NURS4036_Cardiogenic_Shock_Case_Study
advertisement

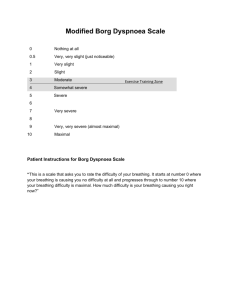
NURS 4036 – Complex Health Challenges CASE STUDY Mr. Borg is a 70-year-old retired black man who was admitted to the emergency room (ER) after arriving by ambulance. According to his wife, he developed vomiting and progressive weakness earlier in the day. When the paramedics arrived at this home, he was in supraventricular tachycardia with a rate of 186 beats per minute (bpm). The paramedics administered adenosine (Adenocard) 6 mg IV, followed by an additional 12 mg three minutes later. Mr. Borg denied the presence of chest pain or shortness of breath upon admission to the ER. He was cyanotic with no palpable blood pressure and a regular heart rate of 160 bpm. A bolus of Diltiazem (Cardizem) 10 mg was administered IV push and he converted briefly to normal sinus rhythm. When he went back into supraventricular tachycardia, a Diltiazem drip was initiated. Blood gases drawn in the ER showed a pH of 7.3 and PaCO2 of 55mm Hg. Mr. Borg was transferred to the ICU with the Diltiazem drip and oxygen at 4 l/min per nasal cannula. In ICU, Mr. Borg’s hypotension and tachycardia persisted and a low-dose dopamine drip was initiated at 2 ug/kg/min. Mr. Borg became more hypotensive, tachycardic, and hypoxic. He was then intubated and placed on a ventilator with 100% oxygen. Furosemide (Lasix) 80 mg and Procanamide (Pronestyl) 500 mg IV bolus were administered. The next morning, Mr. Borg was no longer acidotic, with a pH of 7.36. His heart rate was 140 bpm and the systolic BP was around 100 mm Hg while he was on 9 ug/kg/min of dopamine. The ECG reveals that the distal two thirds of the left ventricle is akinetic. Mr. Borg is scheduled to have a right and left heart catheterization at 13:00 today. Selected Laboratory Values RBC Hgb Hct WBC Sodium Potassium Chloride Cholesterol Triglycerides 4.08 million/mm3 14.2 g/dL 41.70% 20,500/mm3 135 mEq/L 3.3 mEq/L 94 mEq/L 264 mg/dL 334 mg/dL Nursing Admission Assessment: Mr. Borg is a former mail carrier who retired at 10 years ago. He and his wife recently celebrated their 50th wedding anniversary. Their two sons live in cities 1500 km away, and they will be flying in to visit their father as soon as possible. His wife reports that he stopped smoking 20 years ago and continues to drink two to four alcoholic beverages per day. He has gained 40 lbs during the past 10 years. His wife is concerned that he eats and drinks too much and that he spends most of the day sitting in front of the television. Mr. Borg’s wife also reports that he has been taking Benazepril (Lotensin) 10mg/day. Nursing Physical Examination: Height: 5’ 11’’ Weight: 210 lbs (95.45 kg) Vital Signs: BP 90/40; T = 101; P = 135; R = 20. LOC: Sedated & intubated EENT: Within normal limits Cardiac: S1 & S2 audible without murmur, questionable S3 regular rate, unable to assess neck vein distention. Pulmonary: Rhonchi present throughout lungs with fine basilar rales bilaterally. Abdominal: Within normal limits. Genitourinary: Foley catheter in place draining clear yellow urine. Peripheral pulses: 1+ pitting edema which extends to midcalf Current Treatment Plan: Meds: Dopamine 1600 mg in 500 ml D5W; titrate to keep systolic BP >90 mm Hg: Furosemide 40 mg IV tid Potassium 40 mEq in 100 ml D5W over 4 hours bid Thiamine 100 mg IM qd Ceftriaxone 1g q 12h IV Saline lock as needed for medications flush bid, prn Diet: NPO Activity: Bedrest Respiratory treatments: 70% FiO2 ventilator Diagnostic tests: repeat CXR, ECG, CBC, metabolic profile, cardiac enzymes The results of the cardiac catheterization reveal 100% occlusion of the left coronary artery and severe diffuse disease of the left anterior descending coronary artery. The physicians have determined that he is a poor surgical risk and plan to treat him medically. Mr. Borg has interpreted this an indication that his problem is temporary and states, “You can’t keep a good man down.” Over the next several days, Mr. Borg’s blood pressure stabilizes and he is weaned off the dopamine. The Furosemide is changed to an oral dose and the potassium is reduced to 10 mEq po tid. Mr. Borg is also digitalized and will be maintained on Digoxin 0.25 mg qd. His resting heart rate has been approximately 70 bpm. Mr. Borg is also extubated and placed on a no added salt, low fat diet. He is to begin a cardiac rehabilitation program. The physician is planning to discharge him tomorrow following a recovery treadmill test. Discharge Criteria: Average LOS: 7 days Cardiac rehabilitation initiated and follow-up appointments scheduled (including diet, exercise, stress management, and medication teaching) Questions to be Considered: 1. Compare and contrast left versus right ventricular, backward versus forward, and high versus low output heart failure. Given the information provided, how would you categorize Mr. Borg’s heart failure? 2. Compare and contrast the effects of Mr. Borg’s cardiac medications: dopamine, Diltiazem, adenosine, and Digoxin. Why are the Furosemide and Potassium ordered? 3. According to the 4 stages of psychosocial recovery outline under community and self-care for MI patients, what stage is Mr. Borg in? Discuss examples of behaviour that indicate that he is progressing through the other stages of recovery. 4. What ramifications do Mr. Borg’s life-style have on the success of his cardiac rehabilitation program? How might a home health nurse facilitate Mrs. Borg’s participation in his rehabilitation program? 5. Eight weeks after discharge, Mr. Borg asks the cardiac rehabilitation nurse if new lights have been installed because “they all have a yellow ring around them and the edges are fuzzy.” Upon further investigation the nurse determines that Mr. Borg has also had a decreased appetite, intermittent nausea and vomiting, and decreased ability to complete his entire exercise protocol. What should the nurse suspect? What recommendations should she make?