Early Goal Directed Therapy: A review of current methods, their
advertisement

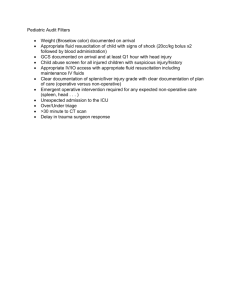
Early Goal Directed Therapy: A review of current methods, their efficacy, and role in a changing paradigm of resuscitation efforts Katie Perz, D.O. Abstract The concept of goal directed therapy has been a constantly changing entity in the field of medicine for some time now. With newer technologies available and new knowledge emerging, the management of trauma, states of shock, and critical care scenarios is continually evolving. The purpose of this review is to identify the mainstays of hemodynamic monitoring and their significance in today’s medicine; it will continue to acknowledge newer modalities of monitoring and establish whether the concept of goal directed therapy within the realm of fluid management and resuscitation is realistic and efficacious. Technology and expanding knowledge have lead to the rise of new monitoring devices that have yet to establish a permanent place in the domain of fluid resuscitation; this review will examine the evidence regarding whether a change in the paradigm of hemodynamic monitoring is appropriate. Through examination of the former and current research surrounding specific devices and modalities incorporated in the strategy of Early Goal Directed Therapy, it is very clear that, while much evidence exists, we are very far from a resolute algorithm to reference when dealing with high risk patients in need of resuscitation. The original concept of goal directed therapy hinged upon parameters such as arterial blood pressure, heart rate, urine output, central venous pressure, and variables derived from the pulmonary artery catheter (PAC). Currently, newer modalities of a less invasive character are coming to the forefront; their non-invasive nature is demanding an audience and a thorough review regarding their legitimacy as guides for patient resuscitation. Parameters such as stroke volume variation (SVV) and pulse pressure variation (PPV) are derived from the Flotrac/Vigileo, PiCCO, and ccNexfin devices. Central venous oxygen saturation, transesophageal echocardiography, transthoracic echocardiography, and esophageal doppler all, when able to be used, provide vital patient information. Lactate levels have been a mainstay of determination of the adequacy of perfusion for some time now, and are currently being evaluated as a tool among many to guide resuscitation therapy. Microcirculation monitoring through Orthogonal Polarization Spectral and Sidestream Darkfield (OPS/SDF) imaging, Near-Infrared Spectroscopy and gastric tonometry combine known techniques with new technology to examine the microcirculation directly and determine the nature of its perfusion. Impedance cardiography (using the NICCOMO and BioZ devices) and electrical cardiometry (using the ICON, Aesculon, and CheetahTM devices) techniques have improved upon previous efforts to establish monitoring of thoracic blood flow, and in turn, cardiac performance. This review examines the current evidence for each of the able techniques and devices as part of a grander purpose of establishing an effective protocol for Early Goal Directed Therapy, in aims of improving outcomes in high risk surgical patients. 1 Introduction The concept of Early Goal Directed Therapy (EGDT) emerged in 1988 when Shoemaker and colleagues showed that morbidity and mortality in high risk patients could be significantly reduced using specific endpoints as part of resuscitative efforts. It has been shown that a small percentage of patients are generally candidates for EGDT (14), but it is these patients that account for the majority of perioperative morbidity and mortality (1). Perioperative clinical determination of the intravascular volume status of a patient can be extremely difficult. While resuscitation is the first step in the management of hemodynamically unstable patients, many studies have shown that less than 50% of these unstable patients will respond to a fluid challenge (4). So, while under-resuscitation results in inadequate organ perfusion, over-resuscitation increases morbidity and mortality (4). The underlying physiologic concept behind resuscitation involves oxygen delivery and identification of which patients are high risk of being unable to supply an amount of oxygen equal to that which is being consumed. Major surgery is associated with a significant systemic inflammatory response, which increases total oxygen demand; this necessitates increased oxygen delivery that many of these high risk patients have difficultly achieving. There is considerable evidence that demonstrates the benefits of monitoring parameters of oxygen delivery and that the practice of augmenting oxygen delivery in high-risk surgical patients during perioperative periods will improve outcomes (1). This monitoring of the adequacy of oxygen delivery can reduce the morbidity and mortality in these patients (which can approach 30-40%) if done effectively. The challenge in today’s medicine involves evaluating which methods are appropriate, accurate, feasible, and cost effective for widespread use. However, the challenge lies in our ability to assess oxygen debt and the nature of “hypoperfusion”. The concept of “fluid responsiveness” is common in today’s medicine to distinguish patients who are under-resuscitated and therefore prone to tissue hypoxia. This paper offers a detailed look at the pathophysiology of oxygen debt, leading to increased morbidity and mortality in high risk patients. It will also address the challenges we face in today’s medical climate within the arena of EGDT and evaluation of a patients need for resuscitation; finally, it will review of many of the devices available to foster progress and measure fluid responsiveness in the realm of EGDT. History Millions of surgical procedures are performed each year; mortality within 30 days of surgery is estimated to be between 0.7 and 1.7% (1). However, it is a small percentage of patients that account for over 75% of deaths, but only 12.5% of surgical procedures. Generally, these patients are undergoing high risk surgery, with an expected mortality rate of more than 5% (1). The nature of high risk surgery involves prolonged procedures, an invasive character, high blood loss, trauma surgery, emergency surgery, or vascular surgery (typically performed on high risk patients), just to name a few. High risk patients have a poor outcome due to their inability to meet the metabolic requirements of these surgeries, namely, increased oxygen demand, which subsequently increases their risk of morbidity and death. It has been shown that those who survive major surgery have lower levels of oxygen consumption than non-survivors, which highlights the concept of “oxygen debt” (1). The concept of early goal directed therapy aims to identify the presence of oxygen debt, or markers that are evidence 2 of it, and then provide a standardized method of guiding the therapy to mitigate the present and future damage to tissues and organs. Currently there are numerous devices on the market evaluating even more specific parameters in aims to identify oxygen debt that could potentially lead to organ damage, morbidity and mortality. However, there is still a lack of evidence regarding how these devices and parameters can fit into a larger scale protocol for managing high risk patients in surgical and intensive care environments. When evaluating what parameters would be useful in identifying oxygen debt, it is prudent to start with the pathophysiology of high risk surgery. High risk surgery is inherently associated with a systemic inflammatory response indicating increased oxygen consumption by the tissues (VO2) (1). This necessitates the increased delivery of oxygen to these areas (DO2), which is generally accomplished by an increase in cardiac output (CO), or an increase in the oxygen carrying capacity of hemoglobin (CaO2). Patients who are unable to augment their cardiac output (those with cardiopulmonary disease, including coronary artery disease, congestive heart failure, etc.) will suffer from an increase in oxygen debt. Commonly the tissue’s initial response is to extract more oxygen from the oxygen load it is presented with; this will lead to a decreased amount of venous oxygen, measured by central venous oxygen saturation (SVO2). When no more oxygen can be extracted from the limited amount being received by the tissues, the lack of oxygen for metabolic processes will lead to a change in the nature of tissue perfusion, ultimately causing a change from aerobic to anaerobic metabolism; this increases anaerobic markers, such as lactate. Reduced perfusion to specific organs can produce specific alterations, such as changes gastric intramucosal pH (pHi), for instance; a similar example is seen when reduced perfusion of other end organs can be measured directly by dark field videomicroscopy. All of these avenues have been studied as potential sources for monitoring with the main goal of being able to identify tissue hypoperfusion and, using a goal-directed approach through a particular monitoring device, provide resuscitation therapy that will improve the state of oxygen debt. However, the variable most commonly considered is cardiac output, which is the most feasible way to manipulate DO2 and VO2. CO represents the top of the algorithm, and if it can be measured that cardiac output is adequate, then there is less risk of decreased end organ perfusion, which can be suggested to decrease morbidity and mortality. Generally, the strategy to influence cardiac output is through fluid resuscitation and inotrope use, but the ultimate goal is to facilitate perfusion of the tissues to achieve oxygen delivery (4). Decades ago, the closest approximation to CO, DO2 and VO2 was heart rate and blood pressure. With the addition of the pulmonary artery catheter (PAC), targets like cardiac index (CI), and oxygen delivery index (DO2I) could be evaluated. It was recognized that, while underresuscitation caused end organ damage, increasing cardiac output and oxygen delivery in patients with adequate organ perfusion served no purpose, and could actually be harmful (4). The concept of goal directed therapy with newer parameters was studied, and with this approach, morbidity and mortality were substantially reduced in comparison to the commonly used blood pressure, arterial pressure and central venous pressure. In 1993, Boyd et al conducted a randomized controlled trial in which the same treatment goals were targeted pre- and post-operatively; a 75% reduction in mortality was shown together with less postoperative complications. Then, Wilson et al conducted a study targeting DO2I, a hemoglobin >11, and pulmonary artery occlusion pressure >12, which confirmed that preoperative 3 optimization of oxygen delivery significantly reduced length of stay and hospital mortality (1). These studies are a few of the many examples showing a substantial benefit from the use of EGDT. However, while it is well accepted that protocol based resuscitation is effective, there is still not a consensus on which parameters should be used to direct therapy. The main reason that there is still not a resolute algorithm for EGDT is that more evidence is necessary. Many of the studies done have either a small sample size, are not randomized control trials, exclude a surgical population, or are not easily extrapolated to apply to an entire population. Many of the newer devices are continuously updating their software programs; this necessitates a deeper critical review of older studies, as newer software improvements improve device accuracy. However, all of these issues can only be rectified with more research. Another dilemma lies in a changing of the paradigm of technology used. Much of the research currently in print involves the use of a PAC or CVP. The paradigm is currently shifting, as new evidence has emerged regarding the decreasing efficacy of old methods to guide fluid therapy. Several authors have validated the fact that the standard parameters of heart rate, blood pressure and urine output are neither predictive of nor able to be routinely manipulated to improve outcome (1). Numerous studies have definitively stated that the CVP is not an accurate measure of fluid responsiveness (3). There exists a very poor relationship between CVP and blood volume and recent data suggests that neither absolute CVP nor change in CVP reliably predicts the hemodynamic response to fluid challenge; in actuality, over 100 studies published to date have demonstrated no relationship between CVP and fluid responsiveness (4). Additionally, PACs are rarely placed in today’s medicine; a recent study recommended against the routine use of PACs in shock and against the use of static preload measurements alone to predict fluid responsiveness (3). Also, while there have been significant advancements in the field of critical care, the PAC has not been implicated in patient survival (35). The ESCAPE trial is the landmark study for the downfall of routine PAC use; performed from 2000-2003, it evaluated the use of the PAC in patients hospitalized for advanced heart failure. It found no difference in the primary endpoint of “days alive outside the hospital” between a PAC monitored group and a group monitored solely by clinical assessment (34). Additionally, more patients in the PAC group experienced adverse events, and possibly even increased morbidity and mortality. This trial was very influential in halting the practice of routine PAC use for decompensated heart failure; currently, it has been suggested that it no longer be used as part of routine management of the critically ill for conditions other than right heart failure, disorders causing abnormalities of pulmonary arterial pressure, and congenital heart disease (34, 35). It is true that both the PAC and the CVP have a role in today’s medicine, but it seems that in the field of EGDT and fluid resuscitation, a changing of the guard has emphasized finding less invasive ways to accurately monitor fluid responsiveness and tissue oxygen debt. This then begs the question, “what parameters do we use?” The debate now circles around using outdated technologies that the community is familiar with (either largely invasive PACs requiring expertise to place and manipulate, or CVPs which have been shown to be ineffective in the realm of guiding fluid therapy), or to challenge the paradigm with new technologies, devices, and parameters that have not yet found a niche in the model of EGDT as part of patient fluid resuscitation. 4 Stroke Volume Variation and Pulse Pressure Variation One of the new modalities being used utilizes arterial based systems of measurement as ways to evaluate fluid status and fluid responsiveness. Systolic pressure variation (the difference between maximum and minimum systolic pressure during one mechanical breath – also known as stroke volume variation, SVV) as well as pulse pressure variation (PPV) has been shown to predict fluid responsiveness (3). Pulse pressure variation is derived from the analysis of an arterial waveform, while SVV is derived from pulse contour analysis, and both have shown to be highly predictive of fluid responsiveness (4). These arterial based systems calculate dynamic parameters including SVV, PPV, SV, stroke volume index (SVI), CO, and cardiac index (CI). Studies have shown that SVV and PPV are more reliable indicators of volume responsiveness than CVP, PAOP, LVEDV index, etc (3). The FloTrac/Vigileo (Edwards Lifesciences, Irvine, CA, USA) is a minimally invasive device that calculates the stroke volume on the basis of the arterial waveform in combination with demographic data. This device is comprised of specialized pressure tubing and monitor connected to a typical radial arterial line. It assesses stroke volume (SV) using signal detection via a peripheral radial artery by analyzing the impact of vascular tone on pressure during a period of 20 seconds. It then adjusts for actual vascular tone at intervals of one minute (20). (It is worth noting that many original studies on the FloTrac/Vigileo were performed using an early version of the software which used a 10-minute adjustment period for vascular tone; the current one minute interval has enhanced the accuracy of the device significantly (20)). Recent studies have shown a good agreement compared to more invasive methods to determine cardiac output (9). One of the parameters calculated by the FloTrac/Vigileo is stroke volume variation (SVV). SVV is a good and easily obtainable predictor of fluid responsiveness, which can be used to guide fluid therapy in mechanically ventilated patients (10). Benes et al conducted a study concluding that optimization of intravascular volume during major abdominal surgery using SVV from the FloTrack/Vigileo is associated with better intraoperative hemodynamic stability and decrease in serum lactate concentration at the end of surgery; it also showed a lower incidence of postoperative complications (10). One study by Mayer and colleagues concluded that an optimization protocol based on flow-related hemodynamic parameters obtained with the FloTrac/Vigileo device reduced the duration of hospital stay and perioperative complications in high risk patients undergoing major abdominal surgery (9). However, two authors in this study are associated with Edwards Lifesciences, so more studies are needed to verify this data. A second family of devices that aim to assess SVV via transpulmonary thermodilution are the PiCCO Devices: the PiCCOplus, and PiCCO2 (Pulsion Medical Systems, Munich, Germany). The PiCCOplus system involves a standard subclavian or internal jugular central venous catheter and a 4F thermistortipped arterial catheter inserted into the left femoral artery. This catheter tip is advanced into the abdominal aorta and is connected to a stand-alone PiCCOplus monitor (20). Continuous cardiac output measurement can be achieved by injection of 20ml of ice-cold normal saline three times into the central venous catheter; this allows calibration of a pulse-contour-derived stroke volume via transpulmonary thermodilution(4). Incidentally, through its thermodilution function, this modality offers a measurement of Extravascular Lung Water Index (ELWI), which, following a significant increase, is a measure that a patient is no longer fluid-responsive (4). Finally, the PiCCO system functions 5 independently, regardless of mechanical or spontaneous respiratory status, and its simplicity and noninvasive character also makes it very suitable for pediatric populations (35). Hofer et al compared the assessment of SVV between the FloTrac/Vigileo and the PiCCOplus system in patients undergoing elective cardiac surgery; this study demonstrated that both systems were comparable predictors of SV changes related to a fluid shift maneuver in patients who had undergone off-pump coronary artery bypass grafting (CABG) (20). Other investigative studies involving the PiCCOplus device established that it could predict fluid responsiveness in patients with severe sepsis, those undergoing neurosurgery, and in cardiac patients with preserved and reduced left ventricular function (20). While many other studies have shown questionable correlation between PiCCO and invasive measurements of SVV, the PiCCO system, like the FloTrac/Vigileo has also undergone software improvements, which should be considered as well. While, anatomically speaking, transpulmonary thermodilution may give inaccurate measurements in patients with intracardiac shunts, aortic stenosis, aortic aneurysm, and extra corporeal circulation, its reliability in studies thus far warrants consideration as a method for EGDT (35). The conflicting data highlights the need for further study, like many of the other new, noninvasive modalities. Pulse pressure variation (PPV) is one of the parameters used as a way of estimating stroke volume, a key component of cardiac output. Several studies have shown that maximizing stroke volume by volume loading during high risk surgery may improve postoperative outcomes (8). This goal is quantified by calculating PPV; by minimizing PPV, one could derive that stroke volume has been maximized. The variation in arterial pulse pressure induced by mechanical ventilation is known to be a very accurate predictor of fluid responsiveness (8). The first method for assessing noninvasive arterial blood pressure using an electropneumatic control loop was the Finapres (Ohmeda Monitoring Systems, Englewood, CO); however it was found to not be a reliable substitute for invasive radial or brachial intraarterial pressure monitoring (19). More recently, the Infinity® CNAP™ SmartPod® (Dräger Medical AG & Co. KG, Lübeck, Germany) has become commercially available, and offers a real-time non-invasive estimate of mean arterial blood pressure (MAP) comparable to an invasive intraarterial device (19). This is a device that places two appropriately sized cuff sensors on the patient’s index and middle fingers; these are then connected to the CNAP device and the Infinity Delta monitor. One particular study demonstrated that both the CNAP (noninvasive) device and the invasive arterial device correlated significantly with percent change in stroke volume induced by volume expansion and concluded that both methods of measuring PPV predict fluid responsiveness (19). However, states of hypotension, shock, hypothermia, and other variables were not considered (19). Another study concluded that a value of ΔPP >11% has a sensitivity of at least 62% in predicting preload-dependent responders to a fluid challenge in mechanically ventilated patients during general anesthesia (19). Lopes et al concluded that by monitoring and minimizing PPV by volume loading during high-risk surgery decreases postoperative complications, the duration of mechanical ventilation, stay in the ICU, and hospital stay (8). In this case, the CNAP device offers a relatively minimally invasive technique to detect the adequacy of fluid resuscitation as part of a goal directed therapy in mechanically ventilated patients. A final device focused on SVV and PPV measurements is the ccNexfin (Edwards Lifesciences, CA, USA); it is a noninvasive hemodynamic monitor which provides real-time, beat-to-beat information on 6 cardiac output (CO), blood pressure (BP), and other hemodynamic parameters. The Nexfin device uses updated implementation of the Finapres method for noninvasive, beat-to-beat BP developed by Wesseling et al in 1995. It uses the pulsatile systolic area in combination with age-related aortic vascular characteristics for calculation of CO (25). One study showed reasonable agreement between CO measurements with the Nexfin and transthoracic Doppler echocardiography (25). Another study comparing the CO measurements obtained by the Nexfin monitor with esophageal doppler measurements showed a strong correlation between the two modalities, and concluded that the utility of Nexfin CO measurements was promising during general anesthesia (26). A third study evaluated the Nexfin in pediatric patients, and concluded that the Nexfin device accurately reflected the intra-arterial mean arterial pressure and diastolic arterial pressure, but underestimated the systolic arterial pressure curve. These results suggested that the Nexfin may be useful in low-to-moderate risk children who have a need for beat-to-beat measurements but in whom invasive monitoring is not indicated (27). Other research has been done in patients receiving mechanical ventilation after CABG procedures, and has demonstrated that the Nexfin device provided reliable, non-invasive systolic pulse variation measurements using the inflatable finger cuff (28). However, despite these promising results, a few studies have concluded that while the Nexfin is a reliable, safe, and convenient method for non-invasive arterial BP measurement, it is not interchangeable with transpulmonary thermodilution to monitor cardiac index (29). Generally, a major limitation of these systems involves the fact that they can be inaccurate with alterations in ventilator settings, mechanical versus spontaneous ventilation, dysrhythmias, and other variables that can all alter arterial based measurements. While one study reported that PPV was a reliable predictor of fluid responsiveness when the tidal volumes were at least 8 mL/kg, this still needs to be replicated (4). To add to this, many studies suggest that in spontaneously breathing patients, pulse pressure is not sufficient to detect changes in stroke volume, and as such, these modalities are only validated for patients who are mechanically ventilated (4). However, a study from Cecconi and colleagues in 2011 out of Italy introduced a randomized control trial evaluating EGDT using FloTrac/Vigileo monitoring in awake patients under spinal anesthesia; it concluded that GDT during total hip replacement surgery using spinal anesthesia in awake patients is feasible and leads to a different type of hemodynamic monitoring (12). Their outcomes suggest that GDT may improve outcomes in this population by decreasing the rate of minor postoperative complications (12). This is an exciting possibility, and more research is expected to investigate further. So, in the case of arterial based parameters of volume status, they are only one point in a series of measurements indicating a patients complete volume picture, as they are typically calculated values that can be altered by many variables. Central Venous Oxygen Saturation Continuous mixed venous oxygen monitoring along with central venous pressure measurements have shown benefit in the emergency department and ICU in management of patients with septic shock (3). The major reason this marker is not more widely used is its invasive nature; mixed venous oxygen saturation requires sampling of blood in the pulmonary artery with a PAC (35). Decrease in venous saturation in the absence of arterial hypoxemia is an indirect indicator of poor CO, and in turn, tissue perfusion (3). While normal SVO2 is approximately 70%, a very low SVO2 is indicative of excessive 7 extraction of oxygen by the blood, suggesting under-resuscitation (35). However, the use of venous or tissue oximetry during emergency general surgery has not gained following due to the dynamic response of these systems; the method may be too slow to guide therapy during active hemorrhage (3). Jones et al tested a noninferiority hypothesis between lactate clearance and central venous oxygen saturation (SVO2) as goals of early sepsis resuscitation (6). This study concluded that there was no difference in mortality for patients with severe sepsis and septic shock resuscitated with a protocol that used lactate clearance compared to a protocol using SVO2 as the method of measuring total body oxygen metabolism (6). Because of the need to place a PAC to obtain mixed venous oxygen saturation, the use of central venous blood saturation has recently gained popularity; however, as CO is our primary marker for tissue perfusion, this method is being overtaken by non-invasive methods that provide the same CO parameter (35). Transesophageal and Transthoracic Echocardiography Transesophageal (TEE) and transthoracic (TTE) echocardiography has gained popularity in the assessment of ventricular function and volume status in high-risk patients (3). Cardiac output can be extrapolated from velocity time intervals and outflow tract measurements (3). Feissel et al demonstrated that the respiratory changes in aortic blood velocity as measured by TEE predicted fluid responsiveness in mechanically ventilated patients, distinguishing it as possibly being more useful than arterial pressure based forms of monitoring (4). Also, cyclic changes in superior and inferior vena-caval diameter as measured by TTE have been shown to adequately predict fluid responsiveness; the distensibility of the inferior vena cava (IVC) and superior vena cava (SVC) were important parameters (4). However, the Doppler requires both high levels of experience and adequate viewing angles for proper measurements, which can be exceedingly difficult in the operating room. This places TTE and TEE echocardiography in the category of a good diagnostic tool but a poor device to actively guide therapy. Esophageal Doppler Esophageal Doppler (Deltex Medical Ltd., Chichester, UK) monitoring views the descending aorta and can use ultrasound transducers to measure blood flow velocity. The probe is inserted orally or nasally to the midthoracic level (between the 5th and 6th thoracic vertebra). At this level, the aorta and esophagus run approximately parallel, allowing interrogation of the descending aortic blood flow (22). On the basis of the measured frequency shift between the emitted and received ultrasound frequency, blood flow velocity is determined (22). From this velocity, combined with the simultaneously measured systolic ejection time, CO, preload, afterload, contractility, and other hemodynamic variables can be calculated. It offers providers a clinical useful alternative to thermodilution in determination of CO. Improved outcomes have been demonstrated involving faster return of GI function, a reduction in postoperative complications, and shortened hospital stay when esophageal doppler was used fur goaldirected fluid administration to maximize CI (1). However, this is a device that utilizes algorithms developed from studies mainly on healthy individuals, so more studies are needed. Also, this modality, like TTE and TEE may not be useful in a transient state such as extreme hemorrhaging or severe shock (3). Nevertheless, direct examination of cardiac filling and function is possible; it simply may not be 8 optimal in the setting of ongoing monitoring except over a very short period of time (3). Some studies should it has little bias and high agreement when compared with a PAC for monitoring changes in CO; other studies show limited agreement between transesophageal doppler and reference methods (1). However, generally, esophageal doppler has been shown to accurately follow changes in CO over time, making it useful for trend monitoring (22). Various studies have demonstrated a reduced postoperative morbidity and shorter length of hospital stay in patients managed with esophageal doppler compared with conventional clinical management (22). Lactate Levels/Lactate Clearance Lactate levels as well as lactate clearance are another modality of evaluating the perfusion status of a patient and response to fluid therapy. Lactate is the product of anaerobic metabolism; in the instance the body’s tissues are being hypoperfused, and in turn, under-oxygenated, lactate is produced and can be used as a measure a derivation of oxygen debt (6). Jones et al tested a noninferiority hypothesis between lactate clearance and central venous oxygen saturation (SVO2) as goals of early sepsis resuscitation (6). This study concluded that there was no difference in mortality for patients with severe sepsis and septic shock resuscitated with a protocol that used lactate clearance compared to a protocol using SVO2 as the method of measuring total body oxygen metabolism (6). It is of note in this instance that lactate clearance can be obtained much easier and is less costly and has fewer complications than SVO2 measurements. Microcirculation Evaluation There are many monitoring methods within the field of microcirculation evaluation, including Orthogonal Polarization Spectral and Sidestream Darkfield (OPS/SDF) imaging techniques, Near-infrared Spectroscopy (NIRS), and PCO2 derived measurements like gastric tonometry (18). The microcirculation plays a fundamental role in gas and nutrient exchange; vascular tone is constantly changing to adapt to changing oxygen supply and demand. In disease states, the microcirculation is affected by an increased permeability; this is a positive adaptation in the sense that it facilitates the inflammatory response, endothelial activation, and specifically, leukocyte diapedesis (18). However, this increased permeability has an effect on cellular oxygenation as well. Local modulaton of arteiolar tone is responsible for adapting microvascular perfusion to local oxygen demand; however, the state of these arterioles and microvascular blood flow is altered in sepsis and low flow states (18). Admist low flow conditions such as hemorrhage or cardiogenic shock, there exists a substantial decrease in functional capillary density, which causes an increase in the diffusion distance of oxygen (18). The severity of this functional capillary density, seen in sepsis as well as low flow states, is directly related to poor outcomes (18). The technique involves applying a light source to the tissue; a selected wavelength is absorbed by the hemoglobin-containing red blood cells and that information is projected on a screen. At that point, vascular density, heterogeneity of perfusion and microvascular blood flow can be evaluated as a point of care measurement that quantifies flow (18). While the utility of this technique is limited by the fact that it can only be applied in organs that can be submitted to transillumination, it has been studied intraoperatively to evaluate the brain, lungs, tongue, liver, and gut (18). In intact patients, the skin, 9 conjunctiva, gingiva, sublingual area, ileostomies, colostomies, and rectal mucosa can all serve as monitoring locations. One of the important microcirculatory alterations involves the homogeneity or heterogeneity of the circulation. Under normal conditions, heterogeneity is minimal and perfusion is matched with metabolism, which improves conditions in hypoxic or low flow areas (18). However, during a septic or low flow state, the microcirculatory alterations normally present to perserve oxygen delivery are dysfunctional, creating a heterogeneity of microperfusion. This heterogeneity is associated with variations in oxygen diffusion distance; the result of this is an oxygen extraction defect and an overall increase in mixed venous O2 (18). Physiologically speaking, tissues to not tolerate this heterogeneity well; they actually tolerate a homogeneous decrease in blood flow better than conditions when uniformity of oxygen delivery is lost. Clinically, the goal of microcirculation monitoring is to identify these areas of heterogeneity and alter patient management appropriately until improvement is seen. Treciak et al hypothesized that changes in microcirculatory flow during resuscitation are associated with changes in organ failure over the first 24 hours of sepsis therapy (7). In this study, sublingual microcirculation was visualized and direct and indirect assessments of tissue perfusion were monitored; these assessments have been demonstrated to predict mortality in critical patients, including those with sepsis (7). The extent of this technique involves merely placing a probe in the sublingual space and obtaining video sequences for twenty seconds from five sites; this data is then quantified into a microcirculatory flow index (MFI), which can be used to quantify the presence or absence of adequate perfusion (7). They found that early increases in microcirculatory flow during protocol-directed resuscitation were associated with reduced organ failure at 24 hours in patients with sepsis (7). While this technology is increasingly promising in the hopes of offering a minimally invasive technique to guide resuscitation, more studies are needed to verify these results. Near-infrared spectroscopy (NIRS) via the EQUINOX rSO2 (Nonin Medical Inc.) is a noninvasive technology that continuously monitors regional tissue oxygenation by evaluation of the microcirculation as well. It utilizes near-infrared light to measure oxy- and deoxyhemogloin, myoglobin, and cytochrome aa3 in tissues (18). Initially used as an assessment of oxygen saturation of the brain, its current expansion into evaluation of oxygenation of tissues other than the brain is promising. There is also growing evidence for the larger applicability of NIRS as an estimate of systemic venous saturation in correspondence with the adequacy of the circulatory status. A number of its limitations have raised questions regarding the clinical utility of cerebral oximetry monitoring. However, a number of clinical studies and case reports have demonstrated that despite such limitations, the ability of cerebral oximetry monitoring to detect otherwise clinically silent episodes of cerebral ischemia in a variety of clinical settings renders it an important safeguard for cerebral function (21). For many of the NIRS systems, accuracy on the FDA application was compared relative to a weighted average of arterial and jugular bulb O2 saturation. In adults and children, the device is not that accurate (+10-15%) on an absolute level of oxygenation, but is fairly accurate (+5%) on a change in oxygenation. In other words, the device indicates a change in oxygenation accurately but does not indicate accurately what the oxygenation actually is; NIRS does not measure microcirculatory blood flow, but it does provide quantitative information on microvascular flow within a few minutes, and can be helpful if used as a 10 method for trending variations in flow (18, 21). An additional study by Lima et al demonstrated that the persistence of low tissue oxygenation saturation (using a thenar eminence NIRS device) during the early resuscitation phase is associated with more severe organ dysfunction (2). Patients in this study who failed to normalize tissue oxygen saturation with resuscitation had a higher disease severity, which further supports the function of NIRS devices in establishing trends of perfusion (2). There is an increasing interest in the utilization of oximetry sensors in somatic sites, including for volume resuscitation in traumatic shock, dehydrated pediatric patients, as an estimate of splanchnic perfusion following cardiac surgery, and other applications (21). Somatic NIRS has been found to correlate with other indices of tissue perfusion, has been used to confirm the development of compartment syndrome, and as far as comparing liver tissue oxygenation with SVO2 and intestinal perfusion with gastric mucosa pH (21). However, when using peripherally, it must be kept in mind that NIRS-derived measurements are influenced by adipose tissue thickness, as well as the presence of edema; because of this the thenar eminence has been used in many studies, as it is less influenced by an increase in fluid content or body mass index (18). However, the influence of temperature and vasoactive substances needs further attention as well as the relationship between peripheral and central microvascular beds as part of NIRS-derived measurements (18). The major concept when considering evaluation of tissue oxygenation relates to the fact that measurements of O2 tension or saturation in a piece of tissue reflect the balance between O2 delivery and consumption in that particular tissue (18). The Lima et al study referenced above also demonstrated that there was no relationship between tissue oxygen saturation values and global hemodynamic variables, suggesting they cannot accurately be extrapolated to represent systemic oxygenation (2). Finally, these measurements are affected by blood flow to the particular tissue, but also hemoglobin content, arterial PO2, and O2 consumption, hindering their utility as global markers of adequacy of perfusion (18). Gastric Tonometry is a third method of evaluating the adequacy of the microcirculation in addition to OPS/SDF and NIRS. The theory behind gastric tonometry is the gut is sensitive to ischemia, and periods of hypoperfusion may cause the release of inflammatory cytokines and bacterial translocation; this can in turn cause damage to remote organs (24). However, if a provider were to monitor perfusion of the gut and help minimize or prevent episodes of hypoperfusion and ischemia, this could improve outcomes in critically ill patients (24). Gastric tonometry measures PCO2 locally in the gastric mucosa with a tonometer placed in the lumen of the stomach; as the CO2 diffuses from the mucosa into the lumen of the stomach, it can be measured and extrapolated into meaningful data (24). At that point, saline solution is anaerobically injected in the device’s balloon; when combined with the CO2 from the gut lumen, is withdrawn and analyzed in a blood gas analyzer. Another method involves injecting air into the balloon; the PCO2 is determined by an infrared detector on a semicontinuous basis (24). This method of using gastric tonometry to assess gastric PCO2 has replaced measurements of gastric pH in some circles, as many say that gastric pH calculations are based on certain assumptions and can be confounded by many factors. However, gastric tonometry is not without its shortcomings – one of the major problems involves the fact that the value representing dysoxia (when oxygen delivery is insufficient to meet metabolic demand) is unknown (24). Also, the use of this monitor in states where tissue blood flow is normal or elevated may not be particularly helpful; however, when considering 11 hypovolemic patients (secondary to hemorrhagic shock, septic shock, etc.), the tonometer has been shown to be a useful tool to guide therapy by some authors (24). Levy et al demonstrated that a gastric PCO2 gap above 20mmHg discriminated survivors from non-survivors (18). Other authors state the technique has been relatively abandoned due to technical problems (18). However, as its use has not been associated with an increase in mortality, when used appropriately, some argue it can be a useful clinical adjunct. Gastric pH, on the other hand, is consistently failing to show benefit in terms of a resuscitation goal. A study by Palizas et al evaluating the outcome of septic shock patients with resuscitation protocols guided by gastric pH monitoring versus CI monitoring failed to demonstrate any survival benefit using gastric pH compared to CI (23). One of the likely problem areas they addressed when considering gastric pH is that its calculation includes arterial bicarbonate, which is a systemic parameter independent of gut perfusion (23). However, there still is potential in the consideration of gastric pH; Palizas et al addressed the fact that normalization of gastric pH within 24 hours of resuscitation was a strong signal of therapeutic success, while a persistent low gastric pH despite treatment is associated with a very bad prognosis (23). In light of this, current research suggests that gastric pH may lend itself as a marker for improvement when used as a trend rather than a resuscitation goal in itself. It can be argued that further studies could evaluate a potential adjunctive role of tonometry-guided resuscitation at earlier stages of septic shock (23). De Backer et al evaluated the sublingual microcirculation in 50 patients with severe sepsis and in a cohort of healthy volunteers and non-infected ICU controls. A significant decrease in vessel density and a significant proportion of underperfused small vessels were noted in septic patients (18). This study, along with others, highlights the fact that microcirculatory alterations were more severe in nonsurvivors than in survivors; additionally, those who survived exhibited a rapid resolution of microcirculatory changes to therapy in relation to non-survivors. Patients who later died from acute circulatory failure or organ failure following recovery from shock all exhibited a persistence of microcirculatory heterogeneity and alterations (18). These studies strongly suggest that microcirculatory alterations are implicated in the development of organ failure, and early improvement in microvascular perfusion in response to therapy was associated with an improvement in organ function. Overall, several clinical studies using various methods of monitoring the microcirculation have shows that patients with severe sepsis frequently have profound alterations in microvascular reactivity, and that these alterations are associated with a high risk of organ dysfunction and death (18). Impedance Cardiography and Electrical Cardiometry Thoracic bioimpedance (or impedance cardiography) is a non-invasive technique developed originally to measure cardiac output in astronauts (35). It involves measurements of impedance with a series of sensing electrodes following delivery of low-amplitude, high-frequency electrical current across the thorax; hemodynamic measurements of CO relate to a change in the thoracic electrical conductivity to changes in the thoracic aortic blood volume and flow (35). It is a non-invasive method, arguably analogous to the Fick method or thermodilution techniques, which measures parameters including CO, 12 SV, contractility, SVR, and thoracic fluid content in patients who are not appropriate for invasive monitoring or in whom it is contraindicated. The NICCOMO (APC Cardiovascular) is a device based on the principle of impedance cardiography (ICG) and is comprised of a high frequency sine wave generator and four dual electrode “stickers” that are used to establish electrical contact with the body. With ICG, the placement of four dual disposable sensors on the neck and chest are used to transmit and detect electrical and impedance changes in the thorax, which are used to measure and calculate hemodynamic parameters. The CO as measured by bioreactance has been shown to be highly correlated with that measured by thermodilution and pulse contour analysis; this could accurately predict fluid responsiveness from changes in CO during passive leg raise (PLR). It has an algorithm with user prompts and an interface that rapidly facilitates the performance of a PLR maneuver (4). In a study addressing the equivalence of bioimpedance and thermodilution methods for CO measurement in patients with advanced, decompensated chronic heart failure, the determinations of CO and CI by both methods were significantly correlated, suggesting a clinical utility for bioimpedance modalities in these patients (30). Conversely, it has also been determined by competing research that in comparing bioimpedance, thermodilution and the Fick method for calculating CO, the three practices are not interchangeable in critically ill patients due to a lack of correlation within the study (31). Another study examined a particular bioimpedance device, the BioZ (CardioDynamics, San Diego, CA), and compared it to invasively measured hemodynamics. The study found a modest correlation between ICG and invasively measured CO, but a poor agreement between impedance cardiography and invasively measured hemodynamic profiles. The study found that ICG did not have a prognostic utility in this particular patient population (32). Finally, an additional study comparing the correlation between impedance cardiography (ICG) and transesophageal Doppler echocardiography demonstrated an agreement between the two techniques and concluded that they can be used interchangeably (33). This study used electrical velocimetry to provide a new algorithm to calculate CO from variations in thoracic electrical bioimpedance (33). One of the major parameters addressed by impedance cardiography is stroke volume (SV). It is an important hemodynamic parameter characterizing how well the heart is functioning mechanically. Additionally, reliable measures of SV during transient events (such as atrial fibrillation, or extrasystole) are very sought after, as many other systems cannot accurately function under those physiologic circumstances (35). This ability to address SV suggests that ICG could be a good tool for screening patients with left ventricular systolic dysfunction (35). It is also a reliable measure for assessing proload status, and could be a cost effective, non-invasive method for follow up of patients with pulmonary hypertension (35). While many researchers admit that it is still difficult to find the formula for SV calculations which will provide acceptable accuracy regardless of the condition of the patient, more evidence is needed. At this point there is some agreement that when comparing a patient to him or herself, this device can be helpful, but at this early point should not be used as a comparison between patients (35). All this being said, there are 2 significant problems when using bioimpedance technology: the effects of excessive lung water (pulmonary edema), and changes in peripheral resistance. Both affect the reliability of CO measurements. These negative influences help to explain the repeatedly poor results from validation studies in critically ill and septic patients (36). 13 To overcome some of the limitations and clinical confounders of bioimpedance, electrical bioreactance (or electrical cardiometry, or electrical velocimetry) has been developed as a similar but alternate way to measure CO; newer methods of processing the impedance signal were identified. The Aesculon device (Osypka Medical Services, Berlin,Germany) uses the second derivative rather than the slope of the impedance wave to measure aortic blood flow, a method the Osypka company calls electrical velocimetry or cardiometry (36). The ICON device functions based on electrical cardiometry, a method for the non-invasive determination of stroke volume (SV), cardiac output (CO), and other hemodynamic parameters in adults, children, and neonates. Because of similar setup, electrical cardiometry (EC) is often confused with the traditional bioimpedance technology most commonly known as Impedance Cardiography (ICG). Though both methods use sensors placed on the thorax, traditional bioimpedance or ICG methods rely on the assumption of periodical volumetric changes in the aorta to determine stroke volume (SV) and cardiac output (CO). In short, ICG attributes the steep increase in the conductivity waveform to a volumetric expansion of the aorta during systole, while EC contributes the increase in conductivity to the orientation change of the RBCs to determine the velocity of the blood flow. Similar to FM radio, the signal is less susceptible to interference from chest wall movement, chest wall and lung edema, and pleural fluid (35). Thus, the algorithm and evident accuracy of EC compared to ICG is what separates the two methods. EC can be used as a method for measuring cardiac output in a wide spectrum of patient conditions and patient populations including neonates and children, while ICG is limited to relatively healthy adults. A final device known as the CheetahTM monitor (Cheetah Medical, Tel Aviv, Israel and Portland, Oregon) has shown acceptable correlation in several studies related to critically ill patients (35). This device is comprised of a high frequency sine wave generator and four dual electrodes that are used to establish electrical contact with the body. It has been shown to predict the need for hospitalization in sepsis, and has shown good correlation between pulse contour analysis and PAC transpulmonary thermodilution in postoperative cardiac surgery patients (4, 35). In these studies is providing reliable measurements of SV, CI, and PVR. Conclusion Despite much research to date, there are many goals facing the field of EGDT, namely, evidence that sheds light on how new technologies fit into large scale patient resuscitation. We need further insight into the modalities we are less familiar with, but also need to consider that even these new modalities have already been significantly improved upon, and that current research condemning them could actually be considered out of date. New software methods, new applications, and utility for more specific patient populations could be the next step to finding a niche for many of these monitoring techniques, instead of simply rendering them “inferior” to dogmatic methods. The major consideration lies in the fact that less invasive devices could be more widely used and provide patient monitoring in areas without the capability to use invasive techniques. Currently, only a small proportion (fewer than 15%) of high risk patients is admitted to an intensive care unit (1). This is a powerful statistic highlighting the widespread need for non-invasive monitoring modalities. As an example, it is 14 commonly viewed as a deficiency if a device is not accurate or does not have utility in every patient population; however, it should be considered that the functionality of a device is exponentially larger when it is a non-invasive form of monitoring. It can be used outside the intensive care units, and can be used with ease. So, while this paper has shown both sides of the argument for many of these devices, it will serve our patients better to continue to research; they may not be efficacious in every patient, but it is quite possible that they can be used in specific patient cohorts and improve outcome for many. It has been well established that every device should be used as part of an entire clinical picture to treat a patient effectively. Each device is never going to be perfect; that is where the knowledge and skill of an experienced medical provider can apply knowledge from each device into a goal directed protocol to improve outcomes. 15 References 1. Lees, N., Hamilton, M., Rhodes, A. Clinical Review: Goal-Directed Therapy in High Risk Surgical Patients. Journal Crit Care, 2009; 13 (5): 231. 2. Lima, A., van Brommel, J., Jansen, T.C., Inge, D., Bakker, J. Low Tissue Oxygen Saturation at the End of Early Goal-Directed Therapy is Associated with Worse Outcome in Critically Ill Patients. Crit Care. 2009; 13(suppl 5): S13. 3. Fouche, Y., Sikorski, R., Dutton, R. Changing Paradigms in Surgical Resuscitation. Critical Care Medicine – vol 38, issue 9, suppl (Sept 2010). 4. Marik, P., Monnet, X., Teboul, J. Hemodynamic Parameters to Guide Fluid Therapy. Ann Intensive Care. 1186/2110-5820; March 21, 2011; 1: 1. 5. Dalfino, L., Gigilo, M.T., Puntillo, G., Marucci, M., Brienza, N. Haemodynamic Goal-Directed Therapy and Postoperative Infections: Earlier is Better. A Systematic Review and Metanalysis. Crit Care. 2011; 15(3): R154. 6. Jones, A., Shapiro, N., Treciak, S., Arnold, R., Claremont, H., Kline, J. Lactate Clearance Vs. Central Venous Oxygen Saturation as Goals of Early Sepsis Therapy: A randomized Clinical Trial. JAMA 2010 February 24:303(8): 739-746. 7. Trzeciak, S., McCoy, J.V., Dellinger, R.P., Arnold, R.C., Rizzuto, M., Abate, N.L., Shapiro, N.L., Parrillo, J.E., Hollenberg., S. M. Early Increases in Microcirculatory Perfusion During ProtocolDirected Resuscitation are Associated with Reduced Multi-Organ Failure at 24 Hours in Patients with Sepsis. Intensive Care Med. 2008 December; 34(12):2210-2217. 8. Lopes, M., OIiveiera, M., Pereira, V., Lemos, I., Auler, J., Michard, F. Goal-Directed Fluid Management Based on Pulse Pressure Variation Monitoring During High-Risk Surgery: A Pilot Randomized Controlled Trial. Journal Crit Care 2007; 11(5); R100. 9. Mayer, J., Boldt, J., Mengistu, A., Rohm, K., Suttner, S. Goal-directed Intraoperative Therapy Based on Autocalibrated Arterial Pressure Waveform Analysis Reduces Hospital Stay in High-Risk Surgical Patients: A Randomized, Controlled Trial. Journal Crit Care, 2010; 14(1): R18. 10. Benes, J., Chytra, I., Altmann, P., Hluchy, M., Svitak, R., Pradi, R., Stepan, M. Intraoperative Fluid Optimization Using Stroke Volume Variation in High Risk Surgical Patients: Results of Prospective Randomized Study. Journal Crit Care, 2010; 14 (3), R118. 11. Hiltebrand, L., Kimberger, O., Amberger, M., Brandt, S., Kurz, A., Sigirdsson, G. Crystalloids Versus Colloids for Goal-Directed Fluid Therapy in Major Therapy. Journal Crit Care, 2009; 13(2) R40. 12. Cecconi, M., Fasano, N., Langiano, N., Divella, M., Rhodes, A., Della Rocca, G. Goal-Directed Haemodynamic Therapy During Elective Total Hip Arthroplasty Under Regional Anesthesia. Crit Care. 2011; 15(3): R132. 13. Drage, S., Boyd, O. Perioperative Goal Directed Hemodynamic Therapy – Do it, Bin It, Finally Investigate it Properly? Journal Crit Care, 2007; 11(5) 170. 14. Ho, B., Bellomo, R., McGain, F., Jones,m D., Naka, T., Wan, L., Braitberg, G. The Incidence and Outcome of Septic Shock Patients in the Absence of Early-Goal Directed Therapy. Crit Care. 1006; 10(3); R80. 16 15. Stewart, R., Park, P., Hunt, J., McIntyre, R. McCarthy, J., Zarzabal, L., Michalek, J. Less Is More: Improved Outcomes in Surgical Patients with Conservative Fluid Administration and Central Venous Catheter Monitoring. Journal of the American College of Surgeons – Vol 208, Issue 5 (May 2009). 16. Futeir, E., Robin, E., Jabaudon, M., Guerin, R., Petit, A., Bazin, J., Constantin, J., Vallet, B. Central Venous O2 Saturation and Venous-to-Arterial CO2 Difference as Complementary Tools for GoalDirected Therapy During High-Risk Surgery. Crit Care. 2010; 14(5): R193. 17. Chacko, A., Hood, E.D., Zern, B.J., Muzykantov, V.R. Targeted Nanocarriers for Imaging and Therapy of Vascular Inflammation. Curr Opin Colloid Interface Sci. 2011 June; 16(3): 215-227. 18. Backer, D., Ospina-Tascon, G., Salgado, D., Favory, R., Creteur, J., Vincent, J. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med. July 2010. DOI 10.1007/s00134-010-2005-3. 19. Biais M, Stecken L, Ottolenghi L, Roullet S, Quinart A, Masson F, Sztark F. The ability of pulse pressure variations obtained with CNAP™ device to predict fluid responsiveness in the operating room. Anesth Analg. 2011 Sep; 113(3):523-8. 20. 21. 22. 23. 24. 25. 26. 27. 28. Hofer, C., Senn, A., Weibel, L., Zollinger, A. Assessment of stroke volume variation for prediction of fluid responsiveness using the modified FloTrac™ and PiCCOplus™ system. Critical Care 2008, 12:R82. Murkin, M., Arango, M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br. J. Anaesth. (2009) 103 (suppl 1): i3-i13. Schober, P., Loer, S., Schwarte, L. Perioperative Hemodynamic Monitoring with Transesophageal Doppler Technology. Anesthesia and Analgesia, Vol. 109, No. 2, August 2009. Palizas, F., Dubin, A., Regueira, T., Bruhn, A., Knobel, E., Lazzeri, S., Baredes, N., Hernández, G. Gastric tonometry versus cardiac index as resuscitation goals in septic shock: a multicenter, randomized, controlled trial. Critical Care 2009, 13:R44. Heard, S. Gastric Tonometry: The Hemodynamic Monitor of Choice (Pro). CHEST 2003; 123:469S–474S. Van der Spoel, A., Voogel, A., Folkers, A., Boer, C. Comparison of noninvasive continuous aarterial waveform analysis (Nexfin) with transthoracic Doppler echocardiography for monitoring of cardiac output. Journal of Clinical Anesthesia. Volume 24, Issue 4 (June 2012). Chen, G., Meng, L., Alexander, B., Phuong, N., Kain, Z. Comparison of noninvasive cardiac output measurements using the Nexfin monitoring device and the esophageal Doppler. Journal of Clinical Anesthesia. Volume 24, Issue 4 (June 2012). Garnier, R., van der Spoel, A., Sibarani-Ponsen, R., Markhorst, D., Boer, D. Level of agreement between Nexfin non-invasive arterial pressure with invasive arterial pressure measurements in children. British Journal of Anesthesia 109 (4): 609-15 (2012). Landsdorp, B>, Ouweneel, D., de Keijzer, A., van der Hoeven, J., Lemson, J., Pickkers, P. Non-invasive measurement of pulse pressure variation and systolic pressure variation using a finger cuff corresponds with intra-arterial measurement. British Journal of Anesthesia, 107 (4): 540-5 (2011). 17 29. 30. 31. 32. 33. 34. 35. 36. Fischer, M., Carjaliu, I., Avram, R., Massetti, M., Gerard, J., Hanouz, J., Fellahi, J. Non-invasive continuous arterial pressure and cardiac index monitoring with Nexfin after cardiac surgery. British Journal of Anesthesia 109 (4): 514-21 (2012). Albert, N., Hail, M., Li, J., Young, J., Equivalence of the Bioimpedance and Thermodilution Methods in Measeuring Cardiac Output in Hospitalized Patients with Advanced, Decompensated Chronic Heart Failure. Am J Crit Care 2004; 13: 469-479. Ejgoren, M., Barbee, D. Comparison of Cardiac Output Determined by Bioimpedance, Thermodilution, and the Fick Method. Am J Crit Care 2005; 14: 40-45. Kamath, S., Drazner, M., Tasissa, G., Rogers, J., Warner Stevenson, L., Yancy, C. Correlation of impedance cardiography with invasive hemodynamic measurements in patient with advanced heart failure: The BioImpedance CardioGraphy (BIG) substudy of the Evaluation Study of Congestive Heart Failure and Pulmonary Artery Catheterization Effectiveness (ESCAPE) Trial. American Heart Journal, Volume 158, Issue 2 (August, 2009). Schmidt, C., Theilmeier, G., Van Aken, H., Korsmeier, P., Wirtz, S., Berendes, E., Hoffmeier, A., Meissner, A. Comparison of electrical velocimetry and transoesophageal Doppler echocardiography for measuring stroke volume and cardiac output. British Journal of Anesthesia 95 (5): 603-10 (2005). Leier, D. Invasive Hemodynamic Monitoring the Aftermath of the ESCAPE Trial. Cardiology Clinics – Volume 25, Issue 4. November 2007. Cybulski, G., Strasz, A., Niewiadomski, W., Gasiorowska, A. Impedance Cardiography: Recent Advancements. Cardiology Journal, 2012. Vol 19, No. 5, pp.550-556. 10.5603/CJ.2012.0104. Critchley, L., Lee, A., Ho, M. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesthesia and Analgesia, November 2010. Issue 111, Volume 5. 18