ЗАТВЕРДЖЕНО
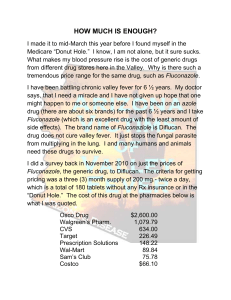
advertisement

APPROVED Order of the Ministry of Health of Ukraine _06.09.2011_ № __570_ Registration certificate №UA/5156/01/03 INSTRUCTION FOR USE of medicinal preparation DIFLUZOL® Composition: Active substance: fluconazole; 1 capsule contains 150 mg of fluconazole, calculated as 100% substance; Excipients: calcium stearate, sodium starch glycollate (type А). Pharmaceutical form. Capsules. Hard gelatin capsules № 1, the corpus is turquoise, the cap of the capsule is green. Capsule content – white or almost white odorless powder. Name and location of manufacturer. OJSC «Kyivmedpreparat». Ukraine, 01032, Kyiv, Saksaganskogo str, 139. Pharmacotherapeutic group. Systemic antifungal agents. Triazole derivative. АТС Code J02A C01. Fluconazole is a triazole derivative with fungistatic effect; it specifically inhibits sterol synthesis in fungal cells. The range of time to onset of symptoms relief after use of 150 mg of fluconazole as single dose is one hour to nine days (average 24 hours). There have been reports of cases of superinfection with Candida species other than C. albicans, which are often inherently not susceptible to fluconazole (e.g.,Candida krusei). Such cases may require alternative antifungal therapy. Fluconazole is highly specific to the cytochrome P-450 enzymes of the fungus. Following oral administration fluconazole is well absorbed. The degree of absorption is not affected by the simultaneous intake of food. The maximum serum concentration is generally reached after 0.5 to 1,5 hours, when the preparation was taken in fasted state. Binding to plasma proteins is about 11-12%. The half life is about 30 hours. After oral administration fluconazole has a bioavailability of more than 90%. Fluconazole has shown good penetration into various body fluids. High concentrations of fluconazole in the skin, well above serum concentrations, have been shown in the stratum corneum, epidermisdermis, and in eccrine sweat. Fluconazole is accumulated in the stratum corneum Fluconazole is eliminated mainly via the kidneys. 80% of the dose is found in urine in unchanged form. The elimination of fluconazole is proportional to creatinine clearance. Indications for use. Previously diagnosed (or episodically manifested) vaginal candidiasis. Contraindications. Fluconazole should not be used in patients with known sensitivity to the drug, any of the inert ingredients or to related azole compounds. Co-administration of other drugs known to prolong the QT interval and which are metabolised via the enzyme CYP3A4 such as astemizole, pimozide, quinidine, cisapride and terfenadine are contraindicated. Special warnings and precautions for use. Fluconazole has been associated with rare cases of serious hepatic toxicity including fatalities, primarily in patients with serious underlying medical conditions. In cases of fluconazole-associated hepatotoxicity, no obvious relationship to total daily dose, duration of therapy, sex or age of patient has been observed. Fluconazole hepatotoxicity has usually been reversible on discontinuation of therapy. Patients who develop abnormal liver function tests during fluconazole therapy should be monitored for the development of more serious hepatic injury. Fluconazole should be discontinued if clinical signs or symptoms consistent with liver disease develop that may be attributable to fluconazole. Patients have rarely developed exfoliative cutaneous reactions, such as Stevens-Johnson syndrome and toxic epidermal necrolysis, during treatment with fluconazole. AIDS patients are more prone to the development of severe cutaneous reactions to many drugs. If a rash, which is considered attributable to fluconazole, develops in a patient treated for a superficial fungal infection, further therapy with this agent should be discontinued. In rare cases, as with other azoles, anaphylaxis has been reported. Fluconazole have been associated with prolongation of the QT interval on the electrocardiogram. Therefore it should be administered with caution in patients with possible development of arrhythmia: congenital or acquired QT interval prolongation, cardiomyopathy, especially in patients with heart failure, sinus bradycardia, symptomatic arrhythmia, concomitant use of preparation which cause prolongation of QT interval and are not metabolized by enzymes CYP3A4, hypokalemia, hypomagnesaemia, hypocalcaemia. Fluconazole should be administered with caution to patients with these potentially proarryhthmic conditions. Patient with liver, cardiac or renal disorders should consult a doctor before starting therapy with fluconazole. Positive dynamics of symptoms usually is observed after 24 hours following administration. But their disappearing might be observed only after few days. If patient did not notice improvement within few days, he (she) should consult a doctor. Special precautions. Administration during pregnancy and lactation Adequate and well-controlled studies in pregnant women have not been performed. Some cases of multiple congenital abnormalities have been reported in infants whose mothers were treated for coccidiomycosis with fluconazole at a high dose (400-800 mg per day) for 3 months or more. The connection between the use of fluconazole and these effects is unclear Pregnant women and women of childbearing potential without effective contraception should avoid treatment with fluconazole. Use of fluconazole in nursing mothers is not recommended. Children. The data about administration of fluconazole in single dose 150 mg in children with vaginal candidiasis are insufficient. Effects on ability to drive and use machines. Fluconazole is unlikely to affect the ability to drive or use machinery. Posology and Method of Administration. Adults. The recommended dosage of Difluzole® for vaginal candidiasis is 150 mg as a single oral dose Elderly. Treatment of patients above 60 years with fluconazole in dose 150 mg without a doctor’s suervision is not recommended. Patients with impaired renal function. Fluconazole in mainly excreted in the urine in unchanged form. For patients with mild and moderate renal insufficiency there is no need for adjustments of single dose. Creatinine clearance (ml/min) Percent of recommended dose > 50 ≤ 50 (without dialysis) Dialysis patients 100% 50% 100% dose after each dialysis session Overdose. There have been solitary reports of overdose with fluconazole and hallucination and paranoid behaviour have been concomitantly observed. In the event of overdose, symptomatic treatment (with supportive measures and gastric lavage if necessary) may be adequate. Fluconazole is largely excreted in the urine; forced volume diuresis would probably increase the elimination rate. A three-hour hemodialysis session decreases plasma levels by approximately 50%. Undesirable effects. Central nervous system disorders: headache, dizziness, vertigo, seizures, tremor, taste preversions, insomnia, drowsiness, paraesthesia. Gastrointestinal disorders: abdominal pain, diarrhoea, flatulence, nausea, vomiting, dry mouth, dyspepsia. Blood and the lymphatic system disorders: leukopenia, including neutropenia and agranulocytosis, thrombocytopenia. Immune system disorders: anaphylaxia, including angioneurotic edema, facial edema, skin itching, urticaria. Metabolism disorders: hypercholesterolemia, hypertriglyceredaemia, hypokalemia. Cardiovascular disorders: QT interval prolongation, torsade de pointes. Hepato-biliary disorders: toxic liver damage, including solitary lethal cases, increased levels of hepatic enzymes (alanine aminotransferase, aspartate aminotransferase, blood alkaline phosphatase) and bilirubin, hepatic failure, hepatitis, hepatocellular damage, cholestasis, jaundice. Skin and subcutaneous tissue disorders: alopecia, increased sweating, exfoliative dermatitis, including Stevens-Johnson syndrome and toxic epidermal necrolysis, rash, гострий acute generalised exanthematous-pustulosis. Other: myalgia, malaise, asthenia, fever. Interaction with other medicaments and other types of interactions. Following types of interactions were observed in cases of multiple-dose administration and were not reported following single dose. Patients who take concomitantly other drugs should consult a doctor before initiation the treatment with fluconazole. Anticoagulants. Bleeding events such as bruising, epistaxis, gastrointestinal bleeding, hematuria and melena have been reported in association with increases in prothrombin time in patients receiving fluconazole and warfarin concomitantly. Careful monitoring of prothrombin time in patients receiving coumarin type anticoagulants is recommended. Azitromycine. No significant pharmacokinetical interactions between fluconazole and azitromycin have been reported. Benxodiazepines (short acting). Substantial increases in midazolam concentrations and psychomotor effects are observed when oral midazolam and fluconazole are co-administered. The effect on midazolam appears to be greater when fluconazole is administered orally than when fluconazole is administered intravenously. If concomitant administration of benzodiazepines and fluconazole is required then the prescriber should consider reducing the benzodiazepine dose and appropriate monitoring of the patient should be undertaken. Cisapride. Cardiac events including torsades de pointes have been reported in patients receiving fluconazole and cisapride concomitantly. Concomitant administration of fluconazole in dose 200 mg daily and cisapride 20 mg four times daily significantly increase concentration of cisapride in blood plasma and leads to prolongation of QT interval. Co-administration of cisapride is contraindicated in patients receiving fluconazole. Ciclosporin. It was found that fluconazole 200mg daily slowly increases ciclosporin concentrations in renal transplant patients, but a multiple dose study with fluconazole 100mg daily showed no effect on ciclosporin levels in patients with bone marrow transplants. It is therefore recommended that ciclosporin plasma concentration is monitored in patients receiving fluconazole. Hydrochlorothiazide: Multiple-doses of hydrochlorothiazide increase plasma concentration of fluconazole. But this should not necessitate a change in the fluconazole dose regimen in subjects receiving concomitant diuretics, although the prescriber should bear it in mind. Oral contraceptives. No relevant effects on hormone levels occurred during a study with fluconazole 50mg, whilst the AUCs of ethinylestradiol and levonorgestrel were increased by 40% and 24% respectively during a study with fluconazole 200mg. During administration of fluconazole in dose 300 mg once per week, the AUC of ethinylestradiol and norethindrone increases by 24% and 13 % respectively. It is considered that multiple dose fluconazole is unlikely to affect the efficacy of the combined oral contraceptive. Phenytoin. Levels of phenytoin may increase to a clinically significant degree during co-administration with fluconazole. Phenytoin levels should be monitored and the phenytoin dose adjusted to maintain therapeutic levels if co-administration is necessary. Rifabutin. Concomitant administration of fluconazole and rifabutin results in increased serum level of the latter. There have been reported cases of uveitis. Close monitoring is required. Rifampicin A 25% decrease in the AUC and 20% shorter half-life of fluconazole occurred when fluconazole and rifampicin were administered concomitantly. An increase in the fluconazole dose should be considered in patients receiving concomitant rifampicin. Sulfonylureas. Fluconazole has been shown to prolong the serum half-life of concomitantly administered oral sulfonylureas (e.g., chlorpropamide, glibenclamide, glipizide, tolbutamide). Fluconazole and oral sulfonylureas may be concomitantly administered to diabetics but the possibility of an hypoglycaemic episode should be considered. Tacrolimus. Increased serum levels of tacrolimus have been reported in patients receiving fluconazole and tacrolimus concomitantly. There have also been reports of nephrotoxicity in patients receiving this combination. Close monitoring is required. Terfenadine (when the dose of fluconazole is 400 mg). It is recommended that terfenadine and fluconazole in dose more than 400 mg should not be administered concomitantly due to the potential seriousness of an interaction of terfenadine and azole derivatives (prolongation of QT interval, arrhythmia). Theophylline. Use of fluconazole for 14 days caused decrease in the mean plasma clearance of theophylline. The therapy should be modified if signs of toxicity occur. Zidovudine. Fluconazole increases concentration of zidovudine in plasma. Patients receiving this combination should be closely monitored. Astemizole. Astemizole or other drugs metabolised by the cytochrome P450 system taken concomitantly with fluconazole may be associated with elevations in serum levels of these drugs in patients. Therefore caution should be exercised when using these combinations and the patients should be carefully monitored. Erythromycin. Erythromycin can increase plasma concentration of fluconazole. Pimozide. Combining fluconazole with pimozide may inhibit the metabolism of the latter. Increased concentration of pimozide in blood may cause prolongation of QT interval; rare cases of torsade de pointes have been reported. Concomitant use of these preparations is contraindicated. Amitriptyline. Fluconazole increases the effect of amitriptyline. Dosage of amitriptyline should be adjusted, if necessary. Amphotericine. Preclinical data about concomitant administration of fluconazole and amphotericine reveal slight additive effect in infections with C.albicans, and antagonism of the two preparations in infections with А.fumigatus. These data are not clinically proven. Carbamazepine. Fluconazole inhibits the metabolism of carbamazepine and an increase in serum carbamazepine of 30% has been observed. Dosage adjustment of carbamazepine may be necessary. Celecoxib. During concomitant treatment with fluconazole (200 mg daily) and celecoxib (200 mg) the celecoxib Cmax and AUC increased by 68% and 134%, respectively. Half of the celecoxib dose may be necessary when combined with fluconazole. Cyclophosphamide. Combination therapy with cyclophosphamide and fluconazole results in an increase in serum bilirubin and serum creatinine. Fentanyl. It was shown that fluconazole delayed the elimination of fentanyl significantly. Elevated fentanyl concentration may lead to respiratory depression and death. HMG-CoA reductase inhibitors. The risk of myopathy and rhabdomyolysis increases when fluconazole is coadministered with HMG-CoA reductase inhibitors metabolised through CYP3A4, such as atorvastatin and simvastatin, or through CYP2C9, such as fluvastatin. If concomitant therapy is necessary, the patient should be observed for symptoms of myopathy and rhabdomyolysis and creatinine kinase should be monitored. HMG-CoA reductase inhibitors should be discontinued if a marked increase in creatinine kinase is observed or myopathy/rhabdomyolysis is diagnosed or suspected. Losartan. Fluconazole inhibits the metabolism of losartan to its active metabolite. Patients treated concomitantly with fluconazole and losartan should have their blood pressure monitored continuously. Methadone. Fluconazole may enhance the serum concentration of methadone. Dosage adjustment of methadone may be necessary. Non-steroidal anti-inflammatory drugs (NSAIDs). The Cmax and AUC of flurbiprofen was increased by 23% and 81%, respectively, when coadministered with fluconazole. Similarly, the Cmax and AUC was increased by 15% and 82%, respectively, when fluconazole was coadministered with racemic ibuprofen (400 mg). Although not specifically studied, fluconazole has the potential to increase the systemic exposure of other NSAIDs (e.g. naproxen, lornoxicam, meloxicam, diclofenac). Frequent monitoring for adverse events and toxicity related to NSAIDs is recommended. Adjustment of dosage of NSAIDs may be needed. Prednisone. Patients on long-term treatment with fluconazole and prednisone should be carefully monitored for possible development of adrenal cortex insufficiency. Fluconazole is a potent inhibitor of cytochrome P450 (isoenzyme CYP2C9 and CYP3A4). Therefore caution should be exercised when using with preparations, metabolized by this enzyme system. List of such preparations include alfentanil, calcium channel blockers (nifedipine, isradipine, amlodipine and felodipine), halofantrine, saquinavir, sirolimus, vinca alkaloids (vincristine and vinblastine). In case of concomitant use of these preparations with fluconasole, blood concentration monitoring is required and and the patient should be closely monitored for development of possible undesirable effects. Vitamin А. This combination may be used but there is a possibility of CNS related undesirable effects (benign intracranial hypertension, which diminishes after fluconazole discontinuation). Interaction studies have shown that when oral fluconazole is coadministered with food, cimetidine, antacids or following total body irradiation for bone marrow transplantation, no clinically significant impairment of fluconazole absorption occurs. Studies of possible interaction with other medicinal preparations have not been performed, therefore interaction is considered possible. Shelf-life. 4 years. Conditions of storage. Store in protected from the light place at the temperature above 25 °С. Keep out of reach of children. Nature and content of container Capsules 150 mg № 1 in blister, 1 or 2 blisters in pack, or № 2 in blister, 1 blister in pack. Dispensing category. Non-prescription medicine – capsules 150 mg № 1. Prescription medicine – capsules 150 mg № 2. Date of the last revision.