NABIM Wheat Allergy and Intolerance Report
advertisement

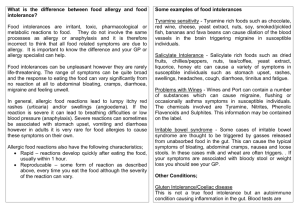
Flour Advisory Bureau Wheat Allergy and Intolerance Review, January 2010 Executive media summary Purpose of the review To evaluate the prevalence of self reported food allergy / intolerance versus actual (medically diagnosed) food allergy / intolerance. With a particular focus on allergy and intolerance to wheat. To highlight and succinctly explain, the difference between wheat allergy, wheat intolerance and coeliac disease. To highlight the importance of proper diagnosis of these conditions, and how a wheat/gluten free diet can be safely managed. Expert involvement The report has been written by Heather Mackenzie B.Sc. PGCert. PhD. Research Associate, University of Portsmouth Heather was supported by Carina Venter B.Sc. Dietetetics Post Grad Dip in Allergy, PhD Senior Research Fellow, University of Portsmouth and also a Senior Allergy Dietitian at The David Hide Asthma and Allergy Research Centre, Isle of Wight. Overview Research shows that up to 20% of adults think they suffer from food allergy or food intolerance. However, evidence suggests that the real prevalence of food allergy and intolerance is less than 2%. It is unknown how many people truly suffer from wheat allergy or wheat intolerance, and how many people are avoiding wheat for no sound medical reason. However, the limited evidence available suggests that for wheat allergy and intolerance the pattern reflects that of food allergy and intolerance generally i.e. self-report is higher than true prevalence. The prevalence of coeliac disease is better researched; evidence suggests that the overall prevalence is approximately approximately 0.8-1.9% of the adult population and 1% of the child population in the UK. Wheat allergy, wheat intolerance and coeliac disease must be diagnosed by a qualified medical professional; self-diagnosis and other diagnostic tests (not conducted by qualified medical professionals) are not reliable. If not properly managed, wheat avoidance can have an impact on nutritional intake and quality of life, and should not be undertaken lightly or without a confirmed diagnosis. Key points Wheat allergy is a reaction to wheat involving an antibody called IgE (Immunoglobulin E). Typically symptoms occur within 2 hours of eating wheat and range from mild to severe, including hives, itching, gastrointestinal symptoms and wheezing. Diagnosis by a medical professional involves the taking of a clinical history followed by skin prick or blood tests and possibly an elimination diet and food challenge. There is a large cross reactivity between wheat and grass; people may show a positive skin prick test to wheat and grass, yet be tolerating wheat in their diet. Wheat intolerance does not involve the immune system and symptoms (often similar to those of allergy but usually less severe), tend to occur after a longer period of time, and after ingestion of a larger amount of food. Diagnosis can only be confirmed through eliminating and then reintroducing wheat into the diet while monitoring reported symptoms. Coeliac disease is immune-mediated, but different antibodies are involved than in wheat allergy. Coeliac disease is a spectrum; there is a wide variation in symptoms experienced, which can include weight loss, diarrhoea, stomach cramps and iron deficiency. Diagnosis will usually involve a blood test and a biopsy to look for damage to the small intestine. The existence of sensitivity to gluten (other than CD) is also currently being investigated. Wheat or other gluten avoidance requires careful planning to ensure the diet contains alternative sources of carbohydrate and fibre needed for a healthy digestion. Good alternatives to wheat include corn, rice, potato, cassava, yam, quinoa, millet, gram (chick pea), sago, tapioca, amaranth and buckwheat. Barley, rye and oats may be tolerated by some individuals with wheat allergy or intolerance (on the advice of a healthcare professional). However, barley and rye must be avoided by those with coeliac disease. Oats may be tolerated by some individuals with coeliac disease (on the advice of a healthcare professional). Avoiding wheat can be disruptive and affect the social life of the individual. Parents of children with food allergies may feel anxious about their child’s health and also have extra demands placed on their time. It's critical therefore that wheat intolerance or allergy is correctly diagnosed and that people do not remove wheat from their diet unnecessarily. Summary In summary, it is reported that many people think they may suffer from wheat allergy or wheat intolerance. However, research suggests that this does not reflect the actual lower prevalence of wheat allergy and intolerance and that wheat allergy and intolerance may not be that prevalent. In children, research suggests that (dependent on age) between 0.0% and 0.4% have wheat allergy or intolerance. In adults we know that 1.4-1.8% of adults are allergic to any food and that allergy to wheat is less prevalent than allergies to other foods (Young, Stoneham, Petruckevitch, Barton & Rona, 1994). Wheat avoidance can have an impact on nutritional intake and quality of life, and studies investigating these are urgently needed. Contacts / Further Information Flour Advisory Bureau Press Office Mars Webb/Philippa Taylor/Wendy Marshall mars@marswebbpr.co.uk Tel: 077177 18063 Tel: 028 4483 2083 WendyMarshall@nabim.org.uk Tel: 020 7493 2521 Carina Venter (report author) via FAB Press Office Philippa@grandunionpr.com Tel: 01442 824844 Tel: 07866 480700 Websites www.fabflour.co.uk COELIAC SOCIETY? ST GEORGES HOSPITAL? ANY OTHERS? Report Copy of report available and included in press packs



![Form: Medical history: for new patients [Form]](http://s3.studylib.net/store/data/007605872_2-8e9e11d5356e956dfeae2f990eec56a6-300x300.png)