Interfacility Transport Protocol
advertisement

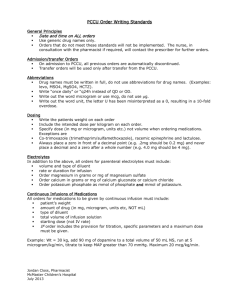
Interfacility Transport Protocol Acceptance of Interfacility Transfers Flow Sheet Original date: June 25, 2007 Take report from hospital personnel Accept transfer? Yes No Discuss with transferring doctor. Accept transfer? Notify Battalion Chief of acceptance. Transfer using Interfacility Transport Protocols No Battalion Chief speaks transferring doctor Operations Issue Battalion discusses with transferring facility Medical Issue Call Medical Director Interfacility Transport Protocol Original date: Revised date: November 25, 2002 June 25, 2007 General: Refer to flow sheet regarding acceptance of interfacility transports 1. Obtain a verbal patient report from the physician or nurse at the transferring facility Age and gender of patient Brief history and diagnosis Reason for transfer Last set of vital signs and level of consciousness Obtain a direct contact number for the transferring doctor prior to initiating the transfer. The patient remains under the care of the transferring physician for the duration of the transfer and the physician must be readily available should issues arise en route to the receiving facility. 2. Receive the patient’s records and permission for transfer from the transferring facility including labs, x-rays, CT scans, EKGs, all other diagnostic tests, face sheet and signed completed transfer form. 3. Obtain a set of vital signs prior to leaving the transferring facility. If significantly abnormal contact the patient’s physician. 4. If the patient is intubated, the paramedic in charge must verify and document endotracheal tube placement prior to and after moving the patient to the transport stretcher (end tidal CO2, EDD and pulse oximetry in addition to physical exam). En route continuous pulse oximetry and capnography should be utilized and documented. Upon arrival at the accepting facility, these parameters must be performed and documented before the patient is transferred to the receiving facility’s stretcher. Obtain a signature from the receiving nurse or physician verifying these findings. 5. Regularly document the patient’s condition or notable changes during transport. 6. Treat the patient according to the orders provided by the transferring physician. If patient becomes unstable en route, follow your South Florida Regional Common Protocols. Contact the transferring physician. If the transferring physician cannot be reached, contact the Medical Director. 7. Give a report to the receiving facility, including the report you received from the transferring facility, and the patient’s condition and treatment during transport as well as all paperwork related to the transport. 8. A nurse, physician, respiratory therapist or other personnel should accompany the paramedic during transport of the patient requiring treatment(s) outside the paramedics’ scope of practice as defined by these protocols and the South Florida Regional Common EMS Protocols. The transferring physician must provide written orders for the transferring hospital personnel to follow en route. Example of such situations include, but are not limited to, a nurse with specialized training regarding balloon pumps in a patients with a balloon pump, a respiratory therapist in patients requiring the use of the hospital’s ventilator, a physician if the patient is in active labor. Intravenous Drip Medication Maintenance: 1. 2. 3. In addition to those medications outlined in the South Florida Regional Common EMS Protocols, the following IV drip medications can be monitored en route without hospital personnel assistance by the paramedics when ordered by the transferring physician and provided by the transferring facility. All of these medications must be run on infusion pumps at all times during the interfacility transport. If the patient deteriorates or has significant change in clinical status contact the transferring physician. If the transferring physician cannot be reached, contact the Medical Director. IV Drip Medications A. Aminophylline Actions: Aminophylline is a bronchodilator that works by relaxing smooth muscle, increasing the contraction of the diaphragm and reducing the lungs sensitivity to allergens. Indications: treatment of moderate to severe asthma and COPD Dose: up to 0.5mg/kg/hr Discontinue infusion if heart rate exceeds 140 bpm, more than 6 PVCs per minute occur, Vtach develops or if the patient develops nausea or vomiting. B. Amiodarone Actions: blocks sodium channels and exerts noncompetitive antisympathetic action. Lengthens cardiac action potential. Produces negative chronotropic effects. Indication: treatment and prophylaxis of frequently recurring Vfib and hemodynamically unstable Vtach in a patient refractory to other therapy. Dose: (assumes initial bolus already given) 1mg/min infusion for 6 hours then 0.5mg/min infusion for next 18 hours. Discontinue infusion if hypotension or symptomatic bradycardia develop. C. Cardizem (diltiazem) Actions: slows conduction through the AV node and prolongs AV nodal refractoriness thereby slowing ventricular rates and interrupting reentry tachycardias. Indication for infusion: Afib or Aflutter with a rapid ventricular response. Dose (assumes initial bolus already given) 5 to 15 mg/hour Discontinue if hypotension or symptomatic bradycardia develop. D. Dobutamine Actions: synthetic catacholamine that increases contractility Indications: inotropic support in adults with cardiac decompensation due to depressed contractility from organic heart disease or cardiac surgery Dose: 2-20 mcg/kg/min Discontinue infusion if symptomatic hypotension occurs. E. GP IIb/IIIa Receptor Inhibitiors Action: bind to platelets at the glycoprotein IIb/IIIa receptors and inhibit aggregation Indication: Treatment of unstable angina; before and after angioplasty and stenting procedures to help prevent restenosis. Dose: Aggrastat (tirofiban) 0.1- 0.15 mcg/kg/min Integrilin (eptifibatide) 0.5 – 2 mcg/kg/min Reopro (abciximab) 0.125 mcg/kg/min (max 10mcg/min) Discontinue infusion if patient exhibits any signs or symptoms of bleeding. F. Heparin Actions: anticoagulant; inhibits thrombin and Factor Xa, inhibits conversion of fibrinogen to fibrin Indication: used in the treatment of deep venous thrombosis (DVT), pulmonary embolism, acute coronary syndromes and stroke. Discontinue infusion if patient has any signs or symptoms of bleeding. G. Insulin (regular) Actions: causes uptake, utilization and storage of glucose. Indications for infusion: Diabetic ketoacidosis (DKA) Dose: 0.1 unit/kg/hour Monitor blood glucose by glucometer hourly. Discontinue infusion if symptomatic hypoglycemia occurs and follow Diabetic Emergencies protocol located in the South Florida Common EMS Protocols (2.8.2) H. Levophed (Norepinephrine) Actions: functions as a peripheral vasoconstrictor (alpha-adrenergic action) and as an stimulator of the heart and dilator of coronary arteries (betaadrenergic action) inotropic Indications: As an adjunct in the treatment of profound refractory hypotension. Dose: Start with 0.5- 1 micrograms per minute and titrate to effect. Usual range is 2-12 micrograms per minute Extravasation leads to necrosis I. Mannitol Actions: elevates glomerular filtrate osmolarity causing an osmotic diuresis. Indications for infusion: treatment of increased intracranial or increased intraocular pressure. Dose: 0.25 – 1 gram/kg over 30 to 60 minutes. Discontinue infusion if hypotension occurs. J. Neuromuscular Blockers ***ONLY IN INTUBATED PATIENTS**** It is the responsibility of the paramedic to confirm proper endotracheal tube placement prior to and during transport as well as upon arrival to the receiving facility. Actions: antagonizes acetylcholine receptors at the motor endplates. Indication: paralysis of the intubated patient. Dose: Vecuronium: 0.05 – 0.075 mg/kg/hr Pancuronium: 0.03 – 0.04 mg/kg/hr Discontinue infusion if the endotracheal tube becomes dislodged. Note: the paralysis caused by these drugs may last for 30 minutes or more. Paramedic must assure that adequate sedation has been ordered. K. Opiates Action: depress the central nervous system and sensitivity to pain. Indications: pain management. Dose: Morphine: 0.8 – 10 mg/hour; titrated to effect Fentanyl: 50 – 100 mcg/hour; titrated to effect Discontinue if symptomatic bradycardia, hypotension or respiratory depression occur. Naloxone may be used according to the South Florida Regional Common EMS Protocols. L. Potassium Actions: important in many physiologic processes. Indications: hypokalemia Dose: usually not faster than 10 meq/hour. Discontiue infusion if ventricular dysrhythmias occur. Requires constant cardiac monitoring during infusion. M. Sedatives Actions: central nervous system depression, sedation, lack of recall. Indications: sedation of the intubated patient. (ABSOLUTELY required if neuromuscular blocker is used). Dose: Propofol: 25 mcg/kg/min; titrate per transferring physician’s orders Versed: 2 –10 mg/hr; titrate per transferring physician’s orders Ativan: 2 –10 mg/hr; titrate per transferring physician’s orders Discontinue infusion if symptomatic bradycardia, hypotension or respiratory depression occur. N. Steriods (methylprednisolone/Solumedrol) Action: anti-inflammatory Indications for drip: spinal cord injury Dose: (assumes bolus already given) 5.4 mg/kg/hr IV for 23 hours. Discontinuation of infusion rarely necessary. O. TPA (tissue plasminogen activator/Alteplase) Action: converts plasminogen to plasmin promoting fibrinolysis. Indication: Acute myocardial infarction Dose (assumes initial bolus already given): 0.75mg/kg over 30 minutes, then 0.5 mg/kg over 60 minutes Discontinue infusion if evidence of significant bleeding. Wayne Lee, MD FACEP EMS Medical Director