Case Study UTI - NHS Education for Scotland
advertisement

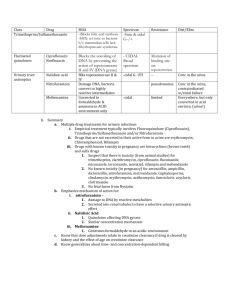
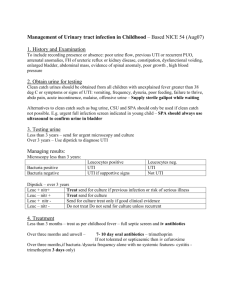
NES Core Course on Antimicrobials Case Study on Urinary Tract Infection Anna, a 20 year-old student, comes in to your pharmacy and asks to speak with the pharmacist. She thinks she has an infection in her urine and asks what you can give her for it. On her PMR you see a three day course of trimethoprim was dispensed 6 months ago. Discussion points 1) What questions would you ask Anna to confirm the diagnosis? What are her symptoms and how long has she had them? Signs and symptoms of UTI include dysuria, urgency, frequency, polyuria, suprapubic tenderness, fever and flank or back pain. Presence of two or more signs or symptoms is suggestive of UTI. The presence of fever and flank or back pain may suggest an upper UTI (pyelonephritis). Check for previous episodes and possibility of pregnancy. Vaginal itch or discharge may suggest an STI or vulvovaginitis (usually due to candida). Urethritis caused by N. gonorrhoeae or C. trachomatis is relatively more likely if a women has had a new sexual partner in the past few weeks or if her sexual partner has urethral symptoms; there is a past history of a sexually transmitted disease (STD); symptoms were of gradual onset over several weeks and there are accompanying vaginal symptoms such as vaginal discharge or odour. Vaginitis is suggested by the presence of vaginal discharge or odour, pruritus, dyspareunia, external dysuria and no increased frequency or urgency. 2) What recommendations would you make? If she has two or more symptoms of UTI she should be referred to her GP for antibiotic treatment. If she has only one symptom, she should be recommended to monitor for worsening of symptoms and encouraged to drink plenty of fluids, pass urine as soon as she feels the need and maintain good hand and toilet hygiene (wiping from front to back to avoid transferring organisms). Evidence for efficacy of alkalinising agents is lacking so do not suggest using them. They are contra-indicated in impaired renal function (CrCl < 60ml/min) and interact with nitrofurantoin reducing the effectiveness of the antibiotic by altering the urinary pH. If there are any symptoms suggestive of urethritis or vaginitis, refer to the GP for further investigation which may include a pelvic examination. -1- Anna states she has a burning or stinging sensation when passing urine (dysuria) and is going to the toilet much more frequently so she is referred to her GP. She returns the next day with a prescription for ciprofloxacin 250mg twice daily for 7 days. 3) What are the likely infecting organisms in UTI and what is recommended first line agent? The spectrum of causative organisms in upper and lower UTI is similar with E. coli being the main pathogen in 70 to 95 % of cases and Staphylococcus saprophyticus in about 5 to 10% of cases. Occasionally, other Enterobacteriaceae, such as Proteus or Klebsiella are isolated. For empiric treatment of uncomplicated UTI in non-pregnant women, the recommended first choice is a 3-day course of trimethoprim or nitrofurantoin, which are narrow spectrum agents. Three days therapy has been shown to be as effective as 7 days. The use of second line agents such as amoxicillin, coamoxiclav, ciprofloxacin and cefalexin should be restricted to treatment of proven UTI and based on sensitivity results. 4) Is ciprofloxacin the most appropriate choice for Anna? No - she has an uncomplicated UTI which should be treated empirically with a short course of a narrow spectrum agent such as trimethoprim or nitrofurantoin. Ciprofloxacin is a broad spectrum antibiotic which should be reserved for second line treatment of lower UTI based on the results of urine culture and sensitivity or for upper UTIs. Given the difficulty of excluding prostatitis in men with symptoms suggestive of UTI, the current recommendation is to treat bacterial UTI in men empirically with two weeks of a fluoroquinolone. Increasing concerns about fluoroquinolone resistance mean that routine use of these drugs in uncomplicated UTI should be discouraged. Ciprofloxacin can predispose patients to infection with Clostridium difficile and MRSA and it can interact with many drugs metabolised by cytochrome P450 in the liver. 5) What would you discuss with the GP? Suggest the use of a narrow spectrum agent such as trimethoprim or nitrofurantoin for 3 days using the above reasons. 6) What other advice would you offer Anna to avoid future recurrence? Clinical Knowledge Summaries website (formerly Prodigy) has a very good patient information leaflet for the treatment of UTI. It can be accessed via http://www.cks.library.nhs.uk/patient_information_leaflet/urinary_tract_infe ction_adults/view_as_a_leaflet Maintain good toilet hygiene Pass urine after sexual intercourse Avoid holding urine in the bladder for a long time – pass urine as soon as you feel the need -2- Treat constipation promptly as this can predispose to UTI. 7) The manufacturers of trimethoprim and nitrofurantoin have applied for reclassification from POM to P. What advantages and disadvantages can you see with this? What steps might pharmacists in the community take to avoid inappropriate use? Advantages - improved patient access to treatment including out of hours, - education on appropriate use of antibiotics, - improved pharmacist knowledge on appropriate antimicrobial use. Disadvantages - increased risk of antimicrobial resistance e.g. trimethoprim in MRSA treatment combinations, nitrofurantoin in ESBLs - risk of mis-diagnosis of an STI, - encouragement of other POM to P classifications – cefaclor, pivmecillinam, ciprofloxacin, - using trimethoprim & nitrofurantoin in Pharmacies may mean GPs are more likely to use broader spectrum agents such as ciprofloxacin, coamoxiclav - gap in overall antimicrobial consumption data. References SIGN Guideline 88 Management of Suspected Bacterial Urinary Tract Infection in Adults. July 2006 Clinical Knowledge Summaries accessed via www.cks.library.nhs.uk Guidelines on The Management of Urinary and Male Genital Tract Infections. European Association of Urology March 2008 accessed via http://www.uroweb.org/nc/professional-resources/guidelines/online/ : -3-