Medical - West Lancs Scouts
advertisement

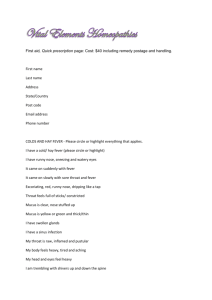
WEST LANCASHIRE COUNTY SCOUTS Overseas Leaders’ Medical Pack In the world of global communication we believe all trip medics should have access to an empathetic, experienced Doctor. Satellite communication is difficult at times however good communication and sound emergency response plans are the core tenets of our operations and training. In a wilderness setting prevention is better than cure. So the message is plan early and phone a friend! Please return to the ACC(Expeditions) after use. These notes have been reproduced by kind permission of Wilderness Expertise Ltd, The Octogon, Wellington College, Crowthorne, Berkshire RG45 7PU (01344 744 430). They are copyrighted and provided specifically for use by Leaders of Overseas Ventures operated by West Lancashire County Scouts and no further reproduction is permitted. Wilderness Expertise can accept no liability for the contents or for any advice herein. 1 Overseas Leaders’ Medical Pack These notes are designed to work alongside your first aid training, and to extend that training and experience in order to preserve life in a remote setting if communication is not possible with your own 24hr support doctor, local medical facilities, or insurance company doctors. The basic principle of first aid must always apply: DO NO HARM Section 1. Guidance on use of medications 2. Acute mountain sickness 3. Dehydration 4. Diarrhoea 5. Ear infections 6. Urinary tract infections 7. Allergic reactions – Anaphylaxis 8. Malaria 9. Heart conditions 10. Psychological considerations 11. Medical evacuations 12. Expedition mortality 13. Post traumatic stress 14. Notes on medications 15. Post expedition health brief 16. Patient treatment 17. Report cards Page 3 4 7 9 12 13 14 16 19 21 22 23 24 27 37 38 40 Key points gain qualified medical advice as soon as practical. Refer to your Critical Incident Plan for all cases of medical treatment, a log of all findings, activities and medication used must be recorded all medications must be secured from theft and misuse. Keep medications cool, dry and out of direct sunlight. Updated by Peter Harvey & Dr Matt Ladbrook Approved by Dr Caroline O’Keeffe, June 2007 2 1. Guidance on Use of Medications Supportive care including rest, hydration and a good diet will enable the patient’s immunity to fight infections. This is the best road to health. Medications should be used as a secondary measure and the benefits weighed up against the side effects. Non-prescription medications On expedition, non-prescription medications should not be given to minors (<18 yrs) without medical approval. Participants may bring their own medications. However it is important to get a full picture by asking for details. Prescription medications On expedition, prescription medications should only be given under the direct or indirect control of a doctor. The insurance contact number supplied is manned 24 hours a day by a doctor who can advise on emergency treatment. For non-emergency treatment, contact the on-call team who will obtain medical advice and contact you with clarification on the appropriate treatment. When medical advice is unobtainable, this MELP is here to guide you until you are able get medical assistance. In these situations the MELP must be adhered to at all times and the Leader must not give treatment he or she has not been trained to give. The specific medical kit, which comes with these notes, is tailored to your activities, group and destination. Summary Keep it simple: rest, oral hydration, food; Medications have side-effects, ensure benefits outweigh risks; Check correct indication for use of medication, allergies, side effects, dosage, expiry date; Stop if a rash or serious side effect develops; Record all treatment and medication use. 3 2. Acute Mountain Sickness (AMS) AMS is a spectrum of illness, ranging from mild symptoms to life-threatening conditions. AMS is caused by going too high, too fast. Few people get AMS below 2400 m. Mild AMS is common and usually self-limiting. Symptoms classically appear 12-24 hours after arrival at altitude. Mild symptoms will usually subside after 72 hours at altitude. Symptoms include: headaches; undue fatigue or shortness of breath; loss of appetite, nausea and/or vomiting; dizziness; difficulty sleeping. Note: symptoms may be worse when sleeping. Mild AMS may progress to more serious HAPE or HACE (see below). However, some patients will develop HAPE or HACE without having displayed symptoms of mild AMS. Prevention acclimatise: above 3000m ascend only 300m a day and rest every third day; remember: ‘climb high, sleep low’; diet: extra fluids, light carbohydrate-rich diet. Treatment DESCEND - DESCEND - DESCEND! avoid heavy exertion; light activity preferable to complete bed rest; absolutely no smoking or alcohol; consider giving Diamox. Climbing is not about the peak - it is about enjoying the journey. People will not enjoy the experience if they are unwell and in pain. Go down - the mountain will be there another time. 4 High Altitude Pulmonary Oedema (HAPE) In this condition, fluid accumulates in the lungs, commonly 2 - 4 days after arrival at altitude. The risk of developing HAPE after a rapid ascent to 3600m is approximately 1 in 200. An important first warning sign is a party member who is more tired than the others. Symptoms worsening shortness of breath, progressing to shortness of breath at rest; dry cough, may produce frothy, pink phlegm; fatigue progressing to unconsciousness; bluish tinge to lips and extremities. Note: symptoms may worsen rapidly at night Treatment DISCUSS WITH ON CALL TEAM sit patient upright; give oxygen and use a hyperbaric chamber, if available; consider giving Nifedipine; descend (unladen) patient without delay and seek medical help. A descent of even 600 m can offer prompt relief. High Altitude Cerebral Oedema (HACE) This condition affects some people as low as 3500m. It is caused by fluid accumulating in the brain tissues. Symptoms severe headache; vomiting and dizziness; visual disturbances, altered eye movements; poor co-ordination and confusion; drowsiness and coma. Treatment DISCUSS WITH ON CALL TEAM descend without delay & seek medical help; give oxygen and use a hyperbaric chamber, if available; consider giving Dexamethasone. 5 Lake Louise Self Assessment Scoring for AMS This simple self-assessment scoring system can help determine whether or not an individual may have AMS. Because all scoring systems tend to over diagnose AMS, scores should be interpreted in light of recent altitude gain and should take allowance of any background illness. Recent ascent AND headache AND other symptom(s) AND a total score of 4 or more suggests AMS. People can become hypochondriacs. A key element is getting honest feedback from the team. Do not rely on this one tool alone. If in doubt call for a consultation. Symptom Headache Gastrointestinal Fatigue/ weakness Dizziness/ lightheaded Difficulty Sleeping Overall, affect on activities? Severity none at all mild moderate severe/incapacitating good appetite poor appetite or nausea moderate nausea or vomiting severe nausea or vomiting not tired or weak mild moderate severe None mild moderate severe/incapacitating slept as well as usual did not sleep as usual woke many times could not sleep at all not at all mild reduction moderate reduction severe reduction (bed rest Score 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 0 1 2 3 Adapted from the Proceedings of the 7th International Hypoxia Symposium, Lake Louise, Canada, 1991. 6 3. Dehydration Dehydration is a common, avoidable condition. It is potentially serious in its own right and also worsens other conditions. Preventable heat-related deaths occur on expedition each year. Under normal conditions, individuals require around 35 ml of water per kg weight per day – this equates to approximately 2.5 L per day for a 70 kg man. Normally around two thirds of our daily need is met by drinking, the remainder comes from water contained in our food. When an individual is drinking sufficient water, they produce plenty (at least 1.5 L a day) of pale, straw coloured urine. Indicators of dehydration are: thirst small volumes of dark urine headaches, dizziness, nausea other signs: sunken eyes, dry mouth, loss of skin elasticity measure pulse and BP (low BP + high pulse suggests dehydration) High temperatures, physical activity, fever, diarrhoea and vomiting all dramatically increase water needs. Prevention educate and set a good example; anticipate daily water requirements; don’t wait until you’re thirsty; monitor drinking using a ‘buddy-buddy’ system; make water readily available; drink from 1 L bottles to aid measurement; individuals should monitor the colour of their urine. 7 Treatment Fluid lost by normal sweating can be replaced by drinking water and ensuring some salt is eaten with food. Excessive sweating, vomiting and diarrhoea cause the body to lose significant amounts of water and salts. In this case, rehydration can be achieved with isotonic drinks such as Dioralyte (a solution made from powder containing water, salts and glucose, see Section 11). Isotonic solutions are absorbed more quickly than water. Rehydration should aim to replace fluid that has been lost: 200 - 400 ml of Dioralyte for each vomit or loose stool is reasonable. Fluid should be taken in frequent, small volumes over 3 - 4 hours, after which the patient should be reassessed. Following this, normal fluids are used to meet the daily requirements and Dioralyte for further losses from vomiting or diarrhoea. Replacement needs are entirely dependent on the amount of fluid and salt lost. In the field, the best rule of thumb is that the patient drinks enough to produce good volumes (1.5 L/day) of pale coloured urine. Home-made isotonic drink can be made by mixing: 1 L sterilised water 12 level teaspoons (40 g) of table sugar 1 level teaspoon (5 g) of table salt Dispose of any unconsumed drink after 24 hours. Fluid and salt can also be replaced by consuming soup, broth and fruit juice – though specific rehydration liquids are probably quicker. Dehydration is hastened by diuretics such as alcohol, tea, coffee and carbonated soft drinks with caffeine these cause the body to lose water. 8 4. Diarrhoea Diarrhoea is the most common traveller’s illness, affecting a third of visitors to developing countries. Whereas mild diarrhoea is simply a nuisance, severe diarrhoea can be life-threatening. Loose Stools are defined as soft, unformed stools with 3 - 4 bowel movements a day. This is not true diarrhoea. Common causes are a change in food or water, medication side-effects (e.g. antibiotics), anxiety or excitement. May last for days or weeks but usually resolves without treatment. Loose stools, which persist after returning home, should be investigated. An individual passing multiple liquid stools should be classed as having diarrhoea. Identifying whether the diarrhoea is invasive or non-invasive (tricky in field), allows appropriate treatment to be followed. Non-invasive diarrhoea These cases are caused by organisms that secrete toxins into the contents of the gut. most common type of diarrhoea usually less serious (except cholera) commonly via faecal contamination of water incubation is usually 12 - 48 hours Infection lasts usually 2 - 5 days Non-invasive diarrhoea is often associated with intermittent abdominal cramps, nausea and vomiting. There may be mild lower abdominal tenderness. Chills and fever are usually mild or absent. With the exception of cholera, non-invasive diarrhoea should not be treated with antibiotics – they are usually ineffective and can predispose sufferers to invasive diarrhoea. Generally, anti-diarrhoea medications (e.g. loperamide) are not recommended – but may be useful to help control severe abdominal cramps or to facilitate patient transport. 9 Invasive diarrhoea (dysentery) These cases are caused by organisms that invade the lining of the gut and can spread throughout the body. Cases are most common in tropical or semi-tropical climates. Average incubation is 48 hours, but could be anywhere from 12 hours to 5 days. Symptoms are the same as non-invasive diarrhoea, with the addition of: chills and fever pus, blood or mucus in the stools (commonly 4 - 5 hours after onset) the patient appears ill Note: symptoms may vary widely between individuals. These cases should be evacuated to medical care and treated with antibiotics. Choice of antibiotic depends on the causative agent. Try to discuss this with the Doctor on call if at all possible. Patients should be barrier-nursed by one or two nominated individuals who are scrupulous about their hygiene. Faeces and vomit must be disposed of where it poses no risks to water or to people. Infected equipment should either be boiled or aired in bright sunlight for two days. The use of anti-diarrhoea medications only prolongs and aggravates this type of diarrhoea. Taking a history Getting good details prior to calling for advice saves time. This is a huge help in determining the type, cause and progress of the infection. Knowing what an individual’s ‘normal’ bowel habit is can be useful! When did the diarrhoea start? Stool: number, colour, consistency, smell and volume? Any mucus, pus or blood present? Associated symptoms: fever, nausea, abdominal pains? How many people affected? Recent fluid and food intake? 10 Examination general impression (ill or not ill?) check vital signs (pulse, BP and temperature) assess for dehydration General treatment for all diarrhoea Essential treatment for vomiting and/or diarrhoea is replacement of water and salt (see Section 3). Nausea and vomiting may be treated with prochlorperazine (see Section 11) if the tablets can be kept down. Consider suppositories? Hot water bottles can help with abdominal cramps. Paracetamol (see Section 11) is good for fever and discomfort). Fasting does not help – food should be taken if tolerated. Stick to a bland diet of complex carbohydrates (potatoes/pasta/rice). Avoid dairy products. Prevention strict hand-washing, including nail-scrubbing even more critical once a case of diarrhoea exists in the group sterilise all drinking water – even for brushing teeth sterilisation by bringing water to a rolling boil, regardless of altitude, kills all organisms that cause diarrhoea sterilisation with iodine/chlorine kills most organisms except some parasitic agents (cryptosporidia and cyclospora) which can be removed by filtration bottled drinks with intact seals are safe other drinks and food should be boiled on first cooking reheating previously undercooked food will not make it safe to eat self-peel fruit and vegetables and use straight away sterilisation of water used in food preparation sterilise cooking utensils avoid contact with all animals avoid seafood and unpasteurised milk 11 5. Ear Infections Ear infections are common in childhood, but uncommon in adulthood. 50% of cases of painful ears are due to pain being referred from another problem – commonly throat or tooth infections or neck muscle problems. Ear infections affect the ear, hearing canal (outer ear) or the inner hearing apparatus (middle ear). Outer ear infection (‘Swimmer’s ear’) common, more so in adults often due to damage by fingernails, irritants or wet conditions symptoms include: itching, pain and inflammation of the skin, slight discharge, tenderness when the ear is gently pulled treat with gentle, dry, non-invasive cleaning twice a day pain killers and dry warmth help symptoms antibiotics not useful unless there is spreading skin infection or boil. Middle ear infection often follows viral upper respiratory infection symptoms: sudden onset pain, sometimes fever, loss of appetite, vomiting and deafness eardrum perforation may be followed by a large discharge of pus and relief from pain (discharge usually settles after 48 hours) wash as above if there is discharge pain killers and dry warmth help symptoms most uncomplicated cases resolve on their own. Consider amoxicillin (see Section 11) if patient is unwell or no better after 72 hours consider antihistamine (e.g. chlorphenamine, see Section 11), if associated with hay fever 12 6. Urinary Tract Infections Cystitis Cystitis is caused by inflammation of the bladder. Main symptoms are: burning sensation on urination frequent and urgent urination The urine may contain some blood. Fever and other symptoms are rare. Symptoms usually resolve in 2 - 3 days. Severe or longer-lasting symptoms, or fever, require treatment with antibiotics. In all cases, double normal fluid intake helps recovery. Cystitis is common in females, but rare in males. Male patients should see their GP on return. Pyelonephritis Infection involving one or both kidneys, characterised by: sudden onset high fever with chills pain over the kidney the patient often looks and feels ill symptoms of cystitis are common slight to moderate bleeding may occur tenderness when gentle pressure is applied to the side of the backbone, just below the lowest rib on the affected side Treatment involves doubled fluid intake and antibiotics (see Section 11), but this condition requires evacuation, medical supervision and intravenous antibiotics. 13 7. Anaphylaxis Anaphylaxis is a serious allergic reaction that can be fatal. The use of an EpiPenand Antihistamine can save the patients life. EpiPenis a device designed to automatically inject adrenaline (or epinephrine) into the muscle of the thigh to treat severe allergic reactions. It is designed to be carried by people who are at risk of anaphylactic reactions and should be carried by them at all times. EpiPencan cause problems in people with heart disease, diabetes, thyroid problems and high blood pressure however if an anaphylactic reaction is confirmed then it is necessary to give it. The oral Antihistamine tablets provides a delayed (>30min) treatment to an anaphylaxis reaction. Signs and Symptoms Minor Itching Rash Flushing Headache Nausea Severe Vomiting Abdominal cramps Light headed / dizzy Swelling lips, throat, tongue, hands & feet Wheezing Coughing / Shortness of Breath Unconsciousness If a patient is developing symptoms of severe allergy: 1) Contact the on-call number immediately for medical advice: The Co-ordinating Medic on duty will assess the situation and provide treatment instruction. If it is not possible to access Doctor’s advice, proceed to step 2: 2) Give a standard dose of antihistamine in tablet form orally to the patient 3) Observe the response and if severe allergy signs and symptoms continue move to step 4. 14 4) Give EpiPeninjection (full directions in the pack) Take EpiPenauto-injector out of the pack Pull off the grey safety cap Hold Auto-injector against the thigh with the black tip against the skin Press Auto-injector hard against the thigh to trigger Auto-injector mechanism Hold against thigh for 10 seconds after triggered Remove Auto-injector Massage injection site for 10 seconds Discard Auto-injector safely 5) Proceed according to advice given by Doctor. EpiPen Storage Where possible, store the EpiPenaccording to the directions on the box, i.e. below 25°C. This is obviously not practical in many field situations however the EpiPenhas been demonstrated to work effectively in temperatures of around 40°C so it can safely be carried in a field backpack. EpiPenshould not be stored in a vehicle as this may lead to prolonged periods of excessive temperatures which may reduce the effectiveness of the EpiPen. 15 8. Malaria Malaria is mainly a disease of the tropics and subtropics, but is the world’s most common infection. It causes approximately 1 million deaths a year, mostly in children in sub-Saharan Africa What is malaria? Malaria is an infection caused by a protozoan parasite, which is spread by the bite of infected mosquitoes. There are 4 types of malaria: ovale, vivax, malariae and the most serious, falciparum. Prevention The best way to avoid malaria is not to get bitten in the first place! These physical measures include: use an insect repellent, preferably one containing 50% DEET (diethyltoluamide) keep covered up with long-sleeved shirts and long trousers when mosquitoes are feeding at dawn and dusk sleep in a properly screened room or tent and use a 'knockdown' spray to kill any mosquitoes in the room consider washing nets and clothes in the chemical permethrin to deter mosquitoes check nets for holes and tuck them in well The second method is to take a chemical prophylactic: before travelling, obtain medical advice on which prophylactic medication to use take your anti-malarial tablets regularly as directed and finish the course Unfortunately, none of the precautions above will give absolute protection. 16 Symptoms Symptoms of malaria are notoriously variable (the disease is sometimes called ‘The Great Pretender’), however, a classical time course is as follows: 6 – 10 days post bite: muscular soreness and low fever after another 4 – 8 days a fever develops, but the patient feels cold and shivers 1 hour later: patient feels very hot, is flushed, may have headaches, may be delirious 2 hours later: drenching sweat develops and the temperature falls. Severe head, back and muscle aches may occur The following symptoms suggest severe malaria: vomiting and/or diarrhoea dark urine shock unconsciousness KEY POINTS: Consider malaria in any patient with a fever who has visited a malaria-affected region. The repeated occurrence of fever is the classical hallmark of malaria. Treatment You should start anti-malarial treatment if a team member develops two of the symptoms listed above even if they think they have not been bitten. If at all possible, you should try to get a medical opinion (e.g. by telephone) before starting treatment. It is vital that you get medical attention at the earliest opportunity, even if the individual begins to feel completely well again. Suspected patients should be encouraged to rest and take adequate oral fluids. Paracetamol is useful for pains and fever. 17 If medical help is not available within 8 hours of the onset of symptoms and you suspect malaria, stop any tablets you are taking to prevent malaria and then follow the following regime: CoArtem (Artemether 20mg + Lumefantrine 120mg) Take four tablets initially, followed by 5 further doses of 4 tablets, each given at 8, 24, 36, 48 and 60 hours Total – 24 tablets over 60 hours Ideally, CoArtem should be taken with milk or a fatcontaining food. Because of the many possible complications of treatment, it is vital that patients receive proper medical attention. Alternative Treatment for patients not taking malarone as a prohylaxis: Malarone (Atovaquone hydrochloride 100mg) 250 mg + Proguanil Take four tablets once a day for 3 days Total – 12 tablets On return Because malaria can cause such varied symptoms, any flu-like illness up to a year after travelling to a malaria containing region should be investigated. Always mention to your doctor that you have travelled to a malaria affected region. 18 9. Angina and Heart Attack The signs and symptoms of cardiac emergencies include chest pain, shortness of breath, fast and slow heart rates, fast breathing, ashen grey skin colour and confusion. Angina If there is a history of angina the patient will probably carry glyceryl trinitrate (GTN) spray or tablets and he/she should be allowed to use them. Where symptoms are mild and resolve rapidly with the patient’s own medication, emergency evacuation is not normally necessary, however the patient should see a doctor as soon as possible. For more severe attacks of chest pain, angina attacks which seem to be worsening or coming more frequently, or where there is a loss of consciousness, emergency evacuation should be initiated straight away. Heart Attack The pain of heart attack is similar to that of angina but generally more severe and prolonged. There may only be a partial response to the patient’s medication (GTN). Patients experiencing chest pain with no previous history of angina should be assumed to be having a heart attack. Signs and Symptoms of Heart Attack Progressive onset of severe, crushing pain in the centre and across the front of chest. The pain may radiate to the shoulders and down the arms (more commonly the left), into the neck and jaw or through to the back Skin becomes pale and clammy Nausea and vomiting are common Pulse may be weak Shortness of breath 19 Initial management of Heart Attack Call immediately for an ambulance (if available) or initiate urgent evacuation. Fetch an AED (defibrillator) if available. Allow the patient to rest in the position that feels most comfortable; in the presence of breathlessness this is likely to be the sitting position. Patients who faint or feel faint should be laid flat; often an intermediate position (dictated by the patient) will be most appropriate. Help the patient to take their GTN spray/tablet (if available). Reassure the patient as far as possible to relieve further anxiety. Give aspirin in a single dose of 300 mg orally, crushed or chewed. Record the time and dose, and pass this information on to emergency medical personnel. If the patient becomes unresponsive Open the airway. Check for breathing. In the absence of normal breathing start CPR (ignore occasional ‘gasps’). Give compressions and ventilations at a ratio of 30:2. If an AED is available, follow the machine’s instructions. CPR should continue for up to 30 min, unless the team is exhausted, in danger or relieved by a more competent team, in which case they should stop. 20 10. Psychological Considerations An expedition is a stressful time for individuals and providing emotional support is critical. This support comes from many sources however as a medic you need to ensure patients are supported. Contentiously – happy people have fewer incidents. Therefore part of caring for people is the emotional and physical support. Breaking Bad News During expeditions bad news may come to the participants via telephone or email (e.g. exam results, bereavements). Ideally, this information will come via you to enable you to deliver the news appropriately. Plan how you intend to structure the discussion. Be straight – you can’t make bad news good news. Formulate answers to likely questions. Consider possible consequences – can the student go home? Rest the group and deliver the news in a place where everyone can have some space. During the discussion be prepared to listen. Allow enough time to talk. Ask the person involved about informing the group. The group should be told as close friends will be the best support. Inform the person involved first, do not allow the information to leak out. Psychological Conditions There are an increasing number of conditions from eating disorders, depression to self-harm. Do not think that the right words or intervention can resolve these complex conditions during an expedition. Expedition members should be observed for mood swings and irrational behaviour however no single sign or symptom can be used to diagnose conditions. On expedition any psychological concerns should be raised with the On-Call Doctor and patients should be observed. Interventions should only be supportive care and to protect the group and patient from harm. 21 11. Medical Evacuations If you are questioning whether to evacuate on a trauma site the answer is probably “yes“. If you are in doubt, evacuate. However, in some circumstances (difficult terrain, poor helicopter access, poor weather, etc) it may be necessary to bring emergency medical aid to the patient. The group comes first and sometimes an evacuation will need to be stopped for the safety of the group. When to evacuate: The following medical signs and symptoms are sure signs that you should initiate the evacuation: Sustained or progressive deterioration; Debilitating pain; Unable to sustain travel; Passage of blood via mouth or rectum. Signs & symptoms of serious high altitude illness; Progressive infection even with correct treatments; Chest pain, not linked musculoskeletal origin; Psychological illness effecting safety. How to evacuate: Full details of the evacuation will be found in the Expedition Leader Pack and the Emergency Response Plan. For medical cases ensure the patient is well packaged and is comfortable. Ensure frequent stops to reassess vital signs. Monitor the group – evacuations are emotionally and physically draining. Watch out for the next injury / incident. 22 12. Expedition Mortality Sometimes things happen that are beyond our control. In remote settings this can sometimes be fatal. With the best will in the world, things do go wrong. When dealing with a patient, one of the most difficult decisions to make is when it is best to stop treatment or halt the evacuation. The following guidelines will help to clarify the situation: Stop if other members of the group are in danger 30 min CPR has been unsuccessful Pronouncing death This can only be done by a doctor. However, in the wilderness, the following signs taken together suggest that the patient has died: patient is totally unresponsive pupils are widely dilated and do not respond to a direct, bright light for 15 seconds no detectable breath sounds for 3 mins no pulses or heart beat detectable for 1 min purple marking on lower parts of body as blood sinks injuries incompatible with life Note: Pulses, breathing and heart sounds may be very difficult to detect in a patient with severe hypothermia. If in doubt, re-warm. “A patient isn’t dead until they are warm and dead” Action record all information inform local Police photograph location and patient’s body do not move the body without police approval inform Home Contact –support will fly out (counsellor / doctor) discuss the situation with the group 23 13. Post Traumatic Stress (PTS) PTS is a normal reaction of normal people to an abnormal situation. Causes – some examples team individual or young child dies multiple casualties Types acute: within 1 - 2 days, remove group from situation and observe delayed: within 3 weeks, personality changes, habits, sleeping problems chronic: as delayed, but extended time period Signs sleep disturbance appetite disturbance nightmares denial Drug dependence (smoking and alcohol) Associated issues new friendships / relationships may develop existing relationships might be strained, leading to tension or conflict you may feel that you can’t give as much as expected accidents more common after severe stress alcohol and medication intake may increase Common feeling associated with PTS Crisis shows up human weaknesses as well as human strengths. Common feelings and emotions are: Numbness: the event feels unreal, like it never happened the misfortune may only be felt slowly there may be denial of what has happened Numbness may be misconstrued as ‘being strong’ or ‘uncaring’. 24 Fear of: damage to oneself and those we love being left alone, of having to leave loved ones breaking down or ‘losing control’ a similar event happening again helplessness Sadness for deaths, injuries and losses of every kind Longing for all that has gone. Guilt: for being better off than others, surviving, not being injured, for still having material things regrets of things not done Anger: at what has happened. at whoever caused it or allowed it to happen. at the injustice and senselessness of it all. at the shame and indignities. at the lack of proper understanding. why me? Memories of feelings, of loss or of love for other people in your life who have been injured or died at other times Disappointment for plans that can now not be fulfilled. Hope for the future and better times. Everyone may have these feelings. Experience has shown that they may vary according to circumstances. Nature heals by allowing these feelings to come out. This will not lead to loss of control - but stopping these feelings may lead to other problems. 25 Managing PTS Activity: Helping others may give you some relief. Reality: Facing the reality by attending funerals, inspecting losses and returning to the scene will all help you to come to terms with the event. Support: It can be a relief to receive other people’s physical and emotional support. Sharing with others who have had similar experiences can help. Privacy: In order to deal with feelings, you may find it necessary to be alone, or just with family and close friends. Do talk with fellow group members. Express emotions and let people share in the grief take every opportunity to review the experience. Do allow yourself to be part of a group of people who care take time to sleep, rest, think and be with those important to you express your needs clearly and honestly try to keep your life as normal as possible take the team to a safe location to enable the group to rest, have time alone/together with good comfort levels and support Don’t allow the group to bottle up feelings avoid talking about what happened expect the memories and emotions to go away - the feelings will stay with you for a long time to come forget that people experience similar feelings 26 14. Notes on Medications All medications have side effects and may interact with other medications. Weighing up whether the intended benefit of giving a medication is worth the potential side effects is an important consideration. Wherever possible, seek a trusted doctor’s opinion before giving a prescription medication. Always ask if the patient has any allergies to medications what other medication they are taking think whether the patient could be pregnant Be aware that medications have internationally recognised names and trade names. Trade names can vary between countries. If possible, ask for advice from a doctor before starting any medication. Antibiotics Supportive care, rest and wound care should be the primary methods to prevent infections. Antibiotics have side effects and should, when possible, be avoided. Antibiotics may affect the action of the oral contraceptive pill – patients should be warned appropriately. Amoxicillin (Amoxil) This is a commonly used penicillin. Indications: chest, urinary, ear and oral infections Cautions: penicillin allergy (around 10%) Side effects: nausea, diarrhoea, discontinue treatment if rash develops Dose: Pneumonia: 500 mg (1 g if severe), 8 hourly Middle ear infection: 500mg, 8 hourly for five days 27 Chloramphenicol An antibiotic ointment used to treat eye infections. Indications: conjunctivitis (sore, red, sticky eye) Dose: apply ointment under the lower eyelid four times daily for five days. Ciprofloxacin (Ciproxin) Indications: respiratory, skin, gastrointestinal, urinary infections Cautions: use with caution if history of epilepsy or seizures, ensure good fluid intake, avoid excessive sunlight exposure (discontinue if rash develops), do not use in children (<16) or pregnant women (risk of cartilage damage), do not prescribe with antiinflammatory medications, like brufen (Ibuprofen / Nurofen) or aspirin, as fits may occur – even in nonepileptics, may impair performance of skilled tasks e.g. driving Side effects: nausea, vomiting, diarrhoea, headache, dizziness and rashes. Dose: All indications: 500 mg, 12 hourly for 5 days Erythromycin Erythromycin is used primarily as a substitute for penicillin in individuals who are penicillin allergic. Indications: chest, skin and wound infections Cautions: do not prescribe with certain antihistamines such as terfenadine (Triludan) and astemizole (Hismanal) – cardiac arrhythmias. Side effects: occasional diarrhoea, nausea, vomiting (increased by high doses) Dose: 250 – 500 mg, 6 hourly Metronidazole (Flagyl) Indications: oral, amoebic and giardia infections Cautions: can cause severe vomiting when taken with alcohol – no alcohol for 3 days after treatment, Side effects: nausea, vomiting, unpleasant taste, rashes Dose: Giardia: 2 g once a day for 3 days. Dental infections: 200 mg 8 hourly for 3 - 7 days. Amoebic dysentery: 500 mg 8 hourly for 5 days. 28 Anti-Malarial Adult Medication Malarone Indications: prophylaxis & Treatment of malaria Cautions: Avoid use during pregnancy and Kidney diseases. Side effects: Dizziness and loss of balance Dose: Prevention: 1 tablet per day at the same time for 2 days pre, during travel in malarial area and 7 days post. Treatment: 4 x tablets once a day for 3 days Doxycycline Indications: prophylaxis of malaria Cautions: should not be given to children under 12 years (stains teeth). Do not give with milk, antacids or iron supplements, increases risk of sunburn Side effects: nausea, vomiting, oesophageal irritation Dose: 200 mg daily (as a single or as divided doses) for a minimum of 1 week Mefloquine Indications: prophylaxis of malaria Cautions: avoid during pregnancy and 3 months after, disturbed sense of balance may interfere with skilled tasks (e.g. driving) and may persist for up to 3 weeks Side effects: nausea, vomiting, diarrhoea, headache, agitation, hallucinations Dose: prophylaxis: start 2 – 3 weeks before travel; continue for 4 weeks after return. If over 45 kg 250 mg once a week CoArtem Indications: Treatment of malaria Cautions: Pregnancy, Renal Impairment, Hepatic Impairment Side Effects: Abdominal Pain, Diarrhoea, Nausea Dose: Take four tablets initially, followed by 5 further doses of 4 tablets, each given at 8, 24, 36, 48 and 60 hours. Total – 24 tablets over 60 hours 29 High Altitude Medication Acetazolamide (Diamox) This medication promotes deeper, faster breathing and may relieve some of the effects of AMS (particularly sleeping problems) in poorly acclimatised individuals. It also speeds up the process of acclimatisation. While there is considerable medical opinion regarding the effectiveness of this medication in treating AMS, the picture is not entirely clear-cut. The medication is still un-licensed in the UK for the treatment of AMS. No medication is as good as effective acclimatisation. The danger of preventative treatment of AMS is that it encourages individuals to go further than they are capable and masks early warning signs. AMS may eventually be diagnosed too late. The most rational use of acetazolamide is to assist the recovery of patients with AMS to lower altitude. Indications: emergency treatment of AMS Cautions: keep well hydrated, should not be given to those who are allergic to sulphonamide medications (e.g. septrin), with kidney or liver disease, to pregnant or breast-feeding mothers Side effects: tingling in lips, hands and feet, altered taste, blurred vision, weak diuretic effect Dose: in the presence of symptoms of AMS, 250 mg 12 hourly until below 2500 m. 30 Dexamethasone Dexamethasone is a strong steroid. At high altitude, it is used to prevent the build up of fluid in the brain (cerebral oedema) that occurs in HACE and contributes to the symptoms of AMS (see Section 2). It is as effective as acetazolamide in treating AMS, but does not promote acclimatisation. As for other AMS medications, dexamethasone is no substitute in itself for evacuation to low altitude and prompt medical attention. Indications: emergency treatment of HACE and/or AMS Cautions: evacuate as quickly as possible Side effects: severe side effects would be rare for the short period of use needed for evacuation to low altitude Dose: 4 mg, 6 hourly Nifedipine (Coracten) Nifedipine is usually used to treat high blood pressure and heart blood vessel disease. It is useful in the treatment of HAPE because it lowers blood pressure in the arteries of the lungs, thereby reducing the amount of fluid that accumulates in them. This can lower blood pressure quite dramatically so please discuss with a doctor before using. Nifedipine has a place in treating casualties with HAPE who are being evacuated to lower altitude. It is not a treatment on its own and is no substitute for descent and administering oxygen. Note that nifedipine is not officially licensed in the UK for the treatment of HAPE. Indications: emergency treatment of HAPE Cautions: avoid in patients with heart or blood vessel disease, in pregnancy, avoid grapefruit juice Side effects: The commonest side effects seen are low blood pressure, headache, flushing, dizziness and ankle swelling. Dose: 30 mg three times a day 31 Painkillers Ibuprofen (Nurofen, Brufen) Non-steroidal anti-inflammatory medication (NSAID) Indications: treatment of muscle/joint pains, period pains, fever and migraines Cautions: should not be given to patients with aspirin allergy or to those with peptic ulcers, only give to asthmatic patients if they have had the same medication before without worsening of asthma, do not give with the antibiotic ciprofloxacin Side effects: indigestion, heartburn, nausea, diarrhoea Dose: initial dose 1.2 – 1.8 g daily in 3 – 4 divided doses with or after food. Maintenance dose of 0.6 – 1.2 g daily may be adequate. Maximum daily dose is 2.4 g. The analgesic action of ibuprofen reaches a maximum after 3 days of regular therapy. Paracetamol (Acetaminophen) Non-opioid analgesic Indications: mild to moderate pain, fever Cautions: do not take with any other paracetamol containing products (e.g. cold treatments). Immediate medical advice should be sought in the event of an overdose, even if the individual feels well, because of the risk of delayed, serious liver damage. Side effects: rare Dose: 1 g 6 hourly Paracetamol / Ibuprofen combined These work well in combination and both can be taken at maximum dose. If used in combination, always use maximum Paracetamol before adding in Ibuprofen. Dihydrocodeine - Opioid analgesic Indications: moderate to severe pain Cautions: enhances effect of alcohol, may affect performance of skilled tasks (e.g. driving), avoid use with head injuries, respiratory depression Side effects: constipation, nausea, vomiting, drowsiness Dose: 30 mg every 4 - 6 hours 32 Other Medication Antacid Tablets Chew 1 - 2 tablets after meals as required for indigestion and heartburn. Chlorphenamine (Piriton) Chlorphenamine is an antihistamine. Indications: symptomatic relief of allergic reactions (e.g. hay fever, insect bites, nettle stings) and emergency treatment of anaphylactic reactions Cautions: may affect performance of skilled tasks, like driving Side effects: drowsiness, the effects of alcohol are increased, headaches, ringing in ears, dry mouth Dose: 4 mg every 4 - 6 hourly, maximum 24 mg daily Dioralyte Dioralyte is a powder used to make oral rehydration drink for the treatment of dehydration. The aim is to replace at least as much fluid as has been lost through vomiting and diarrhoea: 200 – 400 ml of Dioralyte after each loose motion or vomit is sensible. Add one sachet to 200 ml of purified water. Discard 1 hour after preparation unless refrigerated. Discard all drink after 1 day. Loperamide (Imodium) Indications: may have a limited role in the treatment of diarrhoea when abdominal cramps are severe or to assist essential transport of the patient. Replacement of lost body fluids and salts is the first priority of treatment. Cautions: the reduced gut motility produced by this medication probably prolongs diarrhoea illness Side effects: abdominal cramps, bloating Dose: 4 mg initially then 2 mg after each loose stool, maximum 16 mg daily, 5 days maximum. 33 Lactulose Lactulose is an osmotic laxative that increases the amount of fluid in the bowel. Indications: treatment of constipation Cautions: avoid if patient is lactulose intolerant, may take up to 48 hours to work Side effects: flatulence, cramps, abdominal discomfort Dose: 1 sachet (15 ml) at night, increased to twice daily if required Prochlorperazine (Stemetil) Prochlorperazine is a member of the phenothiazine family of medications. It is also an anti-psychotic medication. Indications: severe nausea, vomiting, vertigo Cautions: avoid in pregnancy Side effects: insomnia, dry mouth, drowsiness Dose: nausea and vomiting (acute attack): 20 mg initially, then 10 mg after 2 hours; for prevention use 5 10 mg 2-3 times a day. vertigo: 5 mg 3 times a day, increasing to 30 mg daily if required Salbutamol (Ventolin) Inhaler Salbutamol is a short-acting (3 - 5 hours) bronchodilator Indications: treatment of asthma Cautions: hyperthyroidism , cardiovascular disease Side effects: tremor, headache, fast pulse Dose: Usual dose is 2 puffs, taken separately every 4 6 hours. If no relief, give up to a further 4 puffs. Repeat 6 puffs 20 mins later. If salbutamol fails to provide the usual relief that the patient expects, this may herald worsening of the asthma – urgent medical attention is required. Throat lozenges These are used for mouth and throat infections. They are helpful at altitude in the cold, dry air. 34 Cream and Ointments Anusol A cream containing steroids, anaesthetic and soothing agents. Indications: Used to treat haemorrhoids. Apply twice daily and after bowel movement. Max use 7 days. Betadine Iodine based skin disinfectant Indications: skin disinfection Cautions: flammable, avoid regular use in patients with thyroid disorders, do not apply to large wounds or severe burns, always ask about iodine sensitivity (rare) Side effects: sensitivity reaction (rare) Apply: undiluted to skin wounds twice daily Canesten Indications: Cream preparation used for fungal skin infections, especially in the ano-genital region. Apply 2 - 3 times daily. Patients should be investigated for vaginal infection on return. Note: damages the latex in condoms and diaphragms. I Hydrocortisone cream Indications: hydrocortisone cream can be used for the treatment of allergic contact or irritant dermatitis, insect bite reactions and eczema Cautions: do not apply to the face, ano-genital region or infected skin (including cold sores, athlete's foot and acne). It should not be used over large areas of skin Side effects: worsening local infection, thinning of skin, de-pigmentation Apply: sparingly twice daily for a max of 1 week. Gentisone HC drops Indications: hydrocortisone containing drops for treatment of outer ear/ear canal infection Cautions: avoid prolonged use and use with untreated local infection Side effects: local sensitivity reaction Dose: 3 drops into affected ear, 3 - 4 times daily 35 Dressings and Instruments Flex-Splint When padded can be moulded to support a fracture during evacuation. Isolaide This protects the user when giving mouth-to-mouth resuscitation. Medi-swabs Alcohol wipes for minor cuts and grazes. Flammable. Melolin Dressing Non-adhesive dressing - particularly suitable for covering grazes and superficial burns. Apply shiny surface to the wound. Micropore Tape Hypoallergenic tape for dressings. Sterile Kit The anti-infection kit contains sterile needles and drip needles for use in areas where sterility of these items cannot be guaranteed in hospitals. Syringe and needle can be used for wound cleaning. Steristrips Once thoroughly cleaned, many superficial, gaping wounds can be closed with Steristrips. Apply carefully to hold the wound edges together - if this cannot be done stitching may be required to prevent scarring. Deep wounds or wounds which are not absolutely clean should be left open to heal from the bottom. Steristripsdo not work well over joints. Vaseline Gauze Suitable covering for open grazes and burns where there is skin loss. 36 15. Post Expedition Health Brief Many illnesses will not manifest themselves whilst on expedition, but may cause symptoms on your return. Therefore, it is critical to brief the team that they should listen to their bodies and if they feel unwell they should see their GP and mention that they have been away to he specific country. General points anti-malarial medications and other courses of treatment must be completed see your GP if you feel unwell, especially with fever for more than 24 hours or persistent diarrhoea and tell him/her where you have been (i.e. in a malaria area, if applicable) keep hydrated and rested watch out for ‘post expedition blues’, which can be combated with: contact with other team members support from the experienced personnel within West Lancashire Scout County focusing on new challenge Encourage to discuss issues and concerns with the Leader team. Please do ensure people know they can call. If in doubt - get checked out! 37 16. Patient Treatment Use the mnemonic ‘Dr ABCDE’: D (danger) r (responsiveness) A (airway, with control of cervical spine) B (breathing) C (circulation, with control of bleeding) D (deformity and disability) E (examination, etc.) It’s never too soon to start thinking about evacuation! D (danger) Consider s there a risk to you or other bystanders? is the patient safe to approach? protect the patient from the environment number of casualties? consider the priority of treatment if more than one patient r (responsiveness) What is the patient’s level of alertness? fully alert responds to your voice responds to a painful stimulus unconscious A (airway, with control of cervical spine) is the airway clear? does the cervical spine need protecting? B (breathing) Look, listen and feel: is the patient breathing? what is the breathing rate? does it look and sound normal? consider head tilt and chin lift C (circulation, with control of bleeding) what is the pulse rate? can it be felt at the neck and the wrist? 38 does it feel strong or weak? what is the capillary refill time? control serious bleeding using pressure and elevation D (deformity and disability) perform a rapid but head to toe check looking for obvious injury can they move all four limbs normally? E (examination etc.) expose and examine injuries evacuation plan emotional support evaluate and monitor treatment History: Use the mnemonic ‘SAMPLE’: S symptoms A allergies M medication P past medical history L last oral intake E events (including mechanism of injury) Basic Life Support algorithm: 1. 2. check responsiveness (shout assess AVPU) open airway (head tilt, chin lift / jaw thrust (if spinal) 3. check breathing for 10 seconds: - if breathing continue as above - if not breathing normal start CPR CPR: Chest compressions (1/3 chest) at rate of 100 per minute, 30 compressions then 2 breaths and repeat cycle. Note - if drowning / lightening / Under 12 yrs: Before commencing CPR give 5 breaths Recording Recording findings on the patient cards. 39 17. Report Cards Initial Incident Report To save time and to improve reporting complete the following report before calling in for support: Background: Venture Leader’s name and group name contact information (i.e. telephone number leader can be reached on) exact location summary of events and times Patients: patient numbers and injuries treatment plan rescuers: o on site o required o medical advice required? equipment: o on site o required evacuation plan/options o o internal o external agencies required? 40 Medical Report To save time and to improve reporting complete the following report before calling in for medical advice: Background: Medic’s name and training Summary of events and times o Weather / Terrain o Resources o Evacuation options Patient: Chief Complaint History o o o Events Mechanism of injury / illness SAMPLE history Physical Examination Vital Signs over a period of time o see patient card for details Field Diagnosis Treatment so far Advice: Treatment Plan o Proposed Evacuation o Options o Preference o Requests o Equipment o Resources o Medications 41 42