
Janani Suraksha Yojana with JSY Helpline as a supportive mechanism
Special ANC attention for 7 high API districts, also introducing fortified candies to
address anaemia, through ANC kits.
Dai Incentives for helping the ANM in institutional deliveries at sub centre
Child Health:
Accreditation of Child friendly Health Facilities
Integrated Management of Neonatal and Childhood diseases in 3 districts to continue
Facility based newborn care through SNCUs with NNF support
Integrated Biannual Maternal and Child Health Month- Sishu Sanraksaan Maah
Home based New born care in 10 blocks
School Health Programme- Swasth Pathshala Yojana
NRHM PIP 2009-10: Chhattisgarh
Page 92
Infant and Young Child Feeding training in coordination with WCD department
Care for Severely Malnourished Sick Children- Bal Suposhan Yojana to
operationalised facility based Nutritional Rehabilitation in 48 facilities
Introduction of Zinc in management of childhood diarrhoea
Navajat Swagath Bheit By Mitanins- A scheme to ensure Mitanins visit to newborns on
critical early neonatal period in all blocks
Crèches in district hospitals in coordination with WCD department
Family Planning
Plan for better Provision of Family Planning Services
Adolescent Health:
ARSH Facilities in all CHCs including Sakhi/Sakha Kendra (Counselling Centres)
Pilot in life skills education at select schools
Urban RCH
Urban RCH programme in 4 major cities with Urban Health Care Centres, Community
Level Care Givers, Peer Education Programme.
Tribal RCH
RCH outreach camps in tribal areas
Rural Medical Corps as a special initiative under NRHM part B
RCH interventions for Vulnerable
Emergency fund for conflict affected areas
Special infrastructure provision for conflict areas under special initiatives
Maintaining Sex Ratio-
Better Implementation of PNDT Act
Infection Management in facilities
IMEP through Jeevan Deep
Health Management Information System
Data compilation using telephone inter phase equipments and a health worker
assistance put in place
Electronic Document Management system as NRHM special initiatives
NRHM PIP 2009-10: Chhattisgarh
Page 93
BCC programmes for RCH
Implementation of state BCC implementation framework
Implementation of district BCC plans
Training and Capacity Building for RCH
Training on all identified skill gaps related to RCH as well as on capacity building on
professional public health management
Effective RCH Programme Management
Through placing efficient personnel at all level and through technical assistance
A specialised HR agency to take care of HR management
New technical hands wherever it is necessary
The plan has looked at Equity and Gender concerns in detail and it shall explore all scopes for
better convergence, coordination and synergy with other areas wherever necessary. Planning
for better financial management also has been done. District Health Planning has been
initiated in the state for the year and we expect this to complete by the end of March 2009. A
detailed work plan has been prepared for each components of the PIP.
NRHM PIP 2009-10: Chhattisgarh
Page 94
Table 2.4: Budget Summary for RCH
Budget head
RCH II
Qtr
I
Qtr
II
NRHM Others (specify e.g. state budget, 12th Total
finance commission, DPs etc.)
Qtr
III
Qtr
IV
Total
Rs.
1
%
Maternal Health
(a) JSY
(b) Others
Sub total
2
Child Health
3
Family Planning
(a) Sterilisation Compensation
(b) NSV acceptance
(c) Others
Sub total
4
Adolescent Reproductive and Sexual Health
NRHM PIP 2009-10: Chhattisgarh
Page 95
5
Urban RCH
6
Tribal RCH
7
Vulnerable groups
8
Innovations / PPP/ NGO
9
Infrastructure and Human Resources
10 Institutional strengthening (HRD practices,
logistics, M&E/ HMIS, QA)
11 Training
12 BCC/ IEC
13 Procurement
14 Programme management
15 Convergence/Coordination
14. TOTAL
NRHM PIP 2009-10: Chhattisgarh
Page 96
Process of Plan Preparation
A technical group coordinated by the SHRC comprising SIHFW, UNICEF, RRC for RCH
together with the NRHM/RCH Programme Management Unit did initiate the planning process,
which begun in early December 2008. The programme teams of various national programmes
also were part of these processes. Three consultative meetings held as well as rigorous
correspondence and discussions among various stakeholders. At the district level, district level
planning process with rigorous exercises on log frame and presentation coupled with review and
feedback as well as internal evaluation of the programme implementation status was done in
parallel- All these processes has been carried out with the sole purpose of incorporating the
district specific requirement and need. The district action plans are under the final stage of
preparation. These plans will be appraised and finalised by the state soon.
Background and Current Status
A detailed note has been given as part of the introduction of the comprehensive PIP, and as
such, the need for repetition was not felt. This could be viewed at the introductory part of this
document.
Situation Analysis
A detailed situation analysis has been done at page number of the document as part of the
introduction to the comprehensive PIP. This has been documented with the minutest detail
possible to portray the actual and correct status and information.
Progress and Lessons Learnt
A minute and detailed picture on this has been given at page number of the document as part of
the introduction along with the programmes experience in the comprehensive PIP. Progress on
various programme components are given as part of the work plan under each activity. This has
been compiled with much introspection and evaluation.
RCH-II Programme Objectives, Strategies and Activities:
Vision Statement
Chhattisgarh State is committed to a vision of reducing IMR to less than 30, MMR to below 100
and TFR to 2.1 by the year 2012- the end of the 11th five year plans period. These goals will be
attained by a set of processes that empower local communities that are affordable, and provide
equitable access to health care services, that are gender sensitive and that are contributing
directly or indirectly to the reduction of poverty in the state. For this, the state plans major
NRHM PIP 2009-10: Chhattisgarh
Page 97
interventions to strengthen the public health system as well as to improve current health
programmes related to maternal health, child health, family planning, adolescent health, urban
health and tribal health programmes, disease control and disease surveillance.
Technical objectives, strategies and activities under RCH II
Maternal Health
Introduction:
Women constitute half the human resources and thus the economic wealth of the country and if
about half the nation’s human resource is neglected, the overall progress of the country would
obviously be hampered. Recognizing the need for involving women in various development
activities, the Government of India has initiated several affirmative measures to increase
women’s access throughout the life cycle approach to appropriate affordable and quality health
care. In India about 407 women continue to die every year because of pregnancy related causes
mainly due to the Haemorrhage (both ante and post partum), Toxaemia, and Anaemia,
Obstructed labour, Puerperal sepsis and unsafe abortion etc. So there was a critical need to look
women’s health holistically as a sum total of their social environments and lived experiences
towards understanding their health problems Reproductive and Child Health programme was
launched in October 2007 keeping the child Survival and Safe Motherhood as a main component
for intervention.
Objectives
Broad Objectives:
To improve the health status of women, adolescents and children
To improve the quality of health seeking behaviour of women.
To increase the credibility of service providers through improved quality of service.
Specific Objectives:
Reduction of IMR to less than 50 per 1000 live births, and MMR to less than 1 per 1000
pregnancies
Significant reduction in infant morbidity, especially that due to diarrhoea and ARI.
Significant reduction in maternal morbidity
Improved MTP services in all the facilities.
Reduction in incidence of STD and RTI.
Elimination of Female Infanticide.
NRHM PIP 2009-10: Chhattisgarh
Page 98
Interventions
Essential Obstetric Care
Aiming to provide basic emergency obstetric care to pregnant woman, more emphasized has
given to provide at least 3 antenatal checkups during which weight and blood pressure check,
abdominal examination, immunization against tetanus, iron and folic acid prophylaxis, anaemia
management are to be provide to pregnant women at the level of CHC and PHC. To provide
such comprehensive health care at the level of CHCs, PHCs and SCs provision has made to
make then 24 x 7 hr functional by strengthening them with continues supply of drugs in the form
of emergency obstetric drug kits and availability of skilled manpower.
24-Hours Delivery Services at PHCs/CHCs:
To institutional the deliveries, provision has made to provide round the clock delivery services at
PHCs and CHCs. In this contest least one Medical Officer, Nurse, and cleaner will be available
at the institute beyond normal working hours.
Referral Transport:
To provide the timely care for pregnant woman at the time of delivery or during complication,
special provision has been made to provide emergency transport when pregnant a woman
requires it. . To facilitate the scheme provision has been made in selected states to provide a
lump sum corpus fund to Panchayat through District Family Welfare Officers.
Safe Abortion Services:
Efforts are being made to provide the unmet need of safe abortion services, to avoid abortion in
the unauthorized health facility and so as sepsis and other complications and to improve
utilization of existing facilities and further expand the MTP facilities safe abortion service has
made accessible to all women in the country including the women in rural area. So far, Act has
now been amended to delegate the powers to States to the District level through a committee
headed by Chief Medical Officer or District Health Officer.
Multi Skilling Training:
To overcome the scarcity of specialist manpower at the public health facility, MBBS doctors are
promoted for gaining Anaesthetic Skills in Emergency Obstetric Care and Obstetric
Management Skills to conduct the Caesarean Section at the FRU level.
Setting up of Blood Storage Unit:
NRHM PIP 2009-10: Chhattisgarh
Page 99
Timely treatment for complications associated with pregnancy is sometimes hampered due to
non-availability of Blood Transfusion services at FRUs. To facilitate establishment of Blood
Storage Centres at such FRUs the Drugs and Cosmetics Act have been amended and guidelines
for these Blood Storage Centres, have been prepared and disseminated to the States.
Janani Suraksha Yojana
Initially the scheme was launched as National Maternity Benefit Scheme, later on it modified and
name as Janani Suraksha Yojana. The aim to launch this scheme is to institutionalize the
delivery and to make some financial provision to beneficiary so that the obstetric care should not
delay due to financial reason. In the scheme, special package has been designed considering the
referral transportation and cash benefit to beneficiary.
The scheme has its own objective to reduce the Maternal Mortality and Infant Mortality and
Institutionalization of home delivery.
Accredited Social Health Activist (ASHA)
As a new intervention in the health care delivery system, In the National Rural Health Mission
(NRHM) a new community level link worker has been introduced Accredited Social Health
Activists (ASHA). She is expected to act as a link among beneficiary at village level, Anganwadi
Worker and ANM to facilitate health care provision till the last corner of community settlement.
Objectives:
1.
Reduction of MMR from 379 to less than 100 by the year 2012,
2.
An increase of CPR to 70 % by the year 2010.
3.
Reduction of total fertility rate (TFR) to 2.1 and net reproduction rate to 1.0 by the
year 2010.
4.
Reduction of maternal anaemia levels from 63 percent (NFHS III) to 25 percent by
2012.
5.
Making comprehensive and basic emergency obstetric care services, referral
transport as appropriate in all the 24 X 7 PHC and FRU of phase I and phase II.
6.
Addressing the disparities in maternal health services provision through focus to
urban poor, tribal, vulnerable populations and adolescents age groups.
7.
Ensure Better BCC in order to generate adequate awareness at all levels on
maternal health issues.
NRHM PIP 2009-10: Chhattisgarh
Page 100
Strategies:
To improve the overall health situation and to provide comprehensive care to community, there
are several operational activities being undertaken to make health care system more accessible
and affordable to community. Following are the strategies, which will add value to achieve the
stated objective.
1.
Improving Maternal Health Services through setting up comprehensive emergency
obstetric care in select CHCs, Civil Hospitals and District Hospitals by closing all
possible gaps. The major thrust are multi-skill training, 24-hour institutional
delivery with basic emergency Obstetric care in all Sector PHCs and in every CHC
to make it functional.
2.
Provision of safe MTP and Safe abortion services in all CHCs and District hospitals.
3.
Provision of RTI/STI services in selective CHCs and District Hospitals.
4.
Strengthening/ Building up referral transport systems.
5.
Setting up of Blood storage unit in selected First Referral Unit.
6.
Promotion and appointment of contractual staff to breach human resource gap in
health facilities.
7.
Award and reward for good performing and highly motivated staff.
8.
Provision of performance based incentive for best performing institution, health
professional and supportive staff.
9.
Integrated Outreach of RCH Services through RCH camps in tribal and non-tribal
areas.
10.
Village Health and Nutrition Days where ANM, AWW and Mitanins (Community
Health Volunteers) together work for filling the service delivery gaps
11.
Janani Suraksha Yojana for improving institutional delivery and providing maternity
support to poor women.
12.
BCC on Maternal Health, focus for the year on JSY, issues related to anaemia,
undernourishment, pre-age marriage, all available health facilities with focus on
FRU level services.
13.
Training for improving various Maternal Health Services- SBA training, Safe MTP/
abortion services, Short-term specialist skills training to medical officers.
NRHM PIP 2009-10: Chhattisgarh
Page 101
14.
Indemnity insurance for multi skilled doctors.
15.
Integration of local private specialist with CHC to breach the gap of specialist
human resource at the CHC level.
16.
Accreditation of private health facilities.
17.
Reallocation of Multi skilled doctors to rationalised emergency obstetric care in
selected First Referral Unit.
18.
Development / Renovation of health infrastructure at all level of health care
provision.
19.
Decreasing the ‘iron gap’
Achievements of Year 2008-09:
With a view to increase access to quality health care including services in Immunization
and Safe Motherhood, Government of Chhattisgarh has aimed many activities to provide the
comprehensive care at the level of First Referral Unit (FRU). Strengthen the First Referral Unit;
first step was adopted to provide the skilled manpower at every facility. But due to the limited
availability of human resource in state, it was difficult task to accomplish in limited time frame,
Chhattisgarh was first state who adopted the multi skilling program in the state, latter on
Government of India adopted this strategy to breach human resource gap at national level. Until
November 2007, total 96 Medical Officers were trained under multi skilling training programme.
However, at present it is nonfictional due to guideline suggested by Chhattisgarh for the
Multiskilling and guideline from GOI. Soon new batch will start after finalizing the nomination.
To manage Complications associated with pregnancies as close as to community, most
identified FRUs were selected to make fully operational by setting up of blood storage Unit /
transfusion facilities at the first referral units. In the favour of this, special Provision was only
made for 96 FRU to disburse Rs. 5 lakhs each, Against 96 FRUs, state only able to disburse fund
for 18 FRUs and for 79 FRUs fund will be disbursed this year.
In the Development goal of Chhattisgarh, Safe Motherhood and Child Survival is important an
intervention. At the national level it is estimated that at least 80 % of all deliveries should
conducted in institution by the year 2010 and 100 % percent deliveries should be attended by
trained personnel. Against the national norm, Chhattisgarh has improved progressively since the
day of formation, at present total institutional deliveries across the state is 31.71(Table No: 1),
while the Percentages of assisted delivery is 96.69 % (Table No: 2)
Institutional Delivery
NRHM PIP 2009-10: Chhattisgarh
Page 102
Supervised Delivery, Table No: 2
The Essential Obstetric Care that includes antenatal care, institutional safe delivery services and
postnatal care, Chhattisgarh has improved its overall condition. Out of the total target of 697201
for Registration, 417385 cases was registered that means total 59.87 percentage targeted case
was registered and out of that 82.18 percentage have completed their three ante natal check up.
NRHM PIP 2009-10: Chhattisgarh
Page 103
Table 2.5: Status of Institutional delivery
S. no
Districts
Cases Registered: Cumulative up to month- Nov 2008
Completed 3 Checkups: Cumulative up to month- Nov 2008
Target
Achievement
Percentage
ANC Registered
Achievement
Percentage
1
Raipur
100881
63600
63.04
63600
57353
90.18
2
Mahasamund
28838
14790
51.29
14790
13310
89.99
3
Dhamtari
23588
11921
50.54
11921
9830
82.46
4
Durg
93931
47823
50.91
47823
36548
76.42
5
Rajnandgaon
42974
25456
59.24
25456
22417
88.06
6
Kawardha
19601
14153
72.21
14153
11615
82.07
7
Bastar
43659
26796
61.38
26796
24412
91.10
8
Kanker
21836
10893
49.89
10893
8816
80.93
9
Dantewada
24107
12940
53.68
12940
11071
85.56
10
Bilaspur
66818
47035
70.39
47035
30153
64.11
11
Janjgir
44125
27312
61.90
27312
21772
79.72
12
Korba
33932
20218
59.58
20218
16784
83.02
13
Raigarh
42413
23106
54.48
23106
20692
89.55
14
Jashpur
24802
15212
61.33
15212
14064
92.45
15
Sarguja
66068
42578
64.45
42578
33325
78.27
16
Koriya
19628
13552
69.04
13552
10838
79.97
Total
697201
417385
59.87
417385
343000
82.18
NRHM PIP 2009-10: Chhattisgarh
Page 104
In the historical event and first time in the country, District Hospital Korba has certified as first
Public Hospital by ISO 9001:2000 certifications.
The human resource crisis in health care is an important obstacle in Chhattisgarh to attain the
specified health goals. To overcome this scarcity, state has appointed 300 Staff nurses for 96
FRUs, and PHCs to fulfil the criteria of 7 Staff Nurses. Other than this, the lack of adequate
building structures is also being addressed and the gaps in PHC and Sub centre facilities in
these blocks.
Focus for the current year will be to complete the backlog of operationalising all 96 facilities
selected so far. Apart from this, some of the district hospitals that were set up recently also shall
fall into this category. In addition, remaining facilities will be taken up for filling hard gaps in
terms of infrastructure and equipments.
FOGSI
An agreement has been signed between the State Health Society and The Federation of Obstetric
and Gynaecological Societies of India herein referred as FOGSI to develop capacity of the
Medical officers Non-Specialist posted in CHCs upgraded as FRUs in Chhattisgarh to provide
high quality Comprehensive emergency obstetric care services in FRUs. In the coming years, the
responsibility of training of master trainers and medical officers has been entrusted to FOGSI.
The scope of the MoU is to set up 2 Tertiary Care Training Centres in Chhattisgarh that is Pt.
JNM Medical College Raipur and JLN hospital and Research Institute Bhilai and to train 4
Master Trainers from each institution at CMC, Vellore. Along with this, there is a setup of 8
District Training Centre at District Hospitals of Durg, Rajnandgaon, Dhamtari, Korba, Raigarh,
Ambikapur and 2 other hospitals. FOGSI will be responsible for finalizing dates for the training
of the trainers at CMC Vellore. In this process, FOGSI will be responsible for organizing CTS &
MODCAL training to the master trainers. The expected outcome of the training is at least 48
Medical Officers will be trained in one-year batch wise.
Activities for Year 2009 -10:
FRU Operationalisation:
Blood Storage Facility:
To provide comprehensive Obstetric care to promote caesarean section in First Referral Unit, it
is mandatory to have blood transfusion facility in the FRUs. In the year of 2008-09, 18 out of 96
FRUs were able to received Rs. 5 lakh per unit for remaining, for 79 FRUs remaining fund of
Rs.39500000 will be disbursed in this financial year. Therefore, there is no requirement of fund
for this activity.
NRHM PIP 2009-10: Chhattisgarh
Page 105
The inspection, Licensing and Training component for Blood Storage Unit will be coordinate
with CGSACS along with SHRC Technical support.
Multi skilling of the Medical Officers:
Multi skilling training for LSAS: - to overcome the scarcity of specialists at the level of FRU,
Chhattisgarh was first state to start Multi skilling programme. In the previous course of
Multiskilling training, total 94 Doctors was trained and send back to the nominated FRUs. In
those 48 doctors undergone under LSAS, while 46 in EmOC. Mean while the course was nonfunctional because to integrate same new guideline form the Government of India. In the current
year, new batch for multi skilling will be started soon after inviting nomination from the phase
III FRUs. The expected training load is 78 doctors, that 48 will be in EmOC and 30 will be in
LSAS
In the current year Rs. 6300770is requested in this current year in which total 30 medical officer
will trained in LSAS. Similarly the TOT and reference training for medical officer for the earlier
batches will be arrange this year. (The detailed information in training section).
FOGSI:
Multi skilling training for EmOC:-To provide the comprehensive emergency obstetric service in
FRUs to prevent Maternal Mortality MoU has been sign between the State Health Society and
the Federation of Obstetric and Gynaecological Societies of India to develop capacity of the
Medical officers Non-Specialist posted in CHCs upgraded as FRUs in Chhattisgarh.
As per the understanding Rs. 58, 40,546 is to be released to GOGSI, out of the total sum, In first
phase state has released Rs. 46, 73,106 as first instalment for setting up of 2 TCTCs and District
Hospitals training centre, while in the second instalment Rs. 11, 67,440 is to be released this
year from money received last year.
As per the MoU with FOGSI, the next training batch for EmOC will be undertaken by FOGSI.
Indemnity Insurance for the Multi Skilled MOs
The Medical Officers who are trained in Emergency Obstetric Care and Life Saving Anaesthesia
Skills will be covered under Indemnity Insurance. This scheme will protect them to pay any
claim, in unfavourable condition. It is proposed to cover Rs 5, 00,000/ per Multi Skilled doctor.
In the current year, total 48 doctors are expected to be trained in EmOC while 30 doctors in
LSAS.
Table 2.6: Budget estimation for indemnity insurance
S.N.
Unit Description
Unit Cost
NRHM PIP 2009-10: Chhattisgarh
No. of Units
Duration
Total Cost
Page 106
1
Indemnity Insurance
5000
78
1
390000
Total
390000
Staff Appointment:
One of the most critical human resource gap found at the level of CHCs and PHCs is the
availability of Staff Nurses. The state has only 866 staff Nurses for 137 CHCs and 721 PHCs
(Data till 13/5/2008). To operationalise 64 FRUs and 50% PHCs requirement of staff Nurses
against 7 Staff Nurses at CHC and 3 at PHC, this year we are projecting to appoint total 1152
Staff Nurses in 64 CHCs and 24 x7 Running PHCs to make them fully functional . The budget
requirement will be such that 502 staff nurses will be joining from August 2009, therefore the
budget requirement will be for 8 months and the rest 650 budget requirements will be for
12months
Table 2.7: Budget estimation for appointment of staff nurses
S.
N.
Item
Unit Cost
No. of
Units
Duration
Total Cost
1.
Appointment of 502 staff Nurses
7,000
502
8 months
2,81,12,000
2.
Appointment of 650 staff nurses
7000
650
12 months
5,46,00,000
Total
82712000
In case sufficient number of application not available to fill the required position, border will be
open for recognized private Institution from Chhattisgarh and neighbouring states like Madhya
Pradesh Andhra Pradesh, Orissa and Maharashtra.
Incentivisation:
To motivate the staff in the FRUs level, incentives can be a good strategy to recognise their
performance and dedication. In this aspect, this year a new scheme has been proposed to
provide the performance based incentive to the facilities. In this context, annual based incentive
will be given the facilities for their over and above performance. Considering the demographic
challenger the facilities will be dividing in rural area and Tribal area.
At the level of the Sub centre (4741) minimum benchmark is 40 deliveries minimum annually
similarly 65 deliveries max in year, for which Rs. 50 will entitle to the service provider at the
facility level at min and 65 at max deliveries per annum for which no incentive will provide. as
estimated, 25 more deliveries can be
NRHM PIP 2009-10: Chhattisgarh
Page 107
Table 2.8: Budget estimation for providing incentives
Name of the
institution
Location
No. of
Institution
B
Sub centre
C
Rural
Tribal
Rural
Tribal
D
4741
Rural
136 + 18 (
350
civil
250
Dispensary)
146
2000
PHC
CHC
Tribal
Administrative Rural
block Head
(BMO), BPM
Tribal
and others
District
Authority
(CMHO) and
nodal
Grand Total
721
Proposed Annual
Benchmark
Minimum
Estimated
performance
Maximum
performance
E
F
40
65
25
50
250
350
180
280
Estimated
cases no.
for
incentives
Unit
cost
Total cost Eligible staff
(D*G*H) member and
contribution
G
25
25
100
100
H
50
50
100
100
I
5926250
450
100
100
1540000
350
100
100
15000
1500
15000
1. 50-60, 2.
61-75, 3. 76
and above
50000,
35000,
20000.
NRHM PIP 2009-10: Chhattisgarh
7210000
2190000
500000
17366250
Page 108
J
ANM
ANM
25-MO, 25ANM/Staff N.,
50- Class IV
employees
30-MO,30- SN,
40- other
Supportive staff
5000- BMO,
5000-BPM, 5000
other supporting
staff
Operationalisation of 24 hour PHCs
Out of 64 FRU of Phase I and Phase II, total 72 PHCs (District NRHM Reporting) are providing
service on 24x7 and many of on the basses on call service due to unavailability of Staff nurses.
Activities:
Last year advertises was made to fill requirement of 350 staff nurses. Priority was given to
remote area, where the residential areas are at considerable distance. To take forward this
activity Rs. 42000000 was sanction, which will be utilised in the year of 2009-10.
Similarly to meet need Staff nurses in current year, total budget for 350 Staff Nurses is
requested in NRHM PIP 2009–10. In case sufficient number of application not available to fill
the required position, border will be open for recognised private Institution from Chhattisgarh
and neighbouring states like Madhya Pradesh Andhra Pradesh, Orissa and Maharashtra.
In this way, we will be able to place second staff nurse in the facility.
Supply Equipment or maintenances of non-functional equipment will be taken care with help of
Chhattisgarh equipment management cell.
Table 2.9: Budget Estimation for appointment of staff nurses for 24x7 PHC
S.N. Unit Description
1
Unit
Cost
Appointment of Staff Nurses for 360 10,000
PHCs @ 3 /PHC
Total
No.
Units
350
of Duration
12
Total Cost
42000000
42000000
Incentivisation for service providers:
Already covered in incentivisation
Appointment of ANMs:
As NRHM is sanctioning 2 ANMs per sub centre, thus the second ANM can be appointed district
Panchayat the activity forward remaining budget of Rs. 36840000 will be utilized for in this
year. Similarly, in current year total 1500 second ANM (Assistant ANM) are projected to be
recruited and trained. The Budget can be drawn from NRHM Flexi-pool. The detail can be seen
in the part B of this PIP.
As per the new suggestion for the appointment of 2nd, the priority will be given to or position
will be filled where the Male health worker is available.
NRHM PIP 2009-10: Chhattisgarh
Page 109
Training of ANMs on Skilled Attendance at Birth:
This has been dealt in detail in the training Chapter
Incentives for ANMs:
Already covered in incentivisation
Janani Suraksha Yojana:
High rates of maternal mortality have been recognized as a major public health problem in
Chhattisgarh. Maternal mortality ratio is as high as 379 per 100,000 live births (SRS 2005)
which when compared to 110 per 100,000 live births in Kerala: reveal the true contrast, as well
as, seriousness of the problem.
The table below highlights the contrast in other key indicators as well.
Table 2.10 Comparative performance of Chhattisgarh in RCH indicators
Sr. No.
Indicators
1
Maternal Morality Ratio
100,000 live births)
2
Chhattisgarh
Kerala
Source of data
110
SRS 2005
Infant Mortality Rate (per 1000 59
live births)
14
SRS
data
(Report Oct – 2008 )
3
Proportion of infant deaths that 21.3
contribute to total deaths
3.4
SRS 2005
4
Neonatal
mortality
(per 1000 live births)
rate 36
11
SRS 2005
5
Early Neonatal date rate
36
09
SRS 2005
6
Institutional deliveries
18.1
99.4
DLHS 3
(per 379
Thus promoting institutional deliveries saves many maternal and infant lives. At 2001 2002 the
institutional delivery rate in rural Chhattisgarh was as low as 7.5%, now it is improving, and
according to NFHS 3, it is 18.1 slowly progressive. JSY came in role almost 2006, after which
NRHM PIP 2009-10: Chhattisgarh
Page 110
institutional deliveries starting increasing timely it is improving. Thus, many newborns have
little chance for specialized care when it is most needed for their survival.
Progress so far:
Following data are showing the trend of JSY in Chhattisgarh was improving progressively till
2007-08 if we compare last three year data. In year 2006-2007, the institutional deliveries were
131334 in year 2007-2008 was 120500 and now in 2008 -09 it was 115266. Although we have
achieve only 31.77 % institutional delivery in year 2008-2009.but we need to improving the IEC
of JSY and via strengthening the payment of incentive to the beneficiaries and motivators as well.
Table 2.11: Impact of JSY
S. no.
Districts
Institutional Delivery
Supervised Delivery
1
Raipur
Cumulative Up to Month- Nov 2008
Total
Achievement Percentage
Deliveries
50966
14295
28.05
Cumulative Up to Month- Nov 2008
Total
Achievement Percentage
Deliveries
50966
45471
89.22
2
Mahasamund
12616
6169
48.90
12616
12603
99.90
3
Dhamtari
9819
4420
45.01
9819
9595
97.72
4
Durg
40923
18300
44.72
40923
40662
99.36
5
Rajnandgaon
23032
6653
28.89
23032
22932
99.57
6
Kawardha
13257
2231
16.83
13257
13105
98.85
7
Bastar
23879
9627
40.32
23879
22970
96.19
8
Kanker
10037
3375
33.63
10037
10037
100.00
9
Dantewada
12013
3193
26.58
12013
9586
79.80
10
Bilaspur
40379
10168
25.18
40379
37126
91.94
11
Janjgir
22383
3579
15.99
22383
21127
94.39
12
Korba
17593
4846
27.55
17593
16827
95.65
13
Raigarh
19914
7305
36.68
19914
19141
96.12
14
Jashpur
14159
4315
30.48
14159
13089
92.44
15
Sarguja
39645
11904
30.03
39645
37774
95.28
16
Koriya
12186
4886
40.10
12186
11483
94.23
Total
362801
115266
31.77
362801
343528
94.69
NRHM PIP 2009-10: Chhattisgarh
Page 111
Interventions:
Addressing first delay:
A team ANM, AWW and Mitanin contacts families of pregnant women in
their work area and assist them preparing for childbirth. The team members provide antenatal
check-up (8/8) throughout the pregnancy and give them a small birth plan kit. The kit is opened
in front of the family and contents explained in detail. The team also counsels on danger signs,
and need to arrange money, transport and blood. They are also informed about the Helpline.
Birth-plan is kept with the family, and a copy is maintained by the workers.
Birth preparedness:
Addressing second delay:
This is, in a way, will be the heart of the program. In Chhattisgarh, the
physical distances between services and women in need of reproductive health care are
considerable, and the vehicles are either not accessible at times of emergency, or even when
available, are expensive.
Organizing transport:
To promote rapid referral in times of emergency, helpline maps the resources in every village,
sub centre, PHC, CHC and hospital in the district, listing ambulances and willing vehicle and
phone numbers. The birth plan includes these provisions, as well as, contact details of the owner
of vehicle to use in case of emergencies.
In case of the non-availability of a local vehicle, the family is urged to call up the Helpline,
which will be manned by a facilitator in Raipur, 24 hrs a day, 7 days a week. Helpline number,
which will be provided, needs to be given wide publicity.
The facilitator, using the network of field workers, ambulances and vehicle owners (who are
telephonically connected to each other) arranges the nearest ambulance or vehicle. The
transport cost will be borne by the JSY scheme.
Addressing third delay:
One of the strongest elements of
the intervention is supporting the families when they reach the hospital, many a times, forcing
the system to deliver. The helpline facilitator also informs the nearest health care facility of
arrival of pregnant woman in labour to arrange for necessary obstetric care. At times, the
Mitanin helpdesk in hospitals will also be informed of such referral.
Negotiating with the health system to ensure timely attendance:
Table 2.12: Budget for JSY support for pregnant women
Unit
Unit
cost
NRHM PIP 2009-10: Chhattisgarh
No. of units
Duration
Total
Page 112
Support for home delivery
500
60000
1
3,00,00,000
Support
for
delivery(urban)
institutional 1200
100000
1
12,00,00,000
Support
for
delivery(Rural)
institutional 2000
200000
1
40,00,00,000
360000
1
55,00,00,000
Total
4 % of total requirement for JSY administrative/IEC and cost
2,20,00,000
Total including 4 % of total requirement for JSY administrative/IEC and cost 57,20,00,000
Referral Transport Linkages
Chhattisgarh, the physical distances between health institutions and women in need of
reproductive health care is not considerable. The vehicles for transportation of patient are either
not available during emergency or even when available are too expensive for the poor families.
There is a provision of financial support under JSY for self-referral and transportation from
home to Sub Centre/ PHC/CHC. Nevertheless, some of the cases are referred to higher centre, as
it cannot be managed at those centres. Most of the time the funds available under JSY get
exhausted at the time of first referral and no funds are available for subsequent referral to
higher centres which is usually quite far and the pregnant mother and their relatives have to
manage from their own source.
Strategy:
To promote rapid referral in times of emergency, JSY helpline will be established in the state
(details are given in the next section on JSY). This helpline will start after all the resource form
the Sub centre to PHCs, CHCs and District hospital of particular District. Micro planning will
be done based on micro plan of birth form every village and all the information will provide to
the call centre.
In case of the non-availability of a local vehicle, the family is urged to call up the Helpline,
which will be manned by a facilitator in Raipur, 24 hrs a day, 7 days a week. Helpline numbers
will be given wide publicity.
The facilitator, using the network of field workers, ambulances and vehicle owners (who are
telephonically connected to each other) arranges the nearest ambulance or vehicle. The
transport cost will be borne by the JSY scheme.
NRHM PIP 2009-10: Chhattisgarh
Page 113
Out of the total number of institutional deliveries taking place under JSY, 10% of the deliveries
will fall under the category where the expecting mother might be referred to higher centres. For
these cases, additional funds will be made available at the PHC and CHC to be utilized for
second referral. In year 300000 expected number of JSY cases is around 30000 that is 10 % of
total are expecting for second referral. To rationalise the reimbursement for beneficiaries, the
criteria for reimbursement will be done based on distance between the two referral health
facilities and operational guideline to be issued to the district. In an average cost for second
referral transport is estimated approximately Rs. 750, its will be varied. In case it is needed, the
first referral assistance can be raised from Rs.250 and above as required. For that the amount
proposed in second referral may be partially utilized to compensate the need concern medical
officer will take decision based on the distance from the residence to the PHC/CHC to
compensate the extra amount needed
The fund will be issued to the districts which have highest number of referrals and will
replenished after the district gives 90% utilization of the fund given in each quarter. The project
will take up from April 2009 onwards.
Table 2.13: Budget for JSY referral support
JSY institutional Deliveries 10% of JSY institutional Deliveries Rs
750
for
expected in 2009-10
considered as deliveries required second second referral
referral
300000
30000
22500000
Accreditation of private Facilities:
The private sector accounts for a substantial proportion of healthcare in India (50 per cent of
inpatient care and 60-70 per cent of outpatient care) and so has plays a crucial role in Indian
healthcare system. Consequently, the private healthcare delivery system in India has remained
largely fragmented and uncontrolled, Even in Chhattisgarh it is not different from the national
picture. In the recent years, Chhattisgarh has come up with many models to collaborate with
Private health care to widening the pan of health care service and provide health care vicinity
where community can access when they needed. Taking forward this innovation, Government
has planned to accredited private health facility for JSY Scheme under the NRHM.
In this scheme, the private facility will be identified according to availability of level of basic
emergency obstetric care and comprehensive care. Selection will be done on the basics of
certain decided criteria’s – like for basics obstetric care there should be at least MBBS doctor
or BAMS from recognized institute with support of trained Mid wife / Nurse / Staff Nurse along
with a availability of basic supportive infrastructure like delivery table, basic emergency
equipments, facility for new born resuscitation and proper referral service in case of any
NRHM PIP 2009-10: Chhattisgarh
Page 114
complication. Similarly, for comprehensive obstetric care there should be a facility of LSCS
(Caesarean section), Gynaecologist, paediatrician and Anaesthetist (full time/ on call basis)
along with facility for blood transfusion, laboratory service, basic emergency drug, facility for
communication and proper referral in case of emergency.
Initially under this scheme, pregnant woman for BPL families, rural areas and from urban BPL
will be eligible. For the better functioning on the scheme and documentation of the cases , for
each case Rs. 100 will be paid to respective accredited facility for documentation and reporting
after submission of proper document to respective BMO/CMHO.
No separate budget has been proposed for this activity. The requirement will be met through the
administrative cost of JSY.
New Intervention- JSY Helpline: Extending Help to the deserved:
This activity of last year has not yet taken off. Hence, recently there was a visit of a team
comprising of officials States NRHM, SHRC and UNICEF to Guna district of Madhya Pradesh
to study the effectively operated ‘call centre’ by the Government. As part of the learning, the
earlier plan of establishing the call centre at the State level will not be taken up. However, the
district level call centres will be established in 7 districts where the rural institutional deliveries
are less than that of state average of 13.1 percent (DLHS 2007 – 08). These districts are
Kawardha, Bilaspur, Durg, Rajnandgaon, Koriya, Kanker and Korba. To facilitate the process a
‘JSY call centre coordinator’ will be appointed in the Maternal and Child Survival Cell of RCH
wing of the directorate through UNICEF support. The national medical emergency telephone
number ‘102’ will be activated in these districts for JSY helpline and given wide publicity. To
promote rapid referral in times of emergency, helpline maps the resources in every village, sub
centre, PHC, CHC and hospital in the district, listing ambulances and willing vehicle and phone
numbers. The birth plan includes these provisions, as well as, contact details of the owner of
vehicle to use in case of emergencies. In case of the non-availability of a local vehicle, the family
is urged to call up the Helpline, which will be manned by a facilitator in Raipur, 24 hrs a day, 7
days a week. The facilitator at the call centre, using the network of field workers, ambulances
and vehicle owners (who are telephonically connected to each other) arranges the nearest
ambulance or vehicle. The transport cost will be borne by the JSY scheme.
Table 2.14: Budget for JSY Helpline
S. no.
Budget head
Calculation
Total
Reimburse to JSY Help line @ of Rs 5 per call for 4 Rs 5 *400000
lakhs calls
2000000
Monitoring cost of the responses
40000
NRHM PIP 2009-10: Chhattisgarh
2% of the total cost
Page 115
2040000
Total
Application for JSY beneficiaries:
Aiming the proper documentation and tracking mechanism for monitoring of JSY scheme this
year state has planned to launch an innovative scheme for the JSY beneficiaries. Now all the
beneficiaries have to fill an application to avail JSY benefit under the scheme. This printed
format will be available with the ANM, AWW, and Panchayat institute and soon with the
accredited private facility too. The beneficiaries need to fill the form and send back to the facility
where they are availing service for the delivery.
A cash coupon will be provided along with the application form, by which beneficiaries and
Mitanin can be reimburse the benefit after producing to the respective facility in case Public
Institution , while accredited facility in case of private facility. The time lines to encash this
coupon will be three month from the day of delivery conducted, in case the time line over, the
cash coupon will automatically cancelled. Mitanin will only reimburse the cash, if she stayed in
hospital. In any case, any member from Mitanin family accompany to beneficiaries to refer in
Public Hospital or accredited private facility, Mitanin will be eligible to get reimbursement
from the same cash coupon.
In the initial phase, only beneficiaries for the rural area, BPL Families, and beneficiaries from
urban BPL will be entitles for scheme.
New initiative:
1. Special ANC Clinic in difficult area.
2. Develop software/web based monitoring &evaluation cell at state and district level
under HMIS.
Maternal and infant death auditing committee:
For Maternal and Infant Death auditing, an Auditing Committee needs to be formed and to be in
place. This shall be at the state and at the district level. These committee members at the state
shall comprise of the JSY Nodal (State) and The State Immunization Nodal Officer and their
assistants. At the district level, the members shall consist of JSY Nodal Officer, the DIO, and
their assistants.
The main components for auditing will be of the following:
1. ANC registration
2. ANC Check up
NRHM PIP 2009-10: Chhattisgarh
Page 116
3. Delivery auditing ( Enquire about care received during deliveries)
4. Post partum care, complication
5. BCG Vaccination
6. Probable cause of maternal and infant death
The strategy for review mechanism at the district level could be done quarterly to resolve the
problem at hand. Further, the necessary documentation and dissemination of the reports to the
respective stakeholders would be made available on time for reference and record. The budget
for the auditing process could be availed from the administrative contingency cost of JSY. The
budget requirement for the quarterly meeting at the districts could be as follows:
Rs. 200 per head (Logistic support and refreshment). Total Number of Participants expected for
the meeting consisting of all the stakeholders is 50 at the state as well district. At the state level,
total 4meeting will conduct similarly 72 meeting in district. Therefore, cost of meeting expenses
for all this meetings will be Rs.760000 only.
The budget requisition will be met through the administrative budget head.
Chiranjeevi Yojana
Replication of the Chiranjeevi schemes is being adopted approved by the Governing Board of
NRHM Chhattisgarh, at the present it is planned to replicate this model in Raipur, Durg and
Bilaspur.
Under this scheme, health department has to accreditate private institutions for service delivery
especially for the maternal health .the institutions or gynaecologists and obstetricians, who
provide cashless services, promoting institutional deliveries to all women. The interested doctors
have to sign a memorandum of understanding with the district health authorities. Awareness
about the scheme will be generated in the communities by the authorities, involving Field Health
Workers, Auxiliary Nurse Midwives, Village Heads and even Traditional Birth Attendants. A
broad monitoring scheme has to establish for the proper monitoring of this schemes
The empanelled doctors may conduct the deliveries in their own set-ups or government set-ups.
The department can make a payment of 179500 for a batch of 100 deliveries. This payment takes
care of both normal and complicated labours. It also covers an incentive of Rs.50 for the Dai,
accompanying the enceinte and Rs.200 as transport cost (see annexure 1 for details).
NRHM PIP 2009-10: Chhattisgarh
Page 117
Expected Outcomes
1. Decrease in maternal mortality ratio
2. Decrease in infant mortality rate
3. A significant increase in rate of institutional deliveries
4. Reduction in rate of caesarean deliveries, ascribed to inherent cost structure of the
scheme that discourages unnecessary caesarean deliveries.
This scheme will be replicated in all districts of the state. The Gujarat Model will be adopted for
launching of this scheme. The selection criteria for this scheme will be those institutions that are
performing more than 50 deliveries per month. The budget estimate cost of accreditation of this
scheme for one institution per month is 179500.
Additional administrative cost of 5% of the total budget is 2692500. The administrative cost
will be borne under JSY administrative cost. The target for cases is 15000 @ Rs. 2000
Table 2.15: Budget estimation for Chiranjeevi Scheme
Sl.
No.
Budget Head
Duration Total cost
(month)
1
15000 Cases @ Rs. 2000
12
Total
3,00,00,000
3,00,00,000
Reducing the ‘iron gap’ - improving distribution and compliance of IFA tablets among
pregnant women to control maternal anaemia
The Government of India’s National Nutritional Anaemia Control Program aims at decreasing
the prevalence of anaemia in women in the reproductive age group, especially pregnant and
lactating women, children 6 to 60 months and adolescent girls. The program focuses on
provision of Iron and Folic Acid (IFA) in the form of tablets to these “high risk groups.”
In Chhattisgarh, 63 percent pregnant women are anaemic which is higher than the national
average and the maternal mortality is 379 per 100000 live births. As per SRS, 42% maternal
deaths in India are due to bleeding. These deaths can be averted to some extent if there are
enough iron reserves in the pregnant women. However, in Chhattisgarh as per CES 2006, only
37 percent of pregnant women received adequate IFA tablets and as per DLHS 2007 – 09 only
21 percent consumed adequate IFA tablets. Hence, controlling maternal anaemia by ensuring
NRHM PIP 2009-10: Chhattisgarh
Page 118
distribution and compliance of IFA tablets among pregnant women will go long way in
improvement in maternal health and contribute in reduction of maternal mortality. As per the
practise of village health and nutrition days, tablet IFA is distributed during the immunization
session. It is proposed to monitor the availability and consumption of IFA, provide monitoring
feedback to the department to enable corrective actions.
Implementation Strategy:
There are four Divisional Consultants of Micronutrient Initiative (MI) and Child In Need
Institute (CINI) in the State, who are currently supporting the Vitamin A programme. The
support of these consultants will be extended to monitoring IFA distribution and
compliance.
In 2009-10, this activity can be implemented in four districts comprising of each
divisional headquarter namely Bastar, Bilaspur, Raipur and Sarguja. The criteria of
selection of the districts are in accordance with the existing placement of MI-CINI’s four
Consultants/extenders who are based at divisional headquartering. It is also estimated
that 42 percent of pregnant women in the State are from these four districts.
The DOHFW, CG will ensure timely and adequate supply of IFA (large) tablets.
The Micronutrient Initiative will support in Training of Health Workers and Supervisors,
IEC and social mobilization activities focusing especially on the compliance of IFA
tablets, monitoring, ensuring distribution management from district to field level,
enhancing monitoring through Health Supervisors and improving existing record keeping
and reporting etc.
UNICEF will undertake joint monitoring with MI and will analyze monitoring results.
Provide monitoring feedback jointly to the district and state level health authorities.
Quarterly review meeting at districts and state level will be held.
Broad Area of Activities for improving distribution and compliance of IFA tablets among
pregnant mothers in 4 districts:
Training of Health Workers and Supervisors
Timely and adequate supply of IFA (large) tablets to the districts
Development of communication strategy and print of IEC materials
Development and Printing of Training modules
NRHM PIP 2009-10: Chhattisgarh
Page 119
Field level Monitoring
Field level monitoring by Health Supervisors by using monitoring checklists
Provide monitoring feedback to the district and state level health authorities
Quarterly review meeting at districts and state level
Identification of Nodal officers at state, district, and block levels in Health
Ensuring distribution management from district to field level
Table 2.16: Annual IFA (large) tablet requirement in 4 districts:
Name of Approximate
the
no.
of
District Pregnant
Women in a
year
Approximate
no. of Pregnant
Women
who
are
Anaemic
(@ 63% as per
NFHS-III
No. of IFA
(large) Tablets
for
Pregnant
Women @ 100
tablets
per
woman
(who
are
non
anaemic)
including 10%
wastage
No. of IFA
(large) Tablets
for
Pregnant
Women @ 200
tablets
per
woman who are
anaemic
(including 10%
wastage)
Total
IFA
(large)
tablets to be
required in a
year
Bastar
44423
27986
18,08,070
61,56,920
79,64,990
Bilaspur
76629
48276
31,18,830
1,06,20,720
1,37,39,550
Raipur
98758
62217
40,19,510
1,36,87,740
1,77,07,250
Sarguja
75862
47793
30,87,590
1,05,14,460
1,36,02,050
Total
2,95,672
1,86,272
1,20,34,000
4,09,79,840
5,30,13,840
Budget Estimate:
The supply of IFA (large) will be met through DOHFW and MI will extend all programmatic
support including the use of consultants for this activity. To implement this project, MI would
support approximately to the tune of Rs. 40 lakhs towards programs and monitoring costs of its
consultants. Budget is not required from NRHM.
NRHM PIP 2009-10: Chhattisgarh
Page 120
Other Strategies on Maternal Health- ANC kits for pregnant women in disease-prone
areas:
As per CES 2006, only 37 percent pregnant women in Chhattisgarh receive their entitlement of
100 IFA tablets. Hence, as per NFHS-III, the state has 63 percent pregnant women suffering
from anaemia leading to high maternal mortality. In addition, Chhattisgarh stands 2nd, after
Orissa in terms of malaria problem in the country. In eleven districts API and Plasmodium
Falciparum Proportion is more than 5 and 75 percent respectively. It is well known that malaria
contributes to maternal mortality. As per the study by Sarah Barnett et al measuring maternal
mortality in indigenous population of Orissa and Jharkhand (Biomed journal, February 2008)
haemorrhage was the primary cause of death for a quarter of maternal deaths (25%); closely
followed by malaria (23%); and sepsis (17%). Malaria was the most common cause of death
during the ante-partum period (48%); haemorrhage during the intra-partum period (39%); and
sepsis during the post-partum period (35%). Secondary causes were also identified from the
verbal autopsies. Anaemia was a key underlying factor in 35% of deaths. Malaria (22) and
Sepsis (20) were also highlighted as key underlying causes.
To address the situation, all sub centres in high malaria districts will be given an ANC kit for the
pregnant women who are registered in sub centre for institutional deliveries. The kit will be
given by ANM on the day she is registered as expectant mother. The ANC kit will consist of a
family type long lasting bed net (net size for 4 person), 100 large IFA tablets, integrated ‘Jachha
Bachha Raksha’ Card, a one page brochure encouraging institutional deliveries. With
information on nearest health facilities, broachers on care, precaution, and diets. The
approximate cost of a bed nets, Tab IFA, Jachha Bachha Raksha card will be around 300 per to
Kit. UNICEF will prepare the kit and individual items will be supplied by the state. The
distribution of the kit will be confined to 9 districts where the API index is very high and
morbidity and mortality due to malaria has direct impact on pregnant women. The districts are
Dantewada, Bijapur, Bastar, Narayanpur, Kanker, Jashpur, Koriya, Raigarh and Sarguja.
The budget requirement for this component will be met through the budgeted component of bed
nets distribution.
Preventing Post partum Haemorrhage in rural areas in institutional settings:
As per the study by Sarah Barnett et al measuring maternal mortality in indigenous population
of Orissa and Jharkhand (Biomed journal, February 2008), 28 percent of all deaths occurred at
facility where 15.4 percent of them were due to haemorrhage. These deaths are easily
preventable by administering three tablets of Misoprostol 200 micrograms to each woman
immediately after delivery. It is proposed in 2009 – 10 to introduce Misoprostol in Chhattisgarh
to all districts for deliveries (except for that of district hospital where oxytocin is readily
available). One-day training will be imparted to ANMs on use of Misoprostol and its benefits.
NRHM PIP 2009-10: Chhattisgarh
Page 121
However, given the current rural institutional delivery rate in Chhattisgarh of only 13 percent
(DLHS 2007 – 08), it is estimated that 68000 deliveries per year happen in institutional settings.
Thus, 204000 Misoprostol 200-microgram tablets will be required per year.
Table 2.17: Budget estimation for preventing PPH
S.N. Unit Description
Unit
Cost
1
Cost of Tablet
micrograms)
Misoprostol
2
One day orientation to ANMs
(200 12
Total
--
No.
Units
of Duration
Total Cost
204000
1
2448000
5000
1
-2448000
Procurement of RTI/ STI kits:
Presence of STI/ RTI increases the risk of acquiring HIV/AIDS infection by 8% to 10%.
Therefore, management of STI infections is a significant component of the National AIDS
Control Programme. As per the reports received from 6 out of 17 NACO supported STI clinics in
the state, 558 episodes have been treated in these clinics. Training of trainers for the
participants identified as State supervisory team from 3 medical colleges has been conducted.
Training of Medical officers, staff nurses and lab technicians from NACO supported as well as
NRHM supported clinics is planned to be held in the month of February and March 2009.
Table 2.18: Coverage Targets for STI (STD Clinics)
NRHM PIP 2009-10: Chhattisgarh
Page 122
S.No
District
Category
Population Projection
for 2009 (based o
Census 2001)
Sexually
Active
Population (50 % of
Population)
Population
prone for risky
behaviour
STI Target 33% of
Population
prone
for risky behaviour
NACO
33% STI
Target
NRHM
67% STI
Target
1
Bastar
C
1492694
746347
22390
7389
2438
4951
2
Bilaspur
C
2273503
1136751
34103
11254
3714
7540
3
Dantewada
C
808574
404287
12129
4002
1321
2682
4
Dhamtari
C
814564
407282
12218
4032
1331
2702
5
Durg
A
3180106
1590053
47702
15742
5195
10547
6
Janjgir
D
1511455
755728
22672
7482
2469
5013
7
Jashpur
C
815001
407500
12225
4034
1331
2703
8
Kanker
D
749502
374751
11243
3710
1224
2486
9
Kawardha
C
649495
324747
9742
3215
1061
2154
10
Korba
C
1194708
597354
17921
5914
1952
3962
11
Koriya
D
664655
332328
9970
3290
1086
2204
12
Mahasamund
D
920182
460091
13803
4555
1503
3052
13
Raigarh
C
1454138
727069
21812
7198
2375
4823
14
Raipur
C
3465694
1732847
51985
17155
5661
11494
15
Rajnandgaon
D
1463315
731658
21950
7243
2390
4853
16
Surguja
D
2358172
1179086
35373
11673
3852
7821
23815759.11
11907880
357236
117888
38903
78985
State Total
NRHM PIP 2009-10: Chhattisgarh
Page 123
Table 2.19: budget estimation for STI/RTI kits
Kit
Requirement
Unit Cost
Amount
KIT 1
4873
20
97460
Kit2
95967
20
1919336
Kit3
10663
20
213260
Kit4
1
20
16
Kit5
10663
20
213260
Kit6
1422
20
28435
Kit7
158
20
3159
RPR (50 Test per kit)
2607
300
782100
TPH (50Test per kit)
79
1500
118500
Grand Total
3375540
Table 2.20: budget estimation for STI/RTI kits summarized
S.N.
Unit Description
Unit Cost
No. of Units
Duration
Total Cost
1
STI/ RTI drug kit
20
123747
1
2474940
2
RPR (50 Test per kit)
300
2607
1
782100
3
TPH (50Test per kit)
1500
79
1
118500
Total
3375540
Family Planning:
Objectives:
1. To achieve better contraceptive prevalence rate of 65, TFR of 2.1 and reducing the birth rate
of the state.
2. To improve health services in order to meet the family planning needs at community level.
NRHM PIP 2009-10: Chhattisgarh
Page 124
3. To ensure provision of family planning services at the convenience of people who need them.
4. To ensure adequate training to the service providers at various levels in order to ensure
better service provision, maintaining quality standards and satisfying the clientele
5. To increase the male participation in family welfare activities.
Table 2.21: couple protection status
Activity
Achievement
CPR-Any modern method
49.1
CPR- limiting methods
53.2
CPR-Oral Pills
1.4
CPR-IUDs
0.8
CPR-Condoms
2.9
Unmet needs, spacing methods
10.5
Unmet needs, terminal
5.4
*Source: NFHS- 3
Table 2.22: progress status of sterilisation performance
Total
Sterilization
Vasectomy
Performed
Total
NSVT
VT
Total
CTT
LTT
2002-03
115298
2862
1060
1802
112436
32447
79989
2003-04
115848
3242
2301
941
112606
31860
80746
2004-05
124478
3788
2851
937
120690
35906
84784
2005-06
124499
6699
5653
1046
117800
37957
79843
2006-07
133094
6322
5276
1046
126772
39347
87425
2007-08
153836
9920
8397
1523
143916
44981
98935
--
3914
1071
--
--
--
Year
2008-09
187879
( Till Nov08)
Tubectomy
In order to improve the situation, the state has planned the following strategies:
NRHM PIP 2009-10: Chhattisgarh
Page 125
Strategies:
Promotion of Terminal and limiting methods mainly focus on NSV and CTT,
through fixed day services in peripheries and regular services at district level
Coordinated family planning activity with reputed private providers.
Improving utility of spacing methods by widening IUD use and social marketing of
contraceptives.
Provision of terminal sterilization services in district hospital on daily bases.
Functional CHCs to provide sterilization on a fixed day of the week.
Strengthening the block CHCs and 16 district hospitals to capable of providing safe
MTP services.
Proper referral services in CHCs and District hospitals for timely diagnostics and
referral in case of STI/RTI services.
In three months of the year all the remaining blocks would have at least three
sterilization days in their CHCs, and by the end of the year 2009-10, we will be able
to change to fixed-day weekly-once service availability.
Every village would have one social marketing outlet, which would have supplies of
condoms and OCPs without interruption throughout the year. These would be
managed by partnership with a private distributor network with subsidy to make it
viable to operate in low off take areas.
All PHCs would have one fixed-day of the week where IUD insertion would be
available and other contraceptive follow up would be encouraged. Emergency
contraception would also be available on 24-hour basis.
All 24-hour paramedical and medical staff would be trained to provide basic clinical and
counselling services for RTI and STI with basic investigations (side laboratory level).
Every hamlet would have at least two volunteers who would have a limited stock of the supplies
available- collected either from the village distribution point or from the health department.
These volunteers will get incentives for motivating people.
Social marketing for OCPs and condoms along with other health related commodities
A focused IEC campaign to build up demand for these services, especially for NSVT.
NRHM PIP 2009-10: Chhattisgarh
Page 126
Training of personnel in essential skills on providing better family planning
services, at all levels- on laparoscopic sterilisation, minilap, NSV and IUD insertion
as well on contraceptive update- in order to keep to the quality norms and
regulations at service provision.
Activities:
Fixed Day Male Sterilisation Services in select 32 CHCs in first half of the year and
expansion of the same into another 32 in the second half.
Fixed Day Female Sterilisation Services in select 32 CHCs in first half of the year
and expansion of the same into another 32 in the second half.
Male Sterilisation Camps in all Districts and blocks, as they are organised regularly.
Female Sterilisation Camps in all Districts and blocks, as they are organised
regularly.
Promotion of Spacing methods through BCC and social marketing.
IUD Promotion through public health system as well as Private facilities and training
of CHC/PHC doctors on 380A manikin IUD insertion.
Mitanin to act as a contraceptive depot holder and provide supplied goods as
required by the people.
Training activity for all ANM in alternative methodology for CuT Insertion.
Private Partnership on Family Planning Process
The private providers at state will be involved in promotion of IUD 380 A in the state.
Advertisement for Expression of Interest will be called from private providers who after
inspection by quality assurance cell of the district then accredited by state Government to
provide 380 A IUD to public free of cost, but the incentive of Rs 20 instead of user, shall be paid
to the provider here. The private provider will be given free supply of 380 A and Rs 75 per
beneficiaries. The private providers will give full detail of the beneficiary to be crosschecked by
the district authority. The advertisement cost will be taken for IEC cost allocated to the Districts.
Such providers shall be identified at least 2 per blocks and 5 per district headquarter.
Budget Estimation:
This is covering only the essential family planning measures, not the entire activities planned.
For rest of the activities, appropriate budget heads shall be used to pool necessary allocation.
NRHM PIP 2009-10: Chhattisgarh
Page 127
Table 2.23: Budget estimation for public private initiatives in family planning
Budget Head
Unit
Wages compensation for Female Sterilization Per Beneficiary
beneficiaries
Wages Compensation for Male Sterilization Per Beneficiary
beneficiaries
NSV camps
IUD incentive
Facilities No. of Unit Cost
units
Public
170000
1000
Duration
Total
1
170000000
Private
20000
1000
1
20000000
Public
10000
1500
1
15000000
700
1500
1
1050000
13714000
118000
20
1
2360000
12000
75
1
900000
12
1000000
1
12000000
Private
As per the detailed Camp
budget below
Per Beneficiaries
Public
Private
Annual maintenance of laparoscopic machine in District
the district where machine and surgeons are
available
Grand Total
NRHM PIP 2009-10: Chhattisgarh
235024000
Page 128
Table 2.24: Budget estimation for maintenances of OT and Instrument
Sr. No
Unit Description
No. of Unit
Unit Cost
Duration
Total Cost
1.
Maintenances of OT and Instrument
-
-
1
1000000
Total
1000000
Table 2.25: Budget estimation for Procurement of family planning Kit
Sr. No
Unit Description
No. of Unit
Unit Cost
Duration
Total Cost
1.
NSV Instrument
1000
750
1
750000
Total
750000
Establishment of State Family Welfare Bureau:
The State Family Welfare Bureau is proposed to functioning at State Head quarter Raipur as an
administrative Unit for implementation of Family Welfare programme in all districts of the State.
The Major Services under this head will be implementation of population Policies and
Programmes of the State Government and MCH and FW services extended to Adolescent health
care services, treatment of RTI & STI. The State Family Welfare Bureau will coordinate to
District Family Welfare officer and Chief Medical Health Officer for implementation and
administration of activity at the local level.
Budget Estimation:
Only Public Health expert (post) budget in programme management
Adolescent Reproductive Sexual Health in Chhattisgarh
Even if adolescent comprise 22% of the total population of the state, majority of them are still
left out to avail qualitative health services including counselling and essential treatment from the
state. There has been direct correlation between the awareness generation on adolescent health
and reduction in maternal mortality, infant mortality, morbidity rate, malnutrition, and
population control, reduction in high-risk behaviour and reduction in teenage pregnancy. For
this focus has been given on adolescent health under RCH-2.
The health status of the women in state is alarming and needs immediate attention and address.
Indicators like percentage of women suffering from anaemia (57.5%), percentage of women who
were married at 18yrs or above are only 50.5% and total percentage of population suffering
NRHM PIP 2009-10: Chhattisgarh
Page 129
from sickle cell anaemia in the state is 18% (carriers 15% and diseased 1.2 %) are showing
negative trends and demoralizing picture.
We all know that use of services by adolescent is limited. Poor knowledge and lack of awareness
are the main underlying factors. Service provision for adolescent is influenced by many factors.
For example, at the level of the health system, lack of adequate privacy and confidentiality skills,
are barriers that limit access to services. Shortcoming in their professional trainings often
results in service providers being unable and sometimes unwilling to deal with adolescent in an
effective manner.
In context of the Reproductive and Child health (RCH) programme goals, with special reference
to the reduction of IMR, MMR and TFR, addressing adolescent in the programme framework
will yield dividends in terms of delaying age of marriage, reducing incidence of teenage
pregnancy, prevention and management of obstetric complications including access for early
and safe abortion services and reduction of unsafe sexual behaviour.
Objectives: -
To improve the health awareness in the adolescent age group on personal hygiene,
nutrition, anaemia, sexual and reproductive, RTI and STI, health services etc.
To make the adolescent health care facilities as well as safe abortion services accessible
to handle the problems of unsafe adolescent pregnancies and management of
reproductive tract infections easily accessible to all.
To identify and reduce anaemia among adolescents.
To reduce malnutrition and anaemia amongst adolescent's especially adolescent girls.
To increase the awareness regarding pitfalls of early marriage and child bearing,
regarding family planning and nutritional requirements of adolescents.
To Increase awareness of one’s own body (physical, psychological and reproductive
health etc) and control over it – including fertility control and safe sexual practices.
To provide easily accessible and friendly health care services and counselling for
adolescents.
Strategies:
1. ARSH services to be made available in all facilities in a phased manner.
2. Major effort to screen for and manage anaemia and malnutrition in adolescence and
where relevant for sickle cell anaemia. (Activities for this will be done under a separate
component)
NRHM PIP 2009-10: Chhattisgarh
Page 130
3. Distribution of IFA tablets and deworming tables in schools under school education
program to manage anaemia in defined adolescent age group. (First phase in
government school)(Budget for this will be booked under Sickle cell Anaemia Budget)
4. Higher secondary school based adolescent health education initiatives by building a
local cadre of trained students on life kill education. Awareness on contraceptives
methods to enable well informed choices
5. Counselling and peer education programmes in haat bazaar through ARSH counselling
centres (Sakhi /Sakha Kendra) as well as counselling of the family members of the
adolescent age group.
6. Filling the skill gaps in health personnel for Adolescent Reproductive Sexual Health
(ARSH) and other adolescent health interventions through rigorous training.
7. BCC interventions on adolescent health issues, through regular media and interventions
by Mitanins.
8. Social marketing of sanitary napkins and other adolescent health friendly goods.
9. Intersectoral convergence with the ICDS and Education department
Activities:
1. Training of peer educators will be conducted by using the available training force.
2. Mother NGOs of the area will be involved in community outreach programs to
disseminate information to adolescents in groups through various methods including
sports events and film shows in villages. Vocational training institutes and other
adolescent hangouts will also be targeted for activities by NGOs to maximize the chances
of having an interface with the school adolescents.
3. Sakhi/Sakha Kendras: Staff of selected CHCs preferably will be trained on adolescent
and reproductive health issues to counsel adolescents. The purpose behind this is to
organize ARSH Clinics (Sakhi/sakha- Kendras) in the identified haat bazaar (markets) of
the villages at the block level. In the initial phase, at least one session per month would
be organized by ARSH Clinics (Sakhi/sakha Kendra.) lady health visitor to will be the
focal coordination person for this activity. Their responsibilities would be to look after
mobilization part and the functionality of these clinics in coordination with the ICDS,
AWW. The activities of these ARSH Clinics would be counselling and peer education with
the help of lady visitor on the haat bazaar day at the block level. One of the major roles
of the LHV is to organize meeting at the hamlet level with the support ANM of Mitanins
and AWW trainers to screen out the cases related with reproductive and sexual health.
NRHM PIP 2009-10: Chhattisgarh
Page 131
The purpose of organizing the screening at the hamlet level is to provide an opportunity
to them to alleviate their doubts and queries related with the issues and seek for a proper
address to it. Operationalisation of these Kendras will be collectively done by CHC
staffs, Mitanins Trainers and Mitanins. Operationalisation of Sakhi/sakha Kendra will
be done in two phases: o Phase 1 (In initial two to three months): - Awareness generation on personal
hygiene (adolescent growth and development, menstruation and making of
sanitary napkins at local level), counselling and distribution of IFA tablets for
anaemia, treatment and counselling on contagious disease like itching, answering
the queries of adolescent girls, distribution of deworming tablets, awareness on
DOTS under T.B control programme.
o Phase 2(After the completion of first phase): -Treatment and counselling on
reproductive health, immunisation of the identified left out adolescent girls,
treatment and counselling on premature pregnancy and complications during
delivery and pregnancy.
4. Training of adolescent group in schools on life skill education. The purpose behind this is
to create master trainers at the state level, which in future will serve as a resource force
to build local level cadre on adolescent reproductive sexual health (ARSH). In the initial
phase, the program will be implemented on a pilot basis. We will initiate the activities in
4 government schools of two districts. Priority will be given to take up the tribal districts
in the initial phase (Sarguja and Jagadalpur). Four batches of 15 girls each from four
schools will be trained on life skill education to tackle the problems of adolescent health.
Training of these batches will be done by state level resource persons (4 resource
persons at the state level). On an average, these trainers will be involved for 20 days in a
month to trains the batches in the schools .The capacity building of these resource
persons will be done by SIHFW. Later on as the program progresses, it will include
trainings of adolescent boys too. In the next phase of implementation, the focus will be to
take this program forward at the block level. The state nodal officer will be identified.
The program shall work under the supervision of the Director of Health Services,
Chhattisgarh.
5. Adequate support to be provided for mobilisation and success of Camps organized by
women and child development department under Kishori Shakti Scheme and by Red
Cross/DHS under sickle cell control programme. The latter will be organized to do the
screening of adolescents for anaemia. All adolescent girls will be targeted for this
activity. ANM will be sensitised to ensure the complete coverage. This approach will
address the problem of iron deficiency and prevent sickle cell anaemia. The role of
NRHM PIP 2009-10: Chhattisgarh
Page 132
counsellors, apart from counselling will be to help the adolescents referred to the PHC
/CHC for lab testing and drugs dispensing.
6. IEC campaign through print and mass media to reinstate messages of postponing
childbearing and marriage age and to focus on nutritional needs of the adolescent group,
will lead to the improvement of the status of malnutrition and postpone the age of
marriage.
7. Counsellors trained in 2006/07 and 2008 shall conduct counselling of the adolescents
once a month in the Govt PHC/CHC/Urban Health Centre. Along with this the focus will
also be given on family counselling of members of adolescent age group
8. “Kishori Samuh” formed in each village needs to be strengthened through refresher
training. Required coordination shall be done with ICDS and Education department.
9. Distribution of IFA tablets in schools (DOTS) to manage the anaemia level in adolescent
age group.
10. Coordination with various departments and programme on similar issues.
In the initial phase of the programme, it has been decided to implement Sakhi/Sakha Kendras in
12 districts (Bastar, Kanker, Dantewada, Kawardha, Koriya, Jashpur, Korba, Raipur, Sarguja,
Narayanpur, Bijapur, and Raigarh) of the state.
Activities to take up Sakhi/Sakha Kendras are as follows
Identification and preparation of the list of villages where weekly markets (haat bazaar)
are held. Along with this preparation of the list of ICDS workers, female teachers and
LHV, ANM, and mitanin trainer.
Framing of the guidelines, preparation of training module and budget for the
operationalisation of ‘Sakhi treatment and counselling centres”
One day training of the supervisors, LHV, selected ANMs Mitanin trainers and female
teachers before operationalising “Sakhi treatment and counselling centres” in the
selected districts
To initiate the “Sakhi treatment and counselling centres” in the first phase of the
programme in the blocks of Kanker and Bastar districts
No additional budget has been proposed for this component. The activities financial requirement will be met
through other related budget source.
NRHM PIP 2009-10: Chhattisgarh
Page 133
Implementation of PNDT Act
Current Situation:
The programme implementation as of now needs gearing up in the state- the steering committee
meeting was held and it has decided to have a multidimensional focus on the issue and to move
forward.
Appropriate bodies at district and block levels formed, meetings needs to be regularized
and their capacities need to be enhanced
Mass awareness Programmes through various electronic/print/visual media as well as
through electricity and telephone bills/percolated messages done.
The media like government post card envelop, inland, electricity bills will have printed
slogans on PNDT and a film on PNDT will be used for generating public awareness.
Orientation for various organizations like NGO, development bodies, government
officials have been taken up.
NGO support and participation needs to be expanded.
Strategies:
To ensure NGO support in 4 regions for rapid identification of cases- in the case such
NGOs are not available, allocation of this sum CMHOs to undertake the above tasks
themselves
Support for coordinating functions at Directorate of Health Services to organize
sensitization program at District and Block Level personnel. The sensitization will be on
following topics
o Present scenario of PNDT Act,
o Different records and its maintenance under PNDT Act
o Provision of punitive action, the concerned authority and its power
o Creation of a committee and its responsibility
o Coordination with other enforcing department
Activities:
Regular meetings, monitoring and follow up of the appropriate bodies
NRHM PIP 2009-10: Chhattisgarh
Page 134
Active verification of adherence to norm by registered facility, finding out non-registered
service providers, if any
NGO support in 4 regions for rapid identification of cases- to implement last year’s
component
Support for coordinating functions at Directorate of Health Services
No extra budget requirement is proposed for the current financial year, as the previous year’s budget will be
utilized for meeting the expenses required.
Training:
Following training programmes will be conducted this year.
Maternal Health:
This training was started in Chhattisgarh as a strategy to address the huge gap of skilled
manpower in 2004-05. The MBBS doctors were trained on certain specialist skills in way that
They are able to provide comprehensive obstetrical care. After completion of this course, many
FRUS were started conducting caesarean section. At present 12 FRUs are performing
caesarean and other yet to be start. Taking forward the training component, FOGSI is
undertaking the responsibility of training MOs in Emergency Obstetric Care and Emergency
Anaesthesia will be undertaken by the state. Till date 48 MO’s has already completed their
training in LSAS and this year 30 MO’s will be trained in two batches of 15 trainees each batch
approximately at the three training institutes.
Additionally a refresher training of previously trained MO’s in CmOC will be conducted and
budget provision have also been proposed for Tier III examination of previously trained 49
MO’s.
Table 2.26: Budget estimation for TOT of Master Trainers (Recurring cost)
Description
No of unit
Unit cost
Duration
Total cost
Trainers of Medical College and District
Hospital ( Travel cost + Accommodation +
Food + Training material etc)
26
2000
2 day
104000
National level facilitator (TA +
Accommodation + Food etc
2
12500
2 day
50000
Total
NRHM PIP 2009-10: Chhattisgarh
154000
Page 135
Table 2.27: Budget estimation for Training
Description
No of Unit
Unit cost
Duration
Course on Anaesthesia at Tertiary Care
Training Centres - 4 months
30
200/day
126 days
Course on sick Neonatal and Sick Child
at Tertiary Care Training Centres –
month 1
30
200/day
30
Posting in District Hospital –month
30
200/day
30
TA for candidates
30
500
1 time
Accommodation * ( 5 + 1 months for 2
batches )
3
10000
12 months
Books
30
2000
I time
Total
756000
180000
180000
15000
360000
60000
Table 2.28: Budget estimation for honorarium of teaching faculty
Honorarium for teaching faculty
No of unit
Course on Anaesthesia - 108 days6days/week *18 weeks/ batch*2
batches at Tertiary Care Training
Centres
3 Inst x
faculty
District Hospital Trainers 26days6days/week *1week/ batch*2
batches at Tertiary Care Training
Centres
3 Trainers *
6 Institution
Course on Sick Neonatal and Sick
Child - at Tertiary Care Training
Centres 26days- 6days/week
*1week/ batch*2 batches at
Tertiary Care Training Centres
3 Inst x
faculty
Refreshment (Lunch and tea at
TCTC and Dist Hospital for
participants)To be provided by
3 Inst x
30
NRHM PIP 2009-10: Chhattisgarh
Unit cost
Duration
Total cost
216
1620000
300
52
280800
5 500
52
390000
156working
days
468000
5 500
100 / day
Page 136
Institutions
participants
Consumable for LSAS training for
2 batches at Tertiary Care
Training Centres
3 Institution
100000
1 time
300000
Consumable for Paediatrics
training at Tertiary Care Training
Centres
3 Institution
50000
1 time
150000
Total of II
3208800
1551000
Total of I
Total Of I & II 4759800
Other expenses and contingency @
10 %
-
-
-
475980
Total
5235780
Note: - * days calculated based on 6 days / week for 18 Weeks.
Table 2.29: Budget estimation for training of medical officer trained in earlier batches
Description
No of unit
Unit cost
Duration
Total
LSAS - DA
49
200/day
30 days
294000
Accommodation
3
10000
2 month
60000
TA for candidates
49
500
1 time cost
24500
Trainers fee
4weeks *3
Institutions* 5
Faculties
500
26 working
days
195000
Refreshment (Lunch and tea
at TCTC and Dist Hospital
for participants)To be
provided by Institutions to the
participants
3 Inst x
(49
participants
100/day
26 working
days
127400
NRHM PIP 2009-10: Chhattisgarh
Page 137
Other expenses and
contingency @ 10 %
-
-
Total
700900
-
70090
Total
770990
Table 2.30: Budget estimation Tier three examinations for LSAS
Description
Examination
cost for 2 batch
Duration
Total
Tier three examination for LSAS for current batch
60000
3 days
60000
Tier three examination for LSAS for earlier batches
80000
5 days
80000
TOTAL
140000
Budget is also being proposed for providing institutional support to three training institutes
i.e. (1)JNM Medical College , Raipur ,(2) JLN Hospital and Research Centre, Bhilai and (3)
Chhattisgarh Institute of Medical Sciences, Bilaspur for Up gradation of Anaesthesia Centres &
Paediatric centres. An amount of Rs. 10 lakhs @ each district hospital for Korba, Rajnandgaon,
.Durg, Dhamtari, Sarguja, and Raigarh is proposed for centre up gradation this year.
Table 2.31: Budget estimation for Institutional support
Description
No. of
Unit
Unit cost
Duration
Total
Up gradation of Anaesthesia Centre at
tertiary care training centres
3
500000
1
1500000
Up gradation of Paediatrics Centre at
tertiary care training centres
3
500000
1
1500000
Mannequins paediatrics
3
200000
Centre up gradation for EmOC Centre
at tertiary care training centres
2
500000
1
1000000
Centre up gradation of District Hospital
6
500000
1
3000000
Total
NRHM PIP 2009-10: Chhattisgarh
600000
7600000
Page 138
Table 2.32: Budget estimation for training and institutional support summarized
Description
Unit cost
Grand total
Training component
6300770
13900770
Institutional support
7600000
Family planning:
Training on NSV to medical officers in order to establish fixed day services in facilities:
this shall be done by 12 nationally trained master trainers in 12 districts, and at least 120
medical officers shall be trained on this by the end of the year.
Training of CHC level MOs on Minilaprotomy in order to establish fixed day sterilisation
services: this shall be integrated with the multi skilling training of EmOC; the same MO
trained on EmOC shall be given additional one-month training on this.
Adolescent Health:
Training on ARSH for medical officers shall be given to the same doctors doing training
on EmOC FRU.
Training on running Sakhi /Sakha Kendra (Adolescent Counselling Centres) one LHV
and one male worker from all CHCs shall be trained under this. SIHFW shall conduct the
ToT and rest of the training at districts.
Laparoscopic sterilization training (LTT)
The scarcity if LTT surgeon is the limiting factor in providing Family Planning services. To
address this, 15 days training of 20 doctors will be arranged. This training will be conducted in
state LTT training centre and district hospital Bilaspur
Table 2.33: Budget estimation for training of doctors on LTT
Sl. No
Unit Description
1
Training of Doctors on LTT 25000
@ 3MOs/Batch
Total
NRHM PIP 2009-10: Chhattisgarh
Unit cost
No.
Units
10
Of Duration
1
Total Cost
250000
250000
Page 139
Table 2.34: Budget estimation for training on alternative method for IUCD Insertion for ANM and
LHVs:
Sr. No Unit Description
1.
No. Of. Unit
Duration
Alternative method for IUCD 5140 ANMs, 749 LHVs,350 1
Insertion for ANM and LHVs staff nurses
Total Cost
12000000
Total
12000000
Table 2.35: Budget estimation for sensitizing workshop for district training personal
S.
No
Unit Description
Unit
Cost
No.
Unit
1.
Sensitizing workshop for TOT + logistic
1000
48
Of. Duration Total
Cost
1
Total ( Round Up )
50000
50000
TOT for district level trainers at state level:
A TOT will give to the district level trainers at the state level, 8 people will be selected from each
district and will be trained for CNA activity at the block level training.
For the block level training, budget of Rs. 3 thousand is requested for training material printing
and for organising one-day training program.
Table 2.36: Budget estimation for TOT for district level trainers at state level:
Sr. No
Unit Description
Unit Cost
1.
One day training + Printing of 5000
training material
Total
NRHM PIP 2009-10: Chhattisgarh
No.
Unit
146
Of. Duration
1
Total
Cost
730000
730000
Page 140
Other Training Proposal from SIHFW: (Details annexed)
S.No.
Activity
Outcome / Objective
Outlay (INR
in Lacs)
Remarks if Any
1.1 Training Execution
32 Training Programmes over
more than 200 training days
1.2 Development of Training
Materials
Indegenous / Procured Study
Material for Critical Training
Modules (Development ,
Translation , Review , Printing and
Publishing)
1.3 Integrated Training Management
Manual Development by
professional HR agency in
collaboration with SIHHFW
Integrated and standardized
solution for training organising ,
would also help DTCs
3.290
1.4 Procurement of Video Lessons
and Learning Documentaries on
Public Health Issues
Availability of interesting and
effective training tools in form of
Avs on various areas.
5.000
1.5 Untied Allocations : Provision for
Unforeseen activities necessary
at the time of execution
Contingencies met with , without
disturbing the process flow on
account of unplanned expenses.
5.000 These allocations would require
special permission from a special
committee formed for deciding on
matters of qualification under this
head.
COMPONENT TOTAL (A)
85.476 Please see Annexure No. 1,
Comprehensive Training Plan/
CTP for Year 2009-10
20.000 SIHFW may empanel experts and
bodies for developing the
materials or may procure with
modifications provided by the
content creating organisation.
118.766
Comments
NRHM PIP 2009-10: Chhattisgarh
Page 141
Child Health
Objectives:
1. Reduction of infant mortality rate from the current 59 per 1000 live births (SRS 2007) to less
than 30 by the year 2012.
2. Reduction of under five child mortality rate from the current 81 per 1000 live births
(estimation as per SRS 2005) to less than 40 by the year 2012.
3. Reduction of child anaemia levels from the current 81% (NFHS III) to 25% by the year 2012.
4. At least 80% under five-year-old children sleep under an insecticide treated bed net.
Strategies:
1. At least 80% of newborns will be started on breastfeed within one hour of birth.
2. At least 80% newborns will be assessed by an IMNCI trained personnel to access for
danger signs and ensure prompt referral where indicated.
3. Reduce neonatal deaths in referral units by making Sick New Born Care Unit
operational in 7 district hospitals.
4. 100% measles vaccination coverage by strengthening sub centre level services and its
supervision. (This would be addressed in immunization PIP)
5. At least 80% children eligible receive appropriate dose of Vitamin A and deworming
through a bi-annual approach.
6. Ensure institutional care to treat severe acute malnutrition cases
7. At least 75% diarrhoea cases receive appropriate treatment through ORS and Zinc
therapy.
8. Ensure bi-annual systematic impregnation of bed nets.
9. Ensure effective implementation and monitoring of child health services provision by
establishing Maternal and Child Survival Cell.
10. Ensure community awareness on critical child health issues through planned BCC
interventions.
11. Ensure better penetration and impact of health services, in school-going children.
12. Addressing disparities in child health services outreach services, through special
strategies for difficult areas, urban and tribal areas.
13. Training to fill skill gaps in each of these areas
NRHM PIP 2009-10: Chhattisgarh
Page 142
Activities:
In order to achieve the above objectives the state will undertake a two-prong approach:
1. Community and home based approach (Mitanin programme and HBNC separately
mentioned elsewhere in the document)
2. Health Facility based approach
Under the Community based approach, the Navajat Swagath Bheit and Home based Newborn
Care through Mitanins will raise awareness on newborn care and empower families as well as
communities to take timely, appropriate action when things go wrong during neonatal period
preventing many neonatal deaths. Similarly, the Sishu Sanraksaan Maah twice a year will
improve the access of RCH services to deprived communities in remote rural areas enhancing
child survival.
The Health Facility based approach through operationalising Newborn Corners, Stabilization
Units, Special Newborn Care Units, accreditation of health institutions based on child friendly
practices like promotion of breast feeding, immunisation and correct case management of
Several acute Malnutrition, providing essential newborn to all newborns in 24x 7 hour PHCs
will complement the demand generation created through the community based approach.
The Health Facility based approach will focus on ensuring quality standards in all government
facilities so that clients reaching these health institutions are not let down. To ensure this a State
Task Force for Child Friendly Health Facility will be set up in Chhattisgarh. This Task Force
comprising of Dept of Family Welfare, SHRC, UNICEF, BPNI etc will constitute every year,
an Accreditation Committee of renowned professionals to visit, assess and certify the “Child
Friendly” status of that Health Facility based on erstwhile BFHI assessment criteria using
standard assessment tools and formats.
Child Friendly Health Facility Accreditation:
The initiation of breastfeeding within one hour of birth is 50 percent in Chhattisgarh (DLHS
2007 - 08). Now, as institutional deliveries are increasing in district hospitals due to Janani
Suraksha Yojana, we have increasing newborns who are taking birth in a captive environment.
The last year’s PIP activity of written breastfeeding policy boards and infant and Milk Substitute
act boards at facility levels and neonatal assessment case forms and registers have been initiated
recently. It is expected that this would streamline the routine care at birth to some extent. Also
paediatricians and staff nurses from six district hospitals have been trained on infant and young
child feeding practises. The accreditation of district hospitals is still remaining and would be
taken up this year through the newly formed BPNI in the state of Chhattisgarh. The accreditation
will be coordinated by RCH wing jointly with UNICEF.
NRHM PIP 2009-10: Chhattisgarh
Page 143
No additional budget is required for this activity this year and the approved budget of 2008 – 09
of Rs. 29, 15,000 is carried forward this year.
Integrated Management of Neonatal and Childhood Illnesses (IMNCI) practice in
institutional delivery
75 percent of infant deaths occur in neonates in Chhattisgarh (SRS 2007). Now, as institutional
deliveries are increasing due to Janani Suraksha Yojana, we have increasing newborns who are
taking birth in health institutions. Till now, all 62,000 Mitanins (AHSA) are trained in IMNCI
through the support from NRHM and UNICEF. Training of Medical Officers in IMNCI has been
initiated recently by SIHFW through the Child Survival Cell, which is established with support
from UNICEF. This year, the newly GoI approved FIMNCI package of 11 days training will be
used for training all Medical Officers of PHCs, CHCs and District Hospitals – which will be
coordinated through the Child Survival Cell of SIHFW. These training will be organised in close
collaboration with 1) Pt. J N M Medical College, Raipur, 2) Bastar Medical College and 3)
Bilaspur Medical College. In the state the Paediatrics Dept of Pt J N M Medical College will
synchronise training of Medical Officers and Dept of PSM of Pt J N M Medical College will
coordinate training of ANMs.
This year the IMNCI programme activities will be launch across the state and the major
activities will be training of doctors, distributions of assessment forms for the mitanins and
provisions of referrals. The training will be conducted for medical officers of 24X7 PHCs, CHCs
and District Hospitals (paediatric ward and maternity ward) - therefore total number to be
trained will be 400. There will be 17 batches of training consisting of 26 doctors per batch. The
revised RCH training financial norms from GoI vide letter no D.O. No. A-110033/101/2007 –
Training dated 20 October 2008 will be adopted for these training. UNICEF will provide the
training material.
Table 2.37: Budget estimate as per the revised RCH rates of GoI:
S.No.
Particulars / Activities
Unit cost (In Rs)
No of units
Duration
Total for
one batch
(Rs)
1
TA(Trainees)
1000
26
1
26000
2
TA(Facilitators)
1000
8
1
8000
3
DA(trainees)
120
26
11
34320
4
DA(Honorarium of
Facilitators)
1000
8
11
88000
NRHM PIP 2009-10: Chhattisgarh
Page 144
5
Lunch, snacks, tea
200
32
11
70400
6
Venue hiring
10000
1
11
110000
7
TV and DVD player hiring
1000
3
11
33000
8
Organizational expenses
(photocopying, writing
materials, flip charts,
certificates, LCD etc)
250
26
11
71500
9
Banners (flex+cloth)
800
1
1
800
10
Photography and
documentation
350
1
11
3850
Total
11
Institutional overheads
445870
15% of total
66880
Total for one batch
5,12,750
Grand total for 17 batches
87,16,750
Facility Based Newborn Care (FBNC)
The state with collaboration with UNICEF and NNF has already initiated establishment of Sick
Newborn Care Units for Rajnandgaon, Raipur, Durg, Raigarh and Bastar. Again, this year, in
collaboration with UNICEF and NNF an assessment of current facilities is already done for
Koriya, Korba, Bilaspur and Dhamtari district hospitals. The microplans are prepared
accordingly, which include architectural outlay of the unit, equipments, manpower mapping, and
bridging the capacity gaps.
Operational strategies:
An estimate of requirements in terms of number of neonatal beds and equipments is already
done jointly by Office of Civil Surgeon of the District, Office of Chief Medical and Health
Officer of the District, UNICEF and NNF.
As per the requirement, renovation of the existing infrastructure is necessary in each of
district level facility.
There are certain equipments that already exist with each of the facility in working condition.
However, these provide rudimentary care. Additional general equipments, equipments for
NRHM PIP 2009-10: Chhattisgarh
Page 145
individual patient care and side laboratory are required. The detail is already planned by
CS, CMHO, UNICEF and NNF:
Training of medical staff and para – medicals will be done by UNICEF with their resources
– which are not budgeted in this PIP.
Table 2.38: Budget estimate for FBNC
Sl.
No
Unit
District
Description Hospital, Koriya
District
Hospital, Korba
District Hospital, District Hospital,
Dhamtari
Bilaspur
1
Renovation
Rs. 19,00,000
Rs. 20,00,000
Rs. 25,00,000
Rs. 20,00,000
2
Equipments Rs. 20,00,000
Rs. 20,00,000
Rs. 20,00,000
Rs. 20,00,000
Grand Total
Rs. 1,64,00,000
In addition, contractual staff will be appointed in the SNCUs of Rajnandgaon, Raigarh, Bastar
and Durg (first phase SNCUs) with fixed remuneration per month. The staff for each unit will
consist of a paediatrician, and six staff nurses (50 percent requirement of staff nurses). Rest of
the staff for each unit i.e. two MBBS doctors and six staff nurses will be managed from the
hospital pool. This is with reference to the initiation of the SNCUs in the districts after first
phase, it is estimated that the renovation and equipment purchase will take about 6-8 months
time. SNCUs will be initiated as soon as renovation and equipment purchase is over. In addition,
the remuneration of these four SNCUs for second phase will be proposed and budgeted in the
next financial PIP. The HR requirement will be met through regular appointment process.
Integrated bi – annual maternal and child health month (Sishu Sanraksaan Maah)
Chhattisgarh has been implementing a bi – annual health and nutrition months known in ‘Sishu
Sanraksaan Maah’ in the months of April and October. Five such rounds have been conducted in
October 2006, April 2007, October 2007, April 2008 and October 2008. These rounds are also
in conformation to the recommendations of National Workshop on Micronutrients organized by
ICMR on the 24-25 November 2003. The workshop recommended that Biannual Child Health
and Nutrition Promotion Months be held, six months apart. It would offer a package of child
health and nutrition services comprising of Vitamin A supplementation, deworming and bi –
annual systematic impregnation of bed net. The rounds are based on the globally known REACH
strategy i.e. Regular Events to Advanced Child Health which focuses on providing contact points
for delivery of child friendly health services to pre-school children. The integrated approach is
also in conformity to the Village Health and Nutrition Day guidelines issued by MoHFW, GoI.
The package of services given is as follows:
NRHM PIP 2009-10: Chhattisgarh
Page 146
1. Administration of Vitamin A to eligible children aged 9 months to 5 years age to children
who had not received Vit. A in the past 6 months in a bi – annual approach as per the
guidelines of MoHFW, GoI (bi-annual activity)
2. Administration of vaccines to eligible beneficiaries– focusing on never or partially
vaccinated.
3. Deworming of children aged 1 to 5 years age (bi-annual activity)
4. Providing iron folic acid tablet to all pregnant women and eligible children as per the
recommendation from Secretary Health and Family Welfare, MoHFW, GoI (D.O No. Z.
28020/82/2006-ZH dated 25th November 2006)
5. Systematic bi – annual impregnation of bed nets in high malaria districts of Dantewada,
Bijapur, Bastar, Narayanpur, Kanker, Koriya, Sarguja, Raigarh and Jashpur (bi-annual
activity)
6. Salt testing at the household of pregnant women for iodine content in October only.
As seen, those essential services are covered in these months that need to have a bi-annual
approach. In addition, those services are covered that have poor coverage in the State.
For the last rounds, UNICEF has been supplying Vitamin A solutions, gap filling of Tablet
Albendazole and developing training manuals, operational guidelines and IEC materials. The
Micronutrient Initiative has been assisting the State in printing the manuals, guidelines and IEC
materials. UNICEF and MI also had been monitoring the rounds. One State level Technical
Consultant and four Divisional Consultants have been providing all the facilitative support to
this initiative.
In the last round of October 2008, the coverage with Vitamin A was 78 percent and improvement
from the 68 percent coverage in the earlier rounds. In addition, the deworming coverage was 64
percent in October 2008, an improvement from 41 percent coverage in April 2008. It is
documented that more number of pregnant women benefit from Sishu Sanraksaan Maah in the
two systematic rounds. The session cancellation rate has gone down from 33% to 15%.
Operational strategy
Vitamin A and Tablet Albendazole will be procured and supplied at least one month before
the rounds.
Every ANM will be oriented for half a day on the activity one month before the round.
A beneficiary wise list will be prepared by the ANM before the round, in close coordination
with AWW and Mitanins.
NRHM PIP 2009-10: Chhattisgarh
Page 147
There will be strengthening of routine immunization microplans as all the services will be
delivered in the routine immunization sessions, which are on Tuesdays. For any additional
habitation, same services will be delivered on Fridays.
ANM will administer Vitamin A and immunizations and provide Tab IFA and Tab
Albendazole to eligible beneficiaries.
The Malaria link volunteer or the Male Health Worker will impregnate the bed nets with
2.5% Deltamethrin solution that is supplied by the malaria dept.
Special recording and reporting forms are developed integrating with the current reporting
forms, on which the health workers report.
Banners and posters designed by UNICEF in close coordination with the RCH wing
(DoHFW) and MI will be printed and supplied to the district. There are 35,000 session sites
in the state in these special months. Two posters and one banner per session site will be
printed and supplied.
Additional mobility support will be provided to ANMs for covering 16000 session sites that
are hard to reach. Also, as coverage of essential package of services for child health are
poor in urban areas, special session will be organised in these areas by deploying ANMs
working in rural areas to the urban areas on special days – where all the package of services
will be delivered. These urban sessions are 1200 in number.
A social mobilization campaign will be run in the State in this month covering the print and
electronic media that gives message of provision of essential maternal and child health
services in these months.
UNICEF and MI monitor the rounds and provide feedback to the dept to enable corrective
actions
The following support will be from partners for the April and October 2009 rounds:
Micronutrient Initiative:
1. Print operational guidelines, formats for micro planning, record keeping, tally sheets,
monitoring and bi annual strategy registers (Vitamin A and deworming).
2. Support in district and block level workshops, taskforce meetings and press conference
3. Support in inauguration of the SSM at state and district levels
4. Urban area mobilization through rickshaw raths, miking, FM radio, cable television etc
NRHM PIP 2009-10: Chhattisgarh
Page 148
5. Social mobilization through involvement of local NGOs, wall writing, handbills, banners,
posters etc
6. Improving service delivery in 27 high-risk blocks of the state through special local level
innovative strategies.
7. Award to best performing supervisors and health workers.
UNICEF:
1. Supply of Vitamin A and albendazole (50 percent supply)
2. Developing operational guidelines, prototype of banners, posters
3. Monitoring in close collaboration with Micronutrient Initiative.
Table 2.39: Budget estimate for Sishu Sanraksaan Maah
Sr. Unit Description
No
Unit cost
No.
Units
1
Tab IFA (adult)
7.50
400000
1
30,00,000
2
Syrup IFA
(small)
16,00,000
1
2,40,00,000
3
Social Mobilization Activities 500000
like
News
Paper
Advertisements during the
month
2 times in a 2
month
10,00,000
4
TV Spots
500000
30 days
2
1000000
5
Mobility
support
for 5000
monitoring by district and block
block health officials
district
per 146+18
+
2
16,40,000
6
Urban service delivery
18
2
9,00,000
100
ml/bottle 15.00
25000
Total for one round
NRHM PIP 2009-10: Chhattisgarh
Of Duration
Total Cost
3,15,40,000
Page 149
School Health Programme- “Swasth Pathshala Yojana”
Introduction:
For the past several years, any school health program has been viewed as only school health
services like caring for cuts and some common illness, immunization campaigns & improving the
mid-day meal scheme. Though, these are important components, a comprehensive package that
will create educated healthy citizens is the need of the hour. Healthy bodies will ignite healthy
and creative minds that would be an asset to the state.
In Chhattisgarh, we have proxy data from preschool children that indicates the poor health
status of schoolchildren. As per NFHS III, anaemia in children amongst 6 to 35 months age is 81
percent. 52.1 percent children (under 3 years age) are underweight for their age. 45.4 percent
children (under 3 years age) are stunted i.e. almost every second child is chronically
undernourished. 18 percent of under 3 years children are wasted (too thin for height). Malaria is
one of the main causes of long absenteeism amongst schoolchildren. This could be prevented if
facilities are provided to impregnate bed nets and mass counsel on use of bed net for malaria
prevention.
The Swasth Pathshala Scheme is considered to be in higher priority under RCH/NRHM where
the state government has proposed to take up complete screening of higher secondary and high
school students in the state. This will be organized on a biannual basis and coordinated by a
School Health Coordinator under the RCH unit (Maternal and Child Survival Cell to be
established by UNICEF). The interventions for Swasth Pathshala Yojana are the following:
Primary, middle and secondary schools:
1. It is estimated that there are 6 lakhs children in middle school and 5 lakhs in secondary
school. Iron Folic Acid – Directly Observed Supplementation to all schoolchildren of
middle and secondary schools. This activity will be carried out weekly on Thursdays.
Thursdays will be declared as Iron days (Loh divas) and Iron tablet will be administered
on the spot after prayers by the teachers. Bi – annual deworming in all children attending
primary, middle and secondary schools
2. Capacity building in teachers for detecting common ailments, administering first aid,
delivering messages and demonstrating hand washing and personal hygiene.
3. Bi –annual testing of salt for iodine content. Creating awareness on consumption of
iodised salt.
4. Bi – annual impregnation of bed nets
NRHM PIP 2009-10: Chhattisgarh
Page 150
Middle schools:
1. Annual examination for common ailments and ophthalmic examination and referrals
The school health programme will be coordinated between NRHM, Department of School
Education, Department of Tribal Development, Micronutrient Initiative and UNICEF.
The Strategies for Swasth Pathshala Yojana:
1. Iron Folic Acid – Directly Observed Supplementation to all schoolchildren of middle and
secondary schools. This activity will be carried out weekly on Thursdays. Thursdays will be
declared as Iron days (Loh divas) and Iron tablet will be administered on the spot after
prayers by the teachers.
2. Bi – annual deworming, testing of iodine content of salt will be conducted in June and
December of each year (schools open up by June)
3. Impregnation of bed nets will be synchronized with bi annual ‘Sishu Sanraksaan Maah’.
4. Tab Albendazole 400 mg – 80 lacs in quantity will be procured for deworming. Salt testing
kits will be procured by UNICEF. Deltamethrin solution for impregnation will be provided
by the health department and malaria worker will be entrusted this job.
5. Annual examination for common ailments and ophthalmic examination and referrals will be
done in all the middle schools.
In Chhattisgarh there are around 40 lakhs students’ community who will be benefited from the
biannual deworming drive that will be conducted jointly by health department and Sarva Siksha
Abhiyan (SSA). The drug Iron Folic Acid Tablet and Tablet Albendazole will be purchased and
administration of these drugs to the proposed beneficiary will be done in the presence of Medical
personnel like Supervisor, LHVs/ ANM / BEE or Medical officer. The drive will be done in the
month of June and December in a financial year. Also in this drive health BCC sessions on
personal hygiene, nutrition shall be held and general health check-up will be done by the trained
teachers, health personnel. The PHC doctors will hold screening camps where one ANM / LHV
with some other assistants will support them in conducting this. The screening camps involve
ophthalmic check up, de worming, health education, topics on gender sensitivity, anaemia checkup, basic dental check-up, referral to higher units according to necessity etc. The duration of the
camps will be for three days and special allowance will be given to the health staff and the
Medical officer. The district can also utilize private doctors to conduct such camps. The health
department will design IEC materials books modules to be reprinted by SSA and distribute to the
school and colleges. Biannual deworming drive for all school from primary standard onwards
shall be conducted. During the school health check-up, the other medicine and iron folic acid
will be supplied from the drug kits. In addition to this IFA supplementation to the school-going
NRHM PIP 2009-10: Chhattisgarh
Page 151
adolescents, as well school dropout will be given as special initiative under convergence with
WCD and SSA.
Table 2.40: Estimated budget for Swasthya Pathshala Yojana
Sr. No Budget Head
Unit
Cost
No. of
Units
Duration
Amount
6
School health card
4
1300000
1
5200000
De –worming
.70
3000000
1
2100000
First Aid Kits for children
2000
4600
1
9200000
IFA tablets for school going
adolescent and dropouts
7.5
2830000
1
2,12,25,000
Total
3,77,25,000
Care of children with Severe or Acute Malnutrition - Baal Suposhan Yojana
Background:
As per NFHS III, 52.1 percent children (under 3 years age) are underweight for their age. 45.4
percent children (under 3 years age) are stunted i.e. almost every second child is chronically
undernourished. 18 percent of under 3 years children are wasted (too thin for height). Undernutrition contributes to 53 percent of deaths in children of 0 to 5 years age group. (The
Lancet, Vol 361, June 2003). Children with severe acute malnutrition (SAM) are near to death
and hence require urgent medical attention coupled with nutritional rehabilitation to save
their lives. In addition, though the exclusive breast-feeding till 6 months of age is good at 82
percent, only 54.5 percent children at age 6 to 9 months are started on complementary
feeding. Thus, malnutrition starts ‘setting in’ at 6 to 9 months.
In the PIP budget, provision was made up for establishing Bal Suposhan Kendras in
indentified high prevalence areas 48 CHCs/district hospitals. This year, the recurring cost for
these 48 Bal Suposhan Kendras is being budgeted. The Go guidelines of FIMNCI for treatment
of Severe Acute Malnutrition will be used.
Operational strategy:
1. Baal Suposhan Yojana’ is implemented only in high under nutrition districts.
NRHM PIP 2009-10: Chhattisgarh
Page 152
2. Mid Upper Arm Circumference provided to all the ANMs, Mitanins and Medical Officers is
applied for screening and provides visual impact to the parents on severity of their child’s
malnutrition status. This tape is used only for 1 to 5 years old children.
3. The anganwadi worker will received incentive for referral of severe malnutrition children
to the hospital for treatment.
4. All the Thursday’s will be designated as ‘Suposhan Diwas’ when these referrals will be
ensured and serious cases will be admitted in the PHC / CHC / Hospital.
5. All the Medical Officers will be trained in management of SAM. Quality Assurance of
trainings will be done by UNICEF.
6. The tools for referral and reporting will be developed and implemented.
7. 5 beds will be allotted in 48 CHCs of these districts i.e. a total of 240 beds. A room will be
allotted in each of these CHCs for these 5 beds. The room will be named as ‘Suposhan
Kendra’.
8. Each Bal Suposhan Kendra will be having a feeding demonstrator, cook and regular
feeding facility for those children.
Table 2.41: Budget requirement for Baal Suposhan Yojana
S. No
Budget head
Unit
Unit
cost
No. of
Units
Duratio
n
Total
1
Infrastructure set up cost,
including kitchen
Per facility
100000
20
1
20,00,000
2
Kitchen utensils purchase
Per facility
5000
20
1
1,00,000
3
Food for mother and child
Per bed (5
beds per
CHC)
1000
100
12
1200000
4
Salary for feeding demonstrator
Per facility
5,000
20
12
1200000
5
Salary for cook
Per facility
1,500
20
12
360000
6
Training of doctor (including
TA/DA/Material)
doctor
3000
20
3
180000
7
Incentives for Anganwadi
worker
Identified
malnutrition
cases
50
50000
1
25,00,000
NRHM PIP 2009-10: Chhattisgarh
Page 153
8
Training of feeding
demonstrator and cook
Per trainee
1000
40
1
40000
10
Referral transport
No of
children
200
50000
1
1,00,00,000
11
2nd referral transport
No of
children
referred
750
10000
1
75,00,000
Total
25080000
Swagath’ Package for Mothers and Newborns for institutional deliveries (A package of
services for mothers and newborns)
Introduction
To achieve the maternal and infant mortality goals of Chhattisgarh, there is a need to strengthen
the newborn care much before the baby is born. Important factors for good outcome of a
delivery are - the conditions in which the mother delivers and by whom the deliveries are
conducted.
Learning from market economy and using the same principals, specially the principals for
advertising and sales, it is observed that television and radio advertisements which target the
children are not played late in the night as it expected that children are sleeping at that time.
Thus, lot of emphasis is extended to the timing of advertisement i.e. advertisement for TV go up
during the world cup for cricket and football as there more number of audience watch TV during
this period. Numerous similar examples can be sited which bring out fact that for effective
delivery of message and having a maximum impact the timing and targeting of the messages is
very important. Keeping this in view a package of services has been designed to improve the
coverage of immunization, reduce the morbidity, ensure birth registration etc.
Rationale
There is an old saying that every time a mother gives birth to a child, she gets a new life.
Currently, a number of messages related to health practices are given at various times hoping
for the attitude change resulting in acceptance of best practices. All the IEC materials shows
that, the narrator is talking to select audience for a particular message i.e. to the mother of a
small child for routine immunization, to mother of a sick child with diarrhoea about ORS to
pregnant women about ANC care etc. These messages play an important role in generating
awareness, but how effective they are in bringing about behavioural changes to have an impact
on knowledge, attitude and practice in the target population is a matter of concern.
NRHM PIP 2009-10: Chhattisgarh
Page 154
Lot of time and energy for IEC that is targeted to newborns and mothers are enrooted through
channels that at the end spread too thin in the community. A delivered mother in an institution is
more receptive and is a captive audience for targeting messages on mothers and newborns.
Family members are also more interested in wellbeing of the newborn during this period.
In addition, certain services delivery indicators are poor in Chhattisgarh that require new thrust.
These indicators are: Initiation of breastfeeding within 1st hour is only 36 percent (CES 2006),
institutional deliveries are only 27 percent (CES 2007), children sleeping in insecticide treated
bed net is only 3 percent (CES 2006).
Objectives:
Safe delivery under dignified conditions.
To ensure minimum standard of services provided to the newborns and mother before
discharge from the institution.
Improvement in immunization services to the newborns.
Imparting knowledge to mothers and families regarding childcare.
Empower the mother and family members to identify danger signs and life
threatening conditions in neonates and infants and timely referral for timely care.
(IMNCI)
Birth registration for all the newborns.
Malaria prevention for the mother and child.
To reduce the morbidity and mortality in newborns in Rajnandgaon.
Implementation Strategy:
1. The ‘Swagath Package’ initiative will be implemented in Rajnandgaon, Bastar and
Koriya districts that have the highest IMR (> 100 per 1000 live births as per IIPS 2002
study)
2. The package will be implemented initially only in district hospitals of these districts.
3. The target beneficiaries will be mothers and newborns
4. Swagath package will be delivered to all mothers and newborns admitted to district
hospital. Under the package, the following services will be ensured before the discharge
of mother and newborn:
a. The newborn will be immunized with BCG and OPV (zero dose).
b. PNC care for mother (perineal care) including IFA and standard medication
NRHM PIP 2009-10: Chhattisgarh
Page 155
c. Advice regarding best childcare practices (Breastfeeding, nutrition, hygiene).
d. Practices for prevention of prevalent diseases (ORS, danger signs, IMNCI)
e. Sishu Sanraksak Software will be demonstrated to the mother / family for their ‘on-thespot’ clarification of doubts on child rearing practices. This software is being provided
by UNICEF to the Mitanin helpdesk of all the district hospitals.
f. At the time of discharge the family / mother will be give the ‘Swagath kit’, which will
contain:
i.
Welcome letter
ii.
Mother Child protection card / Immunization card (with dates mentioned of ‘0’ OPV
and BCG)
iii.
IFA tablets and standard medication for PNC mothers
iv.
Pictorial booklet to each mother on danger signs in children and what to do (with
contact details)? (Introduction to IMNCI)
v.
Confirmation of Provisional birth certification and details of obtaining birth certificate
vi.
Sanitary pads
vii.
Insecticide treated bed net
viii.
Cotton cloths for urine / faecal matter disposal – 12
ix.
Recipe booklet on high-energy food.
5. The Mitanin from the Mitanin help desk will delivery this package in close coordination
with the staff from maternity ward and paediatric ward. This Mitanin will be provided
training for one day on ‘Swagath package’.
Areas of support:
UNICEF is ready to print and supply Pictorial booklet on danger signs (IMNCI), bed nets and
welcome letter and MCP cards (provided there are no political overtones on this). UNICEF is
also willing to do the packaging at the central level. The distribution to districts needs to be
taken care by Govt.
NRHM may budget for Tab IFA, sanitary pads, cotton cloths for urine / faecal matter disposal,
recipe booklet.
Budget Estimate:
The estimation for neonatal incentives are made on the assessment that about 7 Lakhs children
are borne in the state in an year, and about a lac of them occur in urban areas. In the remaining
6 Lakhs, it is estimated that 360000 children could be covered under the scheme by Mitanins.
The beneficiaries will be given these benefits.
NRHM PIP 2009-10: Chhattisgarh
Page 156
Table 2.42: Budget support for Swagath package
Sl Unit
Unit
Cost
No of Units
Duration
Total
2
For Incentivising Neonatal
Survival measures(only for home
deliveries)
50
50000
1
2500000
3
Printing of tracking formats and
neonatal messages greeting cards
and referral cards, diaper and
child bed net
150
2,00,000
1
3,00,00,000
Grant Total
32500000
# Content and number of beneficiaries may vary during the implementation phase
Management of Diarrhoea with ORS and Zinc:
India has a national policy for management of diarrhoea among children under 5 years that
recommends the use of Zinc tablets along with Lo - ORS in the treatment of diarrhoea as per the
MOHFW, GoI directive dated 2nd Nov. 2006. The policy recommends for every case of
diarrhoea, a dose of 20 mg/day for 14 days (even if diarrhoea has stopped) for children above age
6 months to 5 years and 10mg/day for 2-6 months.
Table 2.43: Children with diarrhoea who received ORS in Chhattisgarh
STATE
DLHS –II (02-04) (%)
DLHS –III (07-08)
(%)
Chhattisgarh
41.7
36.6
Chhattisgarh (Rural)
39.3
35.7
Chhattisgarh (Urban)
51.4
41.6
Sl. No.
Name of the District
NRHM PIP 2009-10: Chhattisgarh
DLHS –II
(2002-04) %
DLHS –III
(2007-08) %
District
Ranking from
lowest to
highest
performance
(From 1 to 16
Page 157
)
1
Dantewada (including
Bijapur)
19.6
14.6
1
2
Korea
11.2
21.1
2
3
Bastar
(including
Narayanpur)
33.7
22.1
3
4
Korba
37.3
24.5
4
5
Jashpur
83.1
24.7
5
6
Kawardha
47.8
28.0
6
7
Sarguja
35.0
30.5
7
8
Bilaspur
22.2
39.0
8
9
Kanker
53.1
39.6
9
10
Janjgir-Champa
36.8
45.2
10
11
Dhamtari
34.2
47.3
11
12
Raipur
19.0
48.6
12
13
Raigarh
35.9
50.3
13
14
Mahasamund
51.8
50.9
14
15
Durg
57.4
51.1
15
16
Rajnandgaon
45.2
53.0
16
Community-based Trial Demonstrates Longer-term Benefits of Zinc:
Increased ORS use from 50% in control clusters to 75% in Zinc clusters
(Source –Baqui, Black, Arifeen, BMJ 2003)
Suggested Points for scaling up Zinc and Lo ORS in Chhattisgarh.
1. Review the utilization of ORS as per DLHS –III (2007-08)
NRHM PIP 2009-10: Chhattisgarh
Page 158
2. GoI directive on use of Zinc as an enhanced therapy in the treatment of diarrhoea.
India has a national policy for management of diarrhoea that recommends the use of zinc as
adjuvant to ORS in the treatment of diarrhoea as per GoI directive dated 2nd Nov. 2006. The
policy recommends for every case of diarrhoea, a dose of 20mg/day for 14 days (even if
diarrhoea has stopped) for children above age 6 months and 10mg/day for 2-6 months age.
The policy emphasizes that:
a) Zinc tablets should be available in all parts of the country including at Anganwadi
Centres
b) Zinc be made an over-the-counter (OTC) formulation
c) An effective communication strategy be put in place
d) Health care providers are oriented and trained in the use of zinc along with ORS
3. Review the Challenges of Scaling up the revised diarrhoea management program:
An expert group chaired by Prof. M K Bhan, Secretary, Dept. of Bio Technology, Govt. of India
is formed to translate the policy decision into concrete operational and technical specifications
for taking the policy forward and highlighted some of the challenges for scale up. Some of them
are:
a) Low ORS use rates (36 % Children in Chhattisgarh were given ORS during diarrhoea as
per recent DLHS –III -07-08 as compared to 41.7 % as per DLHS –II (02-04))
b) Lack of awareness among the stakeholders about home management of diarrhoea
c) Procurement and supplies
d) Management of diarrhoea by private providers. The district level household survey data
shows that 65% of diarrhoea is treated by the private sector (formal and informal). The
new strategy should effectively reach networks of the formal private sector.
e) Compliance of Zinc therapy for 14 days
f) Monitoring and Evaluation systems
4. Broad Action Plan for scaling up revised diarrhoea management in Chhattisgarh.
Sensitization of state and district level functionaries
Supply of Zinc + Lo ORS to project districts
NRHM PIP 2009-10: Chhattisgarh
Page 159
Development of communication strategy and printing of IEC materials
Printing of Training Modules
Training of block, sector and field level functionaries of Health in year 1 and
Anganwadi Workers and Mitanins in year 2 & 3 and Private Medical Practitioners in
year 3
Field level monitoring
External Evaluation to assess the extent of awareness and utilization of zinc + Lo
ORS in the community
Integrating Record keeping and reporting in the existing MIS
Support by Stakeholders for Scaling up revised diarrhoea management program
Name of the Stakeholders
1) DOHFW, Govt. of Chhattisgarh
2) BIBCOL, DBT, GoI
3) Micronutrient Initiative (MI)
4) UNICEF
Suggested areas of Support by different Stakeholders:
Name of
Stakeholder
Suggested Area of Support
DOHFW, Govt. of
Chhattisgarh
Supply of Lo ORS (already procured by the dept.)
Supply of Zinc (Budgeted Rs. 1.53 crores in NRHM PIP 08-09)
Training of Health Workers in year 1 and Mitanins in year 2 and 3
BIBCOL, DBT, GoI
Supply of Zinc tablets worth Rs. 1 crore
UNICEF
Supply of Low Osmolar ORS and Zinc tablets for district
Rajnandgaon
Development of training and IEC materials in coordination with
DOHFW and MI
Monitoring in the field
Provide ‘Zinc –ORS Coordinator’ to be placed in RCH wing of
NRHM PIP 2009-10: Chhattisgarh
Page 160
Micronutrient
Initiative (MI)
DOHFW, CG
Sensitization of state and district level functionaries
Development of communication strategy and printing of IEC
materials
Printing of Training Modules
Training of MOs and Health Supervisors in year 1, ICDS
Supervisors and Anganwadi Workers in year 2 and Private
Medical Practitioners in year 3
Field level monitoring
External Evaluation to assess the extent of awareness and
utilization of zinc + Lo ORS in the community (baseline and end
line)
Integrating Record keeping and reporting in the existing MIS
Techno-managerial support through network of consultants to
coordinate at state, district and block levels to smoothly
implement the program
Implementation Strategy:
To scale up revised diarrhoea management in 11 low performing districts and district
Rajnandgaon, the state needs Zinc courses of 31, 18,189 which is to the tune of Rs.
2,61,92,787.
The Department of Health & Family Welfare, Govt. of Chhattisgarh will share the cost
of Zinc tablets of Rs. 1, 34, 14,596 for procuring 15, 96,976 lakh courses of Zinc from its
existing NRHM PIP funds where as BIBCOL, DBT, GoI will share Rs. 1 crore for the
supply of 11, 90,476 courses of Zinc (as per their letter D.O No. BIB/MD/OW/09 dated
15 January 2009) and for Rajnandgaon district UNICEF will fulfil the supply of Zinc
tablets.
The DOHFW, Govt. of CG has already procured Lo ORS; hence, the same will be used
for this purpose.
Micronutrient Initiative (MI) will be providing support in terms of Training, IEC, Record
Keeping & Monitoring, Advocacy, Evaluation etc. and provide techno –managerial
support through its Consultants appointed by its existing partner NGO Child In Need
Institute (CINI).
ORS-Zinc coordinator will be positioned in RCH wing of DOHFW, Govt. of CG by
UNICEF
NRHM PIP 2009-10: Chhattisgarh
Page 161
Quarterly meetings chaired by Secretary Health to review the implementation will be
held.
Broad Area of Activities for scaling up Revised Diarrhoea Management Program
Sensitization of district level functionaries
Supply of Zinc + Lo ORS
Development of communication strategy and printing of IEC materials
Printing of Training Modules
Training of block, sector and field level functionaries of Health
Field level monitoring
External Evaluation to assess the extent of awareness and utilization of zinc + Lo
ORS in the community
Integrating Record keeping and reporting in the existing MIS
Scaling up revised diarrhoea management (Zinc + Lo ORS) in all districts of
Chhattisgarh (2009-10)
Table 2.44: Estimated Budget for management with Zinc and ORS
Sl.
No.
Budget Head
Unit Cost
(Rs.)
Unit No.
1
Cost of Zinc Tablets
8.4 per
course
32,11,301 2,69,74,928
NRHM, BIBCOL
& UNICEF
1.1
Sharing of Zinc Tablets by NRHM
8.4
17,79,386 1,49,46,849
NRHM (Already
budgeted Rs. 1.53
crores in 08-09)
1.2
Sharing of Zinc Tablets by BIBCOL
8.4
11,90,476 1, 00, 00,
000
BIBCOL, DBT,
GoI
1.3
Sharing of Zinc Tablets by UNICEF
8.4
2,41,438
20,28,079
UNICEF
2
Program Costs
2.1
Advocacy Workshops/ Project
Launching/dissemination workshop
2,75,000
1
2, 75, 000
MI
NRHM PIP 2009-10: Chhattisgarh
Total Cost
(Rs.)
Source of Funds
Page 162
2.2
Training
2.3
Printing Training Modules
30
9000
2,70,000
MI
2.4
State Level TOT of district health
officials @ 3 persons per district
1000
54
54,000
MI
2.5
Training of MOs and Supervisors at
district HQ
250
2546
6, 36,500
MI
2.6
Training of Health Workers
150
7239
10,85,850
NRHM/MI
2.7
IEC
2.8
Development and Print wall hanging
10
poster @2 per AWC, 2 per SHC, 5 per
PHC, 10 per CHC/DH
80000
8,00,000
MI
2.9
Record Keeping Formats/Registers
50
5600
2,80,000
MI
2.10
Monitoring (Travel cost of
Consultants hired by MI-CINI)
8,75,000
-
8,75,000
MI
2.11
Evaluation (Base line and End Line)
7,50,000
1+1
7, 50,000
MI
2.12
Development of Scale up Guidelines
for revised diarrhoea management
4,00,000
1
4,00,000
MI
Contributions by each partner
NRHM, CG
1, 49, 46,
849
BIBCOL, DBT, GoI
1, 00, 00,
000
MI
54, 26, 350
UNICEF
20, 28, 079
Therefore, the total amount required from the NRHM for the proposed activity for the year
2009-10 is Rs. 1, 49, 46,849
NRHM PIP 2009-10: Chhattisgarh
Page 163
Home Based Neonatal Child Care (HBNCC)
HBNC is being seen as a part of the overall strategy of upgrading neonatal care in the state.
HBNC (Gadchiroli Model) is already a well-recognized methodology for reducing infant
mortality. It involves on site provision of care by trained Community Health workers. In
Chhattisgarh, it will be implemented through Mitanins.
All essential HBNCC interventions (including vitamin K, Birth asphyxia and sepsis management
with cotrimoxazole and gentamicin injections) will be implemented through Mitanins. For this,
Mitanins as well as the required supporting structure will be trained. Mitanin though trained to
be able to independently manage sepsis should use injections only if no other effective
alternative is available. It is necessary to train the Mitanin in sepsis management because – a)
likelihood of ANM reaching the home within 2 hours is difficult in the current set up and b) it is
not medically advisable to bring a newborn to a sub-centre or PHC 5 times c) Majority of the
families will find it too difficult to take the newborn to a functioning facility due to
transport/economic constraints d) Skilled mitanin anyway will be needed for screening the cases.
Curriculum will be worked out by bringing together elements from the existing Mitanin modules
on neo-natal and child survival and HBNCC. Only literate Mitanins will be trained in use of
gentamicin injections. HBNCC will be integrated with the Public Health system through a series
of measures. Apart from training of Mitanins, it will also include training of Mitanin Trainers,
ANMs, Staff Nurses and Medical Officers in HBNC. HBNC operational strategy will be suitably
adapted to the situation of Mitanins and the health system in Chhattisgarh.
Project Phasing:
The project of establishing HBNCC coverage through Mitanins across Chhattisgarh state will be
carried out in two phases. Phase I of four years will be implemented in six blocks of the state.
Since effectiveness of HBNCC methodology is already well recognized, the focus of Phase I will
be on operationalisation issues including feasibility and safety. Phase I will attempt to find
answers to operational challenges and come up with a strategy of scaling up HBNCC throughout
the state. It will involve building capacity for the subsequent scale up including i) Training
manpower ii) and tested and finalized training material, Supportive supervision & monitoring
structures and MIS. Phase I will require four years. Phase II will be focused on expansion to
cover all blocks needing HBNCC interventions.
Current Status
A survey on the children died in their first year was conducted by SHRC in the month of Oct 08
to understand the reasons of neonatal and children death. The sample size of the research study
was 1471 children.
NRHM PIP 2009-10: Chhattisgarh
Page 164
Table 2.45: timing of infantile death as estimated by SHRC
S.No
District
Block
First Day
first week
within 1 month
Within a year
Total
1
13
38
135(9%)
406(28%)
406(28%)
524(35%)
1471
This clearly shows that HBNCC intervention is required to combat the neonatal death.
The program is being envisaged to be started on pilot basis in six blocks of the state as a fouryear intervention. Apart from covering a rural population of around 700,000, this intervention
will provide the state critical experience for future expansion. It will provide a strategy to
overcome operationalisation issues including feasibility and safety. SEARCH Gadchiroli will
provide technical inputs and SHRC will play the facilitation role. It will be implemented through
a MOU between the Dhow, SHRC and SEARCH.
Area to be covered under HBNCC Phase I:
Selection of blocks:
6 predominantly tribal blocks selected based on need for HBNC intervention:
Kanker district: Blocks:
Bhanupratappur (Population 83,130 and No of Mitanin 400) and Kanker (Population 89,625 ,
No of Mitanin 400)
Raipur district: Blocks:
Bhilaigarh (Population 2,18,067 and No of Mitanin 497) and Chura ( Population 1,07,502 and
No of Mitanin 469 )
Bastar district: Blocks:
Darbha (Population 1,04506 and No of Mitanin 396) and Pharasgaon (Population 1,07,145 and
No of Mitanin 380)
Along with the present of no 2542 Mitanins, 176 new Mitanins are required in these 6 blocks
Attempt will be made to cover the entire rural population of the selected blocks. Thus, around 7
lakh rural population will be covered through the Phase I programme. Blocks in Northern
Chhattisgarh, though equally needy, were not selected for Phase I because a highly scattered
distribution of Phase I blocks will pose management problems.
Objective
NRHM PIP 2009-10: Chhattisgarh
Page 165
To reduce neonatal mortality on pilot basis in 6 blocks through HBNCC intervention in coming 3
years and to replicate it in other blocks
Strategy
1. All essential HBNCC interventions (including vitamin K, Birth asphyxia and sepsis
management with cotrimoxazole and gentamicin injections) will be implemented
through literate Mitanin. For this, Mitanin as well as the required supporting structure
will be trained. Mitanin though trained to be able to independently manage sepsis
should use injections only if no other effective alternative is available. It is necessary to
train the Mitanin in sepsis management because – a) likelihood of ANM reaching the
home within 2 hours is difficult in the current set up and b) it is not medically advisable
to bring a newborn to a sub-centre or PHC 5 times c) Majority of the families will find
it too difficult to take the newborn to a functioning facility due to transport/economic
constraints d) Skilled Mitanin anyway will be needed for screening the cases. While the
second set of rest of the Mitanin will be trained on all basic components of HBNCC and
asphyxia management.
2. CG need base Curriculum will be worked out by bringing together elements from the
existing Mitanin modules on neo-natal and child survival, as well as other round of
modules and HBNCC.
3. HBNCC will be integrated with the Public Health system through a series of measures.
Therefore, that it will strengthen the existing public health system in addressing the
HBNCC interventions.
4. In all blocks, the supervisory and mentoring cascade will be developed for
implementation that will be dually supported by district CMHO and SHRC HBNCC
programmed unit.
5. The incentive package for two set of Mitanin as well as for ANMs (which will depend
on decision on govt policy).
6. A non-transfer policy for health staff of 6 blocks will be formulated and implemented.
7. In capacity building along with classroom training and on job training the exposure
visit to Gadchiroli will be worked out.
8. Pre and post project study will be done along with developing a CG need based
HBNCC HIMS for project.
9. The project will be implemented through a third party MOU among SHRC, Govt of CG
and SEARCH, Gadchiroli. The duration of the project will be at least three years. The
NRHM PIP 2009-10: Chhattisgarh
Page 166
cost of the project will be managed through NRHM under RCH section and Mitanin
programme budget.
NRHM PIP 2009-10: Chhattisgarh
Page 167
Operational Activities with Objective
Selection of Mitanins
Mitanin will be the key service provider for HBNC. Currently a Mitanin looks at an average
population of 250. This population is too small for her to keep getting enough cases so as to
continue to practice her skills of sepsis management. Therefore, a population size of around 750
(500 to 1000 depending upon field conditions) per Mitanin would be more appropriate.
Asphyxia and sepsis management and the rigorous recording requirements of HBNC require the
service provider to be literate. Therefore only literate (at least 5th standard pass) will be selected
to be trained in asphyxia /sepsis management (ASM).
Keeping the above two criteria in mind, around one in three Mitanins will be trained in ASM.
Thus, out of 2718 Mitanins present in the selected 6 blocks, around 400 will be ASM trained.
The rest of the Mitanins will be trained in HBNC interventions and Asphyxia management other
than ASM. The ASM trained Mitanin will thus look at around 750 population and attend all
childbirths (and make an average of 10 home visits per newborn) in this population. The nonASM trained Mitanins will play the role of sending message to ASM trained Mitanin to attend the
childbirth and to support the follow-up activities.
HBNC protocol requires intensive home visits by Mitanins. In order to ensure that a high
percentage of timely visits take place and that case-wise detailed records are properly
maintained, it is necessary to institute monetary incentives for the Mitanins. The ASM Mitanin
will need to be paid around Rs. 100 per case for all newborns in the population (and not just
sepsis cases).
Incentives to ANM those are providing ASM at SHC will be get incentive after decision from
govt.
Incentives to Mitanin for HBNC home visits Interface with local Public health
functionaries:
Mitanin (ASHA) is already an established extension of the health system into the community.
By adequately incentivizing her for her service delivery role, this linkage will be further
strengthened.
Existing Mitanin Trainers (MTs) and District Resource Persons (DRPs) will also be trained
in HBNCC so that coordination at field level becomes easier.
All ANMs, LHVs and doctors in selected blocks to be trained in HBNC so that they can also
be service providers for HBNC and provide support to Mitanins
NRHM PIP 2009-10: Chhattisgarh
Page 168
District, CHC and PHC level health officials to be given orientation to HBNC so that they
can provide appropriate support to the programme
Introduction of 2nd ANM concept in these 6 blocks to be attempted so that the proportion of
sepsis cases handled by sub-centre can be increased
ANM to be service provider for asphyxia/sepsis management in village of her residence so
that they keep practicing the skills
Trained health staff not be shifted out of block so that training investment does not go waste
Programme Management Structure
A specialized cadre of Supervisors will be needed for providing intensive guidance and
supervision. The existing MT-DRP set up already has a high workload as they carry out a wide
range of interventions and the support required for HBNCC interventions is more technical.
Therefore, programme intensity cannot be achieved with the existing MT-DRP team and
additional supervisory staff with somewhat more technical background will be needed.
One such Supervisor can support around 15 ASM trained Mitanins so that each ASM Mitanin
can get at least two visits from the supervisor in a month. Therefore each block will need an
average of 8 supervisors( 4 will be from government and the other four will be from non
government ) . Thus, for 6 blocks a total of around 48 HBNC Supervisors will have to be posted.
Attempt will be made to include at least one supervisor per block from health department staff.
Each block team will have a HBNC Coordinator. Since HBNC require a large amount of data to
be managed, each block will have a computerized office and a data operator.
The state level team will have the following members- State HBNC coordinator, State Data
Manager, accountant and support staff.
The selection criteria for the above roles will be as close to the one tested in ANKUR and ICMR
trials. Attempt will be made to ensure that only the candidates with background in healthcare are
selected as Supervisors.
Base line and annual surveys:
These surveys will be needed. The proposed team of Supervisors will carry out the survey after
appropriate training.
Operational Challenges
Since Phase I will focus on operational issues of HBNCC, attempt was made to foresee the kind
of challenges that will emerge in implementing it through Mitanins. These challenges will also
form the research questions as part of this study.
NRHM PIP 2009-10: Chhattisgarh
Page 169
1. The Mitanins will be divided into two categories – ASM and non-ASM. The non-ASM
Mitanins are likely to feel dissatisfied as ASM Mitanins will start coming into their areas,
will learn skills like injections, earn much bigger cash incentive. So far, literate and nonliterate Mitanins were treated equally in the programme. However, this will not be the case
once ASM is introduced. The non-ASM mitanins may start getting the feeling that they are
inferior to ASM Mitanins. This may affect their motivation adversely and a whole lot of
important functions that these Mitanins play may suffer.
Another kind of resentment may arise in a situation where all the Mitanins in a geographic
cluster are literate. In order to have adequate population size, it would be imperative to train
only a third of them in ASM. Literate Mitanins who is not selected for ASM role may
therefore resent their exclusion. Therefore, a strong consensus building effort will be needed
in each of the six blocks while demarcating roles.
2. Introducing cash incentives for neo-natal home visits only in 6 blocks is likely to cause
resentment amongst Mitanins in other areas, starting with the adjoining blocks. Therefore,
effort needs to be made to institutionalize cash incentives for home visits by all Mitanins
across the state.
3. Integrating Mitanin based HBNC with existing public health system will be a challenge. Over
a period, capacity of facilities like PHCs and sub-centres will have to be created along with
strengthening availability of referral transport. In the meantime, involving ANMs, LHVs,
PHC and CHC doctors will require constant effort.
4. Working out the division of roles between SHRC and the health department will also pose a
challenge. For example, the programme involves recruitment of more than 65 staff.
Resolving the issues of who recruits them and whom they report to etc. will also pose a
challenge. Successful resolution of implementation arrangements will require sustained
effort.
5. HBNC (especially ASM) being visualized as an intensive programme needs specialized
support structure. However, this may lead to verticalisation. Disconnect may also arise
between the existing MT-DRP-FC team and the HBNC supervisor-block coordinator team.
Therefore, a strategy needs to be worked out to integrate the two set of field level human
resources.
6. The human resources needed for HBNC (from supervisor level to state coordinator level)
may not be easily available in Chhattisgarh. E.g., a BAMS doctor works as a supervisor in
Gadchiroli. In Chhattisgarh, persons with paramedic qualification or from the Block
Training Teams created by SHRC may have to be recruited. Nevertheless, ensuring that
personnel with adequate background in health sector still will be a challenge.
NRHM PIP 2009-10: Chhattisgarh
Page 170
7. HBNC needs considerable financial resources. The requirement for the 6 Phase I blocks will
be around Rs.9 Crores over next four years. Initiating and maintaining this flow from NRHM
will also be a challenge.
8. Preventing misuse of treatment skills by ASM Mitanins will require effort to build community
awareness.
9. Apprehensions have been expressed by a few of the stakeholders regarding whether
Mitanins can administer injections safely and whether adequate supervision and support can
be provided in a large scale setting. The project in its early stages will have to demonstrate
the safe use of injections by Mitanins.
SEARCH, Gadchiroli role
SEARCH will help SHRC in
Design of modules for ASM and non- ASM Mitanins through a) Desk review of existing
Mitanin modules on Neo-natal & Child survival and b) Training need assessment
(through 3 workshops with Mitanins at the block level)
ToT (Supervisors, block HBNC coordinators) and oversight over training of Mitanins
Exposure Visit of Supervisors, block coordinators, health officials etc to Gadchiroli
Training of Surveyors on Baseline Survey
Training of Data operators, managers, software support for ongoing HMIS for HBNCC
project.
Timeline for different activities in Phase I:
1. Identification of contents of training of Mitanins based on present Mitanin course content
( by Feb 09 )
2. Evaluation of Mitanin present status ( by end of March )
3. Approval for HBNCC project for 6 blocks from CG govt (by end of Jan 09) and NRHM
PIP approval. ( by mid of Feb 09)
4. Signing of tri party MOU (by March 09).
5. Recruitment of block coordinators and state HBNCC unit at SHRC
(March - April 09)
6. Recruitment of trainers of surveyors/Mitanins (March - April 09)
7. Training of trainer supervisors for survey (by end of March 09)
NRHM PIP 2009-10: Chhattisgarh
Page 171
8. Base line data for literate and literate Mitanin and selection of ASM Mitanins (by end of
March 09).
9. Training of surveyors (by end of March 09)
10. Base line survey ( by end of March or April)
11. Redrafting of training modules (by March 09)
12. Training of project managers and block coordinators ()
13. First training of trainer-supervisors of Mitanins in HBNCC ( May – June 09 )
Table 2.46: Budget estimation for HBNCC
S. No Unit Description
Unit
Cost
No. of
Units
Duration Total Cost (Rs.)
1
HBNC consultant ( Paediatrician)
30,000
1
12
3,60,000
2
Block Coordinator
10,000
6
12
7,20,000
3
Field Supervisor ( Out of total 8 field
6000
supervisor 4 will be from NGO and rest
4 will be from government) per block
24
12
1728000
4
Data Assistant
7500
2
12
180000
5
Base line survey in 6 blocks(training,
format, data entry, analysis 0
500000
1
1
500000
A
HR management (consultant, field trainer etc.)- support,
supervision, data management and Base line
1
Training of Mitanins (ASM)
2000
400
1
800000
2
Training of Mitanins (other)
1500
2400
1
3600000
3
HBNC kit( Ambubag, gentamicin etc.,
drugs and Consumables/other
supports)
1000
400
1
400000
4
Mitanin Incentive
100
3000
B
Training of Mitanins (ASM), HBNC kit, Mitanin Incentive
5100000
Total ( A+B)
82,28,000
NRHM PIP 2009-10: Chhattisgarh
3128000
300000
Page 172
Crèches in district hospitals:
Crèche is not a very old concept in our country. One remarkable step in the advancement of
society is characterized by the role played by women in the work sector beyond the domestic
circle.
Facilities could be created to support the increasing role of women in work sector. The
innovative step to start crèches facilities in the district hospitals is an attempt to see and care for
without being negligent about the domestic and familial responsibilities of the women in the
professional world. To start the crèches facility in the districts hospitals is an attempt to address
the care and support needed for the development of the children. Introduction of the facility of
crèches in the hospitals will be useful for social, physical and psychological development of the
children.
The breast-feeding centres or crèche facilities at work places have now become a necessity for
working mothers. We know that breast-feeding is critical for the health and nutrition of the
newborn and the mother. The kind of intensive baby care required for babies at the early stage
cannot be offered in the public nature of the workplaces. The mothers need a private space
where they can breastfeed or the babies can take rest, relax and play. Preparations at the
various levels need to be done to make such crèches where children can play sleep and relax. We
need to equip the rooms with bed, mattresses, curtains, toys and other things that are the basic
needs for setting up of crèches for the children.
It is being proposed to set up the crèches as per the norms and guidelines of childcare. Total 4
staffs will be hired per district for the care and support of the children. We intend to make the
crèche 24 hour functional for this hired staffs will work in shifts. 2 of the staffs will take care of
the children in afternoon shifts and 1 for morning other for night shift. The crèche will serve all
the basic requirement of the children like food, sanitary napkins etc.
The staffs and patients can use the crèches facility for breast-feeding and to take care of their
children. The efficient functioning of the crèches facility will also lead to better quality of service
delivery by the female staffs that in turn will be the impetus for the better functioning of the
districts hospitals.
Objective to provide crèches facility in the districts hospitals
Care and support for the development of children
Better functioning of the districts hospitals
NRHM PIP 2009-10: Chhattisgarh
Page 173
To increase the participation of women staff in the work force and to provide facilities to
the patients for the increased utilization of the services
Strategies
Allocation of space for the functioning of the crèches in the district hospitals
Management of the crèches in the districts hospitals will be done by the contractual staff.
They will work under the supervision of the Jeevandeep Samitis
Budget requirements for one district hospital
Since this activity will be carried out in coordination with Women and Child Health Department
so no separate budget is required for this activity.
Urban RCH
Urban health systems:
The state has four major cities with more than a lakh population, amongst which Raipur, Durg
and Bilaspur are the most highly populated and growing. The growth of these cities is
tremendous after Chhattisgarh has become an independent state. Migration to these cities from
surrounding rural areas is high. Development of these towards advanced cities is generating a
large number of new health challenges to be handled. The rising populations here are largely
served by private providers. The growth of the urban slums is the most challenging feature and
provision of health services, where affordability levels are very low and public systems are
lacking is a difficult problem to tackle. The strategies planned to address this were to set up
urban health centres per ten thousand populations for the poor population particularly living in
the slums, peer education programme for the urban vulnerable and community health workers
per thousand populations. The implementation of these strategies is at the very early stage and
this needs to be strengthened
Objectives:
1. Bringing down the Urban IMR from the current stagnated level.
2. Improving urban health services in order to reach out to the slum and vulnerable
populations.
3. Improving health awareness of the urban communities to optimise use of available
services.
Strategies:
NRHM PIP 2009-10: Chhattisgarh
Page 174
1. Identification of vulnerable areas through urban area mapping of existing and new
colonization by poor population groups and current health service centres.
2. Establish urban health centres per 10000 populations of urban poor areas with trained
nurse, necessary infrastructure and equipments as well as supplies in place.
3. Establish referral linkages from such urban health centres to available clinical facilities
and major hospitals
4. Select, train and deploy Urban Community Health Volunteers per 1000 slum area
population.
5. Identify and train peer educators for vulnerable groups
Progress So far:
A mapping of urban health facilities was done in year 2005-06 and these needs to be updated.
One other major intervention had been filling the equipment gaps in available urban health
facilities and IEC activities. The key interventions like setting up urban health centres, setting up
referral linkages, community caregiver identification and peer education programmes are yet to
be shaped up.
Strategies:
Urban areas are categorized into six (A through F) based on population. The smallest two
groups E & F would just have their sub-centres upgraded by an additional ANM as required by
norms. In C& D towns, the focus would be on opening urban health centres with a part time
doctor under an urban health administration unit – linked for secondary care to the CHC. This is
particularly suited for mining towns that have large uncovered unorganized worker population.
In category A & B towns careful participatory mapping would identify beneficiaries (the 33%
poorest) and then a unit of one lakh beneficiaries would be provided with 10 urban health
centres and one secondary health centre. In all 120 UHCs are proposed.
The design of an urban health centre is roughly a fusion of the current rural sub-centre with
some aspects of the PHC. It will serve 10,000 beneficiaries each and would cost about Rs 2.6
lakhs per year. The secondary centre is situated for every 1-lakh beneficiaries.
In a systematic approach, a limited social insurance package is also proposed to cover the
poorest at government cost and to cover all others with premiums paid/deducted for a limited
range of services in PPP or government facilities. Selection, training and deployment of Urban
Community Health Volunteers per 1000 slum area population will be undertaken this year.
Community Health Volunteers will facilitate a Peer education programmes for marginalised
groups and mobilisation of beneficiaries for RCH services.
NRHM PIP 2009-10: Chhattisgarh
Page 175
NRHM PIP 2009-10: Chhattisgarh
Page 176
Activities:
1. Careful identification of beneficiary families and vulnerable families through a
participatory mapping exercise followed by a door-to-door survey.
2. Community Level caregivers (similar to Mitanin) covering intensively 200 beneficiary
households or 1000 population and visiting on all households in their area.
3. Paramedical and basic medical services, through a network of urban health centreswithout fresh infrastructure creation -. Utilize both NGO and Private sector partners for
this. This may mean an urban health centre for about 10 to 15,000 households. Each such
urban health centre would have a rented premise and two ANMs or nurses or qualified
female paramedicals who can conduct delivery if needed and provide immunisation
services and antenatal care and other services similar to the rural sub-centre. Each such
urban health centre will be attached to 10 to 15 community level caregivers and she
would be their trainers and support. They in turn would support the urban health centre
and ensure minimum attendance and services delivery. Thus, the urban slum area would
be demarcated into sections each of about 10,000 to 15,000 population and each section
or a number of sections taken together could be contracted out. The urban local bodies
would be coordinated for these services.
4. Urban secondary referral services through a linkage with the CHC/district hospital or
PPP arrangements with a network of private clinics for emergency obstetric care,
institutional care of sick child, safe MTP services, FP sterilization services, adolescent
health care and counselling and diagnosis and management of RTIs /STIs/ infertility.
These services are subsidized for the poor and at reasonable cost for the rest with a
provision for exemption of the poorest in special emergencies.
5. Linkages will also be made available to district hospitals and teaching hospitals.
6. Peer caregivers for special highly marginalized groups – the homeless, the street child
and the commercial sex workers etc– reached out through NGO programmes.
7. Peer education programmes in urban schools for adolescents and in adolescent
frequency zones for out of school adolescents.
8. Designing a programme for social health insurance cover for the urban poor to cover all
institutional health needs is ongoing; this is expected to be completed by the end of this
year.
NRHM PIP 2009-10: Chhattisgarh
Page 177
Budget Requirements:
An urban health centre cost would about Rs 2.6 lakhs per year. This excludes infrastructure
costs though it includes rental costs. Approx two ANM @ Rs 5,000 per ANM per month, Rs
24,000 package for minor equipments and training, Rs 36,000 per year for infrastructure
repairs or rent and incidents. Consumables and some of the infrastructure costs would have to
come from the state budget. Since last year budget remains unspent so that budget will be used
and no additional budget is required for this year.
Infrastructure:
This shall be addressed largely by the NRHM flexible pool and the state budget. One of the new
initiatives that the state plans to take up under this is the implementation of IMEP. Another
innovation is to address the major necessity of the state in the nurse training and nurse training
facilities, these are also been budgeted as part of NRHM flexible pool.
Implementation of IMEP and quality assurance cell
Infection control is one of the key areas of intervention under RCH. Sterilization of needles is
one of the main issues at the PHC level. Following difficulties are encountered by the doctors
and nurses in infection control management: State has one incinerator which cater to all
districts which is inadequate to handle the load and thus hospitals and nursing clinics use other
method to dispose of biomedical waste which is some time not meet the infection control
protocol. Basic cleanliness is also a problem and facilities for waste disposal remain very weak.
At least some areas must be marked off for deep burying or landfill and fenced off. If this is not
done disposal of placenta, MTP products and other body fluids etc becomes difficult, unethical,
and dangerous. Incinerators are required in large facilities.
In order to meet the increasing demand of incinerator the state proposes to set up four
incinerators at four places one at Raigarh, Bilaspur, Rajnandgaon, Bastar. To set up incinerator
and induced trained staff to operationalise it NGO/ or private operator help can be taken. The
state government will setup these incinerators and it could be given to the NGO/ or private party
to operate it by charging fees from private hospitals and nursing homes. The waste generated
from government hospitals will be incinerated free of cost. The modalities to operationalise it
will done after getting Expression of interest from NGOs/ private parties
Some area at every block will be marked for deep pit burials that can be used by both private
providers and government hospitals. A third party monitoring systems (neutral monitoring
systems) will be introduced to monitor infection control at the 32 designated FRU where IPHS
norms are maintained. For this, a private body will collect seven swabs for OT area, minor OT,
etc and give reports on anaerobic bacteria presence in the swabs. If the reports are negative it is
NRHM PIP 2009-10: Chhattisgarh
Page 178
ok but if it is positive then the OT will be closed down and fumigation will be held. The
modalities to do such third party monitoring will be implemented after getting expression of
interest from third party.
The district will set up quality assurance cell that will give reports on quality issues and address
the shortfalls. The cell will consist of a senior pathologist in the district, PG gynaecologist, Chief
medical and health Officer of the district, and a senior surgeon. The cell will meet every month
and formulate strategies for infection audit of both private and government organization. The
reports along with observation will be discussed in CMHO review meeting and compliance
assured. Since fund is available with the state for this from last PIP for additional fund is not
required in the current year.
Institutional Strengthening
Major activities that we are taking up under this are the setting up of HMIS and BCC initiatives.
Part of the BCC initiatives is pooled from NRHM also.
Strengthening of BCC/IEC
Chhattisgarh is a tribal state, joining borders with 5 other states and with high cultural
heterogeneity. It has been a challenging area to address for the issues of behaviour change in a
heterogeneous population. Even if the language of communication in Chhattisgarh is
Chhattisgarhi, the use of words and styles differs from area to area. It indicates that no common
strategy is going to work for the entire state as different areas have different dialects of
communication.
Current Status
Key health problems in Chhattisgarh is malaria, T.B, sickle cell anaemia, HIV/AIDS, snake bite,
leprosy , malnutrition, food security etc
In state, key health problems needs focused interventions are as follows:Table 2.47: Key health problems for focussed intervention
S.No Key
health
problems
India (%)
Chhattisgarh (%)
1
Malaria
In 2007 (upto 31st December) the ABER was 14.04,
API 5.95, SPR 4.23 and Pf% 73.5
2
Leprosy
The
country’s In NLEP there are 5636 cases under treatment with
Prevalence rate is Prevalence Rate (PR) of 2.42 per 10,000 population
NRHM PIP 2009-10: Chhattisgarh
Page 179
0.81
per
10,000
population
with
ANCDR 12.1 per
1,00,000 population .
as on Nov,2008 with 5257 new leprosy cases have
been detected with Annual New Case Detection Rate
( ANCDR) of 35.4 per 1,00,000 population ( Sep
quarter ending) since April too Nov,08.
3
T.B
TB and Sickle cell are critical problem in the state , so effective BCC/IEC
materials is required for this
4
Sickle cell
5
Snake bite Jashpur and Bastar districts are mainly affected from this
BCC Matrix was prepared based on the deliberations made in the zone level workshop
indicates a series of behaviour related interventions. The analysis of the BCC matrix and
village health plans (VHPs) shows resistance in families for colostrums feeding, meal to mother
after delivery, delay in bathing after birth expressing breast milk and giving it to child in case of
working mother and hand washing etc
Table 2.48: Key problems needing behaviour change approaches
S.No Key behaviour related interventions
India
(%)
Chhattisgarh
(%)
1
Three or more ANC
52
54
2
Institutional delivery
39
14
3
Percentage of Children who started breast feeding within
one hour of birth
25
4
Percentage of Children who received a prelacteal feed
23.3
5
Immunization coverage
44
49
6
Contraceptive prevalence rate
56
53
7
Spousal Physical and sexual violence
37
30
Source – NFHS-3, India (Ministry of Health and Family Welfare, GOI)
All of above mentioned problems need preventive as well as curative care aspects of health
problems which must be addressed through appropriate BCC/IEC approach It means we need
to do BCC/IEC :
To change the behaviour of the community for the preventive aspect of the above
mentioned problems
NRHM PIP 2009-10: Chhattisgarh
Page 180
To inform the community on the available services/ programs/benefits like JSY,
TSC,NVBDPC,RNTCP,NLEP etc
High prevalence rate of malaria, filaria and sickle cell anaemia indicates the magnitude of the
problem in the state that can be reduced through behaviour change approach. All these need
area specific strategies for the positive change, like to motivate the people through behaviour
change communication for the use of bed nets, avoid water logging in and around habitation
area and collection of garbage in a common place away from the habitation. The approach
would be adopted to impart attention precise to the district wise existing problems in focused
manner.
Use of BCC has been one of the key components in any health sector strategy. It is essential to
modify risk prone life styles and practices to promote healthier lifestyles and practices. In past
the state have had many major rounds of social mobilizations and awareness generation which
have helped to take key health messages to even the most interior of the rural areas. Still there is
a lot of space for the improvement.
Objectives
To have functional BCC/IEC cell at state /district level
To improve the awareness of the community (empowering the family and individuals to
take health related decisions based on information and analysis) on the available health
services it will lead to better utilization of services
To enhance the involvement of the community in the existing programs and community
level process like immunization, institutional delivery, TSC, NVBDPC, RNTCP
VHSC,VHND etc to improve the outcomes and the quality of the program .
Strategies
Establishing BCC/IEC cell at the state and district level
Convergence and coordination with various departments like W&CD, health, PHED,
Education, CGSACS and Panchayats etc
Capacity building of government functionaries on BCC
Integration of health messages with various departments
Research on community/ area specific issues and best practices
NRHM PIP 2009-10: Chhattisgarh
Page 181
Women Health Committee(WHC), VHSC and Mitanins will be instrumental in
facilitating the process and activities at community level
Establishing monitoring /evaluation mechanism
Activities
The BCC/IEC cell will be set up at the directorate. The human resource (HR) of BCC/
IEC cell would be comprised with the government functionaries as well as non-govt
functionaries. To establish BCC/IEC cell will need to have necessary equipments like
computers with adequate software back up for designing, printers, printing materials,
stationeries and furniture etc. Strengthening of the BCC/IEC cell will be done by in
sourcing technical experts of the subject like nutrition, communication, medical doctors,
graphic artist and designers for the effective designing of the communication strategies
etc. The function of the BCC cell would be
To design the behaviour matrix- communication strategies and media materials in
order to ensure in-house production.
The in-house materials production (films, radio programs, posters, Kalajathas,
etc) this will serve as reference materials on health and will be used by other
department for IEC.
The cell has to make operational framework for BCC.
It will work in coordination with the other relevant departments by incorporating
the ideas and components relevant to the context of the subject.
Intersectoral coordination for BCC on common intervention with W&CD, PHED,
Education, Health, SCERT, Unicef, CGSACS Doordarshan etc
Supporting the district BCC/IEC cell in establishing /implementing the different
activities
In the same way the BCC /IEC cell would be in place at the district level ( in 18 districts)
Organizing IEC activities through Women Health Committee (WHC) at hamlet level and
VHSC at village level .Also the IEC activities will be organized at the state level by using
Rajyotsav, exhibition on 26th Jan etc as platforms
Developing area /community specific IEC materials for different age groups- by social,
linguistic and ethnic characteristic
NRHM PIP 2009-10: Chhattisgarh
Page 182
Increasing participation of various stakeholders in VHND
Coordination with various departments through sharing of information’s, documents and
ensuring their representation where required.
Major emphasis would be given on awareness generation on behaviour change. The
action planned for this is to use combination of mediums for the reach and penetration of
the messages. Optimization of KALYANI- a health program (sponsored by GOI) on
television would be one of the focuses for the dissemination of the key messages of
NRHM. Radio would be used as a strategy at the district level for the penetration of the
messages and for the dissemination of the district specific messages
State / district level monitoring /evaluation mechanism and its linkage with HMIS system
The role of SHRC (State Health Resource Centre) will be to conduct research,
development of BCC matrix, create media archive produced on BCC. The collection of
records, documents, clippings will serve the purpose of resource materials on BCC.
Comprehensive approach shall be taken up to address the health related problems like
imparting life skill education to the adolescent groups, distributing BCC kit to the
Mitanins, using combinations of mediums for the dissemination of the messages .
Establishing regular monthly meetings of the Women Health Committees and VHND at
the village level
Mainstreaming gender and equity and strengthening governance through BCC strategy
Indicators
No of different workshop/training conducted at state/district level.
Functional BCC cell at the state and district level
No of BCC/IEC materials( radio programme, films and posters etc) produced
No of Mitanins using BCC kit
No of hamlet/village and VHSC meetings organized
No of operational research conducted
No of program telecasted in coordination with KALYANI
No of area specific BCC/ IEC developed
No of indicators related to BCC addressed in HMIS
NRHM PIP 2009-10: Chhattisgarh
Page 183
The budget allocation in the previous year PIP 2008-09 amounting to 2.579 crore (amount of
Rs 97.3 lac will be utilized by March end of 2009 and Rs 1.6 crore will be carry forward for the
PIP 2009-10).
Additional Budget Requirements: Along with the activities mentioned in the PIP of 2008-09 few
additional activities (old/new) has been taken. For these activities, the budget requirement is as
below:
*The comprehensive IEC plan attached in annexure
Table 2.49: Additional Budget Requirement for BCC/IEC
Sl. No Unit Description
Unit
cost
No.
Duration Total Cost
of
Units
1
State Level /District level BCC cell
500000
1
1
500000
2
Training and exposure visit to other places 25000
( state /districts)
50
-
1250000
3
Research on BCC ( area /community 5,00000
specific issues), Monitoring & Evaluation
4
Printed and AV material (posters, bulletin, 1000000 1
success story reports, health calendar,
Quarterly magazines & diaries etc)
1
1000000
5
Block level BCC interventions (including 4 50,000
urban areas) (Radio, Kalajathas and for
IEC strategy dissemination)
150
1
7500000
6
State Level events
1
1
800000
7
District Level events( Radio, TV, AV, 50,000
Human Media as per IEC strategy
dissemination)
18
1
9,00000
Media Ads on various related health days
12
1
2400000
Total
NRHM PIP 2009-10: Chhattisgarh
800000
200000
5,00000
1,48,50,000
Page 184
Programme Management:
This shall occur by five institutional arrangements that are delineated below. Each of these five
bodies requires careful planning at the level of governance, specifically in allocation of powers.
They need to be able to function with a higher degree of autonomy, decentralisation of powers
and professionalism. The RCH proposal proposes ways and means and budgetary estimates to
strengthen each of these levels. We have adopted the norms suggested for district health societies
staffing. For the state health society, we would need additional technical expertise and hence the
proposed staff would be incorporated within the budgetary outlay we have already suggested.
Institution
Function
Programme Management Institution
Strengthening of the NRHM Initiatives
through strengthening Directorate of
health Services and PMU under RCH-II
Strengthening of the State Health Society
NRHM PIP 2009-10: Chhattisgarh
Administration and Human Resource Issues
Infrastructure Management Cell
Procurement and Distribution through a
separate cell for the same – to be made into an
autonomous body.
Implementation of all technical components of
the RCH and disease control programmes
Monitoring and evaluation of all programmes
Support and monitoring of Jeevandeep Samitis
Financial Management related to programmes:
NGO Programmes
Public Private Partnership Programmes
State Consultants Maternal/ Child Health
Issues
State Consultant – BCC/IEC
State Consultant- Infrastructure Cell
State Consultant – Procurement expert
State Consultant Demography expert
State Consultant – Training Expert
Page 185
Strengthening of the District Health
Societies
Strengthening the Block level programmes
State Consultant – Monitoring and Evaluation
Implementation of Programmes of RCH
District and Block Level Plan development.
Setting up a block PMU
Strengthening HMIS at block level through
computerised data flow
Mobility support
Technical Assistance Institution
The State Institute of Health and Family
Welfare
Strengthening of
Resource Centre
the
State
Health
NRHM PIP 2009-10: Chhattisgarh
All Training Programmes
development in all employees
and
capacity
Mitanin
Jeevan Deep
FRU Technical Assistance
All community level capacity building
initiatives like Swasthya Panchayat Yojana,
VHSC etc.
Community level capacity building
Operational Research and Policy related
Studies:
Programme evaluation studies
Assistance in
development
Support to implementation of effort and
process intensive innovation- especially on
nurse practitioner, Mitanin certification,
vocational ANM stream and multiskilling,
public health management distance education
training and district level planning
Developing comprehensive innovative models
Policy
and
programme
Page 186
for malnutrition reduction
Support in deriving a viable model for HMIS.
The proposal envisages strengthening each of the above three management institutional
mechanisms and two technical assistance agencies along with the establishment of an innovative
Health Management Information System. There is also a special focus on improving financial
management. At the state directorate and NRHM PMU level, the proposal is for 8 consultants as
against six who are functional today. Further, there is a proposal for continuing the district
PMUs as already are in place. To this is added a provision for a block PMU. The budgetary
projection for SIHFW is meant to start the SIHFW functioning on an outsourcing basis- as a
turnkey arrangement – so that after three years it can function autonomously. The budgetary
provision for this by then would be absorbed by the state government with the approval of the set
up for the SIHFW. The SIHFW shall coordinate all training activities and institutions in the state
and ensure the implementation of the HRD policy as regards in service training. The SHRC
support has been assured a three-year term under an MOU between the government of
Chhattisgarh and the SHRC. Two more years of this MOU exist. This support is as envisaged in
the MOU and is as approved in the RCH-II PIP. This is essential for continuing the SHRC’s
support function- both for community programmes and for capacity building. Moreover, for
providing technical assistance to programme and policy design and for support to
implementation of innovative, effort and process intensive new programmes.
Table2.50: Budget Estimate for Programme Management
S no
Unit Description
Unit
cost
No.
of Duration
Units
Total Cost
A
Strengthening State PMU & NRHM
Secretariat
1
State Programme Manager
35000
1
12
420000
2
State Maternal/Child Health officer
34500
1
12
414000
3
State BCC/IEC Officer
25300
1
12
303600
4
State Human Resource officer
25300
1
12
303600
5
State Infrastructure officer
25300
1
12
303600
6
State Procurement officer
25300
1
12
303600
7
State Demography officer
25300
1
12
303600
NRHM PIP 2009-10: Chhattisgarh
Page 187
8
State Training officer
25300
1
12
303600
9
State HMIS officer
25300
1
12
303600
10
State Monitoring/Evaluation officer
25300
1
12
303600
11
State Finance Manager
30,000
1
12
360000
12
State Accounts Manager
25300
1
12
303600
13
State Data officer
23000
1
12
276000
14
Office hands (including 3 accountants)
9200
16
12
1766400
15
State level Travel of PMU officials 57500
Mobility
1
12
690000
16
Interstate
travel
Programmes
1
1
575000
17
Office Establishment/ Contingencies
1
12
2760000
A
&
Exchange 575000
230000
Sub Total
9993800
B
Strengthening District PMU
1
District Programme Managers
28750
18
12
6210000
2
District Accounts managers
20700
18
12
4471200
3
District Data officer
18400
18
12
3974400
4
Consultants for Assisting short term 28750
technical tasks(Assignment based)
18
4
2070000
5
Accounts Assistant
11000
18
12
2376000
data Assistants
11000
18
12
2376000
6
District Level Mobility of PMU officials
11500
18
12
2484000
6
District level PMU Coordination & 18400
Contingencies
18
12
3974400
Sub Total
NRHM PIP 2009-10: Chhattisgarh
27936000
Page 188
Total of salary Part-A+B
NRHM PIP 2009-10: Chhattisgarh
37929800
Page 189
Equity/Gender
A number of indicators show that interventions in NRHM in Chhattisgarh has to an extent
improved women’s access to healthcare but we still have a long way to go. NHFS 3 data shows
that percentage of mothers getting three ANC visits have increased from 33% to 55%. Still 43%
of women are underweight, 59% of women have anaemia, with 18% having moderate to severe
anaemia. More starkly, anaemia in women from Scheduled tribes is as high as74%.
Early age of marriage continues to be a grave concern with almost half the girls still getting
married before 18 years. This has serious consequences not only on their health but also for
their status in society.
NFHS 3 shows that almost all currently married women and men know of female sterilization;
and most know of male sterilization. The contraceptive prevalence rate among currently married
women is 53 percent, up from 45 percent in NFHS-2. The level of contraceptive use in
Chhattisgarh is quite close to the prevalence of the nation as a whole (56%) but still 10 percent
of married women in Chhattisgarh have an unmet need for family planning.
Deliveries by a health professional has increased from 32% to 44%, though only 14% of births
are taking place in medical institutions, which is the second lowest in the country (NFHS 3).
Overall, 30 percent of ever-married women have experienced spousal physical or sexual
violence from their husband with 13% percent report having ever experienced spousal emotional
violence. However, amongst them, as much as 70% of women have neither sought help nor told
anyone about the violence (NFHS 3).
Therefore, we see that though we have made headway in improving women’s access to health
services, the basic causes behind higher mortality and morbidity in women, remain. Hence in
order to bring about gender equity in health, our strategies have to address both practical needs
(short term need related to daily needs: food, housing, income, health of family etc) and strategic
needs (long term needs relate to disadvantaged position, subordination, lack of resources and
education, vulnerability to poverty, violence etc). This means that a plan, in addition to involving
women as beneficiaries and participants in order to improve the condition of their lives, should
also involve and enable them as agents in the process of improving the position of women in
society and transforming gender relations.
The interventions in Chhattisgarh incorporated both these aspects. There is a renewed
commitment to improving women’s access to quality healthcare by strengthening facilities to
provide Emergency Obstetric Care (EmOC), training Skilled birth attendants, multiskilling of
Doctors in EmOC and Anaesthesia, streamlining Janani Suraksha Yojana, introduction of the
NRHM PIP 2009-10: Chhattisgarh
Page 190
JSY help line, recruitment of staff nurses and ANMs, operationalisation of 24hour PHC etc. An
important proposal that has been made this year is that of formation of Maternal and Infant
death auditing committees. For pregnant women in disease prone areas, special ANC kit with
impregnated bed nets and IFA has been planned.
Interventions like Mitanin programme, formation of women health committee and village health
sanitation committee (Convener of VHSC is Mitanin) at village level, has show the way for
leadership building and women’s empowerment. The Mitanins have emerged as women leaders
taking forward and fighting for gender equity. Formation of women’s health committees at the
village level has led to addressing the issues of gender and equity like women exclusion,
discrimination, violence, marginalisation, alcoholism and destitution etc. Activities like Mitanin
diary under Mitanin programme are also focused to address the problems of social exclusion,
marginalisation and health entitlements at the hamlet level. Programmes like Swasthya
Panchayat Yojana and village heath sanitation committee aim to tackle the disparities at hamlet,
village and Panchayat level. It is a mechanism to address the issues related with equity and
gender. It is also an attempt to overcome inter and intra Panchayat variations and disparities.
Making the Mitanin the Convener of VHSC is a further step forward to creating spaces for
women for the proper inclusion of their issues in village health plan with an ownership over
community resources. Peer education on adolescent and reproductive health has been a step
forward to create rooms of expression for adolescent girls to state their problems and queries.
Financial management
There are still a number of issues to be improved under this- receiving, releasing and spending
grants according to work plan as well as getting and giving over the UCs in time, presentation of
FMR in the desired time and structure all these are being improved and the state shall be
fulfilling this within a specific timeframe. The state accounts manager positions has recently
been filled and necessary hands are being given to the financial management cell. At the
districts, focus shall be there to those districts where DAMs are not posted. These vacancies
shall be filled by 2nd quarter. Audit for the last financial year has been commissioned and we
expect this shall be completed within time. The lacunas in financial reporting shall be addressed
immediately. The procedures and guidelines shall be strictly adhered to- some variations in last
year from the structured guidelines has been indicated which shall be taken care of in future.
Convergence/Coordination
Very effective coordination has been achieved among all other convergent sectors/departments
with health. This includes women and child development, Panchayati Raj, Public Health
Engineering, social welfare, civil supplies etc. The Swasth Panchayat Scheme, Village health
and sanitation committee, Village untied fund with ANM-Sarpanch joint bank operation all has
improved this and the district-state missions as well as Jeevan deep bodies right from the PHC
level is also an icon for this. The functional issues to be sorted out between these departments
NRHM PIP 2009-10: Chhattisgarh
Page 191
shall be looked at and resolved in, time to time. The state society meeting and different working
groups as needed shall bind this coordination to further strengths. Convergence must take place
at the level of policy making, planning, framing of programmes and schemes and their
implementation at all levels. Absence of such convergence at higher levels leads to
‘verticalisation’ in various health programmes, which in turn leads to wastage of money, time
and effort as well as needless overlaps.
Thus, the convergence and coordination should be incorporation from the level of the state
stakeholders to the block and village level. These could be the Mitanins, ANMs, AWWs, SHGs,
PRIs and others from the village level and the BDOs, MOs, BMOs and other block officials. At
the district level, the District Commissioner, Collector, DPMU, DHS, CDPOs (ICDS), CEOs and
others. And at the State level the SHS, PHED, State Electricity Board, PWD etc. All these in one
way or the other contribute and are interdependent and complement each other.
The Regional Resource Centre is facilitating for the implementation of RCH II activities by
MNGOs/ FNGOs under NRHM at the underserved and underserved areas and it is providing
technical capacity to these organizations.
MNGO / FNGO Programme in Chhattisgarh:
MNGO scheme is one of the programmes under NRHM. Under this programme, the MNGOs are
appointed at district level that build the capacity of the FNGOS and facilitate them and FNGOs
are appointed at block levels that intervene in the villages. These organizations work at unserved
and underserved areas, as notified by the District Health Society, to generate community
demand for availing modern medical facilities provided under NRHM by the beneficiaries
(Eligible Women, Children and Adolescents). Mean while the Service NGO scheme also works
under same pattern that provides the service delivery at the areas where the demand is
generated. The programme is coordinated by a full time State NGO Coordinator at department
level and the MNGOs are technically supported by Regional Resource Centre. MNGOs and RRC
are appointed by the Ministry of Health & Family Welfare, GOI, and FNGOs are appointed by
the MNGOs with due approvals from District health Societies. MNGOs/FNGOs will work for a
period of three years for the funds are provided by the State Health Society in three instalments
for 18 months, 12 months and six months. The size of funds is in the tune of Rs 15 lakhs per
annum per district. The indicators which these organizations will be working are Institutional
delivery, Complete ANC, Immunization coverage, RTI/STI incidence, Family Planning usage,
Delivery by skilled Birth Attendance etc.
In the state of Chhattisgarh there are Nine MNGOs appointed covering 16 districts and No
service NGO and full time State NGO Coordinator have been appointed so far. Population
Foundation of India is appointed as RRC for the state. Regarding the progress of the MGO
scheme, Six MNGOs covering 10 districts were given the first instalment and rests are pending
due to lack of funds. These six MNGOs have 41 field NGOs appointed with due
NRHM PIP 2009-10: Chhattisgarh
Page 192
recommendations of District health Society respectively. They have been working in the state
covering approximately 800 villages. Another 21 Field NGOs were appointed but they are yet to
receive the funds. The disbursement was made on April 2008 and the RRC has conducted the
first half-yearly review in the Month of September 2008. All the organizations were provided
with reporting formats. FNGOs will be submitting the reports on a monthly basis and MNGOs
will be submitting the reports in quarterly basis. In addition, the MNGOs / FNGOs have to
submit quarterly Statement of Expenditures that is being submitted time to time by all MNGOs
and FNGOs. Regional Resource Centre has been validating the activities of the MNGOs/FNGOS
and submitting reports to State health Society time to time.
Monitoring of the programme has to be done at three levels such as – at block level by the
MNGO for FNGO activities, District Health Society at district level for MNGOs and the central
ministry will do an external monitoring. The State government can undertake interim monitoring
if required.
In the current financial year evaluation and monitoring exercise will completed for the budgeted
FNGO – MNGO on the basis of the conclusions a separate proposal for re-appropriation of
budget will made for it require.
Establishment of procurement cell
Procurement is one of the important aspects in the management of the supply of drugs,
equipments and other necessary goods. Quality assurance and responsible delivering supply of
goods is need quite technical as well as managerial skills. For that establishment of procurement
cell is most important. In the procurement cell, the procurement cell will be consisting with a
team of expert, as follows. Procurement consultant (budgeted in Part-A) Pharmacist, Bio
medical engineer, programmer, and data assistant.
Note: NRHM programme will support the DFW procurement cell the budget will be born from
EUSPP so there is no separate budget required.
District and Block Plans
Block plans are being envisaged and is in the process as BPMUs are in place. On the other
hand, the village health plans (Panchayat Health Plans under Swasth Panchayat) has started to
be formulated and implemented in many Panchayats. First draft is ready of district health plans
of all the districts that are being revised according to the national guidelines and state level
appraisal. These exercises shall be completed by February end.
Definition of Roles of Each Levels
The Profile of SPMU and DPMU as well as BPMU members have agreed and issued. The
contracts of these consultants are being renewed for the next financial year. Other than the
NRHM PIP 2009-10: Chhattisgarh
Page 193
PMUs, the state has further going towards decentralisation and delegation of powers, where
BMO post has been created as a class I post with financial/admin powers. At the district levels,
programme officers are also been placed in the same way.
Synergy with other NRHM Components
The NRHM and RCH coordination at the state is done by the same PMU and society, working
under complete ownership of the health directorate and district health departments. The
coordination with various disease control programmes and convergence is quite good; however,
it needs strong synergy. The completion of merger process of societies and related procedures
shall do this better.
A number of NRHM Additionalities have the potential to have a synergistic impact on
achievement of RCH II goals. The state shall ensure that - the Mitanin (ASHA) spends sufficient
time on RCH related activities. RCH II is perceived as high priority by Rogi Kalyan Samitis
(RKS) and its funds are appropriately allocated to improving delivery and utilization of RCH
services especially by the vulnerable
The State and District Health Missions and integrated health and family welfare societies spend
sufficient time on RCH II and ensure that barriers to effective implementation of RCH II are
addressed. Significant percentage of the untied grants for local health action at sub-centre, PHC
and CHC are used for improved delivery and utilization of RCH II related services
It further encompasses the disease control programmes and integration with nutrition, water and
sanitation in an effort to address determinants of health and better utilization of resources. These
NRHM initiatives/ “Additionalities” would have a synergistic impact on achievement of RCH II
goals/ outcomes:
Community mobilization for health action: Provision of a need based, trained and supported
village Accredited Social Health Activist (ASHA) who will create awareness on health and its
determinants; mobilize the community for local health action and act as the interface with the
health service delivery system.
Capacity building of PRIs to own, control and manage public health services through transfer of
assets and delegation of administrative and financial powers. Flexible/ untied funds for local
health action: Rs 10,000/25,000/50,000 at SHC/PHC/CHC levels respectively. Support for
ensuring that selected health facilities perform to predetermined (IPHS) standards
Elaborate institutional arrangements consisting of National Steering Group, Mission Steering
Group, State and District Health Missions, single Health Society at state and district. The
National Steering Group is chaired by the Prime Minister, while the State and District Health
Missions are chaired by the Chief Minister and Minister-in –charge of the district respectively.
These institutional arrangements are expected to lead to improved ownership of plans and more
NRHM PIP 2009-10: Chhattisgarh
Page 194
optimal
utilisation
NRHM PIP 2009-10: Chhattisgarh
of
sectoral
resources.
Page 195
PART B: SPECIAL INITIATIVES UNDER NRHM
Introduction:
The NRHM part B or flexi-pool component is guided by the National Rural Health Missions
Framework for Implementation. The aims and objectives of this Mission are well thought and
need proper implementation by the executives.
During year 2007 – 08 Chhattisgarh had an unspent amount of Rs. 88.53 Crores and received a
sum of Rs. 33 crores for the financial year 2008 – 09 for Part B flexible pool. However, due to
several reasons, only Rs. 8.31 crores has been spent as on 31 December 2008.
We have therefore proposed for only the following items:
1. Strengthening Routine Sub-Centre functioning
2. Alternative Clinical Human Resources Development through ANM production and
improving Nurse Training Facilities.
3. Vocational Stream of ANM training as a part of Higher Secondary Schooling for Tribal
Areas
4. Establishment of Nursing college in Tribal area
5. Filling Gaps in Rural Medical Services using the three year Medical Training
Programme Going on in the State.
6. Support in creation of Rural Medical Corps in remote and difficult (conflict) areas of
Chhattisgarh.
7. Reservation of candidates from tribal areas for Nursing and ANM course
8. Closing residential and accommodation gaps
9. Nutritional Support for patients with Tuberculosis
10. Distribution of Insecticide treated bed nets for families in high risk tribal areas
11. Strengthening the Mitanin Programme
NRHM PIP 2009-10: Chhattisgarh
Page 196
12. Strengthening the Village Health and Sanitation Committee
13. Behaviour Change Communication
14. Village and Panchayat Level Capability Building
15. Block level Programme Management
16. Monitoring and Evaluation
17. Civil work for Sub centre , Primary Health Centre and Community Health Centre
18. Community Based Monitoring of Health Services
19. Sickle Cell Anaemia
20. Ayush components
21. Third Party Monitoring
22. Filling up vacancies and HR management
Outcomes for Disease Control Programmes
1. Complete implementation of national programme guidelines
2. Integration into district plans
3. Achieving IPHS norms of service delivery in all sub-centres, PHCs and CHCs and
district hospitals by the year 2012.
Sub-centres:
1. Untied funds to sub-centres.
2. Refresher training for staff.
3. Closing infrastructure gaps.
4. Two ANMs per sub-centre.
5. Strengthening monitoring and support
PHCs:
1. Untied funds to PHCs
NRHM PIP 2009-10: Chhattisgarh
Page 197
2. Making Jeevandeep Samitis operational and effective.
3. Multiskilling paramedicals.
4. Implementing policy for filling vacancies in underserved areas.
5. Closing infrastructure gaps.
6. Operationalising newly sanctioned PHCs.
CHCs:
1. Making Jeevandeep Samitis operational.
2. Untied funds to CHCs.
3. Multiskilling for specialist skills to close gaps for emergency obstetrics gaps.
4. Training to ensure all CHCs have capacity to do NSVT and CT and that there is
sterilisation services available on a fixed day per week.
5. Closing Remaining gaps in infrastructure and equipment.
District Hospitals:
Same as for CHCs
For Community level first contact care available to all1. Strengthening the Mitanin programmes:
2. Adequate curative skills for improving child survival to certifiable levels.
3. Linkage with open schools for certifying qualified Mitanins with CHW certificate.
4. Linkage with nurse provided institutional delivery services.
5. Better linkage with ICDS programmes.
6. Health planning and monitoring plan implementation in all villages under the swasthya
panchayat yojana.
Reduction of child malnutrition levels
1. Improved ICDS outreach and effectiveness.
NRHM PIP 2009-10: Chhattisgarh
Page 198
2. Linkage between Mitanin ANM and AWW to be strengthened by joint training.
3. Major BCC with focus on complementary feeding and 6th to 12-month period.
4. All grade III and grade IV to get medical referrals.
5. Institutional care for sick malnourished children.
Filling the HR Gaps
1. Vocational streams for creating ANMs in underserved areas
2. ANM and nursing schools in every district.
3. Special training for Ayush doctors in PHCs.
4. Multiskilling paramedical and medical officers.
5. Special incentives to work in difficult areas.
6. Creation of transfer policy and its implementation.
Decentralisation of health services and increased public participation in all health
services
1. Major focus on district planning.
2. All villages to have village health plans with measurable indicators and monitoring
mechanisms.
3. Capacity building for public representatives on district committees and on hospital
committees.
Professionalization of Management:
a. Bring all programme officers and block medical officers under public health
management programme.
b. Induct district programme managers, block programme managers, and train them in
house on public health management.
c. Improve functioning of all district and state health societies.
d. Put in place professional leadership and staff for SIHFW and district training centres.
NRHM PIP 2009-10: Chhattisgarh
Page 199
Jeevan Deep Samitis: Making PHCs and CHCs fully functional
Situation Analysis:
Provision of infrastructure, plus manpower plus training plus equipment does not add up to
increased quantity or quality of services. Between central and state government, over the RCH-I
and RCH-II programmes there has been an investment of about Rs 10 crores into infrastructure
of these 100 CHCs. For this investment to be converted into actual improvements in services, we
need to invest in some management and motivational processes and resolve along the way a
number of systems issues that arise. The Rogi Kalyan Samiti, which was functional in District
and Community Health centres before Jeevan Deep Samiti, was fulfilling the task of Hospital
Management Committee. As on today, 580 out of 679 facilities concerned have completed the
registration procedure of Jeevandeep Samiti and completing their meetings. Annexure 2 shows
the financial status of these Rogi Kalyan Samiti (Now Jeevan Deep Samiti) in the financial year
2006-07.
Objectives:
In this situation, we are providing funds for:
a) Improved quality of care in 136 CHCs plus 18 district hospitals, all PHCs and sub
centres in these blocks.
b) Ensure that all CHCs and PHCs in these blocks are functioning as 24 hour PHCs of
IPHS standards
c) Ensure that the services provide for equitable access and are woman friendly and
adolescent friendly.
An investment of about Rs 12 crores in the form of untied funds placed at the disposal of the
facilities , and this is used to not only gaps but also stimulate public participation and
accountability is well worth it and could accelerate attainment of quality in each of the facilities.
Key Operational Elements:
a) There would be a participatory hospital management committee built up for all CHCs,
PHCs and district hospitals. This is already achieved.
b) Design quality of care standards and quality of care indicators as applicable to PHC and
CHC and sub centres, including indicators for gender sensitivity and equity in access.
NRHM PIP 2009-10: Chhattisgarh
Page 200
c) Participatory micro planning to ensure that all employees in these blocks understand the
quality standards and identify constraints in closing the gaps: including gaps in minor
equipment. This is facilitated by technical assistance agencies for each district.
d) Initiate and support hospital committee level group processes that will address
motivational and attitudinal issues.
e) Close gaps in infrastructure, manpower and skills and equipment along with measured
improvements in quality.
f) Address all local level “systems” problems- like linkages to a functional ambulance
service, designing a viable referral system, getting access to blood organized, ensuring
that the referral fund through Mitanins is fully utilised. It also requires motivational and
management inputs.
a) At the end of the two years these FRU facilities should provide adequate quality of the
following:
a. Access to Basic and comprehensive Emergency Obstetric Care Services
b. Better quality ANC and post partum and neonatal care,
c. institutional neonatal and sick child care,
d. Reduce unsafe abortions;
e. Improved RTI/STI services with utilisation of referral system and
f. ambulance and laboratory services needed to support this set of interventions
b) The performance of the hospitals would be rated by an independent agency, they would
be accredited using a star rating system, and the best performers would be rewarded.
c) Annual facility development plans shall be made by the society in order to fulfil the gaps
found as part of the assessment and to achieve the various benchmarks on quality norms.
Each district hospital and Civil Hospitals would get a grant of Rs 5 lakhs each and, each CHC,
PHC, would get a grant of Rs one lakhs each from NRHM flexi-pool. To ensure however that
these funds made available under NRHM are used in the manner outlined above we need to
deploy technical assistance agencies whose funds need to come from the RCH-II flexi-pool. This
could be used for following purposes:
a. Renovation or even new construction to ensure that there is conformity to
IPHS standards. Similar standards would be built up for PHCs as well.
b. Improving residences of staff.
NRHM PIP 2009-10: Chhattisgarh
Page 201
c. Buying equipment to close gaps.
d. Local purchase of drugs for the poor.
e. Payment towards fees for the poor to the Jeevan Deep Samiti account.
f. Motivational meetings and training for the Jeevan Deep Samiti members.
As per NRHM the J D Samiti should receive seed fund of 5 lakhs each for District Hospitals and
Civil Hospitals since there is a larger issue of maintenance and improvements, Rs 1 lakh for
each CHCs and PHCs .
Each Jeevan deep Samiti after performance evaluation would draw up an annual plan and work
to implement it and achieve necessary standards.
For strengthening the Jeevandeep Samiti and general administration of the hospital this year it
is proposed to deploy one Hospital Administrator with Civil Surgeon, for each district hospital .
In addition to this for the operationalisation of FRUs and CHC Jeevandeep Samitis, a technical
person like doctors or people with preferably background of hospital management should be
appointed. These persons will help them operationalise the FRUs/CHCs with the help of
Jeevandeep Samitis. For bigger districts, 2 persons may be appointed. In difficult areas, the
salary package may be slightly higher. This can be out sourced to some agency also.
Table 3.1: Budget Estimate for JDS
S. no Particulars
Unit cost
No of unit
Total Cost
1
District hospital/Civil Hospitals
untied fund
500000
36
1,80,00,000
2
CHC untied fund
100000
136
1,36,00,000
3
PHC untied fund
100000
721
7,21,00,000
4
Orientation workshop of JDS
20000
146
29,20,000
Total
106620000
Table 3.2: Budget for maintenance grant for SHCs, PHCs and CHCs:
Sl. No
Particulars
Unit cost
No. Of units
Total Cost
1.
SHCs
10,000
4741
4,74,10,000
2.
PHCs
50,000
721
3,60,50,000
NRHM PIP 2009-10: Chhattisgarh
Page 202
3.
CHCs
1,00,000
136
1,36,00,000
Total
9,70,60,000
Strengthening Routine Sub-centre functioning
Every sub centres will have Rs 10,000 in joint account of Sarpanch and ANM to reduce the out
of pocket expenditure for routine work. This fund will be utilized for proving transport facility for
pregnant mother, incentive to Dai, purchase of consumables, disinfect the facility after delivery
etc. It could also be used to observe the health and nutrition day in a fitting manner.
Another Measure to strengthen the sub centres is to place a second ANM in the sub centres. For
this, Provision of second ANMs in proposed priority area. Second ANM to be introduced in all
sub centres in tribal blocks, which is not co-terminus with a CHC or PHC and the absenteeism,
is not a problem over there. Second ANM also to those sub centres catering to population of
more than 6000 based upon mapping. This is estimated at 30% of sub centres. Another 10 % sub
centres where ANM position is vacant, we need to provide at least one ANM also. Hence, the
additionality is estimated at 40% for the current year, in the salary and personnel heads.
Table 3.3: Budget for Strengthening Routine Sub centre Level Services
Sl. No Item
1
Unit
cost
Untied funds
functions
for
sub
Sub Total
centre 10000
No.
Units
4741
of Duration Total
budget
1
4,74,10,000
4,74,10,000
ISO Certification
Public hospitals are the only available social protection for the poor from disease, disability &
death and from escalating healthcare costs. However, for too long poor quality of public health
institutions and services provided through them have been matters of serious public concern.
Shortage of facilities, increasing workload, ineffective systems and processes are making things
difficult for providing quality service. Although the poor quality of services and infrastructure of
public health systems has been attributed to poor motivation of the workforce, yet, there is
growing recognition that the main causes of poor quality of public health systems are systemic –
a reflection of both quality of hospital management and of public health administration. Patients
often complain about the quality of services provided in the public health sector. Poor quality is
causing loss of customers, loss of lives, loss of revenue, loss of material resources, loss of trust,
wastage of time, and recognition.
NRHM PIP 2009-10: Chhattisgarh
Page 203
Though the private healthcare providers profess themselves as champions of quality of care, they
fail to address the equity concern, leaving majority of the population outside its network.
Therefore, improving the service coverage and quality of care of public health systems has to be
undertaken by the government, who is obliged to provide the healthcare services to the
population.
The challenge before the government is of establishing a system that maximizes the output in
terms of services offered and quality of care provided with available human resource, equipment
and supplies. The process of ISO certification of Korba district hospital (Indira Gandhi District
Hospital) has been an effort in this direction. It has been a major achievement for the
department of health & family welfare, Chhattisgarh, when it became the first ISO 9001:2000
certified district hospital in the country. The key technical players who helped the state to
achieve this distinction are National Health Systems Resource Centre (NHSRC) and HOSMAC.
The success of this hospital has motivated the state to undertake such activities for every hospital
in Chhattisgarh. During the year 2009-10, the state proposes to undertake this process to three
district hospitals and four community health centres, namely, district hospitals of Durg,
Ambikapur and Bilaspur & four CHCs of Durg district.
However, a considerable sum of money is required, for this purpose. The expenditure is incurred
under two major heads namely, onetime process cost and three years’ handholding cost. There is
also an additional cost of refurbishment.
Table 3.3A: Budget support for ISO certification process
S.
no.
Facilities
Activity
Units
Onetime
cost
Handholding cost/ per year for a
period of three years 2010
onwards
Total cost for
first year 200910
1
District
Hospital
ISO
certification
3
20,40,000
13,80,000
61,20,000
2
CHC
ISO
certification
4
6,52,750
4,26,300
26,11,000
3
District
Hospital
Up gradation
3
1,00,00,000
-
Other source
4
CHC
Up gradation
4
30,00,000
-
Other source
5
*The cost of ISO certification is according the norms of Government of India and there
will be additional costs for service tax and audit.
Grand Total for 2009 – 10
NRHM PIP 2009-10: Chhattisgarh
2,69,000
90,00,000
Page 204
*The cost of auditing may vary and gap would be settled through administrative cost under NRHM
**The cost of up gradation includes the cost of renovation and refurbishment, based on the need of the institutions,
under the control of the State.
Assistant Auxiliary Nurse Midwives:
ANMs are the most peripheral outpost of Primary Health Care and Village Panchayats as the
lowermost democratic governance unit, an attempt will be made to fill up this gap by linking
both and nurture an ownership of ANM with an additional ANM by each Panchayat. These
additional ANMs will be recruited as assistants to the already existing ANMs. These assistant
ANMs will be will be provided a crash course training for the first initial three months and
during this period a stipend will be given to them. On completion of the crash course, they will
be recruited and will undergo on job training for completing the ANM course of one and a half
year. They will be paid a salary of Rs. 6000 per month. This means at least one ANM is to be
deployed per Panchayat. Tribal areas and with more population density should be given special
attention.
In this financial year 2009-10, we will be able to recruit 600 assistant ANMs under NRHM.180
of the candidates will be trained in 6 public facilities @ Rs. 3000 per month cost while rest of the
candidates (420) will be trained in private institutes @ Rs. 6000 per month.
These additional ANMs will be selected only from the qualified Mitanins and AWWs. The
education qualification for selection will be 10+2 (Biology).These Assistant ANMs will be colocated where ANMs are already posted and they will work under the supervision of the ANMs
with bonds. For the 1 year the selected 2nd ANM will be paid stipend of Rs1500/- per month after
the success full completion of the training course they will paid remuneration of Rs. 3000 per
month only.
Table 3.4: Budget for Assistant ANM
S.N. Unit Description
Unit Cost
No. of Units
Duration
Total Cost
1
180 Candidates for public 3000
institutes
180
12 Months
12960000
2
420 candidates for private
institutes
420
12 months
15120000
Total
NRHM PIP 2009-10: Chhattisgarh
6000
28080000
Page 205
Support for Sub centres and PHCs Infrastructure
Chhattisgarh has been putting a lot of effort and making steady progress in overall development
of the state and especially in the health sector. However, due to various constraints, development
and progress could not be made as expected. With reference to this, the state still lacks in
building and infrastructure especially those of health delivery centres. The new infrastructure
situation is such that there is still a huge gap of CHCs, PHCs and Sub centres. Most of the
existing centres operational are being used on rental basis. To build and develop this particular
sector the state has sought support from various sources apart from the state’s budget allocation
for gap filling. Though the state is receiving support from the European Commission for the
development of this sector there is still a dearth of funds for full fledge development for meeting
the need of the beneficiaries as required and the state is also committed for this. With reference
to this, the state requests fund support from NRHM flexi-pool. The requirement detail is as
mentioned.
As per gap filling requirement there is the need for 200 sub centres and 9 PHCs infrastructure
building.
Table 3.5: Budget support for Sub centres and PHC Infrastructure
S.N.
Item
Unit Cost
No. of Units
Duration
Total
1
Sub Centres
10,00,000
200
1
20,00,00,000
2
Primary Health Centres
28,00,000
9
1
2,52,00,000
Total
22,52,00,000
Appointment of Hospital Management Professionals for Public Health Facilities for
Technical Assistance:
The placement of these professionals will be in all the 18 district hospitals. The salary package
will be as per qualification i.e. 30 thousand for Diploma holders and 35 thousand per month
for postgraduate in hospital administration / MBA hospital or equivalent degree.
Table 3.6: Budget summary for Hospital Administrators recruitment
NRHM PIP 2009-10: Chhattisgarh
Page 206
S.N. Item
1
Unit Cost
Appointment
of
Hospital 30-35
Administrators to provide support in thousand/
district hospital
month
No. of Duration
Units
Total
18
7560000
12
months
Total
75,60,000
Augmentation of Clinical Human Resources: An Alternative Approach
Deficiency of qualified, skilled work force is one of the major problems dogging Chhattisgarh.
Consequently, quite a large number of facilities remain underutilised. There is dearth of not only
the specialists and physicians but also of even basic staff like ANM, MPW and staff nurses.
Migration of trained nurses to other states and abroad further worsens the situation. To
operationalise the sub centres, primary health centres and community health centres at grass
root level to bring down the maternal and infant mortality down in the state, it is necessary to
have sufficient of numbers of the above mentioned cadres.
During the financial year 2006 – 07 Rs. 15,00,000 was given to each of the existing Nursing
Training and male MPW Training centres. The expected expenditure for continuation of this
effort would go up to Rs. 5,00,00,000 during this year. This sum has been utilised for
refurbishment and infrastructural strengthening of the existing institutions. A part of the money
has been spent on purchase of audio-video teaching aids to provide training at par with other
institutes of national level.
Table – List of existing Nursing Training Institutes of Chhattisgarh.
S.
No.
Facility Level
1
2
Public
no.
(Capacity)
Private
no.
(Capacity)
Total no. Proposed & to be
(Capacity) Approved
Auxiliary Nurse & Midwife 7 (370)
Training Centre
1 (20)
8 (390)
Male
Multi
Purpose 3 (180)
Workers Training Centre
0 (0)
3 (180)
NRHM PIP 2009-10: Chhattisgarh
3 (public)
Page 207
3
Nursing
(Diploma)
Schools 4 (87)
4
B. Sc. Nursing College
5
Post
Basic
College
6
M. Sc. Nursing College
1 (50)
Nursing 0 (0)
0 (0)
4 (110)
8 (197)
6 (485)
8 (535)
1 (20)
1 (20)
2 (40)
2 (40)
*Two centres to be upgraded for LHV training at Bilaspur and Dhamtari (proposed)
** One Regional Health and Family Welfare Training Centre at Bilaspur exists.
*** 14 District Training Centres are not functional and they will be operationalised with support
from European Commission under State Partnership Programme.
Development of Assistant ANMs at Sub Centres
To train and retain, highly essential nursing staff for public health, we are proposing an
alternative approach from the oft-beaten track. We propose to train select Mitanins (the
dedicated community health volunteers, available in almost every hamlet of the State) or Mitanin
Trainers who are efficient and willing to learn as Assistant ANMs. The reasons for this
alternative approach are
1. They have sufficient knowledge about the community health aspects from undergoing
twelve rounds of training. Most of these twelve rounds of training courses focused on
maternal and child health aspects. These training courses also provided them with
adequate knowledge of planning services at local level.
2. Their improved wisdom from the experiences of working with community for last five to
seven years, will be highly useful when assessing community needs and providing the
services.
3. They also have appreciable clinical skill in primary care from providing first level
community care under Mukhya Mantri Dawapeti Scheme
NRHM PIP 2009-10: Chhattisgarh
Page 208
4. Since they are from remote, tribal areas popular with the local population, aware of the
local customs and tradition, familiar with local health seeking behaviour from their
experiences, they will be ideal candidates for such kind of training.
Selection Criteria
1. Must be educated upto standard 10 or above
2. Must have received at least 5 rounds of training till the 10th round training conducted by
SHRC. Of these, 5th round training is a must.
3. Must be willing to serve in remote sub centres
Total 1000 Mitanins or Mitanin Trainers will be selected for this purpose. The selection process
will be conducted by SHRC.
The trainings will be imparted from the institutions, private or public, functional or idle as
described above. They will receive 3 months training at these institutes on theoretical aspects
and 9 months hands-on training at sub centres under the supervision of ANMs.
Each of the 11 training institutes will have 30 candidates per session. Thus, only 330 students
can be covered during each session of 3 months. There will be 3 such sessions through which
990 candidates (say 1000) will be trained. While the 9 months hands-on field training will be
rotator.
On completion of the compulsory one-year theoretical and practical training, they will be
provided government’s diploma certificates that might be used subsequently for working as
ANMs. They will work under the guidance and supervision of existing ANMs.
Budget Summary
Sl.
no.
Activities
1
Accommodation cost
Institutes for 3 batches
2
Study material
3
Stipend
Units Unit Cost
to
NRHM PIP 2009-10: Chhattisgarh
Teaching 11
Duration
Total
50000/month 3 month
4950000
1000
1000
1000000
1000
1500 / month 12
months
1 time
18000000
Page 209
Grand Total
23950000
This will help to improve the coverage of services of those remote sub centres that suffer because
of large catchment areas with only one ANM. The expected beneficiaries of this scheme would be
poor people living in most remote hamlets, paras of forest and tribal areas "where there is no
doctor."
Developing Staff Nurse from existing ANMs
To strengthen the existing nursing capacity of Chhattisgarh further, another strategy is
suggested. Under this strategy, ANMs working with the public health systems for at least 3 years
will be promoted for higher studies of General Nursing and Midwifery (3-year course) and
thereby qualified for Nursing Staff. Under this scheme, 200 nurse staff will be developed. The
selected ANMs will be sent either to public or private nursing institutes for this course.
Selection Criteria
Must have in service, in the capacity of ANMs for at least 3 years or more.
Must not be aged over 35 years
Must have received formal education at least up to 10 +2 Standards
Must had had biology as a compulsory subject during 10+2 studies
Willing to serve the state for next 5 years after completion of the course.
Sl.
no.
Activities
1
Sponsorship
GNM course
Units Unit Cost Duration Total
for 200
Grand Total
50000/
year
3 years
Sum required
current year
for
30000000 10000000
30000000 10000000
Although the overall cost for the entire scheme is Rs. 30000000, yet for first year Rs. 10000000
will be required.
NRHM PIP 2009-10: Chhattisgarh
Page 210
Training of LHVs: Lady Health Visitor (LHV) Cadre
There are 949 sanctioned LHV posts in the state. For many years, there have been no
promotions. As per the position there are 365 existing vacancies of LHVs exist and many ANMs
are eligible to be promoted. In order to improve ANMs’ career path, filling up of LHV vacancies
is urgently needed.
In the current PIP, training of ANMs to be promoted to LHV Cadre will be undertaken. This
training will be organized in the existing Regional Training Centre, Bilaspur and one ANM
Training centre. Last Year’s budget allocation of Rs. 5000000 will be utilized for the current
year, therefore no additional budget is proposed for the same.
Tribal Health
Chhattisgarh is a tribal state (32% tribal population) with 44% of the area under forest cover.
There is quite a marked difference in the health indicators between the tribal population and
others. According to NFHS 3, Neonatal mortality and Infant Mortality Rate amongst tribal are
10 points higher than amongst other communities. In the under five mortality the difference is
much higher, that of 23 points. Malnutrition among tribal is higher. The tribal areas are highrisk malaria endemic areas. Ironically, these tribal areas, which need special and focussed
attention, are actually the most un-served and under-served areas. Poverty, geography and lack
of services have led to higher morbidity and mortality. Hence, the state faces a very grim and
challenging task to ensure better health and health care for the tribal.
Under various sections of the PIP, we have planned for activities specific to tribal areas and
addressing their needs. This section on Tribal health consists of additional interventions, which
have been aimed at improving their access to quality health care and health.
Filling Gaps in Rural Medical Services:
Utilising the ongoing Three Year Medical Training Programme in the State.
Chhattisgarh is facing a severe shortage of medical personnel to serve the rural especially the
tribal and remote areas. Continuous efforts made by the state government to get adequate
number of doctors posted in these areas failed. In tribal areas, we have permission to appoint
Ayurvedic Doctors (BAMS) in mainstream facilities but their availability is also limited. As
result, as many as 1400 doctor’s posts are vacant across the state.
Looking at this, in last year’s PIP, the state proposed that provision be made to appoint medical
personnel from the three-year medical training programme that had been initiated by the state
government and designed and run by the state universities. The state proposed that these
‘Practitioners in Modern and Holistic Medicine’ be placed (only) in Primary Health Centres as
NRHM PIP 2009-10: Chhattisgarh
Page 211
‘Rural Medical Assistant’. The plan also included post-appointment induction training of 3
months in District Hospitals and Community Health Centres, in order to ensure adequate
exposure to clinical services as well as national health programmes.
The current situation is that, out of 398 sanctioned posts, 225 have been filled and rest 173 has
been re-advertised. These Rural Medical Assistants have been placed at PHCs in tribal and
remote blocks of 12 districts. Their post appointment training is yet to be completed.
This year, the state proposes further increase the number of posts of RMAs, to be placed in
PHCs, to one thousand. A TOT for Induction training of Rural Medical Assistants will be
organised. These trainers with other district and block level trainers will train these rural
medical assistant in the respective District and Block hospitals. At present total 1400 number of
required to provide service at the level of PHCs, out of that 1000 RMA will recruit in current
year and remaining gap of 400 RMAs will be address in next financial year .this recruited
RMAs will work under the supervision of medical officer for better performance of PHC .
Table 3.9: Budget for placement and Induction Training for Rural Medical Assistants
S.N.
Unit
1
Unit
Cost
No. of Duratio
Units
n
Total cost
Placement of RMAs in 8000
PHCs
300
12
28800000
1A
Placement of new RMAs 8000
in PHCs( from Aug 09 to
March 10)
700
8
44800000
2
TA for RMAs
500
300
12
1800000
2A
TA for RMAs
500
400
8
1600000
2
Training of RMAs (detail 25125
given below)**
0
40
1
10050000
Total
87050000
**Detail of expenses for induction trainings
Seria
l
Budget Detail
Items
NRHM PIP 2009-10: Chhattisgarh
Unit
Unit cost
Duration
Total cost
Page 212
Trainees
25
TA on actual
25
500
5
62500
Accommodation with food
25
250
5
31250
Out of pocket expenses
25
100
5
12500
pen, 25
300
5
37500
5000
5
25000
10000
5
50000
Training kit ( Bag,
photocopy, material)
Pad,
Venue & Logistics
1
Contingency (photocopy, Banner, PA, 1
System, Photographs)
Resource Person
Honorarium
10
500
5
25000
Food
10
150
5
7500
Grand Total
251250
Reservation for candidates from tribal areas for Nursing and ANM courses:
As mentioned earlier, major challenge for the state is of finding human power willing to serve in
tribal and remote areas. In order to address that, the state plans to reserve seats for candidates
from tribal areas for Nursing and ANM courses. These candidates will have to be nominated by
the Panchayat and they will have to go back to the area for service after finishing the training.
Closing Residential Gaps:
The state is committed towards strengthening Health Sub centres through additional ANMS
based on Panchayats. With two ANMs staying at the sub-centre, there will be an improvement in
sub-centre functioning and provision of services, especially institutional deliveries. In order for
this to happen, additional rooms for residence for the new ANM need to be built. We are
planning to close such residential gaps in 250 such Health Sub centres, which are currently
undertaking institutional deliveries.
The residential unit, which will be an addition to the existing sub-centre building, will include a
room, kitchen and toilet and will be approximately 400 sq feet. The design for construction of
such residential quarter will be as per GOI standard of pre-approved standard by Chhattisgarh
Government. The budget required is Rs 200000 per unit.
NRHM PIP 2009-10: Chhattisgarh
Page 213
Table 3.10: Budget summary for closing residential gap
Sl No.
Item
Measure
Unit
1
Closing
Identified
residential gap HSC
of Unit cost
250 200000
No of units
250
Duration
1
Total
50000000
In addition, we propose to develop the residential accommodation for the doctors selected under
Chhattisgarh Rural Medical Corps. As the doctors would be placed in very remote and difficult
strategy, where the PHCs are distributed widely with sparse population such as Podiprota block
of Korba district, Kusmi, Odgi, Balarampur, Wadrafnangar blocks of Surguja etc., it is
proposed that residential facilities be developed at the block levels instead of having them at
PHC level. The residential accommodation will be built for all the doctors from a particular
block at the block head quarter, while the RMAs, ANMs etc. will stay at the PHC level. It is
proposed that the developmental work may be limited to 10 blocks at the pilot phase. The
infrastructure may be multi-storeyed with expected cost of Rs. 64 lakhs per unit. Based on the
outcomes of retention of doctors the scheme may be scaled up or abandoned.
Table 3.11: Budget Summary for creating residential facility in Naxal affected area
Sl. No.
Number of Blocks / Complex
Unit Cost
Total Cost
1
10 Housing Unit in Naxal effected 50 Lakhs
area, remote and tribal area.
50000000
Distribution of Insecticide treated bed nets for families in high-risk tribal areas:
Malaria is the biggest public health problem in Chhattisgarh. In 2006, Chhattisgarh contributed
7% of the total malaria cases and 11% P. falciparum cases reported in the country (NVBDCP,
2007). As per the available data on malaria upto the November 2008, the central part of the
state, represented by 8 districts (61.09% of the state’s population) report low to moderate
incidence of malaria (8.16it%) and P. falciparum (4.58%), rest of the malaria burden is
collectively contributed by the 5 districts in the north and 3 districts in the south. These are
mainly the tribal districts with API more than 3. As per WHO norms, all families residing in
areas with API above 3 need to be covered with Insecticide treated bed nets (ITN).
NRHM PIP 2009-10: Chhattisgarh
Page 214
This has to be planned in a phased manner. This year we plan to cover 8 such blocks which have
a high ‘primitive tribal group’ (PTG) population like Baigas, Pahari Korwas, Birhor,
Abujhmaria, and Kawar. If we calculate the approximate number of families in a block to be
10,000, with two ITNs required per family, the total comes to 16,000 bed nets. At the rate of Rs
300 per bed net, the total budget comes to Rs 48000000.
Table 3.12: Budget for distribution of insecticide treated bed nets
Sl
No.
Item
Measure
Unit
1
Insecticide treated bed 2 ITNs
nets
family
of Unit
cost
per 100
No of units
240000
Duration Total
1
Total
48000000
48000000
Support in creation of Rural Medical Corps in difficult (conflict) areas in Chhattisgarh
To overcome the reluctance of doctors and nurses to serve in remote rural and tribal areas, the
Government of Chhattisgarh proposes to establish “Chhattisgarh Rural Medical Corps.” The
recruitment to CRMC will be through two routes, namely,
1. Voluntary choice by the doctors who opt for this position in the beginning of their
medical education
2. Doctors from other states who are willing to join CRMC
Besides the above-mentioned sources of cadres, the students appearing in the Chhattisgarh PMT
can exercise the option if they want to join the CRMC on completion of their course. The
Government of Chhattisgarh will meet the full cost of study of those students who do join CRMC
on completion of their course and will groom them accordingly. On the other hand, who do not
volunteer for joining CMRC at the end of the course will have to bear the full cost of their
education and a penalty.
The members of CRMC may be placed in
1. Most remote and difficult area
2. Comparatively less remote but difficult area
3. Least remote but difficult area
An area will qualify for being termed as most, more or least difficult area based on its
NRHM PIP 2009-10: Chhattisgarh
Page 215
4. Population
1. Distance from the district head
quarter and capital city
5. Security threats
2. Amount of forest coverage
6. Education facilities
3. Approachability
The perks and payments
The benefits and payments of members of this corps will vary according to the nature of their
working areas, which is as given below in the table:
Table 3.13: Perks and payments for Rural Medical Corps
Most remote
difficult area
ZONE III
Hardship
allowance
area 12,500
Transport facility
Yes
and Comparatively
less Least remote and
remote and difficult area difficult area
ZONE II
ZONE I
7,500
5000
Yes
Yes
Education allowance 1000 per month per 1000 per month per child 1000 per month
for children
child maximum 2000 maximum 2000
per
child
maximum 2000
Housing facility in Yes
transit hostels
Yes
Yes
Insurance coverage
500
500
500
Earned leave of 30 Yes
days in a year
Yes
Yes
Casual leave of 10 Yes
days in a year
Yes
Yes
One LTC for tour in Yes
India
Yes
Yes
Risk allowance
5000 per month
2500 per month
15,000/-
10,000/-
Total
package
10,000 per month
monthly 25,000/-
NRHM PIP 2009-10: Chhattisgarh
Page 216
Quantification of the Allowances and Other Perks
With the involvement of the Mitanin trainers and block level and district level Resource persons,
a classification of PHCs were carried out and accordingly there are about 80 PHCs in the most
remote and difficult areas of Zone -. There are about 70 PHCs in Zone -2 and 115 PHCs in Zone
-1
At the rate of Rs 25,000/-per month for about 80 PHC doctors in Zone -3 for a year it will cost
around Rs.2.4 Crores. Similarly at the rate of Rs 15,000/-per month for about 70 PHC doctors
in Zone-2 for a year it will cost around Rs.1.26 Crores. By the same calculation at the rate of Rs
10,000/-per month for about 115 PHC doctors in Zone-1for a year it will cost around Rs.1.38
Crores.
Similarly, the two nurses or ANM per Primary Health Centre or two support staff per PHC also
need to be encouraged to serve in these remote PHCs. Zone-1 will be excluded for this
additional incentive to the nursing and support staff.
At the rate of Rs 6,000/-per month for about 160 PHC Nurse/ANM in Zone -3 and 140 PHC
Nurse/ANM in Zone -2 @ Rs. 4000 per month, for a year it will cost around Rs.1.82 crores.
Similarly at the rate of Rs 2,000/-per month for about 160 PHC Support staff in Zone -3 and 140
PHC Support Staff in Zone -2 for a year will cost around Rs.72,00,000.
As an initial attempt during 2009 – 10, only zone – 3 and zone – 2 areas will be considered for
financial package.
Thus, a total of 2.88 Crores per year is needed to encourage the enthusiastic nursing staff and
support staff to venture to go and serve in these remote and difficult areas along with the
doctors.
The total cost on this incentive scheme 7.35 Crores.
Recruitment policy
CGRMC cycle will be for a period of ten years.
Initially, they will be posted to the most remote and difficult area. After serving in these areas for
4 years they will move to the less remote and difficult area where they should serve for another 3
years. Finally they would be posted in the least remote and difficult area for the remainder of
their deputation period cycle of ten years. After ten years, the candidate can re-enter the
CGRMC for another cycle. The direction of posting that has to be followed will be a route from
most difficult to the least difficult area and will not be whimsical. This is described pictorially in
the following diagram:
NRHM PIP 2009-10: Chhattisgarh
Page 217
Career scopes
As the posts available in peripheral to central zones diminish, the CMRC recruits will have to
make certain career options. After ten years of service this cadres will have two options to
choose from
1. To continue in the regular government system as before or
2. To opt out of the CRMC system with a golden handshake
After 5 years of service in CGRMC, a candidate if desires to go for post graduation will be given
priority for PG selection under the special quota for in service candidates for PG. Once they
finish PG, they are eligible for posting at CHCs.
Golden Handshake Offer:
A policy decision on this is to be made. The offer could be a month’s salary for every year’s
service or a consolidated one-year salary and emoluments for ten year of service.
The new recruits to CMRC will replace the vacancies, which resulted from golden handshake.
Fund for Chhattisgarh Rural Medical Corps
NRHM PIP 2009-10: Chhattisgarh
Page 218
The total cost on this incentive scheme to be charged for the year 2009-10 is Rs.7.77 Crores.
Strengthening the Mitanin Programme under ASHA:
Current Situation
At the completion of current year, the Mitanin programme is almost completing its 6 years in the
state. Resulting clear impact on breast feeding practices, institutional delivery, decreasing IMR
etc. 12th round of the Mitanin training will be completed by end of current year. In current year
training was mainly accomplished on
IMNCI based, 10th round of training which also incorporates some critical components of
home based newborn care.
AYUSH based 9th round of training in 56 blocks.
11th round of training on Village health Planning (VHSC) and strengthening in 143
blocks.
IYCF and counselling based 12th round training in 100 blocks.
Pregnancy testing kit (Nischaya) training in 146 blocks.
The current year Mitanin training status (till Dec 08) is as per follows
Table 3.14: Training status of Mitanins
Rounds of Training
Mitanin Training Status
8th round of training on Nutrition and Social Security
57315
AYUSH based 9th round of training
53456 ( ongoing)
IMNCI based 10th round of training-first round 5 day
57489
IMNCI based 10th round of training-Second round 3 day
32081( ongoing)
11th round of training on Village health Planning(VHP)
3538 Mitanin
Training of STT (35)
Training of DRP (437)
Training of MT (2920)
IYCF and counselling based 12th round training
Training of STT (35)
Training of DRP (395)
Training of MT (2920)
NRHM PIP 2009-10: Chhattisgarh
Page 219
Pregnancy testing kit (Nischaya) training
52298
Along with above training the other key activities done under Mitanin Programme are
Formation of VHSC through Mitanin cascade, the Mitanin has been made convenor of
the VHSCs.
MUKHYAMANTRI DAWA PETI YOJANA
On an average , Mitanins participated in
more than 16000 Village Health and
Nutrition Day against 20000 VHND
every month
Orientation of Mitanins on NLEP in selected
districts.
Identification of problems at hamlet level
under NREGA, MDM, JSY program and
it is being addressed at different levels
for solution.
The
To equip Mitanins at the hamlet level to so that she
can provide first contact curative care on time,
provision of Mukhaya Mantri Dawa Peti has been
made. Refilling of drugs in Dawa Peti takes place
once in every two months.
Previously the
procurement and logistics was done by the District
Health Society ( DHS) . In current year, the
procurement and logistics has been done at the state
level and distributed (through CMHOs and BMOs).
Irregular purchase and supply of drugs emerged as a
problem in the state. The districts, based on Mitanin
feedback, have mainly expressed their concern on the
irregular supply of chloroquine, IFA and metro.
Regular supply of drugs needs to be done to provide
first contact curative care on time.
BCC kit for Mitanins has been
formulated and designed. Under which
one book on local food, one flipbook on
key messages, a set of flash cards, a decision chart and a set of three films is
prepared.
A database of 60000 Mitanins and 3400 trainers compiling their social background is
under preparation and it will be completed by March 09.
The process of listing of hamlets without Mitanins has been started; it will be completed
by Feb 09.
Identification of the Mitanins belonging to primitive tribes is completed. In total 693
Mitanins belongs to five primitive tribes. These tribes are Abhujhmaria, Baiga,
Kamar, Birhor and Pahadi Korba.
136 Mitanin Help Desk at CHCs level and 13 MHD at the district hospitals are made
functional this year.
25 Mitanins are working as Convenor for Ayurveda grams
NRHM PIP 2009-10: Chhattisgarh
Page 220
The incentives to Mitanins under different heading – The current status
Table 3.15: Incentives provided to Mitanins under various schemes
S.
No
Incentive purpose
Current Status
1
JSY
All Mitanins are regularly receiving the incentives as
per the guideline. The problem faced under this is
mainly due to unavailability of the fund.
2
Immunisation session
All Mitanins are regularly receiving the incentives every
month as per the guideline. Problem faced in few
districts was due to ambiguity in the guideline.
3
Family Planning
All Mitanins are receiving the incentives as per the
number of motivated cases referred by them. The
problem faced was due to the revised guideline of GOI
in which the incentive eligibility spreads over the wide
range of motivators in place of ASHA. This is required
to be worked out for CG.
4
RNTCP
Hardly 1% (i.e. 600 to 700) Mitanins are DOTS
provider. The availability of fund is also emerged as a
problem. Special attention is required for this.
5
NLEP
Just introduced in the state. An orientation plan is
ongoing.
6
VBDCP(Malaria)
Just introduced in the state. At present it is only for 11
districts, for rest of the 5 district planning is required.
Activities not achieved in current year (2008-09)
Social security incentive to the Mitanins by providing general health insurance
Creation of data base of the number of hamlets without Mitanin
Restart of radio program on Mitanin
The programme will largely involve these strategies:
Continuous training and support to the Mitanins along with the social mobilization,
selection and training and capacity building of 6,000 new women health volunteers to
cover all the hamlets.
NRHM PIP 2009-10: Chhattisgarh
Page 221
Reduction of malnutrition with the application and practices of learnt skills by
strengthening and deepening the health education and counselling work at the
household level and by means of equipping the Mitanins with BCC kit.
Inter-sectoral integration among the related sectors at the habitation and Panchayats
levels and strengthening local planning at Panchayats and village level by making
20,000 village health plans.
Social mobilization, training and capacity building for strengthening of VHSC and to
enhance community participation in local self-governance system.
Strengthening the access of the poor to essential curative care through adequately
provisioned women health volunteers. They are also linked to improved peripheral
primary and secondary medical care facilities, through a functional referral system,
Mitanin help desk (MHD). They enable the public health system to respond promptly
and adequately to needs of institutional care of sick children, referred in by Mitanins
Troubleshooting the problems in incentivisation of the women health volunteers work
especially for JSY, Immunisation session, family planning so that there would be
enough encouragement and recognition of their work both at the family and community
level.
To develop the logistical system for timely drug distribution under Mukhya Mantri
Dawa Peti yojana.
To ensure to continue Mitanin Pati (quarterly newsletter) and its extension for 60,000
Mitanins for cross learning, knowledge management and to motivate them. It will be
helpful in strengthening their self-esteem and an opportunity to bring them together to
build their capacity on problem solving
To recognise the Social and system level problems faced by the Mitanins. This is to
motivate them and to advance the solidarity among the Mitanins. State, district and
block level “Mitanin sammelans” of the women health volunteers to increase their
motivation, maintain their spirit of volunteerism and to strengthen their identity by
bringing them together on a single platform through games, cultural shows and health
related activities etc. Better outcome monitoring and closing all gaps to achieve an
effective health outcome.
Plan for the Mitanin Programme:
Ongoing operational activities with objectives
Sustaining trained Mitanin supported by women health group in every hamlet. In addition to the
existing force of 60,000 Mitanins, 6000 new Mitanins are to be trained to cover all the hamlets.
NRHM PIP 2009-10: Chhattisgarh
Page 222
It will be helpful to maintain and stimulate the ongoing facilitation of service delivery by
Mitanins and community base of all health programmes is sustained through this. In a year, 12
days camp based and 24 days field would be organised for the women health volunteer. The key
training will be on
1.
BCC kit, it will cover all the key messages she has learnt till 12th round of training.
2.
National programmes- RNTCP, NLEP, NVDCP, JSY ,Family planning, Blindness
Control Program etc
3.
Revision of Dawa Peti and AYUSH.
4.
HIV /AIDS, Emergency Contraceptive pills and home visits
5.
Implementation and follow up of Village Health Plan and referral cases.
6.
HBNCC in 6 selected blocks.
Ensure that every sick child suffering from fever, diarrhoea, and ARI are visited on the very
first day of illness with appropriate first contact care through use of Dawa Peti and referral
where necessary. The key factor for this to happen is to ensure effective access to basic
drugs in every hamlet through the Mitanin drug kit. Timely redressal of the referral cases
initiated by the Mitanin under the referrals chain system and support of ANMs /PHCs/CHCs
and district hospitals to receive timely referrals when needed.
Ensure that along with utilisation of Dawa Peti, use of local herbals treatment for illnesses
will be promoted by promoting Herbal Gardens at local level. Ensure required support to
AYUSH in development of Ayurgrams in the state.
Ensure that every newborn is visited on the first day after birth i.e., visit to the newborn on
3rd, 7th, 14th, 21st and 28th day by the Mitanin in the neonatal period as per the Integrated
Management of Neonatal Childhood Illness (IMNCI) training. To ensure that appropriate
classification, treatment and referral are done by the women health volunteer. A mechanism
to monitor and provide feedback for 0-2 months neonates will be operational as per GOI
guideline
Ensure that all pregnant women are counselled on general measures, access to antenatal
care, and referred to an institutional delivery facility for childbirth.
Ensure strengthening of existing Mitanin Help Desk (MHD) by using kiosk for the delivery
of key messages on health at the district level and its expansion to those PHCs which have
huge OPD load for the strengthening of referral support system. Training of BMO’s and
DRP’s on Mitanin Help Desk for the strengthening of referral support system. Effective
NRHM PIP 2009-10: Chhattisgarh
Page 223
functioning of the Mitanin help desk (MHD) in all the districts hospitals and CHCs along
with its initiation in the identified PHCs. This will help in ensuring the increase numbers of
referrals as well as referrals addressed. It will also give an impetus in increasing the
numbers of institutional delivery coupled with the insurance of service provision.
Ensure the participation of all Mitanins in Village Health and Nutrition day every month
with greater involvement of VHSCs members.
Ensure to deal with the problems of child malnutrition by using IYCF practices. Training
and capacity building on behaviour change kit for the Mitanins to combat malnutrition
Ensure training and capacity building on behaviour change kit for the Mitanin to combat
malnutrition by using IYCF practices and increased number of home visits
Ensure that Women Health Committees formed in the hamlets are regularly meeting and key
health messages are discussed there. It also acts as a nodal point for health education and
behaviour changes in certain areas. Active women health committee will support and result
in forming active VHSCs which in further will be helpful in activating quality village health
plan (VHP).
Ensure regular quarterly facilitation of Mitanin Pati across the state
The new operational activities with objective
The HBNCC (birth, asphyxia and sepsis management with home based newborn care)
interventions in 6 selected (Bilaigarh, Chhura, Kanker, Bhanupratapur, Darbha,
Bastar) blocks of the state in coordination with SEARCH, Gadchiroli.
Providing an operational kit ‘Mitanin ASHA strengthening package’ to all 60000
Mitanins. The operational kit is comprised of an umbrella, torch, Dawa Peti, raincoat,
uniform etc. So that with the help of the kit she can easily deliver her task like home
visit in rainy season, home visit during night hours and timely referrals
Ensure to provide BCC kit to all Mitanins. Reduction of malnutrition and to address it
at the hamlet level with the help of counselling skills by using BCC kit. Women health
volunteers should know all malnourished children within under 5 or under 3 age
groups in their respective hamlets. Feeding related counselling with the skills and
practices of IYCF and BCC kit is given to families of grade-1 and grade-2 children in
regular intervals to improve the situation. Severe and acute malnutrition (grade 3 &4)
is referred to health care facilities.
Ensure the provision of recognition of Mitanin in the existing health system by
advocating for free health services to the Mitanin and her family in district
NRHM PIP 2009-10: Chhattisgarh
Page 224
hospitals/CHCs. Also, provide them the platform to enhance their self-esteem and to
express their vision and mission of life. In addition to this, with regards to their career
advancement and progress, 10th and12th pass Mitanins, MTs and DRPs can also opt for
other vocational courses. Providing social security to the Mitanins through general life
risk coverage insurance.
Ensure state, district and block level “Mitanin Sammelans” of the women health
volunteers to increase their motivation, maintain their spirit of volunteerism and to
strengthen their identity. For improving coordination and referral cases management
PHC level Sammelans of AWW, ANM and Mitanins will be organised once in a year in
all PHCs.
Social mobilisation of more than 700 Mitanins belonging to the primitive tribes in the
state. Special efforts need to be given to their capacity building through one-day
orientation program in every month. It would strengthen their understanding on social
issues as well as taking actions for social change. Convergence with the local bodies
like Baiga Vikash Pradhikaran (BVP), Kamar Vikash Pradhikaran (KVP) etc will be
done to improve upon the coordination part.
Ensure smooth procurement, logistics and distribution system of Mitanin Dawa Peti
from CHC’s store to Mitanins through formed VHSCs with active involvement of the
MTs/DRPs and AWCs. It may be initiated on pilot in 50 blocks in first phase.
Ensure recommencement of the radio programmes on Mitanins i.e., Kahat Hain
Mitanin on different issues /topics like for social mobilisation and awareness
generation of the community and Mitanins. Dissemination of information and
awareness building through radio will also be done on Infant Young Child Feeding
(IYCF), Integrated Management of Neonatal and Childhood illness (IMNCI), Home
Based Neonatal Care (HBNC), Ayush ,Swasthya Panchayat Yojana (SPY), Village
Health Plans (VHP), RNTCP, VBDCP( Malaria) ,NLEP, Family planning ,Emergency
contraceptive pills, JSY,TSC , HIV/AIDS, social security, nutrition, govt schemes and
VHSC. Total 13 episodes will be prepared and broadcasted from 5 relay (Raigarh,
Jagadalpur, Ambikapur, Raipur, Bilaspur) centres. Evaluation mechanism to analyse
the impact of Radio program will also be facilitated. Designing the concept of
community radio programme.
Ensure that Mitanins as a convener of VHSC will lead the process of village health
plan at hamlet level with the support of MTs. No of Mitanins leading the active VHSC
and developing VHP in guidance of Mitanin Trainers. Number of functional VHSCs
with the proper utilization of untied fund for the improvement in health, hygiene and
sanitation status of the villages. The village health plans shall include the issues like
NRHM PIP 2009-10: Chhattisgarh
Page 225
food security, safe drinking water and sanitation, early childhood care services and
school health services and access to health care services and health education at the
village and Panchayat level. Ensure development of at least 5000 Village Health Plans
(VHPs) out of 20,000 village health plans by Mitanins as a convenor of VHSCs. It will
also lead to the development of 9820 Panchayats plan in the state.
Mitanin will work as a convenor in the working committee of 25 Ayurgram village in
coordination with AYUSH and SHRC
Indicators:
1. Number of training attended by the Mitanin in days and No of days training done
for Mitanins.
2. Number of Mitanins using operational Mitanin/ ASHA kit.
3. Day 1 visits by the Mitanin during delivery and neonatal period to any home.
4. Micro planning for delivery based on EDD is done with the assistance of women
health volunteers at family level to promote institutional delivery in all possible
cases or at least in those cases with risk factors
5. Mitanins are approached by a certain minimum number of families for common
ailments, first level care is given, and prompt referrals are initiated based on
symptoms in all necessary cases.
6. Mitanins attending Immunisation sessions at AWCs regularly as a token of she is
helping mobilising the community for health services. (The important background
factor here is the prompt disbursement of immunisation camp incentives to
Mitanins.)
7. No of Mitanins using BCC kit during counselling of the families in hamlets.
8. Women Committees formed in the hamlets are regularly meeting and key health
messages are discussed there.
9. No of Mitanins leading the active VHSC and developing VHP in guidance of
Mitanin Trainers.
10. Effective functioning of the Mitanin help desk (MHD) in all the districts hospitals
and CHCs along with its initiation in the identified PHCs.
NRHM PIP 2009-10: Chhattisgarh
Page 226
11. Increased community participation in village health plan at the village and
Panchayat level. Better utilization of the services at the health centres as an
impact of radio programs.
12. Number of qualified (10th and 12th pass) women health volunteers, Mitanin
trainers and DRPs enrolled in vocational courses/ANM training to enhance their
knowledge.
13. Spirit/mobility/self-esteem increased due to “Mitanin sammelans” at the block,
district and state level which will ultimately increase the quality of Mitanins
output and thus will improve the overall impact of the program. Number of
women health volunteers getting incentive for social security.
14. No of Radio programs broadcasted across year from 5 relay centres
The impact of output/outcome indicators discussed above should be visible by a measured
decline in child malnutrition rates, decreased low birth weight rates, decreased anaemia in
women and decreased micro-epidemics and decreased epidemic deaths in gastroenteritis,
childhood acute respiratory infections and malaria, community participation in village health
plan as well as in panchayat plan. By all the above measures linked to improvements in the
facility to reduce the infant mortality rate by the year 2009 -10 to below 35 {current the IMR of
the state is 59 %( Total 59%, Rural 61%)} (Source of data SRS-2006). Current malnutrition
status of 52% shows that more than half of the children are the victims of one or the other form
of deficiencies. So bringing down the malnutrition of the state to below 40% by the year 20092010 will also be the significant area of interventions (Source of data NFHS III-2006).
Institutional Mechanism:
The programme will continue to be led by the directorate of health services/state health society,
coordinated on its behalf by the State Health Resource Centre and will be implemented at the
district level by the District RCH (Health) societies.
SHRC will do TOTs of STT, DRPs, MTs and develop all training material for Mitanin
programme, facilitates the Mitanin training at block level. SHRC will also monitor the entire
Mitanin program and provide timely feedback
Budget Estimate:
Out of the projected below for Mitanin Training & support activities, the state would be getting
at least from ASHA budget under NRHM and for the rest some other sources would be explored.
Table 3.16: Budget estimate for Mitanin (ASHA) Programme
NRHM PIP 2009-10: Chhattisgarh
Page 227
Sl
Unit
Unit
cost
No.
Duration Exp. per
of
year
Units
A.( I)Training and regular support for the strengthening of 60,000 Mitanins
1
Per day cost for Training of Mitanins
85
60000 10
51000000
2
Per day livelihood Compensation for Mitanins
on training days
Audio-visual and other arrangements for 2400
such training camps in the state
Per day Training of Mitanin support teamTrainers (BRPs-1 per 20 Mitanins) Including
RP cost
Training of Block Coordinators (DRPs)
including RP costs.
Per day Compensation for Mitanin support
team- Trainers (BRPs)
Per day Compensation for Mitanin support
team- Trainers (DRPs)
Training Material (lump sum amount together
for all material per mitanin per year)
Total(I)
80
60000 10
48000000
250
1600
2
800000
400
3000
12
14400000
650
460
12
3588000
85
3000
240
61200000
135
292
300
11826000
200
66000 1
3
4
5
6
7
8
A (II) Training of 6,000 new Mitanin
1
Total cost for social mobilisation, training etc. 2000 6000 1
Total (II)
A
Total (I+II)
B. Social security and Mitanin ASHA strengthening package for Mitanins
1.
Yearly premium.
100 66000 1
2
A Mitanin ASHA kit
700 66000 1
B
Total
Mitanin Dawa Peti
Sl
1
2
Unit
Unit No. of Duration
cost Units
Mitanin dawa Peti – Procurement ,logistics 6000 146
and distribution
For Mitanin Drugs (one refill every two
month of Rs 75 for each Mitanin- in addition
to the allocation available with state budgetto fill gaps of chloroquine etc)
NRHM PIP 2009-10: Chhattisgarh
13200000
204014000
12000000
12000000
216014000
6600000
46200000
52800000
Exp. per
year
8,76000
27000000
Page 228
C
Total
D. Social mobilization
1
Block Level Interventions* ( including PHCs),
MHD, PHD Sammellans , Extinct tribe of
Mitanins etc
2
District level Interventions* MHD, district
Sammellans etc
3
State Level Interventions **( Radio Programs ,
State Sammellans, Extinct tribes Sammellans )
D
Total
E Programme Management and Coordination
1
Block Level Programme Coordination and
Monitoring ***
2
District Level Programme Coordination and
Monitoring *** cost per block
3
State level Programme Coordination and
Monitoring
E
Total
Grand Total I
F BCC Kit to Mitanin /MTs and DRPs
27876000
3000 146
12
5256000
5000 18
12
10,80000
5000 146
1
730000
7066000
7000 146
12
12264000
2000 146
12
3504000
6000 146
12
10512000
26280000
330036000
1
BCC Kit to Mitanins/MTs and DRPs ( Budget 1000 60000
60000000
for BCC kit will be from European Union State
assistance )
F
Total
60000000
Grant Total II( Grand I + F)
390036000
Allocation From ASHA budget under NRHM( Allocation for ASHA Dawa Peti Kit 330036000
of 2.7 Crore is included in this)
Assistance from European Union State Budget
60000000
Note: Out of the total outlay of the mitanin program, Rs. 17.70 Crore will be given through
GoI (Including the Dawa Peti), rest of money will manage form the other sources.
Mobile Medical Unit:-
In the state of Chhattisgarh where the population density is quite 154 per sq km. and the
habitation is quite disperse dispensing heath services is a challenge. In order to provide basic
health facility to these under served and unserved area the state need to take help of mobile
health clinics. In the year 06-07 GoI has given funds to procure such vehicle which will house
one examination area , one lad testing area, one drugs dispensing area and one staff vehicle.
NRHM PIP 2009-10: Chhattisgarh
Page 229
State is in process of procuring such vehicle. These vehicles will have two doctors (contractual)
staff nurse, lab technician and one pharmacist as medical unit and in non-medical unit one
supervisor and two drivers. This unit will be made operational by mostly by contractual staff and
Local NGOs who will help to organize family planning camps for male, minor operation,
malaria checkups, follow-ups, etc.
The budget proposed for this project amounting to Rs. 24000000/- has already been sanctioned
in the previous year 2007-08 PIP and so for the current year the same amount will be utilized for
the current year as proposed.
Current status: in state of Chhattisgarh total 52 mobile medical units are working. Out of which
32 units are with Bastar Pradhikaran and 20 units are working with Sarguja Pradhikaran.
Which are located in Districts as follows
Table 3.17: Status of Medical Mobile Units
Sl.
No.
Name
district
of
the RTV
unit
1
Kanker
3
2
Jagadalpur
3
Mobile Marshall
Ambulance
TATA
Sumo
Total No.
MMU
2
1
06
3
4
6
13
Dantewada
4
4
3
11
4
Sarguja
4
-
6
10
5
Korba
2
-
2
04
6
Jashpur
3
-
2
05
7
Kawardha
-
-
2
02
8
Raigarh
-
-
1
01
Total
19
10
23
52
of
The fund for this project is available in the last year PIP which will be utilize in current year,
apart from this fund, this year additional operational cost will be required. For which the
proposed budget will be for the salaries of the drivers (146 for BMO vehicle and 74 for
pradikaran i.e.220) and POL. The salaries will be as per collectorate rate. + 16 trauma unit
vehicle and 20, Other than 76 drivers the salary for others drivers will be incurred through state
budget
NRHM PIP 2009-10: Chhattisgarh
Page 230
Table 3.18: Budget summary for drivers and POL
Sl.
No.
Budget head
1.
Unit cost
No.
Of
units
Amount in Rs.
Salary for driver (40 Pradhikaran + 16 6000X12
MMU +20 Trauma Drivers)
76
5472000
POL ( 74 Pradhikaran + 146 BMOs + 100000
16 MMU + 20 Trauma Vehicles )
256
25600000
Total
31072000
Bal Hruday Raksha Yojana: Chief Ministers’ Child Heart Protection Scheme
The Objective of the scheme is to provide health care to the children of poor and needy Families
under the age of 1 to 15 years who are suffering from heart diseases and require surgical
treatment in Chhattisgarh state. Such heart surgeries will be carried out free of cost in selected
hospital of Chhattisgarh under the Chhattisgarh Health Communities. National Rural Health
Mission. With the expense of Heart Surgery, additional Expenses of the Family members will be
borne by the state.
With the achievement of the given objective the representative of state Health Committees. The
Director of Health &Family Welfare will be liable to play the decided amount for the services
rendered by the Hospital in the form or either cash or cheque or bank draft upon production of
certificate for each surgery.
Table 3.19: Financial status of Baal Hruday Suraksha Yojana
S.No
Opening Balance
Expenses (Jul – Balance
Dec 08)
Amount
Required
for
programme expenses 09-10
1
30000000
10002120
30000000
19997880
Table 3.20: Budget Summary for Baal Hruday Suraksha Yojana
S.NO. Item
No. of
Unit
Per Unit
Cost
Duration Total cost
1
1
35000
12
State Coordinator
NRHM PIP 2009-10: Chhattisgarh
420000
Page 231
2
Computer operator
1
8000
12
96000
3
Office Assistant
2
6000
12
144000
4
Programme Expenses(surgery
cost)
200
150000
1
30000000
5
Contingency
50000
Grand Total
3,07,10,000
Strengthening the Village Health & Sanitation Committee
The Village Health & Sanitation Committee envisaged under NRHM is within the overall
umbrella of PRI. The NRHM acknowledges “Decentralization and Peoples’ Participation” is
essential for Health Sector Reforms and spells out many details of institutional arrangements for
Local Health Planning at the Village level. It has been decided to formulate “Village Health
Plan” at village level to improve upon and make positive changes in the health status of the
villages. The initiatives at panchayat and hamlet level have been initiated much before through
Swasthya Panchayat Yojana and hamlet level meetings. Consolidation of hamlet level problems
is in process through the formation of village health plans and establishing its linkage with
Swasthya Panchayat Yojana at the panchayat level. The implementation and monitoring work of
it across the state is provided to SHRC.
Current Status:
In current year, following activities are completed:1.
2.
In the state, the first activity carried out under this was the formulation of VHSC
guideline in lieu of GOI guidelines. The following process were adopted for this
•
Consultation at various levels
•
Studied existing structures in other states.
•
A process for convergence of different committee of various departments at
village level to ensure the focused and effective implementation of the schemes
and programmers.
•
Incorporated suggestions of GOI guideline and suggestions given by National
Health System Resource Centre (NHSRC).
Following features in VHSC formation in the state are ensured :-
NRHM PIP 2009-10: Chhattisgarh
Page 232
•
Standing committee of Gram Panchayat leads VHSC. The president of VHSC is
also a member of standing committee of PRI. All the ward panchs are member of
VHSC.
•
Adequate representation of the weaker sections (Scheduled Castes, Scheduled
Tribes, and Other Backward Classes) has been taken into consideration.
•
Mitanin (ASHA) is a convener of VHSC on yearly rotation basis. The approach to
have Mitanin as the convenor is a step forward to fulfil the commitment towards
women empowerment.
•
In addition to this, representation from non-governmental sector and Women’s
Self-help groups has also been ensured. The presidents of the village level all
CBOs are the members of VHSCs. The composition of VHSC also includes at least
50% of women participation.
•
Special invitee members in VHSCs are - AWWs, Teachers, ANMs, hand pump
mechanics.
•
Joint account in the name of panchayat secretary and convener Mitanin.
3.
The Untied Fund for the VHSCs of 20,308 villages has been released.
4.
The elaborative & detailed guideline for proper formation of VHSCs has been
framed & circulated to all VHSCs and relevant departments at the block/district level
functionaries of key departments.
5.
For the formation and functioning of VHSCs, social mobilisation campaign “Gram
Swasthya Niyojan Abhiyan” was organised at massive level from 15th June to 15th
Aug across the state.
The important activities and their results under this are as follows:• Organized special gram Sabhas in every revenue village across the state.
• Displays of shows in revenue villages by Prerana Dal (Human Media).
• District and Block level coordination meeting across state.
• Radio Jingle of 30 sec was broadcasted at 07.21 PM from 11th July, 2008 for 30 days.
The achievements of the Mass Social Mobilisation Campaign “Gram Swasthya Niyojan
Abhiyan” are as follows:-
NRHM PIP 2009-10: Chhattisgarh
Page 233
Table 3.21: Achievements of Gram Swasthya Niyojan Abhiyan
S.No Activity
Target
Achievement
1
Number of VHSC formed
20344
18432 ( 90.60 % )
2
Number of VHSC A/c. opened
20344
16892 ( 83.03% )
3
20344
20344
14504(71.29%)
4
Number of Mitanin Trainer (MTs) trained on 2920
VHSC
2920 (100%)
5
Number of DRPs trained on VHSC
427 ( 100% )
6
VHSC guideline shared with the BMOs, 30000
CDPO, CEO etc
30000 (100%)
7
Gram Sabha campaign in Revenue Village
20344
14534 ( 71.44% )
8
Prerana dal activity
9820
Panchayat
5426 Panchayat
(55.25% )
6.
427
After the campaign, plan is to train 10,0000 VHSC members. They are mainly
sarpanch, Sachivs, upsarpanch, and president of VHSC, Anganwadi worker,
Mitanin, ANM and members from VHSC. Training of 1 Lac VHSC members will be
completed by Feb, 2009. The status of the ongoing training of VHSC members is as
follows.
Table 3.22: Status of ongoing VHSC training
S.No
Activity
Target
Achievement
1
VHSCs member training
100000 members
2348 till Dec 08
7.
In parallel to training and use of untied fund, the process for the development of
VHPs has already been started in more than 250 villages. The present status of the
Village Health Plans received from the villages are as follows
Table 3.23: Status of Village Health Plan progress
S.No
Total No of districts
Total No of Blocks
Total number of VHPs initiated
1
12
41
228
NRHM PIP 2009-10: Chhattisgarh
Page 234
8.
Till now we have initiated village health planning in 228 villages and received 41
Village Health Plans (VHP) from 9 districts and 24 blocks at the State level ,
analysis of VHPs is as below :-
NRHM PIP 2009-10: Chhattisgarh
Page 235
Table 3.24: Detailed analysis of Village Health Plans
Interventions
Institutional
delivery
Immunization
No of VHPs
No of villages
performed
normal on the
issues
No
of
villages
where
issues
emerged
No.
of
villages
where VHP
process
is
initiated
0
29
29
7
11
18
Key issues emerged
Interventions addressed for problems
Resistance in family for institutional delivery ,distance between
sub centre and village , ANM doesn’t stay in village , unable to
manage transportation to go even if willingness is there , fear of
operation ,negative impression about govt services since long
time, trust on Dai , expensive ( In cases the government
functionaries demand for money) , doctors insist for caesarean
and doesn’t allow family member to enter in delivery room ),Low
level of awareness, no building available for sub centre in few
villages, discouraging response in the hospitals and delay in
payment of incentive to go there, ANM doesn’t stay at her
headquarter, low awareness about JSY , no availability of women
doctors PHC/CHC
Low level of awareness, Nurse doesn’t come regularly because of
distance, irregular supply of vaccine ,resistance in community for
immunization (Child gets fever after immunization) , No fixed time
for immunization, Don’t go because of fear, less community
participation in VHND, timely information regarding change in
schedule of immunization is not given
Ensuring VHSCs untied fund utilization in
hand pump ,soak pit and village draining
system
Strengthening of VHND
Focusing extinct tribal area through
Mitanins
Strengthening
Sishu
Sanraksaan
Maah
Streamlining the use of SHG untied
fund
Strengthening the Swagath Bheit for
pregnant women and neonate
Strengthening VHSC and its linkage to
TSC
Including topic of safe drinking water , use
of toilet, immunization in training
curriculum of VHSC members
ANC
5
9
14
Coordination between ANM and community ,Irregular stay of
ANM in village ,Weak because of non availability of equipments,
Non availability of machine, No weight machine, , Scattered
household in hamlet.
Including all these topic in Mitanin BCC
kit
Safe Drinking
Water
1
25
26
Waste disposal around hand pump and distance of the hand pump
from the households, Non functional ( leakage in pipe line ) , due
to heavy % of iron in water ( hand pump ) in some places ,
multiple use of existing water supply, ,unavailability of hand
pump in hamlet, Lack of proper drainage system, habitual of
using water from well/conventional sources, unavailability of
local fund to handle the problems of hand pumps in time
Strategically facilitating the social
marketing of family planning methods
NRHM PIP 2009-10: Chhattisgarh
Prioritizing all these issues in village
health plan and swasthya panchayat
yojana ( SPY)
Page 236
Use of Toilet
Family
Planning
0
1
19
5
19
6
Long practiced behaviour and Low level of awareness,
Construction of toilet is incomplete by the Panchayat( They
doesn’t have money to construct) , Few household have individual
toilet ( but most of the male member generally go outside), even if
willingness is there they don’t have sufficient water for it , cannot
afford to construct toilets on their own because of poverty, Funds
not provided for community toilet construction by the panchayats,
, no awareness regarding govt schemes, even families construct
the toilets as per the standard design , which they find non
conductive to use
Facilitating the JSY helpline and CHC’s
mobile unit (ambulance) along with simple
process of money distribution and
monitoring
Low Awareness level and hesitation , non availability of it on
facility
Ensuring convergence /coordination with
UNICEF, CARE, MI, AYUSH, SIRD, PRI,
WCD, Education, local CBOs etc for all
these interventions particularly for
institutional delivery, immunization, use of
toilet, VHSC strengthening etc
Accelerating the process of construction of
ANMs SHC building , so that ANM can
stay at her head quarter
Ensure the re- appropriation of health
staff to have facility for institutional
delivery in most of the CHCs/PHCs
NRHM PIP 2009-10: Chhattisgarh
Page 237
Operational objectives:
1) To develop common understanding & generate awareness among the community,
Community based Organizations (CBOs), members of Panchayati Raj Institution (PRIs)
and representatives of government departments like teachers, hand pump mechanics,
ANMs, AWW etc. This would help to disseminate the objectives and role of VHSCs,
enabling to perform the expected actions of VHSCs as member and special invitee;
effective utilisation of untied fund to address issues of equity and vulnerability.
2) To ensure the strengthening of the formed Village Health & Sanitation Committees
(VHSCs) in the revenue villages, it will streamline the functioning of VHSC and thus to
achieve its objectives. At least 50 VHSC will have their own building at the end of the
year
3) To ensure the development of at least 5000 village health plan out of 20,334 Village
Health Plans in the villages this year , which will ultimately lead to conceptualization
and framing of a Panchayat Plans
Strategies: -
1) Incorporation of NRHM Guidelines on regular basis.
2) Capacity building of VHSCs members and various stakeholders.
3) Conceptualization & formulation of Village Health Plans (VHPs) in accordance with the
Health & Human development indices accumulated under Swasthya Panchayat Yojana.
4) An effective feedback and monitoring mechanism will be established to make planning
process result oriented.
5) Social Mobilisation, inter sectoral convergence and coordination will be the key
strategies for effective functioning of VHSCs.
6) Integration of the VHSC with other programs like TSC etc
7) Institutionalisation of VHSC will be facilitated.
8) Use of Mitanin cascade for the implementation of all activities
Activities: -
The activities will be done through Mitanin Program cascade – MTs, DRPs and (FCs) Field
Coordinators in close support and coordination with BMOs, CHMOs, and CEOs etc.
NRHM PIP 2009-10: Chhattisgarh
Page 238
1) Regularizing monthly meeting of VHSCs and active participation of various stakeholders
through joint and separate directive at regular intervals. Also establishing the block level
Sachivs meeting, sarpanch sangh meetings or facilitating platforms.
2) Ensure the active participation of VHSC in Village Health and Nutrition day to address
coverage , malnutrition , immunisation ,anaprashan, ANC services etc through capacity
building , regular meetings and VHP
3) Ensuring the publication of the documented story of VHSCs in Mitanin Pati, Panchaman,
departmental magazines and in other key newsletters.
4) Two day training of five members from each VHSC will be done by MTs ( Mitanin
Trainers ) and DRPs ( District Resource Person ) on micro planning, equity
,vulnerability , VHP ,institutionalisation of VHSCs and the scope of the utilization of the
Untied fund Grant and the social audit aspect of it. With this the interventions like
immunisation , institutional delivery, National Program RNTCP, Malaria, NLEP and
also the updated directives from GOI etc will be given special focus
5) Structural monitoring and feedback measures will be taken for strengthening of Village
Health & Sanitation Committees (VHSC) to ensure 100% registration of births and
deaths in the villages and to address issues of Infant death & malnutrition, availability of
safe drinking water and other key roles of it
6) Microplanning will be a major tool during the conceptualization & framing of the Village
Health Plan (VHPs). To facilitate the process of micro planning linkages with PHRN,
community monitoring framework , local NGOs and active involvement of different
stakeholders will be addressed through gram sabha, cluster meetings, monthly meetings
and meetings of women health committee etc . Ensure at least 5000 VHP against 20,000
in a year documented plans will be used for advocacy and problem solving
7) Ensuring the role of Community Monitoring Framework (CMF) for effective functioning
of VHSC at the state and the district level. District wise Community Monitoring
Framework (CMF) for NGOs in 6 districts and 12 villages. Support will be ensured
based on their analysis and feedback.
8) In institutionalisation of VHSC, its linkage with Gram Panchayat will be strengthened
through activating the Standing Committee of it and in the block to state level actions.
Efforts to be given to have joint or separate buildings VHSCs at least in 50 villages with
the support of gram panchayats. For this, efforts should more be focused on
strengthening of community process and its linkage with other local bodies or different
departments.
NRHM PIP 2009-10: Chhattisgarh
Page 239
9) Mitanin program cascade will be used for monitoring and feedback mechanism for the
functioning of VHSCs and development of VHPs. In addition, CEOs meetings, Zila
/Janpad meetings and other forums will be used for the development and rapid
implementation of VHPs as well as for advocacy purpose.
10) To ensure active functioning of VHSCs in coordination with other departments like
Women & child development department( WCD), Public Health & Engineering
department( PHED), AYUSH, Education department, Bank, Health department,
SIRD,SIHFW,SRC and Panchayat etc. It will promote and strengthen the inter-sectoral
linkages among the sectors. Coordination with Public Health Resource Network (PHRN)
will also be taken into account.
11) VHSC will work as working committee in developing 25 Ayurveda grams with the
coordination of Ayush department while Mitanin will be convenor for it.
12) Ensure the participation of VHSC in four Gram Sabhas in a year to strengthen the
community process. Ensure special gram sabha on VHP in every village. Addressing the
dimensions of transparency and accountability through social analysis & audit in Gram
Sabha.
Main Indicators: -
1) No of VHSCs functional i.e., regular monthly meeting
2) No of VHSC members received training on different interventions
3) No of Gram Sabha conducting Social Audit of the utilisation VHSCs untied fund and no
of special gram sabhas organised in village on health plans
4) Village Health Plans (VHPs) formed in all the revenue villages by considering
village/hamlet specific issues.
5) Functional VHSC able to utilize the united fund grant properly that shall be visible by the
No. of Social Audits in Gram Sabha, proper submission of Utilization certificates (UCs).
6) The number of VHSC carved out ways to channelize in-flow of funds and resources from
various other developmental departments.
7) No of VHSCs participation in VHND every month
Institutional Mechanism:
SHRC will facilitate the strengthening of VHSC through process like trainings, coordination
among different stakeholders, development of training materials and documentation of VHPs etc.
SHRC is also to monitor the VHSCs and to provide timely feedback to directorate.
NRHM PIP 2009-10: Chhattisgarh
Page 240
Table 3.25: Budget Requirement for Untied Fund for VHSC
Sl.
No.
Key heading
Unit Of
Measure
Unit Cost
No. Of Units
Total Cost
1
Untied fund
No. Of VHSC
10000
20334
203340000
Total
20,33,40,000
Monitoring and Evaluation
Health Management Information System
The Health system has to respond to emergency without wasting any time i.e. the response time
is very less and the resources to tackle the situation has to gathered and deployed to the problem
point. However, the emergency, which can be managed like epidemics, do not crop up overnight.
The signs of such epidemics can be identified by various factors like rise in number of cases in
OPD or IPD, referrals to higher centres etc.
If the Health information system is made sensitive to such abnormalities as mentioned corrective,
action can be taken and the situation can be put to control. The strengthening of HMIS also
induces the sense of fear and sensitivity because of daily monitoring system and feedback, which
can be generated in a click of a button.
The state proposes set up system, which will have five-interface machine a toll free number a
web site to collate the date and back end software to store the data. The ANM Sub Centre will
call up at the Toll free number and the interface machine will read out the daily, weekly,
monthly, annual format as per the choice of the ANM and the ANM will feed the data by
punching the data through analogue telephone or SMS through mobile phone. This data will get
stored at the back end soft ware connected with to the interface machine. Through web site, the
administrator will get the data in any format it wants. The system will get data from PHC, CHC
and District Hospital in same pattern. At the end of the day the system can generate any data
regarding usage of health system, financial transaction taken place like JSY, immunization
incentive, closing stock, number of beneficiaries, attendance of the staff etc. If any centre
irrespective of the its status do not report for three consecutive day the system will send alert
messages to the cell phone of the higher authority. Even in case of emergency cropping up and
showing any trends by the reports collated, the system will give alert massages to the authority
concerned. The system will also check whether the caller is calling from the designated place or
not thus checking the number of absentees at the health centres in the periphery. The system can
be customized to generate any kind of reports with least effort.
NRHM PIP 2009-10: Chhattisgarh
Page 241
Health Worker Assistance System: One other outcome of this telephone based data collection
system can be that it could generate monthly individualised checklist of tasks for all health
workers which will be helpful in monitoring and supporting her effective service delivery as well.
A mechanism towards developing this is under consideration.
The previous year a baseline survey was conducted in the 2 districts, Rajnandgaon and Koriya
by SHRC to have an understanding on the process of data flow and the need of computerised
health management information system in the state.
From the study, it has been found that the ANM who is primarily located in the sub centre is
mostly busy in collecting data from the field. Apart from the routine information that she collects
from the field she also, have to collect information on different health related programme that
goes on from time to time. In case sub centres where with one ANM and one Male Health
Worker (MPW), the ANM gets some help/support from him and manage somehow. However, in
sub centres without any health worker she has to work alone. This renders management of sub
centre and data collection &compilation, and transmission to CHC difficult.
Some other infrastructural and HR issues lacking were those of the absence of safe and storage
system for the data/registers maintained by the ANMs, which results in loss of registers, and also
the durability of the registers is not ensured. Therefore, the loss of data and the problem of data
recovery as and when required. Besides these, there is no data operator/manager at the Subcentre/PHC and even at the CHC level. Another lacuna is that of the lack of computers for
electronic data storage and transportation of the same from the lower to the higher level.
Therefore, there is need to design concise and comprehensive formats and to design customised
software for entering the data. The software should be able generate reports as per need and
may be installed in computers at block levels. A trained data operators and district coordinators
would monitor the data and would be responsible for management of the district data operation
and validation of data, collected at village and block levels.
The proposed Health Workers Assistance System can be a good system where the monthly report
of ANM is analysed and a feedback as well as a checklist with task details for the coming month
is given back to her. Through this, the ANM’s will be in a position to prioritise their work and
based on this can go ahead with it.
The proposed amount in the previous year has been approved and this year an additional sum of
Rs. 1,53,42,800 is necessary to carry out the following programme for which the detail budget
and a brief introduction of the programme is given below:
NRHM PIP 2009-10: Chhattisgarh
Page 242
Documentation Management Solution and Digitization Services
A Document Management System (DMS) is essentially a computer system or a set of computer
programmes used to track and store electronic documents and / or images of paper documents.
This is basically a very powerful management system to document data electronically in lieu of
papers and manual filing and storing data. It has enormous advantages over the existing manual
system. In this context, SIGMA-Tech India Pvt. Ltd. Submitted a study report on the overall data
management and documentation to the State Directorate based on the health systems services of
Chhattisgarh. The report provides a number of suggestions that has the potential to improve and
provide faster, reliable documentation and retrieval of vital paper documents. There is a felt
need for establishing and maintaining such a system for the Department of Health & Family
Welfare, Chhattisgarh for which a proposal has been put forward. With reference to this
proposal, a number of activities – training of workforce, laptops and other supporting
environments – has to be undertaken. This system will be a part of the HMIS.
No additional budget is needed for this activity. The fund will come from administrative head.
Professional Health Management/Training of BMHOs and Reorientation of CMHO
In the previous year PIP the allocation of funds under head of Professionalization of Health
Management focused for training about 300 managerial staff including all BMOs, Programme
officers, Programme Management Unit officials and directorate level programme officials. The
training was proposed to be undertaken under Public Health Resource Network Distance
Learning Programme on processes of District Health Management, with a joint coordination of
SHRC and SIHFW. The fast track training was organized for DPMs, BMOs, other state level
programme officials and civil society members. The current training status is as follows
Current Status of trainings conducted:
So far, the total number of participants trained till December 2008 is 194. The details are as
stated below:
Table 3.26: Status of training and re-orientation of CMHO / BMHO
Sl.
No.
Batch
No.
of Date/Year
participants
1
1st
48
17th
to
22nd 1st
and 2nd
December 2007
September 2008)
2
2nd
30
25th to 30th August 1st
2008
NRHM PIP 2009-10: Chhattisgarh
Rounds completed (3 Rounds of
training/ batch)
(15th to 20th
Page 243
3
3rd
59
13th to 18th October 1st
2008
4
4th
57
1st to 6th December 1st
2008
Total 4 batches
194
Table 3.27: Details of participants trained so far:
Sl. No.
Designation
No. of participants
1
CMHO
3
2
MO
52
3
BMO
32
4
AMO
7
5
DPM
15
6
Civil Surgeons
2
7
DIO
2
8
DMO
2
9
DLO
4
10
DTO
1
11
DHO
3
12
BPM
5
13
BETO
10
14
BEE
2
15
DDA
4
16
AYUSH
2
17
Asst. Professors
2
18
Others(civil society/NGOs/DHS)
46
Total
NRHM PIP 2009-10: Chhattisgarh
194
Page 244
As mentioned the target is to train 300 officials, divided into 6 batches (50 per batch) out of
which 194, i.e. 4 batches, as proposed, have been trained, for the first round, and the first batch
has completed the second round of the same. Two more batches as proposed yet to be trained.
The training curriculum
Systematic coverage of all major health programmes and of all health systems
components in an integrated way.
Not to fragment health management and health administration from public health and
even clinical knowledge.
Based on an understanding of what problems district officers face in implementing the
national guidelines.
Mix of practical skills and understanding of first principles – not merely drilling in of
instructions.
High degree of adaptation to local specificities. The use of the district and state plan as
the tool.
Provide intensive post training follow up and support to the application of these skills
First round of training:
District health planning – basic tools
All aspects of child survival
All aspects of maternal survival
TB, malaria and HIV control programme.
Understanding how to design and conduct rigorous training programmes
Understanding how to design and conduct outcome oriented BCC programmes.
Understand how to manage ASHA and other community based programmes
Second round of training
Other aspects of RCH.
Some other disease control programmes.
Infrastructure, procurement, rational use of drugs, logistics management.
Quality of care systems.
NRHM PIP 2009-10: Chhattisgarh
Page 245
Legal framework of health care.
Constructing public private partnerships
Third round of training- could be optional- or only at state level.
Non-communicable diseases.
Urban health
Tribal health.
Hospital management.
Health management in very vulnerable groups.
Social protection and risk pooling.
Revision of the earlier topics.
The fast track training programme were organised at the state level. Resource person from
National level (NHSRC + PHRC New Delhi) and state level (including Health department,
Health consultant, public health expert and medical college). Last year target was achieved as
per the number of batches but number of participant were less. Accordingly the follow up of Fast
Track training was done.
1. Visited in Sarguja, Ambikapur, Bastar, Koriya, Raigarh, Rajnandgaon, Kawardha
district to involve fast track participant in preparing district health action plan.
2. Meeting with CMHO, DPM, Nodal officers and Fast Track district level participants.
3. List of participants to CMHO and urging them to involve them in DHAP.
4. Discussed Post Fast Track assignments as well as district specific needs.
The experience and outcome of the training was highly commendable. Another component in
addition to the institution training which has been the felt need to give impetus for the
participants is the study tour / field study and also some case studies and documentation of the
same which would enable them to have an in-depth grasp on the issue. Besides these, the
provision for attending state and national level workshops and conventions needs to be
incorporated. This will further enable the participants to build up their capacity and also grow
as future resource persons with better understanding of public health issues and concerns.
As budget for the proposed training will be carried forward for financial year 2009-10, hence no
additional budget is proposed.
NRHM PIP 2009-10: Chhattisgarh
Page 246
Community-Based Monitoring of Health Services
Community-based Monitoring of health services is a key strategy of National Rural Health
Mission (NRHM) to ensure that the services reach those for whom they are meant, especially for
those residing in rural areas, the poor, women and children. Community Monitoring is also seen
as an important aspect of promoting community led action in the field of health.
The provision for Monitoring and Planning Committees has been made at Primary Health
Centre (PHC), Block, District and State levels. The adoption of a comprehensive framework for
community-based monitoring and planning at various levels under NRHM, places people at the
centre of the process of regularly assessing whether the health needs and rights of the
community are being fulfilled.
Community monitoring is to review the progress to ensure that the work is moving towards the
decided purpose, and the purpose has not shifted, nor has the work been derailed in any way.
Such a review can help to identify obstacles in the work, so that appropriate changes can be
made to cross the obstacles.
Current Status:
Chhattisgarh has moved ahead in community based monitoring of health services under NRHM.
The State Mentoring Group has been formed and the Pilot Phase, which was initiated in 3
districts, has been completed. In the Pilot Phase in Chhattisgarh, Community Based Monitoring
of health services was implemented in 3 blocks each in districts of Koriya, Kabirdham and
Bastar.
To realize the objectives in these districts, the following steps and activities were undertaken as
per the norms and guidelines of NRHM. These are as follows:
Formation of State Mentoring Team- At the State level, the State Mentoring team was
formed, involving representatives of the state health department and state level
health sector voluntary networks. This team worked to develop community
monitoring in the state. It organized State level workshop and State level TOT with
State Health Mission.
Selection of State Nodal NGO- A Consortium of state level NGOs was formed as Nodal
Agency. Sandhan Sansthan, CGVHA and PFI-RRC were included in this
Consortium.
Districts were selected by State Health Department in consultation with civil society
representatives.
NRHM PIP 2009-10: Chhattisgarh
Page 247
Blocks were selected by District Health Officers and District Administration in
consultation with nodal persons.
PHCs and SHCs and Villages were selected by District Health Officials in
Table 3.28: Selection of Project Area for Community based monitoring
Districts
Blocks
Koriya
Khadgawan, Manendragarh, Jankpur
09
45
Bastar
Tokapal, Baastanar, Darbha
09
45
Kabirdham
Kawardha, S. Lohara
06
30
24
120
03 Districts
PHCs
09 Blocks
Villages
Table 3.29: Completion Status of activities as per MOU
Activity in MOU
Number
Publication of Guidelines
01
Status
Published a set of Two Guidelines
Published a set of three Folders
Published a set of two Posters
State Level 01Workshop ( 2
Days)
01
Organised on 16-17 August, 2007
State TOT Workshop ( 5
Days)
01
Organised on 16-20 December,2007
District Workshops ( 1 Day)
One in each district
03
Organised all 03 Workshops
District Kawardha: 27 January, 2008
District Koriya: 12 March, 2008
District Bastar:17 March, 2008
State level District Manager’ Workshop
was organized on 20-21 January, 2008
State level Consultation for Planning
Activities of Second Phase,11&12May 08
NRHM PIP 2009-10: Chhattisgarh
Page 248
Table 3.30: Status of activities of second phase (June-November, 2008)
Activity
Training of Trainers
PHC Monitoring & Planning
Committees Formed
PHC Monitoring & Planning
Committees Oriented
Target/Output
Planned
Output
Planned
Output
Planned
Output
Bastar
01
01
09
09
09
09
Koriya
01
01
09
09
09
09
Kabirdham
01
01
08
08
08
06
Total
03
03
26
26
26
24
Objectives
• To ensure regular and systematic information about community needs, which will be used
to guide the planning process appropriately
• To provide feedback according to the locally developed yardsticks, as well as on some
key indicators.
• To provide feedback on the status of fulfilment of entitlements, functioning of various
levels of the Public health system and service providers, identifying gaps,
deficiencies in services and levels of community satisfaction, which can facilitate
corrective action in a framework of accountability.
• To enable the community and community-based organizations to become equal partners
in the planning process. It would increase the community sense of involvement and
participation to improve responsive functioning of the public health system. The
community should emerge as active subjects rather than passive objects in the
context of the public health system.
• Community monitoring will also be used for validating the data collected by the ANM,
Anganwadi worker and other functionaries of the public health system.
Key Strategic action
a) Strengthening of VHSC (along with Mitanin as convener in it) will be effective for
community level monitoring. Some of the important monitoring results will come out in a
form of VHP. We are targeting to develop 5000 VHPs this year.
b) Focus on Jeevan Deep Samiti (JDS) for community monitoring and planning framework.
JDS includes community representatives and we have designed detailed monitoring
NRHM PIP 2009-10: Chhattisgarh
Page 249
c)
d)
e)
f)
/planning guideline for it. Strengthening JDS will provide effective monitoring at
DH/CHC/PHC.
MTs/DRPs (community group will be formed by selecting few MTs/DRPs in all blocks
i.e., 5 MTs and 2 DRPs per block) team will be used to monitor activities at
SHC/PHC/CHC. FCs will be instrumental in Community Monitoring Framework.
Mitanin Help Desk (MHD) will also be used as Community Monitoring desk. It is already
functional in 36 CHC/13 districts
We will develop roles of Zila or Janpad panchayat Standing Committee in it. The
involvement of Zila/Janpad panchayat Samitis will open an opportunity for the inclusion
of community representatives in structured and manageable manner. With this it will also
compliment NRHM guideline on decentralization and participation of various local
bodies
PHRN participants will be assigned some villages, sectors or blocks as per the strength
for monitoring / planning of the services. The existing human resource in blocks and
districts will also be used for this
For this year, the NGOs involved in the process in Bastar, Koriya and Kawardha will act as a
district level Resource Group for expanding community based monitoring in the whole district
through assimilation with the ongoing VHSC and Swasthya Panchayat Yojana processes. A total
budget of Rs 30,000 per block has been proposed for this facilitation.
Activities
In addition, three new districts will be taken up this year. For this, following activities will be
undertaken Strengthening of State Planning and Monitoring Committee
Replicating the pilot basis community base monitoring of health services in rest 15
districts
Implementation of the above Community Monitoring Framework in the selected districts.
The project period will be of 6 months.
Ensuring the village level monitoring through Mitanin cascade of MT/DRP
Ensuring the use of MHD/JDS in Community monitoring
Using PHRN participants or mentors for community monitoring
Ensuring the Zila /Janpad Panchayat related platform for community monitoring at
district level
NRHM PIP 2009-10: Chhattisgarh
Page 250
Regular meetings of the Monitoring committees need to take place even beyond the project
period. It is expected that after the project period, the need for such meetings will emerge from
the committee members themselves and this activity will go on as part of the VHSC process.
The overall responsibility of the activity shall rest upon the Community Monitoring
Framework supported by NRHM with the collaboration of NHSRC and in consultation with
State Health Resource Centre, Chhattisgarh.
Indicators
Replication of the community monitoring pilot base model in rest of the districts
No of Monitoring Committee formed at district/ block/PHC
No of Jan sunwai at block/PHC level
No of VHP used for advocacy at PHC/block/Zila level
Table 3.31: Total Budget for Community based Monitoring
Sl
No.
Component
Total
Amount
1
Budget for continuation of activity in 3 districts already covered under
pilot phase
270000
2
Budget for implementing Community based Monitoring in 3 new districts 2117000
Grand Total
23,87,000
Table 3.32: Budget for continuation of activity in 3 districts covered under pilot phase
Sl
Strategy/Activity
No.
Facilitation of Community based
monitoring in the other villages of
the district
Total budget for 9 blocks covering
3 districts
NRHM PIP 2009-10: Chhattisgarh
No.
of Participants
in Cost per Total
Unit
each unit activity activity
Amount
activity
6
Block/District
NGO
5000
30000
270000
Page 251
Budget for implementing Community based Monitoring in 3 new districts
Table 3.33: Budget Summary for implementing community based monitoring in 3 districts
Sl
Strategy/Activity
No.
No.
of Participants in each unit activity
Unit
activity
Cost per activity
Total
Amount
Block Level
1
Orientation of members of community monitoring
Block
1
20 members per block committee
5000
5000
PHC
3
15 members per PHC committee
2000
6000
Villages
15
10 VHC members per village
3000
45000
40 participants from Health dept, ICDS, PHED etc
10000
10000
Block
Orientation
Provider 1
Sub-Total
2
66000
Formation of Monitoring Committees
Block
1
30 participants (panchayat members/NGO/CBO 1000
for
members and PHC committee members)
meeting
block 1000
PHC
3
500
per
meeting
PHC 1500
Villages
15
500 per village for 2 7500
preparatory visits
NRHM PIP 2009-10: Chhattisgarh
Page 252
and 1 meeting
Sub-Total
3
10000
Gathering data and report
Data gathering on availability of health services by
committee members with facilitation by block NGO
through Village meetings, group discussions and
facility survey
Village data gathering and 15
report
1000
15000
PHC data gathering and 3
report
1000
3000
Sub-Total
4
18000
Conducting Jan Samvad/Jan Sunwai in each of the PHCs and blocks
Block Jan Samvad
1
5 panellists/experts, 200 participants
10000 per block Jan 10000
Samvad
PHC Jan Samvad
3
5 panellists/experts, 100 participants
5000 per PHC Jan 15000
Samvad
Sub-Total
5
25000
Facilitation cost for Block NGO
Block Co-ordinator
6
5000
30000
Office
6
2500
15000
NRHM PIP 2009-10: Chhattisgarh
Page 253
Sub-Total
45000
Per Block budget Total
164000
District Level
1
District Facilitation, training of trainers
District
workshop
Introducing concept
stakeholders
– 1
to
50 participants
6000
6000
Training of block level 1
team
20 participants from 3 block level NGOs
18,000
18000
2
Formation of District
monitoring committee
1
District level meeting
4000
4000
3
Orientation of District
monitoring committee
1
10000
10000
Sub-Total
4
Facilitation
district NGO
38000
costs
for
District Co-coordinator
7
9000
63000
Office
1
20000
20000
Sub-Total
83000
Per District budget Total
121000
NRHM PIP 2009-10: Chhattisgarh
Page 254
State level
1
State level workshop
1
30 participants for 2 days
50000
50000
2
State training of trainers
1
25 participants for 5 days
60000
60000
3
State level facilitation by 7
state Nodal NGO
State co-ordinator @ Rs 18000 plus office expenses 24000
@ Rs 6000
168000
State level budget Total
278000
Total Budget for new Sum Total ofdistricts
1. State level budget
2117000
2. District level budget for 3 districts
3. Block level budget for 9 blocks
NRHM PIP 2009-10: Chhattisgarh
Page 255
The State Level Resource Support: The SHRC
State Health Resource Centre (SHRC) is an innovative institutional capacity that was set up in
2002 by state health department of Chhattisgarh, under Sector investment Programme (SIP).
Worked as the backbone of the community based health sector reforms in Chhattisgarh, the
centre has been able to give shape for a number of successful models of community participation
in health like the "Mitanin Programme" and "Swasth panchayat.” For improving the supply-side
interventions on health care, it has developed "Equip approach" through a set of studies and
research. In order to improve the facility development and management, it was able to suggest a
comprehensive facility development package around the existing Rogi Kalyan Samiti setups, in
the form of "Jeevandeep Scheme.” Once the SIP was over, the SHRC was absorbed for providing
technical assistance in planning and imparting of NRHM. All the community-based components
under NRHM are being implemented also, by SHRC, for the state Government. The NRHM has
requested other states, to setup similar institutes.
The SHRC have been working as an additional technical agency to the department. It is
supporting on a three-year term under a renewable MOU between the State Health Society and
the SHRC. The SHRC MOU is ending by this financial year, which needs to be further
extended/renewed. The technical provided by SHRC support shall be as envisaged in the MOU
and as approved in the NRHM PIP. This is essential for continuing the SHRC’s support functionboth for community programmes and for capacity building. Basically, SHRC plays the role of
Community hand of NRHM in Chhattisgarh. It is also providing technical assistance to
programme and policy design and for support to implementation of innovative, effort and
process intensive new programmes. It plays a critical role in capacity building for district health
planning, through its national level initiative called PHRN. It gives timely inputs to the
government wherever it is necessary, in the areas of private sector regulation, insurance, and
many other initiatives.
In addition to the areas where SHRC is already working, we have incorporated the SHRC
technical support in the field of AYUSH mainstreaming and Medical education this year. In the
community level intervention, we are looking at SHRC on operationalising the Village Health &
Sanitation Committees. We are entrusting the capacity building of officials in district health
planning through the SHRC run national network called the Public Health Resource Network,
which have been actively conducting the trainings as planned.
Looking at the additional tasks that are given the growing need of additional hands to look after
many of the components, we are enhancing the budgetary projection for SHRC- still this is far
below from the NRHM allocation for SHSRCs in bigger states. Hike. This is basically to meet the
needs as per the varied tasks, projected work plan and programmes. The SIHFW shall
coordinate all training activities and institutions in the state and ensure the implementation of
the HRD policy as regards in service training.
NRHM PIP 2009-10: Chhattisgarh
Page 256
Table 3.34: List of functions carried out by SHRC
Technical
Assistance
Institution
Functions
The
State •
Health
•
Resource
Centre
•
Mitanin
Community level capacity building
Operational Research and Policy related Studies:
•
Programme evaluation studies
•
Assistance in Acts, Policy and programme development
•
Support to implementation of effort and process intensive innovationespecially on nurse practitioner, Mitanin certification, vocational ANM
stream and multiskilling, public health management distance education
training and district level planning
•
Developing comprehensive innovative models for malnutrition reduction,
in coordination with ICDS.
•
Coordination mechanisms to ensure convergence- with PRI, ICDS, PHED,
UNICEF, School Education
•
Mainstreaming of AYUSH
•
Operational research for HMIS
•
Support in medical Education Reforms
•
Support in Strengthening Public Health Systems
Table 3.35: Budget Summary for Technical Assistance to SHRC
Strengthening SHRC (Under Existing MoU)
Sl.
No.
Unit Description
Unit cost
Unit
Duration
1
Personnel Cost per month
476,300.00
1
12
Total
5,715,600.00
NRHM PIP 2009-10: Chhattisgarh
Page 257
2
Studies, Workshops and core
publications per event
110,000.00
1
10
3
Tour & Travel per person per month
8,250.00
10
12
4
Office Expenditures
88,000.00
1
12
1,100,000.00
990,000.00
1,056,000.00
5
Contingencies
5,500.00
1
12
66,000.00
Total
8,927,600.00
Sickle Cell Anaemia: (Detection, management and prevention of sickle cell anaemia in
Chhattisgarh)
Introduction:
Sickle Cell Anaemia is a group of inherited red blood cell disorders. Sickle red blood cells
become hard, sticky and shaped as sickles used to cut wheat. When these hard and pointed red
cells go through the small blood vessels, they stick together, clogging the flow of blood. This can
cause pain, a low red blood cell count (anaemia), or tissue death. Sickle Cell Disease (SCD)
often disrupts daily living with illness, pain, trips to emergency departments, stigma and a
compromised quality of life,” It can lead to a number of medical complications including stroke,
acute chest syndrome and organ damage. Children with Sickle Cell Disease will need special
medication and related medical care throughout their lives. Children affected with SCD are at
increased risk for severe morbidity (e.g., severe haemolytic anaemia, splenic dysfunction, pain
crises, and bacterial infections) and mortality, especially during the first 3 years of life. Between
6 and 18 months of age-affected children, most often present with painful swelling of the hands
and/or feet (hand-foot syndrome). Survivors may also suffer because of recurrent and
unpredictable severe painful crises, as well as “acute chest syndrome” (pneumonia or
pulmonary infarction), bone or joint necrosis, priapism or renal failure.
The public health implications of sickle-cell anaemia are significant. Its impact on human health
may be assessed against the yardsticks of infant and under-five mortality. As not all deaths occur
in the first year of life, the most valid measure is under-five deaths. An increasing proportion of
affected children who survive past five years of age but remain at risk of premature death.
Sickle Cell disease is a scourge in Chhattisgarh since long past. Approximately ten thousand
people die in Chhattisgarh State every year with some or other complications related to Sickle
cell disease.
NRHM PIP 2009-10: Chhattisgarh
Page 258
Prevalence:
This disease is distributed in the adjoining States like Madhya Pradesh, Maharashtra, Orissa,
Jharkhand and parts of Andhra Pradesh. However, a detailed survey has not been conducted yet
in Chhattisgarh State. The estimated prevalence rate of 15% carrier and 1.27% sufferer of the
disease in the state of Chhattisgarh
The hospital statistics and studies conducted by the postgraduate students of Raipur Medical
College reveal that the following castes and the tribal populations are predominantly affected in
the region. (Ref. Shukla 58, Makhija 84, Singh 85). Negi at.el, sathe, kar at.el & kate at.el have
reported almost the same prevalence rates in Panika, Agharia, Gond & Halba (Bastar)
population of the region.
Table 3.36: Distribution of sickle cell carrier amongst different group of population
Caste
% of total population of Incidence of Carrier in these cast groups
Chhattisgarh
SAHU
12 %
25.7 %
KURMI
10 %
20 % including Mahavar, Verma, Parganiha, Sinha,
Chandravansi, Nayak, Bais, Baghel and others.
Schedule
Tribe
18 %
20 %
Schedule
Caste
18 %
17 %
Total
58%
82.7%
As per 2001 census the population of Chhattisgarh is 20795956 On rough estimate based on the
prevalence rates of Sickle cell disease, the affected population works out to be around 35 lakhs.
The Present Scenario:
Sickle cell disease affects mostly the socially and economically poor sections of the society. The
table shown at page one shows that the persons belonging to Schedule Tribes, Schedule Caste
and Backward Class making a formidable 58% of the total population are prone to sickle cell
disease. The carriers contribute to add to the scourge due to matrimonial alliances between
them. Thus, the disease goes on, in perpetuity telling upon heavily on the human resources of the
State of Chhattisgarh. The efforts that have been made to estimate the magnitude of the problem
let alone the question of tackling it is far from satisfactory. Proper diagnostic facilities for this
disease are not readily available. There is always a shortage of blood and exchange facility. It is
important to note that if no serious attempt is made, the carriers may multiply in geometrical
progression. Since the plan is to tackle a genetic disease, the aims have to be long term. The
NRHM PIP 2009-10: Chhattisgarh
Page 259
public and medical practitioners need to be sensitized to the issue. Examples are available where
screening of carriers, followed by counselling was done.
It has been found that in a family there are more than one patient, which is only because, lack of
knowledge about the transmission of disease and lack knowledge about the prevention measure.
Objectives
1. Early detection of the patients by screening the target population.
2. Counselling of the family to break the sickle cell cycle in the generation by
preventing the birth of sickle cell child.
3. Intervention to improve quality of life of the affected items (sickle cell disease and
trait)
Strategies and activities
Screening of the target population for early detection of disease: The main aspect of
comprehensive care for sickle cell anaemia patient is early detection to take the measures and
intervention for preventable problems with pain medication, antibiotics, nutrition, folic acid
supplementation and high fluid intake. As well as to identify the couple at the risk of having
affected children so as to prevent the sickle cell cycle.
For the case wise effective management of the patient’s surveillance is important, to screen the
target population an effective affordable technology and which can reach at the large proportion
of community is required. for the early detection and the screening of the population at mass
scale a solubility test can be a tool to detect at sub centre level and if the patient is positive for
the solubility his blood sample can be send to the community health centre for the
electrophoresis. The community health centres pathology can be well equipped for doing the
solubility and electrophoresis and if required a training of pathologist and ANM can be done at
the block and district level.
The target population for the screening is adolescent (22% of total population), new married
couple, pregnant women and all the new born of the affected families. There is the evidence that
the neonatal screening for sickle cell anaemia, when linked to timely diagnostic testing, parental
education and comprehensive care markedly reduces morbidity and mortality from the disease in
infancy and early childhood
Prevention:
The management cost of these patients is very high and resources are limited. Hence, the
prevention appears to be the only solution in present circumstances to break down the sickle cell
cycle (transmission of disease from one generation to another). The risk of having affected
NRHM PIP 2009-10: Chhattisgarh
Page 260
children can be detected before marriage or pregnancy; however, to do so requires a carrierscreening programme.
With the advances in molecular genetics, it is possible to detect the defect at early stage of
pregnancy i.e. by taking chorionic villus sampling from the 9 weeks of pregnancy. The high-risk
couple for these disorders should be identified at the time of antenatal care each pregnancy
should be monitored. The couple should be given appropriate counselling after prenatal
diagnosis and such affected child can be aborted as per the legal norms for the genetic disorder
(MTP Act). The prevention of the birth of the sickle cell child can also be possible by stopping
the marriage of the two sickle trait persons, which required a mass education, and counselling of
the adolescent as well as the decision makers in the family. For this, a counsellor at the district
can be appointed and can be trained for the genetic counselling and the counselling for the
sickle cell affected family can be done.
Surveillance and counselling centre:
To detect sickle cell patient and improve their quality of life. A study shows that sickle cell
patient domain of physical, psychosocial, cognitive and morbidity were affected. In Sickle Cell
Anaemia, patient playing and mobility were most affected. There was feeling of sadness or
disinterest and lack of support from teachers. The school attendance, vocational achievement
perception, entertainment and participation in cultural activities were also affected. The
intensity of weakness and pain was greater in Sickle Cell Anaemia children who felt that they
were affected by a major illness. The unusual finding was that the Sickle Cell Trait children also
showed affection of all domains as compared to normal children, which was perhaps due to the
stigma of the disease.(A. Patel)
To improve the quality of life of sickle cell anaemia patient need a case-to-case record and
counselling. The individual case-to-case record can be kept at the block and the district hospital.
For the prevention of the sickle cell cycle and to Improve the quality of life of sickle cell patient
computerized surveillance system can be established where a case to case monitoring can be
done which can be done through the hospital untied fund or with the help of Jeevan Deep
Samiti.
In this financial year screening of 3 lakhs children will be done. These children will be those
from Ashram and Kasturba Gandhi Balika Vidyalaya. The additional budget requirement will
for salaries of counsellor. The other activities proposed will be carried out with the previous
year’s budget allocation.
Table 3.37: Budget summary for counsellors for Sickle cell control programme
Sl. No
Budget Head
Unit cost
NRHM PIP 2009-10: Chhattisgarh
No. Of units
duration
Total
Page 261
1
Counsellors
8000
18
12
1728000
Budget: No additional Budget is required for the current year. The previous year’s budget
allocation will be utilised.
AYUSH component under NRHM for 2009-10
District Ayurveda hospitals currently provides Ayurveda OPD and IPD services from 30 bed
hospitals, as currently sanctioned, including Panchakarma and Ksharasutra. The need to
provide all the AYUSH health care services under one-roof is essential for popularization of
AYUSH services. Special therapies under AYUSH are effective means for treatment of chronic
illnesses, life style disorders that have become common. Most of the patients seek AYUSH health
care services as an alternative treatment for chronic ailments where the modern medicine offers
little help. This demand of patients necessitates development of District Ayurveda hospital as
AYUSH polyclinic to cater all the services from a single point of delivery. Operating District
Ayurveda Hospitals as AYUSH polyclinics with all the specialized health services of AYUSH will
provide patient the opportunity to select therapies according to their choice, a major step for
consumer sovereignty. As first step, the plan is to develop Unani, Homeopathy and Naturopathy
and yoga clinic for all the AYUSH OPD services under one roof for 6 district hospitals. Such a
polyclinic has already been developed in Jagadalpur district Ayurveda Hospital. The technical
manpower for the Jagadalpur unit is not needed. However, renovation and partition of 4 district
Ayurveda Hospitals and development of Panchakarma services in Durg district Hospital and
Ksharasutra in Bilaspur district Hospital, procurement of Equipments and essential medicines
are required for realising AYUSH polyclinic plan. The plan excludes repairing and partitioning
of the Dalli Rajhera as the hospital building is rented.
The proposed OPD services require technical manpower – one Homeopathy physician, one
Unani physician and one Naturopathy physician. There is also requirement of 2 female and 2
male Panchakarma shayak for the effective functioning of these specialized services in Durg
and Bilaspur. 2 trained OT assistants and one part time sweeper for both the institutions as
auxiliary staff are additional manpower requirement.
Table 3.38: Budget summary for developing AYUSH polyclinic
S. No Unit Description
Unit Cost
1
Construction, Repair and partitioning 5,00,000
2
Procurement of Essential equipment,
No of Units Duration Total Cost
5
1
25,00,000
10,00,000 2
1
20,00,000
60,000
6 months
21,60,000
Appliances & Essential Medicines
3
Technical experts
NRHM PIP 2009-10: Chhattisgarh
6
Page 262
4
Supporting Staffs
20,000
2
6 month
Total cost
2,40,000
69,00,000
Flexible fund for AYUSH Deep Samiti for monitoring
District Ayurveda officers are placed in all the 16 districts of the state. District Ayurveda
officers are functional in all the districts. District Ayurveda officer shoulders the major
responsibility of administration, execution of Central and state level plans at the district level,
monitoring the AYUSH health care institutions efficient functioning in the district ,management
of AYUSH human resource and supply of essential AYUSH medicines to the District Ayurveda
Hospitals and AYUSH dispensaries in the district.
Monitoring of District Ayurveda hospital, AYUSH dispensaries and AYUSH wings in allopathic
centres for effective functionality is ensured by District Ayurveda officers. Monthly review
meeting of the AYUSH physicians and understanding the difficulties faced by the Physicians as
infrastructural gaps, manpower gaps and facility gaps are assessed by the District Ayurveda
officers and solutions provided by District Ayurveda officers.
Monitoring of AYUSH institutions in difficult areas and far off places by District Ayurveda
Officer needs to be supported by conveyance facility as hiring of the vehicle for mobility within
the district and to the state office. This facility can enhance monitoring process and supervising
activities under their jurisdiction, the other utility of mobility support are monitoring the camps
conducted in Godgrahita villages and other supervisor activities of AYUSH institutions
construction within the district .Minimum two visits to every District Ayurveda Hospital, AYUSH
dispensary and AYUSH units under mainstreaming in a year is Essential. Visiting and of
monitoring 20% of AYUSH dispensaries in a month and once monitoring of District Ayurveda
Hospital. Conduction of 2 blocks level meetings of AYUSH medical officers in month and
assessment of the monthly patient data and planning for improvement of services. In the districts
where Ayush centres are present in the blocks there meeting can be conducted in any dispensary.
This fund will be transferred to District AYUSH DEEP SAMITI where the District Ayurveda
Officer can draw the money from the Samiti. The District AYUSH DEEP SAMITI will be
nominated for monitoring of utilization of untied funds. The district Ayurveda Officer can hire a
vehicle, from the flexible untied fund for effective monitoring of the districts. The fund of 1,
00,000 will be provided to the District Ayurveda officer by AYUSHDEEP SAMITI.
Table 3.39: Budget summary for Ayushdeep Samiti
S.No Item
1
Unit cost No of units Duration Total cost
Flexible fund for AYUSH DEEP SAMITI 1,00,000
NRHM PIP 2009-10: Chhattisgarh
16
1
16,00,000
Page 263
Essential medicine for AYUSH centres in rural, remote and tribal areas
AYUSH Heath care service cater services with a large group of institutions with total coverage
of services in rural, remote and tribal areas. AYUSH Dispensaries are 650 dispensaries in rural
and remote areas. The Tribal AYUSH units are 399 and total AYUSH centres serving for health
care in rural and tribal areas are 1049.To ensure timely availability of quality medicines and
supplies in these health institutions in keeping with the needs of the patients in the tribal areas.
These medicines will prevent the AYUSH medicine deficit in the tribal areas and ample medicine
provision for the tribal areas. Every dispensary shall be provided by a fund of 25,000 as
medicine procurement cost. The department of AYUSH shall procure the deficient medicines
depending on the disease prevalence and patients needs.
Table 3.40: Budget summary for Ayush medicine
S.No Item
Unit cost No of units Duration Total cost
1
25,000
Essential AYUSH medicines for rural,
remote and tribal areas
399
1
9975000
Additional manpower for AYUSH units in CHC and PHC
The AYUSH Centres in tribal areas need to be fully functional with required staffs to provide
health care services. In 86 blocks of tribal districts no. of CHC’s where AYUSH physician is
placed is 7. Compounders and Dispensary attendants are in place at 18 centres whereas the
posts of Compounders and Dispensary attendants are needed for 54 CHC’s for effective
functioning. 100 PHC’s in the Tribal areas where AYUSH physicians are already placed for the
AYUSH Health services. The services in these centres can be enhanced by placing a compounder
for supportive services.
Table 3.41: Additional manpower for Ayush Units in CHC and PHC
S.No Item
Unit cost
No of units
Duration (months)
Total cost
1
Man power for CHC
10,000
52
12
62,40,000
2
Man power for PHC
6,000
100
12
72,00,000
Total
NRHM PIP 2009-10: Chhattisgarh
1,34,40,000
Page 264
Telephone Connection for AYUSH district hospitals:
Coordination and linkage among District Medical Officers and District Ayurveda officers is not
effective. The communication among AYUSH physicians is essential for referral of needy
patients, continuous support by district Ayurveda officers and identification of critical difficulties
in District Ayurveda Hospital. Timely reporting and data validation will be enhanced by the
provision of telephones in District Ayurveda hospitals. Unit cost per connection will be around
Rs 1000 as yearly recurring cost and the establishment cost will be borne by Ayushdeep Samiti
of the institution. Only limited number of outgoing calls from the facility will be allowed through
this phone.
Essential maternal and child health training for AYUSH doctors
The AYUSH doctors in the state are playing a major role of provision of Health care services.
Chhattisgarh has a major bottleneck in provision of equivalent health care services in the state
with difficult terrains with poor service levels. Considering the Underserved areas and tribal
remote areas the Government has taken important steps of posting AYUSH physicians in
mainstream health. Understanding the critical role of AYUSH physicians in health care in
Chhattisgarh recurrent training of AYUSH physicians is essential. The training of AYUSH
physicians for Essential Maternal and Child Health has been initiated in the state by the budget
allocation under NRHM. At present the targets to be achieved by the budget allocation of 200809 is the training of 360 AYUSH physicians. The recruitment process of 297 is initiated and the
AYUSH physician will increase by approximately 150.The training of these physicians for
Maternal and Child Health is essential
Decentralized training in all the three Government Medical Colleges of Raipur in collaboration
with the doctors who have under taken TOT training for facility based new born care in IMNCI
to prevent extra absence in the Dispensary which can create difficulty to the patients.
For this training 15 physicians will be grouped under one batch, the total batches to be trained
will be approximately 10. Module formation will be executed by experts selected and this
prepared module will be incorporated in all the Nodal agencies for training. Total number of
days involved in training total 12 days with 8 days training for child health and maternal health
training for 4 days. Ayush component for the training will be undertaken by Government
Ayurveda College (BAL roga, stri, and prasuti tantra vibhag) of Raipur. Module formation,
printing, training cost and boarding& lodging of AYUSH physicians will account up to 1, 00,000
per batch.
AYUSH physicians trained for Essential Maternal and Child Health training in the first phase
will be deployed in the 24*7 PHC and CHC for provision of Maternity Services all round the
clock.
NRHM PIP 2009-10: Chhattisgarh
Page 265
Table 3.42: budget summary for training of AYUSH doctors on Essential Maternal and Child Health
S. no Item
1
Unit cost No of units Duration (months) Total cost
Training of AYUSH doctors 1,00,000
for Essential Maternal and
Child Health Training
10
1
10,00,000
Public health management training for AYUSH MOs
AYUSH medical officers play a critical role in the delivery of health services in remote and rural
areas. Posts of AYUSH doctors have been created in Allopathic centres by the state government
for filling the manpower deficiency in mainstream health. Continuous training of AYUSH
physicians is essential for provision of quality services. The AYUSH professionals that are
District Ayurveda officers and AYUSH Medical officers will play a major role as health
managers of the districts and blocks and will continuously work for quality services, planning,
and execution of district and block level AYUSH plans. The AYUSH health planning so far is
centralized with the department planning the activities at the state level. The micro level
planning is deficient in the district and dispensary level where the need of the same is not
reflected in the AYUSH planning. So the training of District Ayurveda officers and AYUSH
medical officers need to be trained for basics of public health perspective of Health, assessing
the needs of the district and block ,how to plan a good district level and block level plan and
execution of the same. This training will help the physicians to get the deeper knowledge of
planning and management that is deficient now. 16 district Ayurveda officers and one AYUSH
medical officers from all the district depending on the higher service grades will be selected for
the training. Those matching one criterion that the physician selected for the training does not
retire in next three years, will be selected for 32 members. The state level planners for
department of AYUSH also need to be trained and 8 members from the state involved in higher
level planning ,so the total members for the training are 40 and the training schedule will be of 5
days. This training will be conducted by State Health Resource centre.
Table 3.43: budget summary for Public Health training of AYUSH doctors
S. no.
Items
Units
1
Training of AYUSH doctors for 1,50,000
public Health Management
No of units
Duration
Total cost
1
1
1,50,000
National level consultative workshop for AYUSH mainstreaming
Mainstreaming of AYUSH needs to be major strategy for uniform service provision at all the
allopathic centres with complementary care. This activity of co-location and development of
NRHM PIP 2009-10: Chhattisgarh
Page 266
AYUSH centres in allopathic units needs to be planned by computing the needs. This planning
needs a consultative workshop of AYUSH doctors in activities under taken by NRHM and
addressing the needs of the physicians. First workshop for computing the needs of health care
institutions in Chhattisgarh, second workshop is envisaged for a detailed planning on the
mainstreaming component. The third round of workshop needs to be undertaken for preparation
of road maps for the activities undertaken in NRHM for mainstreaming AYUSH. For workshop
of 16 District Ayurveda Officers and 6 members from the State for the planning board and
execution of mainstreaming component, with involvement of external experts for mainstreaming
as 8 members (total 30 members) for computing needs, detailed planning and for preparation of
road map for AYUSH mainstreaming and selected physicians of dispensaries need to be trained
for implementation of road map at the specific districts. At every district level, four physicians
are selected to be trained for the successful implementation of mainstreaming component at all
the districts.
The AYUSH physicians of the units created in CHC and PHC need to cater AYUSH services and
they are mainly posted in the centres .Total 434 Ayush physicians are present in CHC and PHC
in Tribal Areas, these physicians need to be trained for handling the services in CHC and PHC.
These physicians need to be trained for handling the services and serve as agent of
implementation of mainstreaming component in PHC and CHC. They are grouped in a batch of
35 physicians to be trained for 3 days. State Health Resource Centre is nominated for the
execution of the national level workshop.
Table 3.44: budget summary for AYUSH workshops
S.
no.
Items
Units
No of units
1
Workshop for Dist Ayurveda 5,00,000 1
officer/State implementers and
External experts
3
15,00,000
2
Training of AYUSH physician 50,000
for AYUSH Mainstreaming
1
7,50,000
3
Documentation and publication
1
1,00,000
15
1,00,000 1
TOTAL
Duration Total cost
23,50,000
AYUSH training for ANMs and Anganwadi workers
As a major intervention of mainstreaming the Department of AYUSH has included the training of
ASHA in AYUSH based principles, this training has already completed in the State of
Chhattisgarh as training of Mitanni’s for Propagation of AYUSH preventive principles and home
NRHM PIP 2009-10: Chhattisgarh
Page 267
remedies as herbal treatment. As an innovative strategy, the department of AYUSH needs to train
the Anganwadi workers working for Mother and Child Health and the ANMs, who are the grass
root level health care providers in Allopathic units. The Anganwadi workers can enhance the
child nutrition and Maternal Health by the AYUSH herbs. These ANM’s and Anganwadi workers
can propagate the AYUSH based preventive principles and herbal remedies for common public.
As first phase of training the 35,000 Anganwadi workers are to be trained for AYUSH based
heath principles for maternal and child health. In the next phase, the 5000 ANM’s can be
trained. The training will be conducted at the block level with two days training by State Health
Resource Centre.
Table 3.45: training of anganwadi workers and ANMs on AYUSH medicines
S. no Items
Total participants No of Days
Per day cost
Total cost
1
Anganwadi
workers
35,000
125
87,50,000
2
Training
material
35,000
Total
2
1(Unit Cost)
50(per module) 17,50,000
1,05,00,000
Training of paramedical staffs for AYUSH
The major supporting staffs of the Ayurveda dispensaries are compounders. A large cadre of 725
compounders working in AYUSH health care sector. The compounder handles record and
medicines. Medicine preparation and dispensing to the patient is the primary work of
compounders. The compounders are not trained for preparation of simple Ayurvedic herbal
combinations. To enhance the performance of compounder and for the patient to receive correct
herbal combination for the ailments the compounder’s essential needs to be trained. Right
medicine to be dispensed is very essential for proper cure of diseases and by training of
compounders, the right method of dispensing of medicine can be inculcated in the compounders
Ayurvedic medicines need to be stored with caution and basic understanding of the herbal
combination. This basic understanding of preservation of Ayurvedic herbs need to be
incorporated in the compounder .As compounders are not trained for preservation and
preparation of herbs. Tons of Ayurvedic medicines are wasted with improper knowledge of
medicine storage and this can be avoided by training of AYUSH compounders for better methods
of medicine storage. The compounders are grouped in a batch of 40 members and trained at
Government Ayurveda College and 6 district Ayurveda Hospitals as 4 days training. In the first
NRHM PIP 2009-10: Chhattisgarh
Page 268
phase approximately 400 compounders needs to be trained for Medicine preparation and
dispensing.
Table 3.46: Training of paramedical staffs for preparation, storage and dispensing of AYUSH
medicine
S. no.
Items
Units
No of units
Duration
Total cost
1
Training Compounders for
medicine preparation, storage and
dispensing
75,000
10
1
7,50,000
.
Supporting AYUSH cell in SHRC:
The focus of NRHM for AYUSH has increased tremendously in Chhattisgarh. As a special
initiative for improvisation of AYUSH health care services and educational system in
Chhattisgarh. New initiative under NRHM has conceptualized AYUSH technical assistance cell
in SHRC. This ideology has improvised the planning skills of Directorate AYUSH, betterment in
implementation of programmes and formulation of better monitoring strategy. For the same
purpose, two technical consultants have been appointed under SHRC. To support the existing
cell for efficient functionality this needs budget allocation as salary for existing technical
consultants. To enhance the support to the existing cell additional man power are required as
Accountant, who will be handling the budget allocation to the districts and dispensaries by
various agencies and tracking the money inflow and outflow in the department. This will
facilitate for better functioning of the administrative department of AYUSH. To assist the finance
officer two-office support hands are required. For consultation and support of Experts as short
term consultants is essential for the AYUSH cell SHRC for enhancing the planning skills and
improving the technical advisory To support the new financial technical group budget
allocation under NRHM is to be materialized
Table 3.47: budget support to SHRC for supporting AYUSH Cell
S. No Unit Description
Unit
Cost No
(month)
Units
Of Duration
(year)
Total Cost
1
Personnel
programme 20,000
coordinators AYUSH
2
1
4,80,000
2
Salary For Accountant
17,000
1
1
2,04,000
3
Office Support hands
15,000
1
1
1,80,000
NRHM PIP 2009-10: Chhattisgarh
Page 269
4
Monthly Recurring Cost And 50,000
Mobility
2
1
12,00,000
5
short term provisional fee and 3,000
travel for technical experts
50(days)
1
1,50,000
Total Cost
22,14,000
Consultancy for developing an action plan for AYUSH epidemic management
Provision of health care services under mainstream by AYUSH is a constant effort under taken
under NRHM. The involvement of AYUSH health care professionals in national health
programmes is a major intervention in inclusion of AYUSH in public health. The support
provided by AYUSH doctors in National programmes and Epidemic control is not commendable
because the efforts under taken are not coordinated with the Directorate health services and at
all the levels of Health care provision The Support by AYUSH manpower in national
programmes is aimed at inclusion of AYUSH health care services for public. AYUSH based
principles can be used for epidemic control or even as palliative management. EPIDEMIC
control is a new and innovative strategy in AYUSH that is still under developed with less
research and defined protocol. A book can be developed and printed for AYUSH based Epidemic
control after the consultancy for Action plan for Epidemic control. The AYUSH based protocol
need to be developed for Epidemic control.
To fill the gaps in a similar intervention as that implemented in Kerala in the form of Integrated
epidemic cell ,where disease surveillance and Epidemic control under AYUSH guidelines was
included in PIP 2008-09 for recruitment of technical consultant as the AYUSH based protocols
are essential for the epidemic control team to function. This amount shall be re-appropriated
and carried forward for consultancy for developing plan of action for epidemic control with
publishing of the recommendations by the expert in the year 2009-10.
Support to maternity and child wards in government Ayurveda Colleges
The development of Maternity and Child ward was featured in PIP 2008-09, with the placement
of Technical Experts and other supporting staffs as 3nurses, peons and Sweepers for the wards.
The Technical Experts as one obstetrician and Paediatrician have been recruited and the
Functioning of the experts initiated. The four months’ Salary for the experts and other staffs need
to be provided by the NRHM flexi pool.
AYUSHDEEP Samiti
The state is having 7 district Ayurveda hospitals and 692 AYUSH dispensaries. Also as a part of
mainstreaming AYUSH, the infrastructural development is essential to provide better services in
a systematic manner. As identified by the state this could be addressed by setting up facility
NRHM PIP 2009-10: Chhattisgarh
Page 270
management committee in the same line of Jeevandeep Samiti in AYUSH facilities. Accordingly,
a programme in the name of Ayushdeep Samiti is being drafted where setting up quality criteria
for AYUSH facilities, training of functionaries on facility development as well as management,
untied funds for up gradation of facilities. Dissemination of guidelines, registration of
participatory Ayushdeep committee and initial training was budgeted as amount 34, 00,000 in
NRHM PIP 2008-09.Due to certain reasons the fund is not utilized in 2008-09 which will be
carried forward for to next year PIP 2009-10.
Table 3.48: Budget summary for AYUSH Deep Samiti
S. no.
Items
Units
No of units
Duration
Total cost
1
Technical Experts
30,000
2
4
2,40,000
2
Supporting Staffs
52,000
1
4
2,08,000
Total
4,48,000
AYUSH melas in Block and District head quarters
Popularization of Ayurveda based curative care and promotion of Indian systems and
homeopathy needs to be further emphasized as the deserving level of outreach still lacking in
want of proper facilities, infrastructure and man power. In order to bridge this alternative
strategy needs to be worked out like putting consolidated efforts pooling the available manpower
to centralized location where people could mobilize and all available services could be provided
along with effective IEC on planned manner. Already the department of AYUSH is
incorporating the Godgrahita scheme where the AYUSH physician selects neighbouring 5
villages where any other form of Health care services is not present and they conduct Health
camps in these villages once in a week .If this Godgrahita scheme is funded by this AYUSH
melas scheme approximately 5 villages by every AYUSH dispensary will be benefited by health
care services. The budget allocated for this component is 68.40 lakh in NRHM PIP 2008-09, due
to certain reasons the fund for this component was not utilized. The same fund will be carried
forward from 2008-09 to 2009-10.
AYURVEDGRAM
To popularize the AYUSH promotive, preventive and curative principles in the villages the
Chhattisgarh Government has initiated the Ayurvedgram scheme as pilot project in 25 selected
villages out of 121 selected villages by department of AYUSH as Ayurvedgram .In these 25
villages health melas and IEC is conducted to provide Ayurveda health care services with basic
concept of health and maintenance of Health with the budget allocation of 1,00,000 lakh rupee
per village .This scheme is extended to all 121 villages in the financial year 2009-10.The
NRHM PIP 2009-10: Chhattisgarh
Page 271
Ayurvedgram concept was included in PIP 2008-09 with a fund of 10,00,000 rupees. Due to
certain reasons, the amount for training of participants in AYUSH is not utilized. This shall be
carried forward to PIP 2009-10 as training (2-day workshop) of all 121 Ayurveda physicians of
Ayurvedgram for creation of understanding of the scheme and effective implementation of the
action plan in all the villages.
AYUSH Component under NRHM for 2009-10
Table 3.49: AYUSH components Summarised
S. no Components
Budget (in lakhs)
1
Flexible fund for AYUSH deep samiti for monitoring
16
2
Essential
areas
3
Additional manpower for AYUSH units in tribal CHC and PHC
134.4
4
Essential maternal and child health training for AYUSH doctors
10
5
Public health management training of AYUSH Medical Officers
1.5
6
National consultative workshop for creation of road map of AYUSH 23.5
mainstreaming
7
AYUSH training for ANMs and anganwadi workers
105
8
Training of paramedical staffs of AYUSH
7.5
9
Supporting AYUSH cell in SHRC
22.14
10
Support to maternity and child ward in government Ayurveda 4.48
college
11
AYUSH melas in block and district head quarter
12
Ayurvedgram
medicine for Ayush centres in PHC/CHC in tribal 99.75
Total
42427
Third Party Monitoring
The NRHM has put forward a very much useful mechanism of community based monitoring of
health services and facilities. A participatory framework from top to bottom level has been
NRHM PIP 2009-10: Chhattisgarh
Page 272
derived under this framework. Pilot activity towards materializing the community based
monitoring has been initialized and this is being scaled up during coming financial year. The
internal monitoring part through the HMIS and routine reporting mechanism are being
strengthened through SWOT analysis, field studies and innovative strategy, which may take some
more time to take good shape. But the third part of triangulation of monitoring, the external
analysis is totally dependent on the major national studies like NFHS, SRS, CES etc. The SHRC
has conducted some of the studies but they were largely looking for evidence based planning
rather than improving programme management. The joint review mission and other review by
government of India are largely based on field level observation where primary data are absent.
Due to lack of state specific studies and reports, area-wise lacunae are not being pointed out in
an adequate manner, which makes the planning as well as programme implementation totally
dependent on internal data and state averages received from National surveys. To have the state
specific/regional/district/sub-district data is very much critical in order to take forward the
programme as well.
Present system of Program monitoring is done through routine reporting and some amount of
checks by the district and blocks officials. This form suffers from a number of deficiencies – chief
among them being the lack of time of the concerned authorities that makes on the spot
monitoring sporadic and knee jerk reactions to crises in the field. Using reported data for
monitoring is also not very effective as these are too expensive for any kind of direct analysis at
the point of collection in addition to the tendency to falsify data to cover up non-performance in
its attempt to ensure quality service delivery at the frontline and first referral level. The program
will now move away from traditional ways of monitoring service delivery through routine
reports and surprise checks.
In order to have effective monitoring, feedback has to be continuous, based on a set of quality
indicators with mutual agreement of all stakeholders - neutral and unbiased. Monitoring data
will require extensive analyses to show trends and shortfalls so that these can be rectified on a
continuous basis instead of one-time knee jerk reactions. Ideally, this should also be done by an
independent agency that looks at the situation with a third eye but with clear guidelines to
prevent subjective interpretations. The services of dedicated professional staff will be utilised
who will visit, evaluate and work with the resultant data to provide an analysis of the situation.
This will help health administrators to use such data to conduct regular reviews and pinpoint
gaps in program implementation.
It is therefore planned to monitor some aspects of program implementation using a third party /
agency that is specially recruited for the purpose.
The purpose of program monitoring is mainly:
1. To provide adequate feedback to health Administrators on the Quality of programme
implementation.
NRHM PIP 2009-10: Chhattisgarh
Page 273
2. To support administrators to provide support and attention to selected clusters and areas
of intervention based on the feedback.
3. To provide feedback and end use monitoring of supplies, untied funds to improve the
quality and efficiency of governments supply estimation and distribution.
4. To provide adequate data for reports.
5. To provide lessons on programme design and supply management.
6. To provide data for program advocacy in order to feed into the work of the NRHM cell
PHC /CHC and SHC Quality as measured by the facility quality-monitoring format that
observes and scores each centre on a number of mutually agreed indicators, which will include
1) Supplies: the presence, adequacy, maintenance and use of essential equipment
the facilities.
supplies in
2) Staff presence and patient load and regularity of outreach visits: Head count of staff and
patient load and details of outreach visits and comparison with reported data.
3) The Sanitation / cleanliness Quality: An observation schedule that measures health facilities,
maintenance
4) Safety and Waste disposal
5) Use of Grants
6) Record maintenance
Similarly, the outreach of various programme components also could be monitored.
The third party co-opted for the purpose will take on the role of visiting health facilities and
reporting on about 5-10% of them every month. This will ensure that program-monitoring data
will be based on a minimum number of health facilities, which will be representative of the field
situation. It will also ensure that at least 50% of facilities will be evaluated externally each year.
The third party will engage monitors who will visit a minimum number of schools each month
and canvass the monitoring schedules. The data provided by the monitoring schedules will be
collated at a central point and analyzed along mutually agreed lines to produce a report on
implementation.
By allocating the ‘slog work’ to a third agency it will be possible to free the time of the health
administrators for qualitative work and to devote time to strategizing on next steps, evolving
NRHM PIP 2009-10: Chhattisgarh
Page 274
creative solutions etc. The authorities will use the data to plan for support training, as well as
give the weak institutions more focused direction and attention.
Table 3.50: Budget summary for Third Party Monitoring
Unit Description
Unit Cost
No. of Duration
Unit
Total Cost
Contracting
in
third
party 1000000
institutions/groups / advertisement for
recruitment of HR
4
1
40,00,000
Miscellaneous
expenditures
dissemination of reports etc.
4
1
10,00,000
like 250000
Total
50,00,000
Filling up vacancies and Human Resource management
The programme management staffs under NRHM were appointed by government of India in
2005. In the state vacant District Programme Management Unit (DPMU) and Block programme
management unit post under NRHM were filled in year 2008. Still one DPM, 7 DAM and 2
DDO, 83 block programme manager and 70 block data cum account assistant positions are
vacant. At the state programme unit consultant position for maternal health, child health,
infrastructure, Procurement expert, BCC/IEC, the monitoring, evaluation, and State Data
Manager are vacant which needed to be filled this year.
To do Human Resource management functions like issuing ToR, to do the personnel review,
disbursing salaries and other emoluments are also very much critical in a scenario where more
than 300 people are working for the programme. In order to address this we are planning to
have a human resource manager to work under SPMU.
To recruit on all the vacant position under NRHM. The recruitment can be out source to any
state level or national level agency/civil society. We propose to identify an agency where clear
terms of reference will be signed with the agency/civil society. This further will be done in
collaboration with State Health Resource Centre or National Health System Resource Centre.
In addition, this process could be outsourced to whichever agency that takes up the task
NRHM PIP 2009-10: Chhattisgarh
Page 275
Table 3.51: Budget summary for HR recruitment process
Unit Description
Unit
Cost
Out sourcing recruitment under NRHM to state 250000
level or national level agency /civil society.
No. of
Unit
Duration
Total Cost
10
1 year
2500000
Total
2500000
Special initiative: Establishment of Snakebite Case Management Unit in district hospital
Snakebites are quite high in northern and southern Chhattisgarh. Every year, despite all the
preparatory measures as well as remedial interventions, many people die. To address this, we
plan to ensure timely and proper first aid to the affected, where we shall train a set of motivated
volunteers who shall initiate suitable first contact care for the patient. To pilot this, we have
taken Jashpur District and according to the success of this, the effort shall be scaled up to the
entire state. The budget allocation from the previous year’s PIP has been utilised and as
additional budget requirement for further equipping and scaling of this project for the current
year 2009-10 additional budget proposal is put forward for the current year. The requirement
involves the refilling of the anti venom vaccine as well as anti venom powder and that of
ventilators. Special addition to this project will be that of an Ambulance each in two CHCs,
Pharsabahar and Pathalgaon. This has been proposed in view of quick transport and referral of
the patients due to critical time factor involved in the case. The requisition for ambulance and
ventilator will be fulfilled through the mobile units, with ventilators attached, procured from
2008-09 allocation. The additional budget required will be for Anti venom, incentives for
Referral and training and IEC for snake bite etc.
Table 3.52: Budget Summary for Snakebite case management
Sl. no
Unit Description
Unit Cost
No. of Unit Duration
Total Cost
1
Referral
1000
1000
1
1000000
2
Anti venom
500
1000
1
500000
4
Training/IEC
100000
Total
NRHM PIP 2009-10: Chhattisgarh
100000
16,00,000
Page 276
Capacity Building and Mobilization of PRI for local Health Planning:
The inception of Swasthya Panchayat Yojana has been done by the department of Health and
Family welfare, Chhattisgarh with the assistance of SHRC, to place health on the Panchayat
agenda and to increase the participation of the Panchayats on the health issues. This
Programme has been running since 3 years.
In order to generate awareness about the objectives of Swasth Panchayat yojana, “Sarpanch
Sammellan” was organized in all districts in the first year of the program. Approximately 20,000
Sarpanchs, Panchs and Sachivs participated in it.
Current Status:
The main activities done under Swasthya Panchayat Yojana (SPY) are
Establishing strong linkages of Swasthya Panchayat Yojana with local bodies PRI (
Panchayati Raj Institutions) through VHSC
Formation of VHSCs and activation of VHSC by making it functional
ToT of MTs and DRPs have been completed on Village Health Plan (VHP). Training of
the members of VHSC on Village Health Plan ( VHP) is ongoing
Training of the Mitanins on Village Health Plan ( VHP ) is ongoing
The data on 32 indicators has been collected and fed into the computer database. Based on the
database, Human Development Indices of the Panchayat was computed and ranking the
Panchayats was done and 2 top scoring panchayats were awarded and last 2 were provided
financially supported. In the year 2007-08 and 2008-09, health related information was collected
at hamlet level based on 32 indicators. The reason behind to collect the information at hamlet
level was to do intensive health planning at the Panchayat level.
The main objective behind collecting these 32 indicators is the conceptualization & formulation
of a Village Health Plans. Training of state level team, DRPs and MTs have been completed in
all districts. The 11th round (Jurmil Banabo Swasthya Gaon) of training of these indicators have
been framed for the consideration of inter hamlet & inter Panchayat variations. It also ensures
the coordination among different departments like Education, ICDS, Health, Social welfare
Panchayat, Agriculture, Public Distribution System, and PHED Department at grass root level.
The training of Mitanins on VHP will be completed by Feb, ‘09 and the development of the
Village Health Plans (VHP) will be initiated after this. The fund allocated for Village Health
Planning (VHP) last year will be used for the current year.
NRHM PIP 2009-10: Chhattisgarh
Page 277
The budget allocation in the previous year PIP 2008-09 amounting to 98, 20,000 will be
utilized for the mentioned activities. Therefore, no additional budget is required for the
current year proposed activities. This will be carry forward activities.
Programme Management
Setting up a block PMU as per GOI guideline, which will strengthen HMIS at block level
through computerised data flow. The unit will ensure proper utilization of fund received from the
district. The BPMU will consist of a block programme manager and Account Assistant under
contractual basis. The education qualification of the block programme manager is Post
Graduate in any subject with two years of experience and the account assistant should be B.Com
with one-year experience. The unit will be stationed at the CHC and report to the BMO and
DPMU.
The proposed budget of Rs. 27010000 has been approved and sanctioned last year and an
additional amount of Rs. 134282400 is necessary for this year, thus Rs. 134282400 is budgeted
for the current year 2008-09 for further strengthening of the PMU. Additional HR at the PHC
level for accounts and data assistants are required for further strengthening and smooth
functioning of the Programme unit.
Table 3.53: Budget Summary for Programme Management
Sl
No.
Building and Strengthening Block Unit
PMU
Cost
No. of Unit
Duratio
n
1
Block Programme Managers
13800
146
12
24177600
2
Account cum Data Assistant
11500
146
12
20148000
4
Travelling @1000
1150
146
12
2014800
5
Contingency
2000
146
12
3504000
Total
Total cost
49844400
1
PHC level Accounts and data 6000
assistant
721
12
51912000
2
PHC Level Contingency
721
12
4326000
Total
NRHM PIP 2009-10: Chhattisgarh
500
106082400
Page 278
Chhattisgarh Health Equipment Management System
Introduction:
The CGHEMS is one of the innovative schemes in Chhattisgarh to rationalize the equipment
selection, purchasing, distribution, installation, repairing and maintenances in all type of public
health facilities. There are evidences in the state that a number of facilities are functioning
without basic equipment, while others having excess equipment lying idle. The main constrains
in the equipment management is that most of the time the staff are unaware about the existence
of the equipment in the facility, lack of technical personnel to repair the equipment, improper
stock recording and lack of user training. In addition, there is a need for relocation of excess
equipment purchased and need for quicker disposal for beyond economic repairable equipment.
To overcome this problem and to make the system more ideal, Chhattisgarh Health Equipment
Management System was established to ensure that every institution will have functional
equipment with proper repairing and maintenance mechanism in place. All other activity
undertaken by CGHEMS and its administrative costs are borne by EUSPP except, the training
part has been proposed under NRHM.
Activity:
Following training activity for users are proposed under many tasks of CGHEMS to be funded
by NRHM.
Training:
Two categories of Staff targeted are staff nurses and ANM. 71 staff nurses and technical
demonstrators are considered TOT for the programme. The venue will be the district level
hospital. Along with the Staff Nurses, all CMOs/CS are expected to be sensitized on equipment
management. The duration for this training will be three days and it will be a residential
training. For ANM it will be one day training.
As per the need assessment, training will be provided on equipment management for the
following equipments:
NRHM PIP 2009-10: Chhattisgarh
Page 279
1. Baby warmer
2. Suction pump
3. O.T. Lights
4. Emergency light
5. Foetal Heart monitor
6. Baby Incubators etc.
Budget estimation:
The expected load for this training is 5671, in that 4645 ANM, 1026 Nurses.
The estimated budget for above activity is Rs. 28, 99,400/.The cost of training will be as follows:
Rs 900/ per person for 71 nurses for TOT and, at the rate of Rs 500/ for 5,671 (ANM and
Nurses).
Table 3.54: Budget summary for Training of paramedical staff under CGHEMS
Sl. No.
Personnel to be No. of Units
trained
Unit cost
Total Cost
1
TOT for Nurses
71
900
63900
2
ANMs
4645
500
2322500
3
Nurses
1026
500
513000
Total
NRHM PIP 2009-10: Chhattisgarh
28,99,400
Page 280
PART C – PIP ON IMMUNIZATION
In last two year, the immunization status has increased significantly. The state has taken special
initiative to increase the immunization coverage for under five children that is Sishu Sanraksaan
Maah. In this, all under six left out children were immunized bi annually. The immunization
status in state reported by different survey is as follows.
Reported and evaluation coverage:
Table 4.1: Comparison of Reported and Evaluated Coverage 1998/9-2007/8 (%)
Antigen
NFHS Reported
II
Coverage
2004-05
1999
Reported
Coverage
2005 – 06
CES
2005
Fully
vaccinated
21.8
91.42
96.93
44.4
BCG
74.3
100.41
101.57
DPT-3
40.9
95.12
98.65
3 Doses
Polio
NFHS
III
CES
2006
DLHS -3
(2007-8)
48.7
57.8
59.3 (12-23
Months)
89.2
84.6
96.1
94.8 (12-23
Months)
65.5
62.8
65.2
71.4
2006
69.7
of
91.42
96.93
72.0
62.5
78.1
79.9
Drop-out BCG 46.16
– Measles rate
8.95
4.57
19.3
25.8
18.7
---
TT 2 + booster
93.52
95.78
76.3
90.8
---
Measles
40
58.2
Table 4.2: Vaccine preventable diseases
Disease
2004-05
Cases
NRHM PIP 2009-10: Chhattisgarh
2005-06
Deaths
Cases
2006-07
Deaths
Cases
Deaths
Page 281
Measles
Nil
Nil
113
Nil
128
Nil
Diphtheria
Nil
Nil
Nil
Nil
Nil
Nil
Pertussis
Nil
Nil
Nil
Nil
Nil
Nil
Neonatal Tetanus
Nil
Nil
1
1
Nil
Nil
Polio
Nil
Nil
Nil
Nil
Nil
Nil
Source: Reported and investigated information.
Outbreaks reported and outbreaks investigated in the last year
There was no outbreak reported last year.
Table 4.3: Cold Chain Storage Points
Cold Storage Point
Total Number
Proposed Expansion
State Store
1
One storage Point
District Store
16
ILR Storage Point
16
25
Assessment of critical bottlenecks for full coverage
Accessibility: Due to geographical terrain of the state of Chhattisgarh there are many under
served and unreachable areas. In fact, it is computed that 40 % sessions are organized in hard to
reach in rural areas. The micro plans would require more enhancements so as to ensure that no
session is cancelled.
Utilization / Adequate Coverage:
Low awareness of vaccination schedule is one of the major causes of low attendance in
immunization session.
Objective:
The objective of programme based on review of past performance, assessment of critical
bottlenecks, and planned activities to increase the immunization coverage.
NRHM PIP 2009-10: Chhattisgarh
Page 282
Action Plan and Budget for 2009-10:
Table 4.4: Budget Summary and Action Plan for Immunisation services
Service Delivery: -
Norms*
Expenditure &
Achievement
Remarks
2009-10
2005-06
Expenditure
Mobility support for
supervision
Supervisory visits by state
and district level officers for
monitoring and supervision
of RI
Focus on slum &
underserved areas in urban
areas:
Mobilization of children
through ASHA/mobilizers
* Description
Funds
requirement
Target
@Rs.50,000 per District for
district level officers (this
includes POL and
maintenance) per year
=16 *Rs 50000/-
800000
No of sessions
Supervised
By state level officers @
Rs.100,000 /year
=1*Rs100,000/-
100000
No of districts visited
for RI review
Hiring an ANM
@Rs.300/session for four
sessions/month/slum of
10000 population and
Rs.200/- per month as
contingency per slum of i.e.
total expense of Rs. 1400/per month per slum of the
immunizations will be held
at the Anganwadi centre.
Hiring of ANM for
immunization =1368
AWC X12X300
=Rs4924800
5745600
No of sessions with
hired vaccinators
@ Rs 150/session (for all
states/UT.s)
Rs 150* 12 month*4
session* SHC(4741)
34135200
No. of sessions with
ASHA
Alternative Vaccine
Delivery:
NRHM PIP 2009-10: Chhattisgarh
0
Contingencies=
Rs.50X1368X12 =
Rs.820800
No of sessions with
AVD
Page 283
revised
NE States, Hilly terrains
and geographically hard to
reach areas e.g. Session
site>30 kms from vaccine
delivery point, river
crossing etc.
@ Rs.100 per session
Rs. 150 * 1500
225000
For RI session in other
areas
@ Rs.50 per session.
=4692 SHC *4* 12*
Rs 50/-
11260800
Support for Computer
Assistant for RI reporting
(with annual increment of
10%)
State @Rs 12,000- 15,000
p.m.
=Rs 12000 * 12
144000
Districts @ Rs 8000- 10,000
per month
=Rs 8000*12*16
1536000
Printing and dissemination
of immunization cards, tally
sheets, monitoring forms,
etc.
@ Rs 5 per beneficiary
=950000 no*Rs 5/-
4750000
Review Meetings
No of C.A. in position
No of meetings held
Support for Quarterly State
level Review Meetings of
district officers
@ Rs 1250/participant/ day
for 3 persons
(CMO/DIO/Dist Cold Chain
Officer)
=Rs 1250/-* 3*4*16
240000
Quarterly Review &
feedback meeting for
exclusive for RI at district
level with one Block MO.s,
ICDS CDPO and other
stakeholders
@ Rs 100/- per participant
for meeting expenses (lunch,
organizational expenses)
= Rs 100/*[146{4(BMO +
CDPO + others)} +
4{1(CMHO + DPO
+ others)}]
259200
NRHM PIP 2009-10: Chhattisgarh
Page 284
Quarterly review meeting
exclusive for RI at Block
level
@Rs 50/-pp as honorarium
for ASHAs (travel) and Rs 25
per person at the disposal of
MO-I/C for meeting
expenses(refreshments,
stationery and misc.
expenses)
=(59489* 4* Rs
50)+ (59489+146)*
Rs 25/- * 4
17860900
Trainings
No of persons trained
District level orientation
training for 2 days ANM,
Multi Purpose Health
Worker (Male), LHV,
Health Assistant (Male /
Female), Nurse Mid Wives,
BEEs & other specialist ( as
per RCH norms)
Three day training of
Medical Officers on RI
using revised MO training
module
As per revised RCH norms
for trainings, copy attached
= Rs 450/-* 2*
(4800ANM+
2514MPW(M) +
749LHV+146 BEE)
7388100
Resource Person
=274batch* 2day*
Rs 600/-
328800
Venue Hiring Charges
=274batch* 2day*
Rs 8000/-
4384000
As per revised RCH norms,
copy attached
=Rs 450/- *
*3*(1382)
1865700
Resource Person
=41 batch* 3day* Rs
1000/-
123000
NRHM PIP 2009-10: Chhattisgarh
No of persons trained
Page 285
One day refresher training
of District RI Computer
Assistants on RIMS/HMIS
and Immunization formats
under NRHM
One day Cold Chain
handlers training for block
level cold chain handlers by
State and District Cold
Chain Officers and DIO for
a batch of 15-20 trainees
and three trainers
Venue Hiring Charges
=41batch* 3day* Rs
8000/-
984000
As per revised RCH norms ,
copy attached
=Rs 450* 16
7200
Resource Person
= 1 batch * 1 day*
Rs1000/-
1000
Venue Hiring Charges
=1batch* 1day* Rs
10000/-
10000
As per revised RCH norms,
copy attached
=Rs 450/* (146
Block)
65700
Resource Person
= 8 batch * 1 day*
Rs 1000/-
8000
Venue Hiring Charges
=8batch* 1day* Rs
8000/-
64000
NRHM PIP 2009-10: Chhattisgarh
No of persons trained
Page 286
One day Training of block
level data handlers by DIO
and District Cold chain
Officer to train about the
reporting formats of
Immunization and NRHM
As per revised RCH norms,
copy attached
Rs 450/- * 146 blocks
65700
Resource Person
= 8 batch * 1 day*
Rs 1000/-
8000
Venue Hiring Charges
=8batch* 1day* Rs
10000/-
80000
To develop sub-centre and
PHC microplans using
bottom up planning with
participation of ANM,
ASHA, AWW
@ Rs 100/- per sub centre
(meeting at block level,
logistic)
4692* Rs100/-
469200
For consolidation of
microplan at PHC/CHC
level @ Rs 1000/- block &
at district level @ Rs 2000/per district
(146* 1000) +
(16*2000)
178000
POL for vaccine delivery
from State to District and
from district to PHC/CHCs
Rs100,000/ district/year
16*100000
1600000
Consumables for computer
including provision for
internet access for RIMS
@ 400/ - month/ district
(Rs 400/- * 12* 16
districts) + (Rs 400/* 12 * 1 state level)
81600
No of persons trained
Microplanning
Injection Safety
NRHM PIP 2009-10: Chhattisgarh
100% of
SC/PHC/CHC/Districts
have updated
microplans every year
% Funds used
% Funds used
Page 287
Red/Black Plastic bags etc
@ Rs 2/bags/session
Rs 2/- * 2 bags per
session*4 sessions*
12* 4692 SHC
900864
Bleach/Hypochlorite
solution
@ Rs 500 per PHC/CHC per
year
Rs 500 /-* (723 +
136)
429500
Twin bucket
@ Rs 400 per PHC/CHC per
year
=Rs 400/- *
(723+136)
343600
Temperature record books
Rs. 40 per cold chain
equipment per year
Rs. 40 * 1500
60000
Charts on storage of
vaccines in ILR
Rs. 12 * 700 per ILR
Rs.12 * 700
8400
Chart on ice packs
preparation in DFs
Rs. 12 * 700 per DF
Rs.12 * 700
8400
Chart on hub cutters
Rs. 12 * (723 CHCs + 136
PHCs + 4692 SCs)
Rs. 12 * 5551
66612
Chart on injection safety
Rs. 12 * (723 CHCs + 136
PHCs + 4692 SCs)
Rs. 12 * 5551
66612
Any State Specific Need
with justification
% Funds used
9,66,52,688
* These revised norms are under consideration of Empowered Programme Committee and will be sanctioned after approval of same; otherwise old norms will apply
NRHM PIP 2009-10: Chhattisgarh
Page 288
PART D: NATIONAL DISEASE CONTROL PROGRAMMES
Revised National Tuberculosis Programme
Situation analysis & epidemiological parameters for Chhattisgarh
Population 2,36,45,997
Percentage of tribal population 34%
No. of TUs (For every 5 Lakh Population) 61,
No. of DMCs ( For every 1 Lakh Population) 287,
No. of DOT Centres 5836,
No. of Medical Colleges 3,
NRHM PIP 2009-10: Chhattisgarh
Page 289
Year
Population
in lakhs
OPD
No.
of
Suspected
examined
Suspected
Referred /
Lakh
%
suspected
of
Total
OPD
No. of S+
pt.
Diagnosed
Total
pt.
registered
for T/t
Total
ACDR
ACDRNS+
cases
ACDR
NS+
Table 5.1: Burden of Tuberculosis in Chhattisgarh
2005
222
4135826
90361
407
2.18%
12140
23530
106
9704
44
2006
228.59
4301322
109282
480
2.54%
13273
28209
123
10737
47
2007
232.56
4702938
110679
476
2.35%
13002
27504
118
10598
46
Year
NSN Cases
initiate on
treatment
New
EP
cases
initiated on
treatment
Total
SP
ReT
on
CAT-II
No.
of
Paediatric
cases out of
new case
>90%
3
Month
conv. Rate
of
NSP
Patients
>85%
Success
rate of NSP
Patients
Table 5.2: Progressive report on no. of TB case treatment
2005
9202
2208
1631
916
86.00%
83.00%
2006
11620
2887
1847
1309
89.00%
83.00%
2007
11074
2981
1685
1316
89.00%
85.00%
NRHM PIP 2009-10: Chhattisgarh
Page 290
Activities in RNTCP
1. Referral of all Suspects from OPD and field to Primary Health Centre or
Community Health Centre and District Hospital
2.
Microscopic Examination of Sputum.
3.
Categorization of Patients for treatment.
4.
Treatment by DOTS Methods.
5.
Regular follow-up using sputum examination for to note the progress of the
disease
6.
Counselling of DOTS Provider.
7.
IEC Activities using Banner, Poster, Wall Panting, TV: Along with strengthening
supply and diagnosis side, it is very important to create awareness among
community for early detection and compliance to treatment.
8.
Regular training of Medical & Paramedical Staff.
9.
Sensitization of PRI and others.
10. Involvement of all Health Providers- Public Private Partnership
Monitoring & Evaluation
1) Regular Field visits.
2) Record & Reports Checking
3) Contact with patients, Family members
4) Regular Quarterly Meetings at State level, Districts level and Sub-divisional level
Table 5.3: Budget summary for RNTCP
Sr.
No.
Category of Expenditure
Budget estimate for FY 2009 - 2010
1
Civil works
30,68,400
2
Laboratory materials
48,37,702
3
Honorarium
24,34,150
NRHM PIP 2009-10: Chhattisgarh
Page 291
4
IEC/ Publicity
28,10,975
5
Equipment maintenance
14,94,000
6
Training
52,51,864
7
Vehicle maintenance
35,50,000
8
Vehicle hiring
50,59,800
9
NGO/PP support
51,88,100
10
Miscellaneous
40,80,102
11
Contractual services
3,13,63,272
12
Printing
33,29,502
13
Research and studies
-
14
Medical Colleges
18,50,100
15
Procurement –vehicles
2,50,000
16
Procurement – equipment
1,90,000
17
a.
7,47,57,967
18
b. Total ( Tribal annual action plan- copy enclosed)
75,82,040
19
Grand Total (a & b)
8,23,40,007
Total (General annual action plan)
National Vector Borne Disease Control Programme
Situational analysis with epidemiological parameters:
Malaria is the number one public problem in Chhattisgarh. In 2007 (upto 31st December) the
ABER was 14.04, API 5.95, SPR 4.23 and Pf% 73.5.
NRHM PIP 2009-10: Chhattisgarh
Page 292
Epidemiological Situation of Chhattisgarh
State of the Year 2005, 2006 and 2007
2005
2006
2007
District
District
District
0 to 2
Bilaspur, Janjgir, Raipur, Mahasamund, Dhamtari, Durg
Janjgir, Raipur, Mahasamund,
Dhamtari, Durg
Bilaspur, Janjgir, Raipur, Mahasamund,
Dhamtari, Durg, Rajnandgaon
2 to 5
Rajnandgaon, Kawardha
Bilaspur, Rajnandgaon,
Kawardha
Kawardha
API
5 to 10
Korba, Raigarh
Korba, Ambikapur, Raigarh
Ambikapur, Raigarh
10 to 20
Ambikapur, Korea
Korea, Jashpur
Korba, Korea, Jashpur, Kanker
20 & above
Jashpur, Jagdalpur, Dantewada, Kanker
Jagdalpur, Dantewada, Kanker
Jagdalpur, Dantewada
NRHM PIP 2009-10: Chhattisgarh
3
Page 293
Epidemiological Situation of Malaria in Chhattisgarh State
20.00
18.00
16.00
14.00
12.00
10.00
8.00
6.00
4.00
2.00
0.00
2000
2001
2002
2003
2004
2005
2006
2007
ABER
18.97
17.79
16.22
15.74
15.16
16.51
15.38
14.04
API
16.75
12.89
10.64
8.28
7.87
8.01
7.53
5.95
SPR
8.83
7.25
6.56
5.26
5.19
4.85
4.90
4.23
SFR
6.23
5.03
4.73
3.90
3.99
3.62
3.80
3.11
Burden of vector-borne diseases:
Due to varied ecological conditions and geography, the problem of diseases like malaria has
been showing a distinctive pattern and bulk of the burden is borne by the tribal forested area in
the north and the south. Malaria has been the major health problem in the state. In 2006,
Chhattisgarh contributed 7% of the total malaria cases and 11% P. falciparum cases reported in
the country (NVBDCP, 2007). As per the available data on malaria upto the November 2008, the
central part of the state, represented by 8 districts (61.09% of the state’s population) report low
to moderate incidence of malaria (8.16%) and P. falciparum (4.58%), rest of the malaria burden
is collectively contributed by the 5 districts in the north and 3 districts in the south. The problem
is further compounded by the reports of chloroquine resistance in P. falciparum from Surguja,
Kanker and Bastar districts. There are 93 PHCs in the state with a population of 83 Lakhs that
have API of 2 and above and are declared as High Risk. Major Vector Control strategy includes
indoor residual spraying with DDT in 13 Districts and that with Synthetic Pyrethroid in 3
Districts viz. Jagadalpur, Dantewada and Kanker.
Activities
1. Up-gradation of peripheral health facilities and small hospitals in the diagnosis and
treatment of severe malaria
2. Use of second line Sulpha-Pyrimethamine / artesunate combination therapy in the drug
resistant areas.
NRHM PIP 2009-10: Chhattisgarh
Page 294
3. Facility assessment at secondary & tertiary care centre.
4. Establishment of FTDs/DDCs wherever needed.
5. Ensuring availability of qualified staff equipment/material at different levels
6. Establishment of district vector borne disease control society.
7. Establishment of technical resource group on malaria management in the medical
college.
8. Meeting of district level officers to plan about MDA & other activities related with ELF.
Proposed Interventions in Relation to the Objectives and Strategies
Integrated Vector Control Management
A. Indoor Residual spray: Mapping of insecticide resistance based on available data is
regularly done and regarding the susceptibility status of vector mosquitoes to different
insecticides can be classified as under.
Table 5.4: Distribution of Insecticide use
Insecticide used
Name of the districts
DDT 50 % WDP
Surguja, Koriya, Jashpur, Bilaspur, Korba, Raigarh, Janjgir,
Mahasamund, Kawardha, Rajnandgaon, Dhamtari, Durg, Raipur
Synthetic Pyrethroid
Bastar, Kanker and Dantewada
The population projected for IRS and the requirement of insecticides are shown in the following
table.
Table 5.5: Insecticides requirement
Year
Eligible population in lakhs
DDT
50%
WDP
Quantity of insecticide Received for the year
required in M.T
2009-10
Synthetic
DDT
Pyrethroid
in 50%
terms of 2.5% WP WDP
NRHM PIP 2009-10: Chhattisgarh
Synthetic
DDT
Pyrethroid
in 50%
terms of 2.5% WP WDP
Synthetic
Pyrethroid
in
terms of 2.5%
WP
Page 295
2009-10
66 lakh
30 lakh
993
110
890
0
Currently Synthetic Pyrethroid (Alphacypermethrin 5% WP) is being used in 3 districts as
mentioned above.
Spray staff: The staff engaged for indoor residual spray will be paid only daily wages.
The spray operation will be commence from 16th June to 31 August of the year (Ist Round) and
2nd Round from 1st September to 15th November of same year as per the schedule.
BCC for creating awareness among the households for maximum acceptance will be carried out
using village level IEC as well as gram sabhas.
Monitoring and evaluation will be carried out by mapping of vector density and bio efficacy of
insecticide towards vector for monitoring the impact of IRS in the PHCs in endemic areas
covered under IRS wherever feasible with the help of NIMR. The checklist developed for the
supervision will be used for timely corrective measures during the spray operation.
B. Distribution and promotion of use of Insecticide Treated bed nets
Stratification of the area and use of ITN will be as under.
Table 5.6: Classification of eligible beneficiaries for ITN as per API
High risk >3 API
Middle risk 2-3 API
Low risk < 2 API
Highest risk villages as per Beneficiaries: Pregnant women Pregnant
available resources for the and infants
infants
ITNs
women
and
C. Biological Control (Use of Larvivorous fish):
Use of larvae eating fishes for control of mosquito breeding will be promoted on a much larger
scale. This will involve establishment and maintenance of hatcheries, at the district, block and
PHC levels.
Training to the staff involved will also be imparted and the required equipments for fish
transportation. Provision of storage tanks at PHC level has also been proposed under the
project.
The community, NGOs, schoolchildren will be actively involved in this activity.
NRHM PIP 2009-10: Chhattisgarh
Page 296
In addition to the facilities established in the state for the promotion of this activity it is proposed
to utilize all the natural water bodies as hatcheries in all the districts and blocks of the state.
Existing hatcheries will be maintained for ensuring the availability of fishes. It is also proposed
to provide necessary equipment in all districts for the transport of fish.
D. Advocacy to promote community awareness: Participation of community in various activities
under the programme is of utmost importance. Community participation in activities like use of
insecticide treated mosquito nets and use of biological control using larvivorous fishes for the
control of mosquito breeding will be enhanced by advocacy at the local level. NGOs will be
roped in to improve the acceptance of these methods of vector control by the community.
Awareness promotion on other aspects such as EDCT, pregnancy and malaria will also be
intensified under the project.
E. Information Education and communication: To promote awareness in the community the
IEC activities initiated under the EMCP will be sustained further. The IEC strategy will include
other vector borne diseases also. To have an integrated awareness campaign particularly to
disseminate messages through all possible media which are effective?
F. Training of medical and Para medical personnel: Different categories of staff working at
different levels will be trained. Integrated training programmes covering vector borne diseases
will be organized. Refresher training will be organized for all categories of staff every three
years.
The training load in the state for the year 2009-10 is as under.
Table 5.7: Training load for Vector borne disease control programme
Sr.
No.
Training course
1
Orientation Course for Medical Officer 16
PHCs.
5
122
2
Orientation Course in Spray Technique.
16
1716
3
Orientation
Course
for
Inspectors / Sector Supervisors.
17
846
4
Course in Malaria Microscopy for Lab 20
Technician. Induction Level
20
269
NRHM PIP 2009-10: Chhattisgarh
No.
of No.
of No.
of
Courses
Courses
Participants to
sanctioned
Projected
be trained
16
Malaria 0
Page 297
5
Clinical Management
1
4
100
6
Malariology
1
1
25
7
Chloroquine
Training
5
110
2000
Course
60000
8
Resistance
Assessment 12
Training of MPWs/ASHAs
The state is utilizing the facilities available with various training institutions in the state for
imparting training to various categories of staff. The institutions, which have already been
identified and will be effectively utilized for this purpose, are as under:
Table 5.8: List of state institutions imparting training on vector borne disease control programme
S.No.
Name of training institution
Categories of staff being trained
1
PSM
Departments
of Clinical management training for specialists.
Government Medical Colleges
(1)
2
State Institute of Health and Training in Malariology for Medical Officers and
Family Welfare (1)
MPHS
3
Regional Training Centre (1)
4
Regional Office for Health & Basic and reorientation training for Laboratory
Family Welfare, GoI, Raipur
Technicians.
5
NIMR Raipur Unit
Training for MPHWs and FHWs.
Reorientation training for Laboratory Technicians
and training for entomological staff.
G. Intersectoral collaboration/public- private partnership
Under NVBDCP, also it is proposed to have fruitful partnerships with field level NGOs to
implement various activities for better service delivery and acceptance of the community.
Linkages also will be established with various industries, project authorities, mines, forest,
railways and other sectors to have better prevention and control of VBD prevention and control
services to high-risk population. A state level Task Force has been established under the
leadership of Health Secretary to have intersectoral collaboration.
NRHM PIP 2009-10: Chhattisgarh
Page 298
H. Management Information System: It is proposed to make the MIS fully functional through
the web-based software. Deficiencies as regards manpower, hardware and connectivity will be
rectified.
I. Operational Research. It is proposed to undertake operational research in all key areas by
involving NIMR Field Unit, Raipur and the newly formed Regional Office for Health & FW, GoI
and the Medical Colleges of the state.
The proposed operational research activities under the project are as under.
1. Proposed studies on vector bionomics and transmission dynamics by NIMR Raipur Unit.
2. Monitoring of drug resistance in P. falciparum by NIMR Raipur Unit, ROH&FW and
Medical Colleges.
3. Mapping of vector resistance to insecticides to be jointly carried out by NIMR Raipur
Unit and Directorate of Health Services
Monitoring and evaluation
The important aspects for monitoring and evaluation under the project are proposed as under.
1) Mapping of resistance in vector mosquitoes to insecticides as well as in malaria parasites
(P. falciparum) to the chloroquine.
2) Interaction with stake holders by organizing meetings and workshops
3) Frequent field visits
4) Sample surveys to validate information on monitoring indicators of major objectives.
5) Process and performance indicator for each activity will be monitored regularly.
6) Impact indicators will also be set and monitored.
7) Progress of activities will be monitored at quarterly intervals against the set benchmarks.
8) Roles and responsibilities of functionaries at different levels will be defined.
9) Close interaction with NVBDCP and all related institutions functioning in the state will
be ensured.
10) Utilization of funds and commodities will be monitored regularly through SOEs and stock
position reports.
NRHM PIP 2009-10: Chhattisgarh
Page 299
Filariasis:
Mass Drug Administration – 2007:
Table 5.9: population covered under mass drug administration in 2007
Sl. No.
Name of District
Population
Eligible
Population
Pop. Covered
%
1
Raipur
3569947
3061203
3052258
99.71
2
Durg
3283341
2000000
1919414
95.97
3
Dhamtari
866668
799110
711504
89.04
4
Mahasamund
1029708
896306
873221
97.42
5
Bilaspur
2403427
2268797
2068037
91.15
6
Janjgir
1501153
1313602
1244645
94.75
7
Jashpur
828524
748507
607981
81.23
8
Raigarh
1478784
1266186
1080344
85.32
9
Ambikapur
2375608
1191681
1064719
89.35
17337160
13545392
12622123
93.18
Total
Table 5.10: no. of hydrocoele and lymphoedema cases recorded in 2007
Sl. No
Name of District
Hydrocoele Cases
Lymphoedema Cases
1
Raipur
1471
685
2
Durg
1108
2788
3
Dhamtari
143
47
4
Mahasamund
777
416
5
Bilaspur
334
157
NRHM PIP 2009-10: Chhattisgarh
Page 300
6
Janjgir
43
461
7
Jashpur
333
124
8
Raigarh
2707
681
9
Ambikapur
640
195
7556
5554
Total
Table 5.11: Result of Microfilaria Survey carried out in 2007
Sl. No.
Name of District
Population
BSC
BSE
Positive for Mf
1
Bilaspur
2403427
10826
10826
59
2
Janjgir
1501153
3508
3508
62
3
Ambikapur
2375608
5411
5411
74
4
Raigarh
1478784
3758
3758
5
5
Jashpur
792670
2500
6
Raipur
3569947
33862
33862
9
7
Mahasamund
1029708
4889
4889
137
8
Dhamtari
866668
5008
5008
84
9
Durg
3283341
3827
3827
27
17301306
73971
67331
452
Total
Awaited
Proposed activities for Lymphatic Filariasis elimination:
MDA For LFE And Morbidity Management MDA will be taken up in all the nine endemic
districts annually for 5 years by ensuring 85% coverage to bring down MF rate less than 1%.
Assessment survey will be carried out after 5 years in children and if a single case is found
positive MDA will continue for 2 more years.
Morbidity management of Lymphoedema cases and hydrocoelectomy camps for disability
prevention and personal protection measures to prevent man mosquito contact will also be taken
up simultaneously.
NRHM PIP 2009-10: Chhattisgarh
Page 301
A. Planning and Preparatory Activities for Elf: during the preparatory stage, the following
activities have to be implemented from the state and district level.
1. Meeting of district level officers to plan about MDA and other activities related with
ELF.
2. Meeting of the District level coordination committee (three meetings prior to MDA).
3. Organizing press meet/media flash.
4. IEC activity by the MOPHCs and para medical staff.
5. Advocacy workshops.
B. Training and Capacity Building Of Different Tiers Of Health Personnel:-To sensitize about
MDA, morbidity management, and mapping of Lymphoedema cases.
The training programmes will be organized through the District Training teams.
C. Surveys to Estimate Filaria Endemicity: though mapping of a major portion of Filariasis
cases has been completed in 9 districts, this activity will be further enhanced to find out each and
every Filariasis case in other districts as well.
D. Drug Delivery Component for Dec, MDA: The MDA will be carried out through the PHC
staff with the support of various health functionaries, NGOs, and personnel from various state
departments. DEC will be procured and supplied by the Govt. of India.
Detailed activity plan for each PHC will be prepared for the MDA including the IEC activities
and the door-to-door campaign that is required for its success
E. Information Education And Communication Strategies: All the activities related with ELF
require a strong IEC support and therefore various IEC activities are planned to promote the
awareness. IEC materials for inter personal communication and display will be prepared and
distributed. Print and electronic media will also be used in a big way to disseminate the
messages.
Monitoring And Evaluation:
The evaluation of the drug compliance will be carried by the districts. The PSM Departments of
Medical colleges will also be involved for this activity. An amount of Rs. 2.35 lakhs is proposed
for this purpose
Budget Summary:
Table 5.12: Available budget support from World Bank for NVBDCP
NRHM PIP 2009-10: Chhattisgarh
Page 302
Directorate of National Vector Borne Disease Control Programme
Proforma for Action plan for World Bank Project's for year 2009-10 under Cash Assistance
Components
Detail of Requirement
Total
Requirement
during 2008-09
Consultant Entomology
12 000 per month
1,44,000
Investigator
6500 per month
78,000
2 Data Analyst
8000 per month
1,92,000
Computer Operator
6500 per month
78,000
Secretarial Assistant
6500 per month
78,000
1. Human resources
1.1 Salary for the State staff presently working
under Project (to be revised)
Total
5,70,000
1.2 Salary for the staff as per Annexure I Human Resource Component
1.2.1 State
State Coordinator + M&E
35,000
4,20,000
Consultant (Procurement & supply chain)
25,000
3,00,000
Consultant (Financial Management)
25,000
3,00,000
Consultant (Social mobilization/NGO/PPP)
25,000
3,00,000
Consultant (Training)
25,000
3,00,000
GIS data entry
6,500
78,000
Accountant
10,000
1,20,000
Secretarial Assistant (one per state)
6,500
78,000
Total
NRHM PIP 2009-10: Chhattisgarh
18,96,000
Page 303
1.2.2 District
Malaria consultant/VBD consultant district
30,000
3960000
Accountant per district
1,000
1,32,000
Secretarial Assistant (one each district)
6,500
8,58,000
Malaria Technical Supervisor (3 per district) @ 10,000
1per 2.5 lakh pop.
39,60,000
Lab Technicians (3 per district in endemic 10,000
areas)
39,60,000
Data Entry Operator (one per district)
8,58,000
6,500
13728000
Sub Total
2. Training
2.1 Medical Specialist at District Hospital
16 Batches @ 20000
3,20,000
2.2 Medical Officer
35 Batches @ 15000
5,25,000
2.3 Laboratory Technicians (Induction)
20 Batches @ 10000
2,00,000
2.4 Laboratory Technicians (Re-orientation)
20 Batches @ 10000
2,00,000
2.5 Health Supervisors (M)
10 Batches @ 10000
1,00,000
2.6 Health Supervisors (F)
16 Batches @ 10000
1,60,000
2.7 Health Worker (M)
115 Batches @ 10000
11,50,000
2.8 Health Worker (F)
100 Batches @ 10000
10,00,000
2.9 ASHA Training in 4 quarters
8000 Batches @ 3000
2,40,00,000
2.10 Community Volunteers other than ASHA
20 Batches @ 10000
2,00,000
2.11 Other Specify (Spray Squads) 400 Squads
8 Batches @ 10000
80,000
Sub Total
2,79,35,000
3. Planning & Administration
3.1 Office expenses for state level
NRHM PIP 2009-10: Chhattisgarh
50000 per month
6,00,000
Page 304
3.2 Office expenses for district level
20000 per month
38,40,000
3.3 Accounting and Auditing cost
3,00,000
3.4 Bank Charges
7,500
Sub Total
47,47,500
4. Monitoring & Evaluation
4.1 Hiring of vehicles for field visit and 100000 for state and 4,20,000
supervision
20000 for districts
4.2 Travel related
D.A.)/Honorarium
expenses
(T.A.
/ 200 TA per day for 1,92,000
DMO 200 per day for
VBD
Cont.
600 per day for 6 HS
per day (20 days)
4.3 Review meeting of States / District
50000 for state and 2,10,000
10000 for districts
4.4 Other cost associated with the Monitoring 20000 per district and 5,20,000
and Evaluation
200000 for state
Sub Total
13,42,000
5. IEC
5.1 Health Camps / Mela
State and District Level
26,00,000
5.2 IEC Awareness through NGOs / CBOs /
Panchayat
10,00,000
5.3 Other IEC activities (Electronic and Print
Media)
50,00,000
Sub Total
86,00,000
6. Operational expenses for treatment of bed nets
6.1 Supervision of bed net impregnation and 10000 Rs. Per District
distribution
1,60,000
6.2 Training material etc.
2,00,000
NRHM PIP 2009-10: Chhattisgarh
Page 305
6.3 Materials for treatment of nets (buckets,
plastic sheets, hand gloves, rope etc)
3,00,000
6.4 Activities through Health System
1,00,000
6.5 Activities through NGOs/CBOs/Panchayat
Raj and other private partners
3,00,000
Sub Total
10,60,000
7. Operational Research
7.1
Operational Research Activities in
collaboration of NIMR and ROH&FW &
Medical Colleges
10,00,000
Sub Total
10,00,000
8. Selective Vector Control
8.1
Spray wages, spray equipments,
transportation, dumping, supervision, impact
assessment, supervision of spray coverage &
quality
(Give details for each component)
Spray Wages
400 gangs @ 18000 3,60,00,000
per month for 5 months
Spare parts for spray pumps
30000 per district
4,80,000
Dumping & Transporting of Insecticides
50000 per district
8,00,000
Supervision
20000 per district
3,20,000
Impact Assessment
10000 per district
1,60,000
Sub Total
3,77,60,000
9. MIS
9.1 Recurring expenditure on internet facility 10000 for state and 10,80,000
& internet rent/maintenance etc.
5000 per district per
month
NRHM PIP 2009-10: Chhattisgarh
Page 306
Sub Total
10,80,000
10. EDPT
Blood Slide Collection
Lancet
1 crore Lancet @1.25 1,25,00,000
per Lancet
Microslide
1000000@
slide
Remuneration to Asha/ Mitanin @ 5/- per slide
5/- per slide
0.55
in case of Positive Rs. 20 per case to 20/- per case
Asha/Mitanin
MF 2 Forms/register and stationary
1500000
form
@0.30
per 5,50,000
5,00,000
8,00,000
per 4,50,000
Blood Slide Examination
Laboratory Articles
25,00,000
Registers and Forms/register and stationary
10,00,000
Sub Total
1,83,00,000
Up scaling of Larvivorous Fish
Maintenance of Hatchery
including
Transportation
forwarding of Fish
(Village level) 100
rupees
per 1,19,88,000
and
packing panchayat per month
for 9990 panchayat
Sub Total
1,19,88,000
GRAND TOTAL
12,99,46,500
NRHM PIP 2009-10: Chhattisgarh
Page 307
Table 5.13: Domestic budget support of NVBDCP
Component 1:(Filaria elimination programme)
S.
no.
Component
Details of requirement
1
Planning and preparatory meetings for ELF
1.1
State level meeting of District level
officers.
1.2
State level TAC meeting
1.3
Meeting of district level co-ordination
committee(DCC) and press meeting
followed by meeting of district officials,
NGO etc
Meeting of 9 district level co- 45000
ordination committee(DCC)
and press meeting followed
by meeting of district
officials, NGO etc
1.4
Second meeting of DCC and press meet
Second meeting of 9 DCC
and press meet
45000
1.5
Third meeting of DCC and press meet
Third meeting of 9 DCC and
press meet
45000
1.6
2 TAC meeting at District Level
One-day State level meeting
of District level officers.
Total
10000
10000
45000
200000
2
Training and Capacity Building for different tiers of Health Personnel
2.1
2 days Training for District Level
Officers
2 days Training for District
Level Officers
40000
2.2
1 batch in each district MO- PHC
1 batch in each district MOPHC
279000
2.3
1 batches in each district Para medical
staff
1 batches in each district
Para medical staff
800000
2.4
1 batches in each district Drug
Distributors
1 batches in each district
Drug Distributors
800000
1919000
NRHM PIP 2009-10: Chhattisgarh
Page 308
3
Mapping to estimate filaria endemicity
3.1
Operational cost for morbidity
management
Operational cost for
morbidity management
450000
3.2
Material for Night Blood Survey
Rs. 50000 per district
Material for Night Blood
Survey
450000
900000
4
Drug delivery component for DEC MDA
4.1
Contingency expenses for drug delivery
of DEC
15693965 population @ 20
paisa per head in 9 districts
4000000
4.4
Subsidy for transportation to cover POL
Exp.
9 Districts
720000
4720000
5
IEC
5.1
IEC activities in 9 endemic districts of
state
@ Rs. 1.5 Lakhs per district
1350000
5.2
Printing of IEC Material, enumeration
registers and reporting formats
@ Rs.1.00 Lakhs per
district*9
900000
5.3
Dissemination of messages through news
papers, TV and Radio etc
@ Rs.50000 Lakhs per
district *9
450000
2700000
6
Monitoring & Independent evaluation
6.1
Monitoring and assessment by the states
1 per district per year @
Rs.20,000/-
450000
6.2
Independent evaluation by the centre
1 per State for the year @
Rs.75,000/-
75000
525000
7
Hydrocoele Operation
NRHM PIP 2009-10: Chhattisgarh
Page 309
7.1
Camps for Hydrocoele operations
@ Rs.1.00 Lakhs per
district*9
900000
Sub TOTAL
1,18,64,000
Component 2 :( Payment of Salary to Contractual MPW)
Component
Details of component
Total
Payment of salary of 830 MPW(Male)contractual
Remuneration 6000 per month 5,97,60,000
Grand Total(component 1+component2)
7,16,24,000
Table 5.14: Budget summary for NVBDCP
Sl. No
Components
Total
1
Malaria(world bank assistance)
12,99,46,500
2
Filaria (Domestic Budget Support of NVBDCP)
1,18,64,000
3
Payment of salary of 830 MPW(Male)contractual
5,97,60,000
(Domestic Budget Support of NVBDCP)
20,15,70,500
Grand Total (Malaria+MPW+Filaria)
Leprosy Eradication
Situational Analysis with epidemiological Parameters
Table 5.15: Epidemiological situation of Leprosy India vs. Chhattisgarh
2007-08
Indicators
India
Chhattisgarh
PR/10,000
0.74 (87228)
2.34 (5465)
ANCDR/1,00,000
11.70 (137685)
33.4(7808)
35.1(8187)
as on June‘08
NRHM PIP 2009-10: Chhattisgarh
Page 310
MB%
47.2
49.9
Child %
9.4
6.6
Female %
34.5
33.1
Gr. I deformity %
5.4
3.6
Gr. II deformity%
2.5
3.5
Cure rate
90.2
92.3
Table 5.16: Epidemiological Trend of Leprosy from 2002-03 to November 2008
Indicators
02-03
03-04
04-05
05-06
06-07
07-08
Nov’08
2009-10
PR
7.20
6.01
3.60
2.00
1.46
2.39
2.42
2.0
ANCDR
85.9
71.6
59.0
40.0
26.3
36.4
35.61
40
PD Ratio
0.83
0.83
0.61
0.50
0.55
0.65
0.68
0.68
MB %
40.7
44.73
47.44
50.69
52.23
49.91
53.91
55.00
Child %
11.27
9.09
9.02
6.70
6.19
6.66
7.61
5.00
SC Rate
95.6
97.3
84.8
52.1
26.4
43.2
46.00
40
ST Rate
103.5
37.7
29.0
20.3
12.9
20.9
22.22
18.00
Female %
34.7
32.00
33.36
30.64
31.34
33.10
36.35
40.00
Gr
II
Disability
Rate
2.65
2.07
2.49
2.32
2.82
3.51
3.84
2.00
29% increase in new case detection from 6047 in 2006-07 to 7808 in 2007-08
10 districts with ANCDR > 20 per lakh , of these 3 districts with > 50 viz. Mahasamund
(94.5), Raigarh (61.9) and Raipur (52.6)
6 districts reporting >500 new cases – Raipur (1777), Mahasamund (912), Raigarh
(879), Durg (859), Bilaspur (818) & Korba (559)
NRHM PIP 2009-10: Chhattisgarh
Page 311
Out of 147 blocks, 73 blocks (50%) with ANCDR > 20 in 11 districts and 21 blocks with
ANCDR > 50 in 5 districts. State ‘s ANCDR is 35.4 which 3 times higher than country’
ANCDR which is 12
19 blocks reporting >100 new cases, mostly in Korba(3), Mahasamund (4), Raigarh (3)
and Raipur (7)
4 urban areas (out of 9) has ANCDR >50 per lakh.
There are 18 districts in the state with operational health care reporting system in 16. Out of 16
reporting districts only 4 (Surguja, Kanker, Koriya & Dantewada) have achieved the primary
goal of Elimination as a public health problem i.e. Prevalence Rate of <1 per 10,000 population,
while 6 districts are high endemic with Prevalence rate of more than 2.5 /10,000 namely
Mahasamund (), Raipur (), Raigarh (), Bilaspur (), Janjgir (), & Korba () as on October 2008.
Mahasamund and Raigarh are the two districts with highest new case detection rate higher than
state’s average ANCDR of 35.4 per 100000 populations.
Prevalence
64% increase in registered cases from 3332 in 2006-07 to 5465 in 2007-08
Grade II disability among new cases
Increased from 169 (2.8%) in 2006-07 to 274 (3.5%) in 2007-08
Raipur reported highest cases (82) and Durg (48)
About 3500 cases listed since 2000-01. Present status to be ascertained & RCS to be
conducted
Grade I disability among new cases
281 (3.6%) cases reported in 2007-08 indicating low level of reporting
Reconstructive Surgery
1 Govt. & 2 NGOs conducting RCS operations
128 RCS were conducted by the state
NRHM PIP 2009-10: Chhattisgarh
Page 312
Table 5.17: Grade II deformity load since 2001
Time Period
Case Load
2001 – 2007
2767
2007 – 2008
274
Till Nov. 08
204
Total
3224
Table 5.18: Reconstructive Surgeries performed from 2001 to 2008
Institutions
2001 -2007
2007 -2008
2008 -09
RLTRI, Raipur
404
109
77
TLM, Champa
100
19
32
TLM, Baitalpur
153
19
32
Total
657
128
109
Grand Total
894 (27. 72 %)
Analysis of BLAC (BLOCK LEPROSY AWARENESS CAMPAIGN) since 2004
Four BLAC Were Conducted In The State
63 Blocks Were Identified With PR > 5 Per 10,000 In 2004
12 Blocks Taken For Analysis
None Of The Blocks Achieved Elimination Level Till March’08
As Per Block Information , Out Of 44 Blocks Taken For BLAC IV , More Than 51 %
Villages Are Endemic Where New Cases Have Been Detected During Any time Since Last
Three Years Considering Lower Range Of Incubation Period To Be 3 Years.
Table 5.19: Progress of Block leprosy awareness campaign
NRHM PIP 2009-10: Chhattisgarh
Page 313
No. of blocks covered under BLAC taken Blocks achieved elimination on
for analysis
March’08
India
I
II
III
IV
All Four
No.
%
158
73
35
29
18
64
40.5
9
8
4
3
0
0
Chhattisgarh 12
Table 5.20: New Cases Detected in a campaign mode- BLAC – IV Sept TO Jan.08
S.No
District
No. of Blocks Endemic villages/ Total Total no. of new cases
Covered
villages
detected
(% of endemicity)
1
Bastar
3/14
141/308
(45 %)
23
2
Bilaspur
9/10
736/1492
(49 %)
62
3
Durg
2/12
135/263
(51 %)
47
4
Janjgir
1/9
41/72
(57 %)
22
5
Jashpur
1/9
41/110
(37 %)
34
6
Kawardha
¼
74/181
(41 %)
19
7
Korba
2/5
122/296
(41 %)
122
8
Mahasamund
5/5
622/1088
(57 %)
247
9
Raigarh
6/9
554/947
(59 %)
200
10
Raipur
13/15
921/2319
(40 %)
172
11
Total
43/146
3387/6636
948
(29.45%)
(51 %)
(12 %) of total NCD in
year 2007-08
NRHM PIP 2009-10: Chhattisgarh
Page 314
Constraints:
Non-existence of district nucleus (one district leprosy officer=full/part time, 1 medical
officer, two para medical staff) in the state set up which is severely hampering the
implementation of the programme thereby effective supervision & monitoring. .
Activities:
Repeated training & orientation of all level of health functionaries.
Training of Mitanin & group meeting at village level.
Scrolled display panels at district & medical college hospitals.
Revolving display panels at selected square of main roads.
Display hoarding, tin posters
IEC through School health education.
Group meeting- mahila mandal & SHG foe IEC activity
Counselling to patients, family member & community members
IPC among community members & through cured leprosy patients.
NGO meeting & workshop, IMA workshop.
Sensitization meeting of PRIs, opinion leaders & influential persons.
Regular urban leprosy situation review.
Table 5.21: Financial Status of Fund utilisation
Allotted Budget for 2007-08
Rs 99.90 lac (funds received Rs 46.88 L+ Pre
balance Rs 31.59 L= 78.47 Lac)
Budget utilized during the year 2007-08
Rs 75.15 Lac
Percentage of utilization
97 %
Status of audit for 2007-08
Already Submitted
Approved budget for 2008-09
RS 168.11 Lac
Funds in hands as on 01.12.08
Rs 40 Lac
NRHM PIP 2009-10: Chhattisgarh
Page 315
Requirement of second instalment, if any
Rs 84.11 Lac
Monitoring and evaluation
Monitoring & Supervision Through Regular Field Visits By State & District Level
Officers
Quarterly Review Meetings
State & District NLEP Co-Ordination Meetings
Budget Summary for Leprosy programme
Table 5.22: Contractual Services for Leprosy Programme
Sl.
No.
Item
No. Consolidated salary per Cost for the
month
year
1
SLS: Surveillance Medical Officer
1
20
240
2
Budget & Finance
Administrative Officer
cum 1
15
180
3
Administrative Assistant
1
7
84
4
Data Entry Operator
1
8
96
5
Drivers
1
4.5
54
Sub Total
5
-
654
DLS: Drivers
8
4.5
432
Total
13
1
Officer
1086
Table 5.23: Services through Mitanin (ASHA) (‘000)
Sl.
No.
Item
1
Performance
incentive to Mitanin
based MB
1200
PB 1300
Rs. 500/- each Rs. 600
300/- each
390
2
Sensitization
ASHA 20000
Rs. 50/- each
Unit
of
NRHM PIP 2009-10: Chhattisgarh
Rate per unit
Cost for the
year
1000
Page 316
(Mitanin)
Total
1990
Table 5.24: Drugs, Material & Supplies. (‘000)
Sl.
No.
Item
District Cost per
District.
Cost for the year
1
Supportive Drugs
18
25
450
2
Laboratory reagents & Equipments
18
12
216
3
Printing of forms etc.
18
15
270
Total
936
Table 5.25: Vehicle Hiring and POL/Maintenance
Sl.
No.
Office
No.
unit
1
State Leprosy Office
1
2
85
170
2
District Leprosy Office
18
18
75
1350
19
20
Total
of No.
Vehicle
of Rate per year/ Cost for the year
per vehicle
1520
Table 5.26: IEC (‘000)
Sl. No.
Medium
1
Mass Media
2
Outdoor Media
1450
3
Rural Media
2000
4
Advocacy meetings
1000
Total
NRHM PIP 2009-10: Chhattisgarh
Cost for the year
(TV Radio Press)
550
5000
Page 317
Table 5.27: Training & Capacity Building (‘000)
S
No.
Category & Type of Training
1
Technical & IEC training for MO (Rural) 700
– 04 days
23
29.8
685
2
Technical & IEC training for MO 200
(Urban) – 04 days
7
29.8
209
3
Re-orientation training
Officer - 02 days
55
17.3
952
4
Technical & IEC training for Health 700
Supervisor (M&F) – 03 days
23
16.3
375
5
Technical & IEC training for Health 2200
Worker (M&F) – 03 days
73
14.05
1026
6
Laboratory technicians training – 05 146
days
5
24.1
121
of
Total
Unit
Medical 1650
No.
Batches
of Unit
Cost
5596
Cost for the
year
3368
Table5.28: Disability Prevention & Medical Rehabilitation
S. No.
Item
Norm & rate
1
MCR footwear
120 pair/ district per year @ Rs. 540
250/- per
2
Aids & appliances
Rs. 12,500 per year (18x12500)
3
Welfare allowance for RCS 150 Rs. 5,000/- per patient
patients
750
4
RCS 150 Nos.
750
Total
NRHM PIP 2009-10: Chhattisgarh
Rs. 5,000/- per RCS
Cost
225
2265
Page 318
Urban Leprosy Control Programme
Table 5.29: No. of urban areas identified for support
Sl. No.
Type of Urban Area
No.
Unit cost per year
Total cost for the year
1
Township
12
57
684
2
Medium cities – I
2
120
240
14
-
924
Total
Table 5.30: List of townships of Chhattisgarh
S. no.
District
Township
1
Sarguja
Ambikapur
2
Koriya
Koriya
3
Janjgir
Janjgir
4
Durg
Durg
5
Durg
Bhilai
6
Rajnandgaon
Rajnandgaon
7
Korba
Korba
8
Raigarh
Raigarh
9
Kawardha
Kawardha
10
Bastar
Jagadalpur
11
Mahasamund
Mahasamund
12
Dhamtari
Dhamtari
Medium Cities
1
Raipur
NRHM PIP 2009-10: Chhattisgarh
Raipur
Page 319
2
Bilaspur
Bilaspur
Table 5.31: Budget requirement for NGOs (000)
No. of NGO
Rate per NGO project per year
Cost for the year
2
500
1000
Supervision, Monitoring and Review
Table 5.32: Budget summary for review meeting
Sl. No.
Activity
Periodicity
Unit cost per meeting
Cost for the year
1
State level
Quarterly
15
60
2
District level
Monthly
-
-
Table 5.33: Budget summary for Travel for supervision and monitoring activity
Sl. No.
Travel cost categories
Annual Rate per year
Cost for the year
1
State
50
50
2
Districts (18)
15
270
Total
320
Table 5.34: Office expenditure (000)
S.
No.
Item
1
Rent, Telephone,
Charges, Misc.
No.
units
Electricity,
per Cost
year
for the
P&T
Districts
18
18
324
State Leprosy Cell
1
38
38
Sub Total
2
of Rate
year
362
Office equipments maintenance cost
NRHM PIP 2009-10: Chhattisgarh
Page 320
State Leprosy Cell
1
30
30
Total
392
Table 5.35: Consumables ('000)
Item
No. of units
Rate per year
Cost for the year
Districts
18
14
252
State Leprosy Cell
1
28
28
Stationary items
Total
280
Grand Total
19276
One Crore Ninety Two Lac Seventy Six Thousand Rupees (to be brought down to 160 lacs…..)
National Blindness Control Programme
Situation analysis with epidemiological parameters in CG
Incidence of blindness in Chhattisgarh is 3.6 lakhs that is the incidence rate is 2 per 1000
population. The prevalence rate (as per 2000- 01) in India is 1.10% where as in Chhattisgarh is
1.60 %. In the vision 2020, it is estimated to decrease at prevalence rate by 0.3 % till year 2020,
and up to 0.5 % by year 2010.
Table 5.36: Causes of Blindness in India and Chhattisgarh
Causes
India
Chhattisgarh
Cataract
62.8 %
71.5 %
Refractive error
19.7 %
10.6 %
Corneal Blindness
0.9%
0.2%
Glaucoma
5.8%
3%
Surgical comp
1.2.%
1.6%
Post surgical disorder
4.7%
6.2%
Others
5%
6.9%
NRHM PIP 2009-10: Chhattisgarh
Page 321
As per the data available the load of cataract cases is much higher, as well as the blindness
during surgical camp and post surgical disorder is also significant.
Activities:
1. Strengthening of Regional Institution of Ophthalmology (RIO) and providing ophthalmic
equipments.
2. Strengthening district hospitals IN Durg, Bilaspur, Raipur, and Bastar.
3. Appointment of ophthalmic assistant & ophthalmic surgeon.
4. Up gradation of Sub District hospital/ community health centre: Non-recurrence assistance
of Rs. 5 lakhs for up gradation of ophthalmic units with equipments for IOL surgery/ SICS.
IOL suture etc. This year Gidam, Udaipur, Tilda, Makdi, Pharasabahar, Bodala,
Dharamjaygarh, Jaijaipur, Kurud, Mungeli, Basana, Dondi, Mohala, Koyliben, Sonhat,
Kartala in 2009-10.
5. Development of Vision Testing Centre (VTS) at PHC and voluntary sector.
6. Support in Development of Eye bank development: Supported by GOI
7. Operationalising Eye wards and Eye OT to served underserved area in the state: For 20
bedded Ward and OT.
For 20 bedded Ward and OT: of each ward required following staff.
Table 5.37: budget summary for staff requirement for NBCP for 20 bedded Ward and OT
Sl. No.
Post
No.
Salary per Month
Annual
1
Staff Nurse
3
10,000
3,60,000.00
2
OT assistant / Technician
1
8000
96,000.00
3
Ward Boy
2
4000
72,000.00
4
Sweeper
1
3000
36,000.00
5
Total
564000.00
For 10 bedded ward and Eye OT
Table 5.38: budget summary for staff requirement for NBCP for 10 bedded Ward and OT
NRHM PIP 2009-10: Chhattisgarh
Page 322
Sl.
No.
Post
No.
Salary
Month
per Annual
1
Staff Nurse
2
10,000
2,40,000.00
2
OT assistant / Technician
1
8000
96,000.00
3
Ward Boy
2
4000
72,000.00
4
Sweeper
1
3000
36,000.00
5
Total
6
444000.00
All the eye surgeons are posted in district hospitals but no eye surgeon is posted at community
health centre; hence need at least one eye surgeon in above community health centre where
wards and OT are constructed.
The eye surgeon can be contractually appointed @ Rs. 30,000/ month, or can be hired from
private institution and can be paid per case.
1. Mobile Ophthalmic check up and cataract detection Van cases: One well equipped
mobile van with an ophthalmic assistance, a nurse and driver to conduct the village eye
check up camp to be started to served underserved area in state. One mobile van for five
to six blocks can be started or 2 mobile vans for a district having 10 to12 or more blocks.
The first priority can be given to tribal and hilly area. This Van can also promote the Eye
Donation and Awareness generation for Eye Health care. This van will be designed in
with all the eye care massages and will be having optician to prepare eyeglass (New
Initiative)
Table 5.39: Budget support for Mobile ophthalmic check up
Sl. No.
Post
No.
Salary per Month
Annual
1
Ophthalmic Nurse
1
10,000
120000.00
2
OT assistant / Technician
1
10,000
120000.00
Total
2,40,000
2. Free spectacles to School children and operated cataract cases: free spectacle can be
distributed to needy and poor school age children up to 10 Std. these spectacles can be
provided @ Rs.150 /- (125/ -) per spectacle. Free spectacles can also be distributed to all
cataract operated cases @ Rs. 200 /- Per spectacles. (these free spectacle are with
specification of A Carbon frame of appropriate size and plain English white glasses-
NRHM PIP 2009-10: Chhattisgarh
Page 323
after a market research it has been found that the good quality glasses available @ of Rs.
50 to 70 Varies from number to number)
3. Free spectacles to Schedule Tribe and Schedule Caste patient in rural area: This is
another initiative in the state to provide the free spectacles to the schedule tribe and
schedule caste people in the state, these spectacles can be prepared @ Rs. 150 /spectacles(These free spectacles should be with specification : a Carbon frame of
appropriate size suitable to the patient and plain English white glasses- after a market
research it is found that the good quality glasses available @ of Rs. 50 to 70. It Varies
from number to number)
4. Training of technical persons:
5. Training of ANM, AWW and Mitanin on Preventive Eye Care, Blindness Control and
Treatment.
6. Eye check up and free spectacles distribution to Mitanins: All Mitanin eye check will be
done in the current year and spectacles will be given at free of cost. All Mitanin Eye
check-up will be done at Respective Community health Centre and free spectacles will be
distributed to the needy Mitanin. (Budget @Rs. 150/- spectacles). (New initiative)
7. Demand Generation (For cataract operation, eye care and eye donation) and incentives
to Mitanin: This can be done by community awareness and community mobilisation by
community health volunteer (Mitanin), ANM and AWW. Each Mitanin can be given Rs.
50 for Mobilisation of cataract case. [ Rs. 50 * 100000)
8. Awareness Generation through IEC, BCC, and IPC: One of the most important causes
of blindness in our country and state is ignorance of the eye problems; hence, it is very
important to create awareness regarding eye care, and eye care services available in
public health services.
9. IEC through
a. Electronic Media: - 2, 00,000 /- and special fund can be kept for community
Radio programme/ local media.
b. Print Media: - In this hoardings, wall painting, slogan writing, poster printing,
information booklets, pamphlets, leaflets. Can be published.
c. Outdoor publicity: organising Kalajatha (infotainment), organising poster
preparation, writing competition, sport events for blindness control.
d. Eye donation fortnight:
NRHM PIP 2009-10: Chhattisgarh
Page 324
i.
At state level: 35,000/-
ii.
DBCS: - 35,000/- Each district. (18x 35,000= 630000)
e. World Sight Day:-
i.
Event organisation at state level: 400000/-
ii.
DBCS @200000x18= 3600000
10. Establishment of self vision testing centre at public places.
11. Maintenance of Ophthalmic equipment.
Monitoring and Evaluation:
Monitoring and evaluation of programme will be done by programme management unit at state
level, district level and block level and report will be submitted every month to the state office
and District blindness control society, state blindness control programme unit, SPM and State
Health Resource Centre.
Monitoring and Evaluation team
State level technical team: A state level 5 to 10 member team will be formed for the technical
evaluation of programme. This committee will be headed by state blindness control programme
office and 3 essential team members from the technical backgrounds like a ophthalmic surgeon,
public health specialist from SHRC, a person expert in spectacles preparations apart from this
SPM and other deputy director also be a part of the team. This evaluation can be done based on
following indicators.
1. No of surgery done during season:
2. No. of patient lost eye sight after operation operated or any complications
3. Spectacles distributed to the school age children, cataract patients and tribal patient
at free of cost are with the specification and as per the norms. (after the verification
of 5 to 10 % of distributed spectacles )
4. Functioning of the wards, OT and equipment in the state.
5. Functioning of all the institutions providing eye care Regional ophthalmic centre etc.
6. Functioning of Mobile van for eye testing
7. This team will evaluate team twice in a year at the interval of six months.
NRHM PIP 2009-10: Chhattisgarh
Page 325
District level programme Monitoring and Evaluation team: a district level programme
monitoring team headed by District CMHO will be formed in which District Programme
Manager and members of district blindness control society will and block programme manager
will be major role players. They will monitor
1. Functioning of the OPD and IPD services
2. Functioning of Mobile check up van
3. Organising Cataract Surgery camps at PHC/CHC/ District hospitals:
4. Functioning of spectacles shop
5. School eye check-up and distribution of spectacles to school age children, post
cataract cases and schedule caste and schedule tribe patient.
6. Training of Mitanin and ANM
7. Functioning of all the eye care equipments.
Table 5.40: Budget Summary for NBCP
Sr.
No.
Budget head
No. of
Unit
Unit cost
(Lakhs)
Total
Cost
(Lakhs)
1
1. Strengthening of Regional Institution of Ophthalmology
(RIO) and providing ophthalmic equipments. Medical
Colleges(Retina Unit /Low vision unit and paediatric
ophthalmic
2
40
80
2
Strengthening district hospitals
4
20
80
4
Up gradation of Sub District hospital/ community health
centre:
16
5
80
Restructuring vision testing centre at PHC / Voluntary org.
100
0.5 lakhs
50
Operationalising existing eye ward and Eye OT (20 bedded)
8
5.64
45.12
Operationalising existing eye ward and Eye OT (10 bedded)
8
4.44
35.52
Appointment of ophthalmic surgeon
8
0.25
02
Free Spectacles to school children
20000
0.0015
30
7
9
NRHM PIP 2009-10: Chhattisgarh
Page 326
10
Free Spectacles to ST and SC patient in rural area.
30000
0.0015
45
11
Training of Technical Personnel:
1. training of Ophthalmic nurse and Ophthalmic assistant
200
0.02
04
2. training of DPM
18
0.03
0.54
12
Training of community health volunteer
60000
0.002
120
13
Eye check up and distribution of Spectacles to Mitanin
30000
0.0015
45
14
Incentive to Mitanin For Mobilisation of cataract case
100000
0.0005
50
15
IEC
10
Self Vision Testing boards
1000
0.005
5
16
Equipment maintenance
18
3
54
17
Monitoring and Evaluation
state level monitoring team
1
1
2
District level monitoring team
18
0.5
9
18
Cataract Surgery
100000
.003
300
19
Other ophthalmic diseases
30000
.0026
78
Total
446791
86.5709
1125.18
Integrated Disease Surveillance Project
Situation analysis with epidemiological parameters:
NRHM PIP 2009-10: Chhattisgarh
Page 327
Out breaks reported in the year 2008-09 under IDSP
Table 5.41: epidemic outbreaks and action taken report
S. Week
No No.
Name of
District
Disease/
Illness
Population No. of
Affected
cases/
No. of
deaths
Date of
start of
outbreak
Date of
reporting
Current
Status
Action taken
1
18.10.08
Week
no. 48
Dhamtari
Village
Arjuni
Diarrhoea,
Gastro
Enteritis
560
56 / 1
16.10.08
18.10.08
Gram –ve
motile
organism seen
non cholera
District Rapid Response Team (RRT)
investigated the outbreak. Leakage of
pipeline of well rectified which caused
contamination of drinking water.
House-to-house survey done for new
cases. Treatment of cases done.
Chlorine tablets and ORS packets
distributed. Health education given
regarding personal hygiene.
2
29.09.08
Week
no. 39
Koriya
Village Mahora &
Pandopara
Diarrhoea
&
Vomiting
180
04/02
22.09.08
23.09.08
Under
Observation
Medical camp conducted in the
affected area. House-to-house survey
done for new cases. Disinfection and
chlorination of drinking water sources
done. Chlorine tablets and ORS
packets distributed. Health education
given regarding personal hygiene.
3
17.08.08
Week
no. 33
Janjgir
Pamgarh
& Sakati
Diarrhoea
&
Vomiting
400
22 / 0
11.08.08
11.08.08
Under
Observation
District Rapid Response Team (RRT)
investigated the outbreak. Leakage of
pipeline of Tube well rectified which
caused contamination of drinking
water. House-to-house survey done
for new cases. Treatment of cases
done. Chlorine tablets and ORS
packets distributed. Health education
NRHM PIP 2009-10: Chhattisgarh
Page 328
given regarding personal hygiene.
4
09.08.08
Week
no. 32
Durg
Village Changori,
CHC
Patan
Chicken
Pox
50
5/0
06.08.08
08.08.08
Under
Observation
Medical officer with team visited the
affected area. Treatment of cases
done. Health education given.
Table 5.42: Outbreaks reported in Epidemic
section
NRHM PIP 2009-10: Chhattisgarh
Page 329
Activities at the state level will include:
1. preparing and sending monthly summaries of the disease situation to the central level;
2. training state and district level staff;
3. implementing periodic surveys for non-communicable diseases and/or their risk factors;
4. implementing Quality Assurance surveys (in conjunction with GOI);
5. integration of disease control efforts based on the surveillance data;
6. supporting districts in data analysis, transport of laboratory specimens, and outbreak
investigations;
7. Analyzing surveillance data across districts.
Monitoring and evaluation of programme will be done based on following Indicators
1. Number and percentage of districts providing monthly surveillance reports on time - by state
and overall;
2. Number and percentage of responses to disease-specific triggers on time - by state and
overall;
3. Number and percentage of responses to disease-specific triggers assessed to be adequate by state and overall;
4. Number and percentage of laboratories providing adequate quality of information - by state
and centre;
5. Number of districts in which private providers are contributing to disease information;
6. Number of reports derived from private health care providers;
7. Number of reports derived from private laboratories;
8. % of states in which surveillance information relating to various vertical disease control
programs have been integrated
9. % of project districts and states publishing annual surveillance reports within three months
of the end of the fiscal year;
10. Publication by CSU of consolidated annual surveillance report (print, electronic, including
posting on the websites) within three months of the end of fiscal year
NRHM PIP 2009-10: Chhattisgarh
Page 330
Table 5.43: Proposed Action Plan & Budget For Year 2009-2010
Sl. No.
1
Activities
2
To be
implemented
from
Physical
Target
Time Frame
3
4
5
Q1
Q2
Q3
Responsibility
Unit
Cost
Multiplying
Factor
Budget
Required
Remarks
6
7
8
9
10
Q4
A. CIVIL WORK
1
Renovation of DSU
District
5
3
2
-
-
CMHO,
DSO
1,40,000
5
7,00,000
Janjgir, Jashpur, Kawardha,
Narayanpur & Bijapur
2
Renovation of District Lab.
District
8
2
4
2
-
CMHO, CS
& DSO
1,40,000
8
11,20,000
Bilaspur, Raipur, Janjgir,
Jashpur, Kawardha, Koriya,
Narayanpur & Bijapur
Sub total
18,20,000
B. PROCUREMENT OF LABORATORY EQUIPMENTS
36,40,000
1
Equipment of State Lab - 1 No.
State
1
-
1
-
-
DHFW, SSO,
DME & Dean
MC, Raipur
8,50,000
1
8,50,000
As per standard list of IDSP
2
Equipment of District Labs.
District
5
-
2
3
-
CMHO, CS
& DSO
6,00,000
5
30,00,000
Raipur, Bilaspur, Koriya,
Narayanpur & Bijapur. As per
standard list of IDSP
3
Hot Air Oven & Auto Clave for
district laboratories
State
18
-
18
-
-
DHFW, SSO
2,50,000
18
45,00,000
For all the District Labs.
4
Equipment of Peripheral Labs.
District
49
-
20
29
-
CMHO, CS
& DSO
40,000
49
19,60,000
As per standard list of IDSP
SUB TOTAL
1,39,50,000
C. PROCUREMENT OF OFFICE EQUIPMENTS
1
Air Conditioner for District
Surveillance Unit
District
10
10
NRHM PIP 2009-10: Chhattisgarh
-
-
-
CMHO &
DSO
20,000
10
2,00,000
Page 331
3
Telephone for District Surveillance
Units
District
1
1
-
-
-
CMHO &
DSO
10000
1
10,000
2
Telephone for Peripheral
Surveillance Units
District
88
44
44
-
-
CMHO &
DSO
10000
88
8,80,000
4
Over Head Projector for District
Surveillance Units
District
18
18
-
-
CMHO &
DSO
10000
18
1,80,000
SUB TOTAL
12,70,000
D. FURNITURE & FIXTURES
1
Furnishing of District DSU.
District
4
2
2
-
-
CMHO, CS
& DSO
60,000
4
2,40,000
Raipur, Raigarh, Narayanpur &
Bijapur.
2
Furnishing of District Lab.
District
5
2
3
-
-
CMHO, CS
& DSO
60,000
5
3,00,000
Raipur, Raigarh, Koriya,
Narayanpur & Bijapur.
3
Furnishing of Peripheral
Surveillance unit at CHC / Block
PHC - ( 1 No. per PSU)
Block / CHC
44
-
22
22
-
CMHO, CS
& DSO
10,000
44
4,40,000
4
Furnishing of Peripheral Lab (1 No.
CHC / Block PHC)
Block / CHC
44
-
22
22
-
CMHO, DSO
& BMO
10,000
44
4,40,000
SUB TOTAL
14,20,000
E. MATERIAL & SUPPLIES FOR LABORATORIES
1
For State Laboratory
State
1
-
1
-
-
DHFW, SSO,
DME & Dean
MC, Raipur
2,00,000
1
2,00,000
2
For District Laboratory
District
18
-
18
-
-
CMHO, CS
& DSO
1,00,000
18
18,00,000
3
For Peripheral Laboratory at CHC
( 1 No. per PSU / CHC)
District
146
-
146
-
-
CMHO, DSO
& BMO
10,000
146
14,60,000
SUB TOTAL
34,60,000
F. REMUNERATION OF CONTRACTUAL PERSONNEL
NRHM PIP 2009-10: Chhattisgarh
Page 332
18
3
Additional fund
3 months
84,000
12
10,08,000
Remuneration of contractual
staff has been fixed based on
survey held in 2003 hence
40 % increase in remuneration
is proposed.
SSO, CMHO
& DSO
39,200
18 *12
84,67,200
Remuneration of contractual
staff has been fixed based on
survey held in 2003 hence
40 % increase in remuneration
is proposed.
75,00,000
Salaries for contractual staff of
2 microbiologist and 17
Epidemiologist
3 months
District
DHFW &
SSO
3 months
District Surveillance Unit
3 months
2
3 months
1
3 months
State
3 months
State Surveillance unit
3 months
1
SUB TOTAL
94,75,200
G. INFORMATION, EDUCATION & COMMUNICATION
1
Organisation of sensitization
workshops
District
18
4
4
4
6
SSO, CMHO
& DSO
30,000
18
5,40,000
Once in a year in each district.
2
Review meetings of district
committee
District
72
18
18
18
18
SSO, CMHO
& DSO
2,500
72
1,80,000
One meeting in each district in
each quarter.
3
Press advertisement
District
2
-
1
1
-
SSO, CMHO
& DSO
3,60,000
Rs.20,000 per district x 18
districts.
4
Print media (Pamphlets, Brochures
etc.)
District
2
-
1
1
-
SSO, CMHO
& DSO
3,60,000
Rs.20,000 per district x 18
districts.
5
Other media including indigenous
methods
District
18
-
1
1
-
SSO, CMHO
& DSO
3,60,000
Rs.20,000 per district x 18
districts.
6
Organisation of sensitization
workshops
State
2
-
1
1
-
DHFW &
SSO
50,000
2
1,00,000
7
Review meetings of state committee
/ DSU
State
4
1
1
1
1
DHFW &
SSO
12,500
4
50,000
4
Press advertisement
State
2
-
1
1
-
DHFW &
SSO
1,50,000
1
1,50,000
NRHM PIP 2009-10: Chhattisgarh
Page 333
5
Print media (Pamphlets, Brochures
etc.)
State
-
1
1
-
DHFW &
SSO
1,50,000
1,50,000
6
Telecasting of TV spots
State
-
1
1
-
DHFW &
SSO
4,00,000
4,00,000
7
Broadcasting on Radio
State
-
1
1
-
DHFW &
SSO
1,50,000
1,50,000
SUB TOTAL
28,00,000
I. TRAINING
1
1 day's orientation of CMHOs &
CSs of state.
State
36
-
36
-
-
DHFW &
SSO
2,500
36
90,000
2
1 day's refresher training of BEE /
Multi Purpose Supervisors / Multi
Purpose Workers
District /
Block
7200
1800
1800
1800
1800
SSO, CMHO
& DSO
650
7200
46,80,000
4
3 day's training of Peripheral Lab.
Teach. / Lab. Assistants.
District
270
-
90
90
90
SSO, CMHO
& DSO
1,200
270
3,24,000
5
1 day's Workshop of MOs of District
Hospital - Raipur, Durg, Bilaspur &
Raigarh.
District
45
22
23
-
-
SSO, CMHO
& DSO
1,200
45
54,000
6
3 day's training of Medical Officers.
District
450
90
120
120
120
SSO, CMHO
& DSO
2,000
450
9,00,000
7
6 day's training of Lab. Technicians.
State
35
35
-
-
-
SSO, CMHO
& DSO
3,500
35
1,22,500
SUB TOTAL
61,70,500
J. OPERATIONAL COSTS
NRHM PIP 2009-10: Chhattisgarh
Page 334
As discussed with National
Project Officer during his visit
to Raipur in September 2008.
STATE LEVEL: Travel cost, POL,
Maintenance or hiring of vehicles,
Office expenses on telephone, fax,
electricity etc., Office stationery and
other consumable items, DA to
officers / staff engaged under IDSP,
Miscellaneous including
contingencies.
State
Surveillance
Unit
1 unit
3 months
3 months
3 months
21,90,000
CMHO &
DSO
1000*12
146
17,52,000
CMHO &
DSO
1,30,000
18
23,40,000
DHFW &
SSO,
3,50,000
1
3,50,000
3 months
4
146
3 months
18 units
15,000
TA/DA of block level staff for
submitting IDSP weekly reports
to DSU every week for data
feeding.
3 months
District
Surveillance
Unit
CMHO, DSO
& BMO
3 months
DISTRICT LEVEL: Travel cost,
POL, Maintenance or hiring of
vehicles, Office expenses on
telephone, fax, electricity etc.,
Office stationery and other
consumable items, DA to officers /
staff engaged under IDSP,
Miscellaneous including
contingencies.
3 months
3
3 months
146 units
3 months
District
Surveillance
Unit
3 months
TA/ DA of peripheral staff for IDSP
report collection ( Block to District)
3 months
2
3 months
146 units
3 months
District
Surveillance
Unit
3 months
PERIPHERAL LEVEL: Travel cost,
POL, Maintenance or hiring of
vehicles, Office expenses on
telephone, fax, electricity etc.,
Office stationery and other
consumable items, DA to officers /
staff engaged under IDSP,
Miscellaneous including
contingencies.
3 months
1
SUB
TOTAL
66,32,000
K
PRINTING
1
Printing of Forms, Formats &
Register
State
1
1
NRHM PIP 2009-10: Chhattisgarh
-
-
-
DHFW &
SSO,
2,00,000
1
2,00,000
Page 335
Rs. 200,000 per year.
2
Printing of Forms, Formats &
Register
District
18
18
-
-
-
CMHO &
DSO
1,00,000
18
SUB TOTAL
18,00,000
Rs. 100,000 per district per year.
20,00,000
L
IT EQUIPMENT
1
Computer P IV with Laser Printer,
Scanner and UPS
District
2
-
2
-
-
CMHO &
DSO
75,000
2
1,50,000
May be supplied by Central
Surveillance Unit / NIC.
2
Replacement of old UPS supplied
during the inception of the project.
State
2
-
2
-
-
DHFW &
SSO,
5,000
2
10,000
May be supplied by Central
Surveillance Unit / NIC.
3
Replacement of old UPS supplied
during the inception of the project.
District
16
-
16
-
-
CMHO &
DSO
5,000
16
80,000
May be supplied by Central
Surveillance Unit / NIC.
4
Replacement of old UPS supplied
during the inception of the project.
Medical
College
3
-
3
-
-
Dean,
CMHO &
DSO
5,000
3
15,000
May be supplied by Central
Surveillance Unit / NIC.
SUB TOTAL
2,55,000
GRAND TOTAL
53112700
Unit cost has been calculated as per IDSP Financial guidelines.
NRHM PIP 2009-10: Chhattisgarh
Page 336
National Iodine Deficiency Disorders Control Programme (NIID)
Situation Analysis:
In the 1960s, correction of iodine deficiency was exclusively handled through
administration of iodine in the form of potassium iodide solution or Lugol’s solution.
Initially, IDD was thought to be a problem in the sub-Himalayan region. The highly
endemic region of India is the sub-Himalayan belt stretching from Kashmir in the
Northwest to the Naga Hills (Nagaland) in the East, extending about 2,400 km. However,
surveys carried out subsequently by the Ministry of Health and Family Welfare (MOHFW)
showed that iodine deficiency disorders exist even in riverine and coastal areas. Goitre
surveys conducted in 283 districts in 25 States and four Union Territories over a wide
period of time (1960’s to 1990’s) have identified 241 districts as IDD endemic. No state /
UT in India is free from IDD. The implications of iodine deficiency for the unborn are of
serious concern in India where 25 million women become pregnant each year. Half of the
newborn is unprotected against brain damage simply because their mother did not consume
adequately iodized salt during their pregnancy. Impact of iodine deficiency on physical
performance and productivity of adults cannot be underestimated in a country where the
population below poverty line, nearly a third of the total population, depends on physical
labour for its livelihood.
In the state of Chhattisgarh, salt from 59 percent of households were found with > 15 PPM
iodine, another 9 percent were found to have 1 to 15 PPM of Iodine, while salt from 30
percent households did not have iodine. (Coverage Evaluation Survey, UNICEF & GoI
2005), Iodine.
Activities:
1. Set up an IDD control cell comprising of representation from DOHFW, DWCD,
Education department, Civil Supplies and Salt Traders, civil society organizations
like UNICEF who meet regularly to monitor & evaluate progress towards achieving
USI.
2. Regular rapid testing of salt quality in all government programs (like ICDSsupplementary nutrition program, MDM) through use of MBI Salt Testing Kits.
3. Regular reporting on the quality of the tested salt that is collated at block/district
and state level. This report is used to initiate action by authorities at various levels.
4. Initiate road and railway check points to prevent entry of non-iodized salt into the
state.
5. Initiate the school movement for iodized salt program- a program guided towards
increasing awareness on iodize not only within the students but also among their
families and neighbours.
6. Regular meetings with the salt traders and promote sale of iodized salt.
7. Conduct IDD surveys in all the 18 districts
8. Supporting Sishu Sanraksaan Maah for use of iodized salt.
9. Awareness campaign and celebrating world iodine day: As awareness generation,
campaign worldwide celebration of ‘world iodine day’ on 22 October every year.
This year state will decide to celebrate this day as awareness generation
programme.
The budget proposal forwarded the last year was not sanctioned and as such, as per the
NRHM guideline for allocation of Funds the proposal for the year 2009-2010 is as stated
below:
Monitoring of Programme
1. State level technical committee will be set up for monitoring the programme in
which, Join Director of the programme, representative from technical supporting
organisation like State Health Resource Centre, UNICEF, CARE and
Micronutrition Initiative will be the part of the committee. Bi annual evaluation
will be done with a representative sample from the entire districts as well as
evaluation of each district programme.
2. A District level team will be formed for operationalising evaluation and monitoring
of programme based on indicators like percent of household using IODIZED Salt
and Use of IODIZED salt in Government run programme.
The budget requirement will be met through the grant received from the treasury route
that includes the IDD and infrastructure.
NRHM PIP 2009-10: Chhattisgarh
Page 338
PART E: CONVERGENCE
Introduction:
The Health department will have convergence in action in the State for achievement of
NRHM goals with various departments like Women and Child Development, Education,
Rural Development and Panchayati Raj, Social Welfare etc.
Prevention of Anaemia among children and adolescents:
Increased proportion of women and children in India are suffering from several forms of
infections and diseases. One of the common causes for these recurrent episodes of infection
is reduced immune power of the body. According to the NFHS-III, 81% of children aged 6
months to 3 years, living in Chhattisgarh are anaemic. However, paediatric iron tablets are
supplied for use among children, it is not consumed well and the compliance is poor. Iron
in syrup form seems to be accepted better by young children in some states where it is
introduced recently. Therefore, we, at Chhattisgarh, may adopt the same strategy to
supplement iron deficiency through provision of iron syrup. It can be given to both the preschool and young children along with iron tablets. Anganwadi seems to be the best service
delivery point for this scheme. In addition, schools can be other suitable venues with easy
access to children.
Another group in great need of iron supplementation is young adolescent girls. They have
increased need of iron during this period to meet their growth need and menstrual blood
loss. It is a well documented fact that anaemia of pregnant women gives rise to low birth
weight baby and expose the young infant to increased risk of death during pregnancy and
delivery. Anaemia would lead to the vicious cycle of low iron level, infections and low birth
weight. To break this vicious cycle the adolescent may be supplied with iron
supplementation.
a. The Department of Health and Family Welfare will provide iron syrup in
requisite amount for children aged 6 months to 3 years.
b. Paediatric iron tablets will be provided through the sub centres and anganwadi
to preschool children aged 3 to 6 years.
c. Adult iron tablets will be provided to out of school adolescent girls aged 11 to
18 years from anganwadi centres in weekly doses.
d. School going adolescent girls aged 11 to 18 years will be supplied with iron
tablets on a fixed day every week under the direct observation of the teacher,
while the schools will receive its iron tablets supply from the Department of
Health and Family Welfare.
NRHM PIP 2009-10: Chhattisgarh
Page 339
For distribution of IFA tablets and Syrup for Anganwadi, centres will be through the WCD.
In addition, this will be procured from the state budget. This component has been
incorporated under child health.
Referral of sick Newborn, Young child and malnourished children with
complications.
After the IMNCI –Newborn and Child Survival training of Mitanins the post natal visit to
families has increased detecting sick newborns and active referral to PHCs and
hospitals.AWW will also be oriented to do joint post natal visit and weighing of newborns.
Similarly, a malnourished child with complications will be referred to PHC for primary
treatment or to a Paediatrician at CHC or to Nutrition Rehabilitation Centre. The
AWW/Mitanin will be given an incentive of Rs.100/- for referral by the Health department.
AW centre would be taken care by Medical Officers of PHC periodically, for example one
PHC caters 25-40 AWCs, MO will go to AW centre and screen the children and
adolescents and make necessary referrals if require..
Timely initiation of Complementary Feeding-
“Annaprasan” ceremony for all infants reaching six months of age will be a celebration
event during monthly Health and Nutrition day in every Anganwadi Centre. Both ANM and
AW Worker will jointly organize this event.
Integrated Health, Nutrition, Immunisation and Development card for children and
mothers:
To avoid duplication of efforts on gathering information on the above parameters by
DWCD and Health Department, efforts will be made to integrate required information into
one card. This card will be issued at the time of registration of pregnancy of the mother and
will be used till the newborn child reaches the age of five. It will have a cross referencing
number with JSY Scheme. The cost of printing of this card will be made out of DWCD funds
allocated for this and will be regularly updated and used by both departmental
functionaries.
AYUSH Orientation
To AW Workers-similar to the orientation given to Mitanins.
Bal Suposhan Yojana-
Already described under Child Health
Swasth Pathshala Yojana:
Already mentioned under Child Health
Monthly village health and nutrition Melas:
NRHM PIP 2009-10: Chhattisgarh
Page 340
Since the last quarter of 2003, the state has initiated the efforts for coordination between
ANM, AWW and the Mitanin and state wide training programmes were organised in order
to achieve this. A monthly mela was envisaged where all maternal as well as child health
issues could be provided under one roof on a single day. There was support from all
concerned departments and Care, and this gave good results to an extent. Now, this has
been adopted by the ICDS and Health Programmes. In this duration, number of Anganwadi
centres increased to 29000 from the earlier 22000 and the sub-centres to 4694 from the
earlier 3818 and the coverage has been expanded.
Involvement of Total Sanitation Campaign in quality of health services–
This campaign is being run by Department of PHED with link departments. This
programme is having provision for the construction of toilets and urinals in government/
semi government institutions. State NRHM would like to request to the nodal department
for construction and renovation of the toilets in the hospitals & health-care institutions, as
these areas are the critical areas of concern in the quality of hospital services. We are not
asking for budget allocation, we are just looking forward for collaboration and support
with the department of Public Health Engineering Department. We will provide mapping
details of the areas that require the provision of toilets. Planning & implementation will be
done by the nodal department in coordination with department of health & family welfare.
The PHED has already ensured toilets for each Mitanin (community health volunteer).
Meanwhile Mitanins will generate awareness about water & sanitation issues & promote
the usage of toilets.
Budget Requirements:
The other initiative shall continue with available local resources like CARE organization,
untied sub-centre fund, Village health and sanitation committee funds under NRHM. With
reference to the budget requisition of prevention of anaemia among children and
adolescents, this will be covered under procurement. No separate budgeting has been made
for these on these grounds for other programmes.
NRHM PIP 2009-10: Chhattisgarh
Page 341
Provisional NRHM PIP 2009-10:
to be submitted to GoI- at a glance
S.No. Component
Salient Features
A.
PART A - RCH Flexipool
1
MATERNAL HEALTH
1.1
FRU Operationalisation
1.2
Indemnity insurance for multiskilled Medical Officers
1.3
Multiskilling programme for operationalization of FRUs
1.4
Referral Transport
1.5
Integrated Outreach RCH Services
1.6
Janani Suraksha Yojana
1.7
JSY Helpline
1.8
Accreditation of Private Facility
1.9
Preventing Post partum Haemorrhage in rural areas in institutional settings:
Included in procurment budget head
1.1
ANC kits for pregnant women in disease-prone areas
Converge with Malaria bed net
Incentivising the Caesarian deliveries
in CHCs, PHCs & Subcenters.
Providing indemnity insurance to multi
skill trained doctors as security against
any mishaps during discharging their
services
MOU with FOGSI,Institutional
upgradation of selected training
centers
Providing Ambulance (including
support) for support
Providing RCH Outreach Camps in unserved/ under-served areas (ANC kits
for pregnant women in disease prone
areas.)
Incentive to the beneficiaries,
motivators & administrative cost
Fulfilling emergency requirements
through JSY Helpline
Page
Proposed Budget
Number Outlay 2009-10
1,73,66,250
3,90,000
11,67,440
2,25,00,000
-
57,20,00,000
20,40,000
-
distribution programme
1.11
Maternal and infant death auditing committee
1.12
PNDT & Sex Ratio
1.13
Replication of "Chiranjivi scheme"
-
The Committee would conduct
investigations to establish the causes
of deaths- expenditure will be incurred
from JSY administrative cost
Operationalising PNDT Cell (Activity
may be carry forwarded )
1,00,00,000
accreditate institutions with more
than 50 deliveries per month
Sub Total: Maternal Health
62,54,63,690
2
CHILD HEALTH
2.1
Facility Based Newborn Care
2.2
Home Based New Born Care
2.3
Swagat package for mother & newborn for Institutional Deliveries
2.4
Child Friendly Health Facility Accreditation
2.5
Sishu Sanrakshan Mah
2.6
Baal Suposhan Yojana
2.7
Management of Diarrhoea with ORS & Zinc
2.8
IMNCI
2.9
School Health Programme
2.10
Creches in District Hospitals
2.11
Sub Total: Child Health
NRHM PIP 2009-10: Chhattisgarh
1,64,00,000
Strengthening Facility based newborn
care in Raipur Medical College
provision of home based care for the
new born
Incentivising institutional Delivery
82,28,000
3,25,00,000
-
To ensure that all the newborns are
born in baby friendly health facilities &
start on breast-milk immediately
Integrated bi- annual maternal and
child health month
Care of Children with Severe or Acute
Malnutrion
Care & Support for the development
of children
Management of Neonatal and
Childhood Illness
Sawasthya pathshala yojanaOrganizing Screening Camps
Setting up of creches in district
hospitals for child care
3,15,40,000
2,50,80,000
1,49,46,849
87,16,750
3,77,25,000
-
Page 343
17,51,36,599
3
FAMILY PLANNING
3.1
Family planing process in Public and Private sector
3.2
Maintenance of OT & instruments
3.3
Establishment of State FW Bureau
3.4
Terminal Limiting Method
3.5
Spacing Method
3.6
Other Segregation Activities
3.8
NSV Kit
20,88,50,000
10,00,000
-
Only the Public Health Expert post
created in this activities and
budgetedin Programme Mangaement
Organising camps in districts, WITH
FOCUS ON NSV.
Promoting IUD
49,00,000
1,20,00,000
Annual Maintenance of Laparoscope
Machine in the districts .
Procurement of NSV kit
7,50,000
Sub Total: Family Planning
22,75,00,000
4
ADOLESCENT & REPRODUCTIVE SEXUAL HEALTH
4.1
Adolescent Friendly Services
5
Urban RCH
5.1
Other Urban RCH strategies/activities
6
Infrastructure & Human Resources
6.1
Civil Works and human resources
7
Training
7.1
Maternal Health Training
NRHM PIP 2009-10: Chhattisgarh
Setting up Sakhi/ Sakha Kendras,
Imparting the knowledge at school
level
Infrastructure development, last year's
money and EUSPP supported fund
available
8,27,12,000
appointment of staff nurses at
CHCs and PHcs based on
IPHS,minor civil works for
operationalisation of FRUS (Blood
Storage).
Page 344
7.1.1
Institutional Support - Strengthening departments of paediatrics in 3
Training Institutes
7.1.2
Multi-skill Training
7.2
Child Health Training
7.2.1
IMNCI Training
7.2.2
HBNC Training
7.3
Family Planning Training
7.3.1
Family planning Training of Doctors on LTT @ 3 MOs/Batch
7.3.2
Alternative method for IUCD insertion for ANM and LHVs
7.3.3
ToT for district level trainers at state level
7.3.4
Sensitizing workshop for ToT plus logistic
7.5
Training Activities (SIHFW) (Component A:F)
Multiskilling Training of CHC Mos
for FRU operationalization (carried
forward)
Multiskilling Training of Health-care
personnel at all Levels
63,00,770
IMNCI Training for staff nurses,
ANMs/LHVs, Anganwadi workers
Training for providing care for the
new-born
2,50,000
1,20,00,000
7,30,000
50,000
1,18,76,600
Training Activities
Sub Total: Training
3,12,07,370
8
BCC/IEC
Organizing District level events
through Radio, Kalajattha and for
IEC strategy dissemination, printed
materials, posters, workshops,
Establishment of the BCC/ IEC Cell
9
Urban RCH
Selection and training of community
care givers, peer educators
11
PROGRAMME MANAGEMENT
11.1
Strengthening of State Society / SPMU
State PMU
11.2
Strengthening of District Society / DPMU
District PMU
NRHM PIP 2009-10: Chhattisgarh
1,48,50,000
-
3,79,29,800
Page 345
11.3
Establishment of procurement cell
-
Budget will be born by EUSPP
Sub total of Programme Management
3,79,29,800
12
Convergence /Coordination
12.1
Providing Technical Advice to
MNGOs
Encourage institutional delivery of
positive mothers
1,19,47,99,459
TOTAL RCH II FLEXIPOOL
* denotes unused funds of prior year available, no additional allocation
required.
B.
PART B - NRHM SPECIAL INITIATIVES
1
Jeevan Deep Samiti
1.1
Maintenance grants for SHCs, PHCs and CHCs
1.2
ISO Certification
2
Sub Centre Strenthening
2.1
Improved Public Health Care
Facilities- CHCs, PHCs, also
ensuring their unctioning &
accessibility
Maintenance of SHCs, PHCs and
CHCs
ISO certification of 3 district
hospital and 1 CHC
Strenthening the Sub - centers by
fund allocation & additional/
panchayat based ANMs
10,66,20,000
ANM Appointment
appoint assisstant ANM/2nd ANM
Support for PHC & Sub Centres infrastructure
200 Subcentres and 9 PHCs
2,80,80,000
22,52,00,000
75,60,000
2.2
Placement of Hospital Management professionals at Government Health
Facilities for Technical Assistance
3
Alternative Nursing Staff
sponsorship of 200 ANM
3.1
Training of LHVs:
training of ANMs to be promoted
to LHV Cadre(Carry Forward)
4
Rural Medical Assitants
NRHM PIP 2009-10: Chhattisgarh
9,70,60,000
90,00,000
4,74,10,000
228
1,00,00,000
-
231
6,78,50,000
Page 346
17,70,00,000
5
Strenthening Mitanin Programme
Improving Community level health
care & service utilization
7
Mobile Medical Units
Increasing the reach of Medical
Services
3,10,72,000
8
Bal Hriday Suraksha Yojana
3,07,10,000
9
Strengthening Village Health & Sanitation Committee
10
Monitoring & Evaluation
11
Telephones for Sub Centres / New PHCs
Heart Surgeries of identified
children
Activization of VHSCs through
Gram Swastha Swachta Samiti
Niyojan Abhiyaan
Developing & usage of HMIS (Some
financial requirement for the
above activities will be made
through administrative cost)
Only recurring cost which will be
born by available untie dfund at
the facility level, no separate fund
12
State Level Technical Assistance- SHRC
Personal, operational
research,workshops
89,27,600
13
*Special Initiative - Snakebite Care in Northern Chhattisgarh
16,00,000
14
Sickle Cell disease control programme
15
Strengthening of AYUSH
Procurement of vaccine, referral
and training/IEC of the community
volunteers including system
grassroot workers.
Screening, public awarness ,
treatement and rehabilitation and
establishment of sickle cell clinical/
treatement unit and research
centre
Development of AYUSHDEEP AND
AYUSH GRAM, training of ayush
doctors maternity and child ward
in aurvedic college ,
humanresources integrated
epidemic cell and ayush technical
NRHM PIP 2009-10: Chhattisgarh
20,33,40,000
34,34,000
-
17,28,000
4,24,27,000
Page 347
assistance in state level
16
Third Party Monitoring
17
Filling up vacancies in HR Management
18
Community Monitoring at various levels
19
Professionalisation of Health Management
20
Building and Strengthening of Block PMU
23
Support in creation Chhattisgarh Rural Medical Corps for difficult areas
24
Closing Residential and Accommodation Gaps
25
Capacity building & Mobilization of PRI for local health planning
NRHM PIP 2009-10: Chhattisgarh
To support the administration and
implimentres regarding
programme throuth t ird party
monitoring system support.
Hiring of HR agency TO ENSURE
BETTER HR MANAGEMENT
Monitoring of community based
NRHM intervention through
accredated block /district/ state
level committee based on
triangulation approach
Capacity building of the
government health officials and
technical persons in public heailt
under PHRN through contact
sessions
Development of programme and
financial management unit at the
block level in order to accelerate
the NRHM activities
Development of an
incentive/package for the doctors
& other health care personnel to
support the difficult areas
Closing residential gaps in PHCs
50,00,000
25,00,000
300
23,87,000
-
10,60,82,400
303
7,35,00,000
10,00,00,000
233
o
capacity building and development
of village health plans
Page 348
27
Distribution of Bed Nets
28
29
29.1
Chhattisgarh Health Equipment Management System
PROCUREMENT
29.2
Procurement of Drugs & Supplies
Procurement of Equipments
Provide bednets to tribal families
in high risk areas
Capacity building for technical staff
234
4,80,00,000
28,99,400
10,00,00,000
Procurement of RCH Kit, Kit
A,B,ANM kit, NRHM Kit, PHC/CHC
Kit, RTI/STI kit(requested by
CGSACS)
Drugs and Supplies for routine
CHC/PHC and Subcentres as per
GoI lists (May be in Kind/ cash)
Sub Total: Procurement
10,00,00,000
1,53,93,87,400
Total for NRHM Special Initiatives
* denotes unused funds of prior year available, no additional allocation
required.
PART C - IMMUNIZATION
C
9,66,52,688
Strengthening immunization
coverage rates
9,66,52,688
Total for Immunisation Activities
1
PART D - NATIONAL DISEASE CONTROL PROGRAMMES
D
RNTCP
1
Malaria Control
2
Filaria Contol
NRHM PIP 2009-10: Chhattisgarh
8,23,40,007
To achieve & maintain a cure rate
of at least 85% , strengthening the
referral system, increasing
involvement of other sectors
Control of Malaria (WORLD BANK
ASSISTENCE)
Control of Filaria & Maleria
(Domestic Budget Support)
12,99,46,500
7,16,24,000
Page 349
3
4
Leprosy Eradication
Integrated Disease Surveillance Programme
5
6
Blindness Control
Iodine Deficiency Disease Control
1,60,00,000
5,31,12,700
Control of Leprosy
Integrating & Strengthening
disease surveillance at state &
district level
Control of Blindness in the State
Elimination of Iodine Deficiency
Disorder
11,25,18,000
-
Total for Disease Control Programme
46,55,41,207
PART E - CONVERGENCE
Coordination with Other Departments
-
Total for Convergence Activities
1
NRHM Total Outlay 2009-10
1,19,47,99,459
1,53,93,87,400
9,66,52,688
46,55,41,207
-
PART -A
PART -B
PART -C
PART -D
PART -E
3,29,63,80,754
Total (Part A, B, C, D, E)
88,80,00,000
66,00,00,000
Infrastructure and maintenance(Central Govt. Scheme)
Special accomodation/Residential Facilities at naxalite affected area,
recommended by Ministry of Tribal GoI
GRAND TOTAL
NRHM PIP 2009-10: Chhattisgarh
4,84,43,80,754
Page 350
Budget detail RCH Flexipool , Part - A 2009-10
Unit of
S.No
Budget Head
Physical Target
Rate
Measure
QI
Q II
Q III
Q IV
Total
Annual
Financial Allocation (Rs. Lakhs)
(Rs./
Unit)
Total
QI
Q II
Q III
Q IV
Annual
1
MATERNAL HEALTH
1.1.
Operationalise facilities (details of infrastructure & human resources, training, IEC/BCC,
equipment, drugs and supplies in sections 9, 11, 12 and 13)
1.1
Operationalise Block PHCs/ CHCs/ SDHs/DHs as FRUs
1.1.2
Indeminity Insurance to Multiskilled MO's
78
20
20
19
19
78
1.1.3
ANM incentive at Sub & PHC centre
474100
1.1.4
Incentive at PHC Level
1.1.5
5000
100000
100000
95000
95000
390000
118525
118525
118525
118525
474100
50
1481562
1481562
1481562
1481564
5926250
721
1
1
1
1
4
100
1802500
1802500
1802500
1802500
7210000
Incentive at CHC Level
136 + 18
1
1
1
1
4
100
385000
385000
385000
385000
1540000
1.1.6
Administrtive Head of the block (BMO) and BPM and other supportives
146
1
1
1
1
4
15000
547500
547500
547500
547500
2190000
1.1.7
District Authority (CMHO) and nodal
3
3
3
500000
0
0
0
500000
500000
1.1.8
FOGSI
0
1
291860
291860
291860
291860
1167440
1.1.9
EMOC institutional upgradation training
1.1.10
Home deliveries
60000
15000
15000
15000
15000
60000
500
7500000
7500000
7500000
7500000
30000000
1.1.11
Institutional deliveries, urben
100000
25000
25000
25000
25000
100000
1200
30000000
30000000
30000000
30000000
120000000
1.1.12
Institutional deliveries, rural
200000
50000
50000
50000
50000
200000
2000
100000000
100000000
100000000
100000000
400000000
1.1.13
4 % on Admn and IEC Cost
0
0
0
0
0
1
5500000
5500000
5500000
5500000
22000000
1.1.14
Secod referal transport for Materanal and neonatal care
7500
7500
7500
7500
30000
750
5625000
5625000
5625000
5625000
22500000
0
30000
NRHM PIP 2009-10: Chhattisgarh
Page 351
1.1.15
2
2.1.1
2.1.2
JSY Helpline: Extending Help to the deserved:
0
0
0
0
0
1
510000
510000
510000
510000
2040000
Sub-total Maternal Health (excluding JSY)
10743422
10743422
10738422
11238424
43463690
Sub-total JSY
143000000
143000000
143000000
143000000
572000000
Maternal Health Grand Total
153743422
153743422
153738422
154238424
615463690
CHILD HEALTH
0
Facility Based Newborn Care (FBNC), CH
1
1
1
1
1
4
Child Friendly Health Facility Accreditation
4100000
4100000
4100000
4100000
0
16400000
0
2.1.3
IMNCI
0
10000
2179186
2179188
2179188
2179188
8716750
2.1.4
Integrated bi - annual maternal and Child health month( Sishu Sanraksaan Maah)
0
1
7885000
7885000
7885000
7885000
31540000
2.1.5
School Health Programme (Swasth Patshala)
1
1
1
1
1
4
1
9431250
9431250
9431250
9431250
37725000
2.1.6
Bal Suposhan Yojana ( Care of children with Severe or Acute Malnutrition )
4
1
1
1
1
4
2
6270000
6270000
6270000
6270000
25080000
2.1.7
Swagath Package for Mothers and Newborns for Institutional deliveries
0
1
8125000
8125000
8125000
8125000
32500000
2.1.8
Management of Diarrhoea with ORS and Zinc
4
1
1
1
1
4
1
3736712
3736712
3736713
3736712
14946849
2.1.9
Home Based Neonatal Child Care (HBNCC)
4
1
1
1
1
4
1
2057000
2057000
2057000
2057000
8228000
43784148
43784150
43784151
43784150
175136599
1
3428500
3428500
3428500
3428500
13714000
Sub-total Child Health
3
3.1
FAMILY PLANNING
0
Calculations do not reflect the true picture. It would be updated subsequently
(Details of training, IEC/BCC, equipment, drugs and supplies in sections 11, 12 and 13)
3.1.1
Organise NSV camps in districts.
0
3.1.2
Compensation for female sterilisation Public
170000
42500
42500
42500
42500
170000
1000
42500000
42500000
42500000
42500000
170000000
3.1.3
Compensation for female sterilisation Private
20000
5000
5000
5000
5000
20000
1000
5000000
5000000
5000000
5000000
20000000
3.1.4
Compensation for NSV Acceptance (Public)
10000
2500
2500
2500
2500
10000
1500
3750000
3750000
3750000
3750000
15000000
NRHM PIP 2009-10: Chhattisgarh
0
Page 352
3.1.5
Compensation for NSV Acceptance (Private)
700
175
175
175
175
700
1500
262500
262500
262500
262500
1050000
3.1.6
IUD incentive (public).
118000
29500
29500
29500
29500
118000
20
590000
590000
590000
590000
2360000
3.1.7
IUD Incentive (Private)
12000
3000
3000
3000
3000
12000
75
225000
225000
225000
225000
900000
3.2.1
Annual Maintenance and supply of antiseptic etc for lapascopic machiene in the dist hospital
where machine surgeons are available.
12
1000000
12000000
0
0
0
12000000
3.2.2
NSV Instrument
1
187500
187500
187500
187500
750000
3.3.1
Maintenances of Operation Theatre and Instrument.
1
500000
500000
3.4.1
Establishment of State Family Welfare Bureau
4.1
0
56875000
56875000
56875000
227500000
0
Funds for adolescent Health Clinic (ARSH CLINIC) Sakhi Sakha Kendra
4.1.3
Developing training module for the life skill education at the state level workshop
4.1.4
Implement ARSH knowledge at school level by peer educators
Sub-total ARSH
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
0
URBAN RCH
Urban RCH Services
Sub-total Urban Health
6.1
56875000
Adolescent friendly services
4.1.2
6
0
0
Funds for adolescent Health Clinic (ARSH CLINIC) Sakhi Sakha Kendra
5.1.1
1000000
ADOLESCENT REPRODUCTIVE AND SEXUAL HEALTH / ARSH
4.1.1
5
12
0
Sub-total Family Planning
4
12
TRIBAL RCH
0
Tribal RCH services
0
NRHM PIP 2009-10: Chhattisgarh
0
Page 353
0
0
0
0
6.1.1
Other Tribal RCH strategies/activities (please specify – PPP/ Innovations/NGO to be mentioned
under section 8)
0
Sub-total Tribal Health
7
0
0
0
0
0
0
0
0
0
0
VULNERABLE GROUPS
0
7.1
Specific health activities targeting vulnerable communities such as SCs, STs, and BPL
populations living in urban and rural areas (not covered by Urban and Tribal RCH)
0
0
0
0
0
0
7.2
Services for Vulnerable groups
0
0
0
0
0
0
7.3
Other strategies/activities (please specify – PPP/ Innovations/NGO to be mentioned under
section 8)
0
0
0
0
0
0
0
0
0
0
0
Sub-total Vulnerable Groups
8
8.1
INNOVATIONS/ PPP/ NGO
0
PNDT and Sex Ratio
0
Sub-total Innovations/ PPP/ NGO
9
9.1
0
0
0
0
INFRASTRUCTURE AND HUMAN RESOURCES
Contractual Staff & Services
9.1.1
Appointment of 502 staff Nurses (fw)
502
9.1.2
Appointment of 650 staff nurses (fw)
650
650
502
502
502
502
7000
0
9370667
9370667
9370666
28112000
650
650
650
650
7000
13650000
13650000
13650000
13650000
54600000
13650000
23020667
23020667
23020666
82712000
Sub-total Infrastructure and Human Resources
10
0
INSTITUTIONAL STRENGTHENING
0
10.1
Human Resources Development
0
0
0
0
0
0
10.2
Logistics management/ improvement
0
0
0
0
0
0
10.3
Monitoring & Evaluation / HMIS
0
0
0
0
0
0
0
0
0
0
0
0
Sub-total Institutional Strengthening
11
TRAINING
0
NRHM PIP 2009-10: Chhattisgarh
Page 354
11.1.1
Laparoscopic Sterilisation Training (LTT) Training of Doctors on LTT @ 3MOs/Batch
10
3
3
2
2
10
11.1.2
Alternative method for IUCD Insertion for ANM and LHVs
6239
11.1.3
Sensitizing workshop for district training personal
11.1.4
11.1.5
25000
75000
75000
50000
50000
250000
1560
1560
1560
1559
6239
1
3000000
3000000
3000000
3000000
12000000
48
12
12
12
12
48
1000
14000
12000
12000
12000
50000
TOT for district level trainers at state level:
146
37
37
37
35
146
5000
185000
185000
185000
175000
730000
Other Training Proposal from SIHFW
4
1
1
1
1
4
1
2969150
2969150
2969150
2969150
11876600
1
1
1
1
4
1575193
1575193
1575193
1575191
6300770
7818343
7816343
7791343
7781341
31207370
Multiskilling Training of Health-care personnel at all Levels(Maternal Health)
11.1.7
Sub-total Training
12
BCC / IEC
0
12.1.1
State Level /District level BCC cell
1
0
1
12.1.2
Training and exposure visit to other places ( state /districts)
50
12
12
12
12.1.3
5
1
1
1
12.1.4
Research on BCC ( area /community specific issues), Monitoring & Evaluatin
Printed and AV material (posters, bulletin, success story reports, health calendar, Quarterly
magazines & diaries etc)
1
1
12.1.5
Media Ads on various related health days
12
3
Sub-total BCC/ IEC
13
13.1
13.1.1
14.1
3
500000
0
500000
0
0
500000
14
50
25000
300000
300000
300000
350000
1250000
2
5
100000
100000
100000
100000
200000
500000
1
1000000
1000000
0
0
0
1000000
12
200000
600000
600000
600000
600000
2400000
4200000
3700000
4100000
2850000
14850000
3
PROCUREMENT
Procurement of Equipment
Procurement of RCh Kit A,B, ANM, NRHM kit, PHC/CHC kit RTI/STI kit (requested by CGSACS)
Sub-total Procurement
14
3
1
0
0
PROGRAMME MANAGEMENT
Strengthening of State society/State Programme Management Support Unit (details of
training under section 11)
NRHM PIP 2009-10: Chhattisgarh
Page 355
0
0
0
0
14.1.1
14.2
14.2.1
Contractual Staff for SPMSU recruited and in position including establishment cost & others
12
months
4
4
4
4
Strengthening of District society/District Programme Management Support Unit
4
4
4
4
16
Sub-total Programme Management
15
Convergence/ Coordination
16
MNGO Funds
17
Establishment of Procurment Cell
18
Chirinjevi Scheem
2498450
2498450
2498450
2498450
9993800
6984000
6984000
6984000
6984000
27936000
9482450
9482450
9482450
9482450
37929800
0
12
months
Contractual Staff for DPMSU recruited and in position
16
12
months
4
4
4
4
16
1
1
Sub- Total Convergennce / Coordination
TOTAL RCH II FLEXIPOOL
GRAND TOTAL
NRHM PIP 2009-10: Chhattisgarh
0
2500000
2500000
2500000
2500000
10000000
2500000
2500000
2500000
2500000
10000000
292053363
300922032
301292033
300532031
1194799459
Page 356
Budget detail RCH Flexipool , Part - A 2009-10
Financial Allocation (Rs. Lakhs)
S.No
Budget Head
QI
Q II
Q III
Remarks
Total
Q IV
Annual
1
1.1.
2
3
4
5
6
MATERNAL HEALTH
Operationalise facilities (details of infrastructure & human
resources, training, IEC/BCC, equipment, drugs and
supplies in sections 9, 11, 12 and 13)
Sub-total Maternal Health (excluding JSY)
10743422
10743422
10738422
11238424
43463690
Sub-total JSY
143000000
143000000
143000000
143000000
572000000
Maternal Health Grand Total
153743422
153743422
153738422
154238424
615463690
0
CHILD HEALTH
Sub-total Child Health
43784148
43784150
43784151
43784150
175136599
Sub-total Family Planning
56875000
56875000
56875000
56875000
227500000
FAMILY PLANNING
ADOLESCENT REPRODUCTIVE
HEALTH / ARSH
AND
SEXUAL
Sub-total ARSH
0
0
0
0
0
Sub-total Urban Health
0
0
0
0
0
URBAN RCH
0
TRIBAL RCH
Sub-total Tribal Health
7
0
0
0
0
0
0
VULNERABLE GROUPS
Sub-total Vulnerable Groups
8
0
INNOVATIONS/ PPP/ NGO
0
0
0
0
0
0
8.1
0
PNDT and Sex Ratio
Sub-total Innovations/ PPP/ NGO
9
0
0
0
0
13650000
23020667
23020667
23020666
82712000
INFRASTRUCTURE AND HUMAN RESOURCES
Sub-total Infrastructure and Human Resources
10
0
0
INSTITUTIONAL STRENGTHENING
Sub-total Institutional Strengthening
11
13
14
0
0
0
0
0
TRAINING
Sub-total Training
12
0
7818343
7816343
7791343
7781341
31207370
0
BCC / IEC
Sub-total BCC/ IEC
4200000
3700000
4100000
2850000
14850000
Sub-total Procurement
0
0
0
0
0
9482450
9482450
9482450
9482450
37929800
PROCUREMENT
PROGRAMME MANAGEMENT
Sub-total Programme Management
15
Convergence/ Coordination
16
MNGO Funds
17
Establishment of Procurment Cell
18
Chirinjevi Scheem
0
Sub- Total Convergennce / Coordination
TOTAL RCH II FLEXIPOOL
GRAND TOTAL
2500000
2500000
2500000
2500000
10000000
2500000
2500000
2500000
2500000
10000000
292053363
300922032
301292033
300532031
1194799459
NRHM PIP 2009-10: Chhattisgarh
Page 358
Part B NRHM Flexipool
Detailed Budget 2009-10
No. of Units
Sl No
1
Unit of
Measure
Strategy / Activity
Q1
Q2
Q3
Total Cost (Rs.)
Q4
Total
Unit
Cost
Q1
Q2
Q3
Q4
Total
Jeevan deep samiti( Hospital Development committee)
1.1
Assistance for district hospital / Civil Hospital
36
18
18
36
500000
9000000
9000000
0
0
18000000
1.2
Assistance for CHCs
136
68
68
136
100000
6800000
6800000
0
0
13600000
1.3
Assistance for PHCs
721
180
180
361
721
100000
18000000
18000000
36100000
0
72100000
1.4
Block level orientation / workshop
146
37
37
37
146
20000
740000
740000
740000
700000
2920000
0
0
34540000
34540000
36840000
700000
106620000
5000000
4000000
0
0
9000000
5000000
4000000
0
0
9000000
35
Jeevan deep total
2
2.1
ISO Certificate for 3 District Hospital
ISO Certificate for 3 District Hospital
3+1
1
1
2
4
Total ISO
3
Budget for maintanance Grant for SHCs ,PHCs,& CHCs
3.1
SHCs Maintanance
4741
1185
1185
1185
1186
4741
10000
11850000
11850000
11850000
11860000
47410000
3.2
PHCs Maintanance
721
180
180
180
181
721
50000
9000000
9000000
9000000
9050000
36050000
3.3
CHCs Maintanance Grant
136
34
34
34
34
136
100000
3400000
3400000
3400000
3400000
13600000
24250000
24250000
24250000
24310000
97060000
sub Total Maintanance Grant
4
0
Sub centre Strengthening
4.1
Untied assistance
4.2
Training of 2 ANM for private and public centre
4.3
Appointment of Hospital Administrators to provide support in district hospital
Sub centre Strengthening Total
4741
1185
1185
1185
1186
4741
10000
11850000
11850000
11850000
11860000
47410000
600
150
150
150
150
600
600
7020000
7020000
7020000
7020000
28080000
18
18
18
420000
1890000
1890000
1890000
1890000
7560000
20760000
20760000
20760000
20770000
83050000
0
5
0
Support for Subcentres and PHCs Infrastructure
5.1
Sub Centre
5.2
Primary Health Centre
200
50
50
9
50
50
9
200
1000000
50000000
50000000
50000000
50000000
200000000
9
2800000
0
0
25200000
0
25200000
50000000
50000000
75200000
50000000
225200000
2500000
2500000
2500000
2500000
10000000
2500000
2500000
2500000
2500000
10000000
Sub Total
6
6.1
The proposed study for development of Alternative Nursing Staff
Sponsorships to for 200 student for 18 months course, course fees, food, hostel and study material
200
200
200
50000
Total
7
Tribal Health
7.1
placement and Induction Training for Rural Medical Assistants
700
400
700
700
700
700
8500
16962500
16962500
16962500
16962500
67850000
7.2
Closing residential gap (HSC)
250
63
63
63
61
250
200000
12600000
12600000
12600000
12200000
50000000
7.3
10 Housing Unit in naxsal effected area, remote and trible area.
10
3
3
2
2
10
5000000
15000000
15000000
10000000
10000000
50000000
7.4
Distribution of Insecticide treated bed nets for families in high risk tribal areas
80000
20000
20000
20000
20000
80000
600
12000000
12000000
12000000
12000000
48000000
7.5
Support in creation of Rural Medical Corps in difficult (conflict) areas in Chhattisgarh
4
1
1
1
1
4
1
18375000
18375000
18375000
18375000
73500000
74937500
74937500
69937500
69537500
289350000
0
0
0
0
0
Tribal Health Total
8
0
Strengthening Mitanin programme under ASHA
8.1
Strengthening Mitanin programme under ASHA
4
1
1
1
1
4
4
37500000
37500000
37500000
37500000
150000000
8.2
Mitanin Drug Kit
4
1
1
1
1
4
4
6750000
6750000
6750000
6750000
27000000
44250000
44250000
44250000
44250000
177000000
Total Strengthening Mitanain Programme
9
9.1
0
Procurements
5
5
5
5
20
Procurment
5
5
5
5
20
0
0
0
0
0
sub total procurment
NRHM PIP 2009-10: Chhattisgarh
0
0
25000000
25000000
25000000
25000000
100000000
25000000
25000000
25000000
25000000
100000000
Page 360
10
Mobile Medical Unit Recurring Cost
10.1
Remmunaration of Drivers
10.2
POL for the Vehicle
8
11
76
10
20
20
26
76
72000
720000
1440000
1440000
1872000
5472000
256
64
64
64
64
256
100000
6400000
6400000
6400000
6400000
25600000
0
0
0
0
0
0
7120000
7840000
7840000
8272000
31072000
1
1
1
1
1
1
1
7500000
7500000
7500000
7500000
30000000
1
1
1
1
1
1
Total Mobile Medical Unit Recurring Cost
Bal Hridaya Suraksha Yojana : Chief Ministers’ Child Heart Protection Scheme
11.1
Bal Hridaya Suraksha Yojana : Programme Exp
11.2
Human Resource and Contingency
177500
177500
177500
177500
710000
7677500
7677500
7677500
7677500
30710000
0
0
0
0
0
50830000
50830000
50830000
50850000
203340000
0
50830000
50830000
50830000
50850000
203340000
0
0
0
0
0
0
858500
858500
858500
858500
3434000
Bal Hridaya Total
12
12.1
0
Untied fund for village health and sanitation committee
Untied fund
20334
5083
5083
5083
5085
Untied fund Total
13
Monitoring and Evaluation
13.1
Documentation Management solution and digitization services
13.2
Mobility , stationary and other exp. Per annum
509
1
1
1
1
4
5609
1
1
1
1
4
Total Monitoring and Evaluation
14
15.1
0
0
858500
858500
858500
858500
3434000
Budget for implementing Community based Monitoring in 3 new districts
1
1
1
1
1
4
4
67500
67500
67500
67500
270000
1
1
1
1
1
4
4
529250
529250
529250
529250
2117000
596750
596750
596750
596750
2387000
2231900
2231900
2231900
2231900
8927600
2231900
2231900
2231900
2231900
8927600
Community Monitoring Total
15
10000
Community based Monitoring
Budget for continuation of activity in 3 districts already covered under pilot phase
14.1
14.2
20334
0
State level resource support -SHRC
State level resource support -SHRC
1
Total State level resource support -SHRC
NRHM PIP 2009-10: Chhattisgarh
1
1
1
1
4
0
1
Page 361
16
Sickle Cell Anemia
16.1
Screening of the target population
0
0
0
0
0
0
16.2
One counsellor at the each district hospital which can be collaborated with the district hospital and under the CMHO
432000
432000
432000
432000
1728000
16.3
Counsellor’s training on the genetic counselling of sickle call affected couples and family
0
0
0
0
0
0
16.4
Target adolescent, school , collages and women groups education and counselling
0
0
0
0
0
0
16.5
Target adolescent, school , collages and women groups education and counselling
0
0
0
0
0
0
0
432000
432000
432000
432000
1728000
18
1
1
1
1
Total Sickle Cell Anemia
17
4
8000
10
Ayush Components
17.1
Flexible fund for ayushdeep samiti for monitoring
0
400000
400000
400000
400000
1600000
17.2
Essential Medicine for ayush centre in PHC/CHC in trible areas
0
2493750
2493750
2493750
2493750
9975000
17.3
Additional Manpower for ayush unit in trible CHC and PHC
0
3360000
3360000
3360000
3360000
13440000
17.4
Essential Meternal and Child Health Training for Ayush Doctors
0
250000
250000
250000
250000
1000000
17.5
Public Health Management Training of Ayush Medical Officers
0
37500
37500
37500
37500
150000
17.6
National Consultative work shop for creation of road Map of ayush mainstreming
0
587500
587500
587500
587500
2350000
17.7
Ayush Training for ANM and Agw worker
0
2625000
2625000
2625000
2625000
10500000
17.8
Training of Paramedical staff
0
187500
187500
187500
187500
750000
17.9
Supporting Ayush cell in SHRC
0
553500
553500
553500
553500
2214000
Support to meternity and Child ward in Govt Ayurveda College
0
112000
112000
112000
112000
448000
Ayush Components
0
10606750
10606750
10606750
10606750
42427000
17.10
NRHM PIP 2009-10: Chhattisgarh
0
0
0
Page 362
18
Third Party Monitoring
18.1
Contracting in Thired party institutions/groups
1
1
1
1
1
4
1000000
1000000
1000000
1000000
1000000
4000000
18.2
Miscellaneus expenditure like dissemination of reports
1
1
1
1
1
4
250000
250000
250000
250000
250000
1000000
1250000
1250000
1250000
1250000
5000000
1000000
500000
500000
500000
2500000
1000000
500000
500000
500000
2500000
0
Third Party Monitoring
19
Filling up vacancies and HR management
19.1
Human Resource manager will work under SPMU unit.
19.2
Out sourcing recruitment under NRHM to state level or national level agency /civil society.
10
4
2
2
2
17.1
Special initiative -snake bite care in Northern Chhattisgarh -Pilot in Jashpur district
Anti venom, incentives for Referral and training and IEC for snake bite etc.
1
1
1
1
1
4
1
400000
400000
400000
400000
1600000
0
0
0
0
0
0
400000
400000
400000
400000
1600000
146
1
1
1
1
4
13800
6044400
6044400
6044400
6044400
24177600
146
1
1
1
1
4
11500
5037000
5037000
5037000
5037000
20148000
146
1
1
1
1
4
150
503700
503700
503700
503700
2014800
146
1
1
1
1
4
2000
876000
876000
876000
876000
3504000
PHC level Accounts and data assistant
721
1
1
1
1
4
6000
12978000
12978000
12978000
12978000
51912000
PHC Contingency
721
1
1
1
1
4
500
1081500
1081500
1081500
1081500
4326000
26520600
26520600
26520600
26520600
106082400
0
0
0
0
Total Special initiative -snake bite care
18
250000
0
Total Filling up vacancies and HR management
20
10
Programme Management
Block Programme Managers
18.1
Account cum Data Assistant
18.2
Travelling @1000
18.3
Contingency
18.4
18.5
Total Programme Management
19
19.1
0
Teaching aid and other support for strengthening public health system
Up gradation of Dept
3
1
1
1
3
Total
NRHM PIP 2009-10: Chhattisgarh
Page 363
20
0
Chhattisgarh Health Equipment Management System
Personnel to be trained TOT for Nurse, ANMs , Nurses
20.1
5742
Total Health Equip. Mngt Syst
21
Provision for the Bio-medical Waste Management at district hospital in first phase through outsourcing-
22
Biomedical waste management (Outsourcing)
Bio-medical Waste Management Total
Grand Total
NRHM PIP 2009-10: Chhattisgarh
1435
1435
1435
1437
5742
0
1900
724850
724850
724850
724850
2899400
724850
724850
724850
724850
2899400
0
0
0
0
0
391486350
390706350
409206350
347988350
1539387400
0
0
Page 364
Part B NRHM Flexipool
Detailed Budget 2009-10
Sl No Strategy / Activity
1
Total
34540000
34540000
36840000
700000
106620000
5000000
4000000
0
0
9000000
24250000
24250000
24250000
24310000
97060000
0
20760000
20760000
20760000
20770000
83050000
50000000
50000000
75200000
50000000
225200000
2500000
2500000
2500000
2500000
10000000
Support for Subcentres and PHCs Infrastructure
Sub Total
6
Q4
Sub centre Strengthening
Sub centre Strengthening Total
5
Q3
Budget for maintanance Grant for SHCs ,PHCs,& CHCs
sub Total Maintanance Grant
4
Q2
ISO Certificate for 3 District Hospital
Total ISO
3
Q1
Jeevan deep samiti( Hospital Development committee)
Jeevan deep total
2
Total Cost (Rs.)
The proposed study for development of Alternative Nursing Staff
Total
7
8
9
Tribal Health
Tribal Health Total
74937500
74937500
69937500
69537500
289350000
Strengthening Mitanin programme under ASHA
0
0
0
0
0
Total Strengthening Mitanain Programme
44250000
44250000
44250000
44250000
177000000
sub total procurment
25000000
25000000
25000000
25000000
100000000
7120000
7840000
7840000
8272000
31072000
Bal Hridaya Total
7677500
7677500
7677500
7677500
30710000
Untied fund for village health and sanitation committee
0
0
0
0
0
Untied fund Total
50830000
50830000
50830000
50850000
203340000
Monitoring and Evaluation
0
0
0
0
0
Total Monitoring and Evaluation
858500
858500
858500
858500
3434000
10
Mobile Medical Unit Recurring Cost
8
Total Mobile Medical Unit Recurring Cost
11
Bal Hridaya Suraksha Yojana : Chief Ministers’ Child Heart
Protection Scheme
12
13
14
0
Procurements
Community based Monitoring
NRHM PIP 2009-10: Chhattisgarh
Page 366
Community Monitoring Total
15
2231900
2231900
2231900
8927600
432000
432000
432000
432000
1728000
10606750
10606750
10606750
10606750
42427000
1250000
1250000
1250000
1250000
5000000
1000000
500000
500000
500000
2500000
400000
400000
400000
400000
1600000
26520600
26520600
26520600
26520600
106082400
Special initiative -snake bite care in Northern Chhattisgarh Pilot in Jashpur district
Total Special initiative -snake bite care
21
2231900
Filling up vacancies and HR management
Total Filling up vacancies and HR management
20
2387000
Third Party Monitoring
Third Party Monitoring
19
596750
Ayush Components
Ayush Components
18
596750
Sickle Cell Anemia
Total Sickle Cell Anemia
17
596750
State level resource support -SHRC
Total State level resource support -SHRC
16
596750
Programme Management
Total Programme Management
NRHM PIP 2009-10: Chhattisgarh
Page 367
22
Teaching aid and other support for strengthening public health
system
Total
23
0
Chhattisgarh Health Equipment Management System
Total Health Equip. Mngt Syst
24
0
724850
724850
724850
724850
2899400
Bio-medical Waste Management Total
0
0
0
0
0
Grand Total
391486350 390706350 409206350 347988350 153938740
0
Provision for the Bio-medical Waste Management at district
hospital in first phase through outsourcing-
NRHM PIP 2009-10: Chhattisgarh
Page 368
Annexure : Village Health Plan
NRHM PIP 2009-10: Chhattisgarh
Page 370
NRHM PIP 2009-10: Chhattisgarh
Page 371
NRHM PIP 2009-10: Chhattisgarh
Page 372
NRHM PIP 2009-10: Chhattisgarh
Page 373
NRHM PIP 2009-10: Chhattisgarh
Page 374
NRHM PIP 2009-10: Chhattisgarh
Page 375
NRHM PIP 2009-10: Chhattisgarh
Page 376
Annexure:
ISO Certification of Korba District Hospital
NRHM PIP 2009-10: Chhattisgarh
Page 377
NRHM PIP 2009-10: Chhattisgarh
Page 378
NRHM PIP 2009-10: Chhattisgarh
Page 379
NRHM PIP 2009-10: Chhattisgarh
Page 380
NRHM PIP 2009-10: Chhattisgarh
Page 381
Annexure : IEC integrated Plan/calendar
Programme
Activities
Amount
RNTCP
IEC/ Publicity
2810975
2600000
Malaria
5.1 Health Camps / Mela State and
District Level
5.2 IEC Awareness through NGOs /
CBOs / Panchyat
1000000
5.3 Other IEC activities (Electronic and
Print Media)
5000000
IEC activities in 9 endemic districts
ofstate
Filaria
1350000
@ Rs. 1.5
Lakhs per
district
900000
@ Rs.1.00
Lakhs per
district*9
450000
@ Rs.50000
Lakhs per
district *9
Printing of IEC Material, enumeration
registers and reporting formats
Dissemination of messages through
news papers, TV and Radio etc
Leprosy
Mass,Media,
(TV Radio Press)
550000
Out door Media
1450000
Rural Media
2000000
Advocacy meetings
1000000
Blindness
Self Vision Testing boards 1000
500000
IDSP
Organisation of sensitization workshops
5,40,000
Review meetings of district committee
1,80,000
Press advertisement
3,60,000
Print media (Pemphlets, Brouchers etc.)
3,60,000
Other media includind indigenous
methods
3,60,000
NRHM PIP 2009-10: Chhattisgarh
Remarks
0.005
Page 382
IDDCP
BCC Kit for Mitanin
Organisation of sensitization workshops
1,00,000
Review meetings of state committee /
DSU
50,000
Press advertisement
1,50,000
Print media (Pemphlets, Brouchers etc.)
1,50,000
Telecasting of TV spots
4,00,000
Broadcasting on Radio
1,50,000
Printing of monitoring formats, IEC
materials, radio spots
300000
BCC Kit to Mitanins/MTs and DRPs (
Budget for BCC kit will be from
European Union State assistance )
60000000
60000
Bal.Amt. 8-9
Part A
State Level /District level BCC cell
500000
200000
Training and exposure visit to other
places (state /districts)
1250000
600000
Research on BCC ( area /community
specific issues), Monitoring & Evaluatin
500000
Printed and AV material (posters,
bulletin, success story reports, health
calendar, Quarterly magazines &
diaries etc)
1000000
1000000
Block level BCC interventions
(including 4 urban areas) (Radio,
kalajattha and for IEC strategy
dissemination)
7500000
2500000
State Level events
800000
500000
District Level events( Radio, TV, AV,
Human Media as per IEC strategy
dissemination)
900000
900000
NRHM PIP 2009-10: Chhattisgarh
Page 383
Media Ads on various related health
days
2400000
1000000
AV Van
3284000
Technical Support to District
3200000
Concept And material Development
Workshop
300000
13484000
Total
PNDT
26168000
Assistance for coordinating activities,
especially awareness roles at
Directorate Level, brochures
hoardings, posters, and electronic media
etc.
2000000
Social Mobilization Activities like News
Shishu Sanrachan Mah Paper Advertisements during the month
ORS and Zinc
97560975
500000
TV Spots
500000
Development and Print wall hanging
poster @2 per AWC, 2 per SHC, 5 per
PHC, 10 per CHC/DH
800000
NRHM PIP 2009-10: Chhattisgarh
Page 384
RNTCP STATUS IN CHHATTISGARH: 2008-2009
Revised National Control programme was implemented in Chhattisgarh state on 15.8.2002 in
four districts namely, Raipur, Bilaspur, Durg & Rajnandgoan. In a phased manner RNTCP was
implemented in all the districts as mentioned below.
Dhamtari, Kanker, Janjgir, Raigarh, Kawardha
26th January 2004
Mahasamund
24th March 2004
Korba, Jashpur
5th May 2004
Bastar
29th May 2004
Koriya, Sarguja, Dantewada
15th August 2004
GOAL OF RNTCP : State is committed to the goal of RNTCP to reduce the mortality &
morbidity due to TB & cut the transmission of infection until TB ceases to be a major public
health problem.
OBJECTIVES: State is also committed to achieve the objectives of the programme “To achieve
& maintain a CURE RATE OF ATLEAST 85% among newly detected cases who are infectious
(NSP-New sputum positive) & to achieve & maintain a DETECTION RATE of 70% of such
cases in the population”
STATE PROFILE UNDER RNTCP:
•
Population - 2,40,31,000
•
No. of districts implementing RNTCP- 16. Out of total 146 blocks, 68 blocks are Notified
Tribal blocks
•
No. of TUs (TB units For every 5 Lakh Population) – 61
•
No. of DMCs (Designated Microscopic centre For every 1 Lakh Population in non tribal
area & for every 50, 000 population in tribal & hilly area) – 287
•
No. of DOT (Directly Observed Treatment )Centers - 5836
•
No. of Medical Colleges implementing RNTCP- 3/3
NRHM PIP 2009-10: Chhattisgarh
Page 385
•
Percentage of tribal population
- 34%
STAFF POSITION OF STATE TB CELL:
Staff Pattern:
•
Joint Director, TB - Present
•
State TB Officer- Present
•
Deputy STO - vacant
RNTCP Contractual Staff Status at STC :
Post
Sanctioned
In place
State Medical Officer
1
0
TB/HIV Coordinator
1
1
Microbiologist
1
1
Accountant
1
1
IEC Officer
1
1
Pharmacist
1
1
Data Entry Operator
1
1
Secretarial Assistant
Sanctioned
1
Driver
In place
Distri
ct
level
infras
tructu
re/sta
ff
positi
on
under
RNT
CP:
0
1
State 1
Contractual
Government under RNTCP
staff
NRHM PIP 2009-10: Chhattisgarh
Page 386
No.
DTOs
8
2.
No. of
MOTCs
61
53
4
3.
No. of
STS
61
0
47
4.
No. of
STLS
62
0
55
5.
No. of
LTs of
DMCs
287
179
106
1.
16
0
(2 Full time)
Performance Trends:
Annualized case detection Rate & Treatment success rate in Chhattisgarh
NRHM PIP 2009-10: Chhattisgarh
Page 387
CURE RATE (>85%)-4Q07
100
PERCENT
95
90
85
85 85 85
81
80
79
84 84
83
81
80
83
84
85
84 84
85
86
83
81
83
82
83
75
70
02
4Q
03
2Q
03
4Q
04
2Q
04
4Q
05
2Q
05
4Q
06
2Q
06
4Q
07
2Q
07
4Q
QUARTER
17
ACDR-NSP (>70%)-4Q08
100
90
80
Percent
70
65
60 60
60
59
50
50
47
42 41
49
52
56
56
51
60
55
59 61
62
54 53 56
52 51
40
30
20
10
2Q
03
3Q
03
4Q
03
1Q
04
2Q
04
3Q
04
4Q
04
1Q
05
2Q
05
3Q
05
4Q
05
1Q
06
2Q
06
3Q
06
4Q
06
1Q
07
2Q
07
3Q
07
4Q
07
1Q
08
2Q
08
3Q
08
4Q
08
0
QUARTER
16
THE 5 COMPONENTS OF DOTS :
Political & administrative commitment
NRHM PIP 2009-10: Chhattisgarh
Page 388
Diagnosis by Sputum Smear microscopy
Adequate & uninterrupted supply of the right drugs
Directly observed treatment
Accountability & Robust Reporting
To realize the five components of DOTS, state has taken many initiatives as mentioned below by
identifying the priority areas:
1. Involvement of general health system: By imparting on job training for different health cadre
staff like, BMOs, Medical officers, Supervisors & Para Medical staff.
2. Emphasis on Public Private Partnerships: By involving other government health sectors in
RNTCP. In the year of 2008, state has involved many PSUs like Bhilai steel plant,
BALCO,NTPC, CSEB by establishing DMCs. State also successfully conducted training of M.Os
of Indian Railways & Jail, followed by establishing DMCs.
3. Effective efforts to involve Private practitioners: State successfully organized state level
workshop of pediatricians to involve them in the programme so as to ensure a standardized
treatment for pediatric TB patients. State also successfully organized the state level workshop to
involve all the catholic health facilities of the state, who are delivering health care services in
the remote areas. State is also planning to have a partnership with IMA o involve all the private
practitioners in the programme.
4. Effective involvement of Medical colleges: State has successfully formed the state task force.
Chairman of the STF being Director Medical education. In all the medical colleges, core
committee has been formed to supervise the RNTCP activities on monthly basis. In STF
meetings, advocacy has been done to take up Research activities in Medical colleges. Separate
funding has been done under Medical College Head for training of the medical college faculty.
Chhattisgarh state hosted the ZTF meeting for the year-2008. Participants from five states
namely, West Bengal, Orissa, Bihar, Jharkhand & Chhattisgarh attended this work shop.
5.As the sputum microscopy is the back bone of programme & one of the components of DOTS,
state has successfully established a Annual maintenance contract this year, to ensure quality
microscopic activities at the field level.
6. To ensure the uninterrupted drug supply, State has innovated a mechanism of transportation
of Drugs from state Drugs Store to various districts.
7. State is committed to address the issue of TB HIV co infection. Successful coordination has
been done with CGSACS to establish a mechanism of cross referral of TB HIV co infected
NRHM PIP 2009-10: Chhattisgarh
Page 389
patients. At state level, state TB- HIV coordination committee has been formed to supervise the
TB HIV collaborative activities.
8. To strengthen the referral system of TB patients, between the bordering states, INTER STATE
MEETING between Chhattisgarh, Orissa, Madhya pradesh & Jharkhand is planned. This
innovation would facilitate the tracing of TB patients migrating between these states.
9. A separate training session has been planned to train the Mithanins (ASHA) & Anganawadi
workers, who play a role of DOT providers. Planning also has been done to train AYUSH &
RMA (Rural medical assistants)
10.Establishement of Sputum collection centers in difficult to reach area in tribal blocks.
11. Planning has also been done to provide the honorarium to the Cured / Treatment completed
TB patients & transportation assistance to the Tb patient on Treatment, as per the Tribal action
plan under RNTCP.
12. Five two wheelers are out of order, which have to be replaced & procured.
CHALLENGES:
1. Quality of ImplementationEstablishment of fully functional STDC at State level is essential for monitoring quality of
implementation of the programme in the State. STDC is also essential to carry out the training
activities. The posts of Epidemiologist, Medical Officer, Lab Technician, DEO cum Statistical
Assistant are to be sanctioned on a contractual basis.
2. Strengthening IRL (Intermediate Reference Laboratory) : To provide services for the Drug
Resistant TB (MDR TB)cases. State requires additional funds for strengthening the
infrastructure of IRL, under following heads:
1. Electrification: Rs.2 Lakhs
2. Repair of leaking Roof: Rs.3.41 Lakhs
3. Cold Room & Incubation room: Rs.10.00 Lakhs
4. A.C - Rs.2.6 Lakhs
5. Computer, FAX, Photocopier – Rs.1.20 Lakhs
6. Generator – 100 KB – Rs.16.00 Lakhs
7. Fuel for generator- Rs.3.00Lakhs
NRHM PIP 2009-10: Chhattisgarh
Page 390
8. Vehicle –Rs. 5.50 Lakhs
9. Civil work / Drainage system – Rs. One Lakh 10. Lab Materials - Rs.2.5 Lakhs
11. Furniture – Rs.50,000/12. Stationery – Rs. 50,000/-
PRIORITY DISTRICTS for RNTCP:
Name of the priority districts
Activities planned
Bastar,
Cure rate & case detection low
Dantewada, Jashpur
establishment of sputum collection
centers
Involvement of Private hospitals.
Special IEC activities in local
language.
Training of AYUSH & RMAs in
RNTCP.
Filling up of Vacant posts
Training of general health staff
Sensitization of PRIs
Raigarh, Surguja,
Koriya Janjgir ,Kawardha
Budget summary
Sr.
No.
Category of Expenditure
Budget estimate for FY 2009 2010
1
Civil works
30,68,400
2
Laboratory materials
48,37,702
NRHM PIP 2009-10: Chhattisgarh
Page 391
3
Honorarium
24,34,150
4
IEC/ Publicity
28,10,975
5
Equipment maintenance
14,94,000
6
Training
52,51,864
7
Vehicle maintenance
35,50,000
8
Vehicle hiring
50,59,800
9
NGO/PP support
51,88,100
10
Miscellaneous
40,80,102
11
Contractual services
3,13,63,272
12
Printing
33,29,502
13
Research and studies
-
14
Medical Colleges
18,50,100
15
Procurement –vehicles
2,50,000
16
Procurement – equipment
1,90,000
17
a.
7,47,57,967
18
b. Total ( Tribal annual action plan- copy
enclosed)
75,82,040
19
Grand Total (a & b)
8,23,40,007
Total (General annual action plan)
NRHM PIP 2009-10: Chhattisgarh
Page 392
Annexure
NRHM
Sl.
No
Unit Description
Unit cost
No. Of Units
Duration
Total Cost
Venue
Part A-FP
1
Training of Doctors on
LTT @ 3MOs/Batch
25000
10
1
250000.00
State LTT training
Centre & District
Hospital ,Bilaspur
Part A-FP
2
Alternative method for
IUCD Insertion for
ANM and LHVs
5140 ANMs, 749 LHVs,350 staff nurses
1
12000000.00
SIHFW for TOT &
Districts for further
training
Part A-FP
3
Sensitizing workshop
for TOT + logistic for
CNAA
1000
48
1
50000.00
SIHFW/ DHS
Part A-FP
4
One day training +
Printing of training
material for CNAA
5000
146
1
730000.00
District Health
Society/CMHO
Part A-MH
5
Training In EmOC &
Em Anaesthesia
Part A-CH
6
IMNCI training (11
days ) of Medical
officers
512750
17 batches of 26
participants each
11
8716750.00
SIHFW/District
training Centres
Part A-CH
7
Training of doctor
(inclTA/DA/Material)for
execution of Bal
Suposhan Kendra
3000
20 doctors
3
18000.00
SIHFW/UNICEF
Part A-CH
8
Training of Health
Workers revised
diarrhea management
(Zinc + Lo ORS) in all
districts
150
7239
??
1085850.00
District Level
16939500.00
NRHM PIP 2009-10: Chhattisgarh
Page 393
Part A
9
Training and exposure
visit to other places (
state /districts) under
BCC/IEC
25000
Part A
10
Training Activity As per SIHFW- PIP 2009-10 ( refer Annex.For details
Part B
11
Orientation workshop of
JDS
20000
146
Part B
12
Sponsorships for 1000
student for 18 months
diploma course, course
fees, food, hostel and
study material
(Alternative Nursing
Staff)
100000
Part B
13
Training of RMAs (post
induction training)
251250
Part B
14
Training and regular
support for the
strengthening of 60,000
Mitanins
Part B (
Ayush)
15
Training of AYUSH
doctors for Essential
Maternal and Child
Health Training
100000
10
Part B (
Ayush)
16
Training of AYUSH
doctors for public
Health Management
150000
Part B (
Ayush)
17
Workshop for Dist
Ayurveda officer/State
implementers and
500000
NRHM PIP 2009-10: Chhattisgarh
50
-
1250000.00
11876600.00
SIHFW
_
2920000.00
SIHFW
1000
18 months
100000000.00
ANMTCs
40
3 months
10050000.00
SIHFW/DTCs
204014000.00
SHRC
12 days
1000000.00
SHRC/AYUSH Deptt.
1 batch of 40
doctors
5 days
150000.00
SHRC
1
3days
1500000.00
SHRC
Page 394
External experts
Part B (
Ayush)
18
Training of AYUSH
physician for AYUSH
Mainstreaming
50000
15
8 days
750000.00
SHRC
Part B (
Ayush)
19
Anganwadi workers
35,000
2
125
8750000.00
SHRC/AYUSH dept.
at block level
20
Training material
35,000
Part B (
Ayush)
21
Training Compounders
for medicine
preparation , storage
and dispensing
75,000
Part C (
Immunisation)
22
District level orientation
training for 2 days
ANM, Multi Purpose
Health Worker (Male),
LHV, Health Assistant
(Male / Female), Nurse
Mid Wives, BEEs &
other specialist ( as per
RCH norms)
Part C (
Immunisation)
23
Three day training of
Medical Officers on RI
using revised MO
training module
1(Unit Cost)
1750000.00
4 days
750000.00
SHRC/AYUSH dept.
at block level
As per revised RCH norms
for trainings, copy attached
= Rs 450/-* 2*
(4800ANM+
2514MPW(M) +
749LHV+146 BEE)
7388100
District Level
Resource Person
=274batch* 2day* Rs
600/-
328800.00
Venue Hiring Charges
=274batch* 2day* Rs
8000/-
4384000.00
As per revised RCH norms,
copy attached
=Rs 450/- *
*3*(1382)
1865700
Resource Person
=41 batch* 3day* Rs
1000/-
123000
NRHM PIP 2009-10: Chhattisgarh
10
50(per module)
Page 395
TOT at
SIHFW/District Level
Part C (
Immunisation)
Part C (
Immunisation)
Part C (
Immunisation)
Part D
( RNTCP)
24
25
26
27
Venue Hiring Charges
=41batch* 3day* Rs
8000/-
984000.00
As per revised RCH norms ,
copy attached
=Rs 450* 16
7200
Resource Person
= 1 batch * 1 day*
Rs1000/-
1000
Venue Hiring Charges
=1batch* 1day* Rs
10000/-
10000.00
One day Cold Chain
handlers training for
block level cold chain
handlers by State and
District Cold Chain
Officers and DIO for a
batch of 15-20 trainees
and three trainers
As per revised RCH norms,
copy attached
=Rs 450/* (146
Block)
65700
Resource Person
= 8 batch * 1 day* Rs
1000/-
8000
Venue Hiring Charges
=8batch* 1day* Rs
8000/-
64000.00
One day Training of
block level data
handlers by DIO and
District Cold chain
Officer to train about
the reporting formats of
Immunization and
NRHM
As per revised RCH norms,
copy attached
Rs 450/- * 146 blocks
65700.00
Resource Person
= 8 batch * 1 day* Rs
1000/-
8000
Venue Hiring Charges
=8batch* 1day* Rs
10000/-
80000.00
One day refresher
training of District RI
Computer Assistants on
RIMS/HMIS and
Immunization formats
under NRHM
Annual Training Of
Medical & Paramedical
Staff
NRHM PIP 2009-10: Chhattisgarh
State Level/SIHFW
District Level
5251864.00
Page 396
District Level
State & District Level
28
Part D (
NVBDCP)
Part D
(
NVBDCP)ELF
29
2.1 Medical Specialist
at District Hospital
20000
16 Batches
320000.00
2.2 Medical Officer
15000
35 Batches
525000.00
2.3 Laboratory
Technicians (Induction)
10000
20 Batches
200000.00
2.4 Laboratory
Technicians (Reorientation)
10000
20 Batches
200000.00
2.5 Health Supervisors
(M)
10000
10 Batches
100000.00
2.6 Health Supervisors
(F)
10000
16 Batches
160000.00
2.7 Health Worker (M)
10000
115 Batches
1150000.00
2.8 Health Worker (F)
10000
100 Batches
1000000.00
2.9 ASHA Training in 4
quarters
3000
8000 Batches
24000000.00
2.10 Community
Volunteers other than
ASHA
10000
20 Batches
200000.00
2.11 Other Specify
(Spray Squads) 400
Squads
10000
8 Batches
80000.00
Training and Capacity
Building for different
tiers of Health
Personnel under ELF
NRHM PIP 2009-10: Chhattisgarh
Page 397
Part D
(NLEP)
30
2 days Training for
District Level Officers
2 days Training for District
Level Officers
40000.00
1 batch in each district
MO- PHC
1 batch in each district MOPHC
279000.00
1 batches in each
district Para medical
staff
1 batches in each district
Para medical staff
800000.00
1 batches in each
district Drug
Distributors
1 batches in each district
Drug Distributors
800000.00
Technical & IEC
training for MO (Rural)
– 04 days
700
23
29.8
685000.00
Technical & IEC
training for MO
(Urban) – 04 days
200
7
29.8
209000.00
Re-orientation training
of Medical Officer - 02
days
1650
55
17.3
952000.00
Technical & IEC
training for Health
Supervisor (M&F) – 03
days
700
23
16.3
375000.00
Technical & IEC
training for Health
Worker (M&F) – 03
days
2200
73
14.05
1026000.00
Laboratory technicians
training – 05 days
146
5
24.1
121000.00
NRHM PIP 2009-10: Chhattisgarh
Page 398
RLTRI ,Raipur
Part D
(NPCB)
Part D
(IDSP)
31
32
1. training of
Ophthalmic nurse and
Ophthalmic assistant
2000
500
10000.00
2. training of DPM
3000
18
54000.00
Training of community
health volunteer
0.002
60000
12000000.00
Training of ANM and
AWW
0.0013
35000
4550000.00
1 day's orentation of
CMHOs & CSs of state.
2,500
36
90000.00
State
1 day's refresher
training of BEE / Multi
Purpose Supervisors /
Multi Purpose Workers
650
7200
4680000.00
District / Block
3 day's training of
Peripharal Lab. Teach.
/ Lab. Assistants.
1,200
270
324000.00
District
1 day's Workshop of
MOs of District
Hospital - Raipur,
Durg, Bilaspur &
Raigarh.
1,200
45
54000.00
District
3 day's training of
Medical Officers.
2,000
450
900000.00
District
6 day's training of Lab.
Technicians.
3,500
35
122500.00
State
NRHM PIP 2009-10: Chhattisgarh
Page 399
SIHFW/Directorate