Immunization-Coalition-Research-Barriers-Best
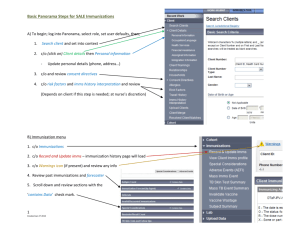
advertisement

Immunization Limited Literature Review - 2010 Barriers/Best/Promising Practice Barriers 1. Exposure to immunization media messages among African American parents, Lashuay N, Tjoa T, Xuniga de Nuncio ML, Franklin M, Elder J, Jones M, Preventive Medicine, November 2000, Vol. 31, Issue 5, pages 522-528. Results: 88% of African Americans reported seeing or hearing immunization information from the following media outlets – 63%-television ads, 51%-billboards and 42%-radio. Barriers to receiving immunizations included a) perception that immunizations caused mild disease after the shots (62%); b) fear of HIV from needles (27%); c) pain (19%) and; d) money (26%). 2. Influenza among healthy young children: changes in parental attitudes and predictors of immunization during the 2003 to 2004 influenza season, Daley MF, Crane LA, Chandramouli V, Beaty BL, Barrow J, Allred N, Berman S, Kempe A, Pediatrics 2006; 117; e268-e277, www.pediatrics.org/cgi/content/full/117/2/e268. Summary: Media exposure significantly changes parental perceptions in attitudes. Key messages were associated with specific perceptions: Hearing about Colorado’s influenza outbreak-increased perception of severity of influenza Hearing children died=decrease perception of vaccination risks Hearing about vaccine shortages=increase perception of severity of influenza and increase in perceived social norms of vaccination Hearing young children should be immunized=decrease in perception of vaccination risks, increase in perceived social norms and increase in perception of the susceptibility of their child to influenza Perceived barriers were: inadequate vaccine supply (23%), child being sick interfered with vaccination (19%), did not know if influenza vaccination was recommended for their child (15%), wait times (12%), appointments difficult to make (10%), office hours for vaccination inconvenient (9%), other important tasks (10%) and cost (8%). Other perceived barriers included less parental education and preseason intention not to immunize were predictors of not immunizing one’s child. Positive predictors of influenza immunizations were a doctor’s recommendation and increase perception that immunization was the social norm. 3. Health disparities and prevention: racial/ethnic barriers to flu vaccinations, Chen JY, Fox SA, Cantrell CH, Stockdale SE, Kagawa-Singer M, Journal of Community Health, February 2007, Vol. 32, No. 1 Summary: 2004 telephone survey of congregation members aged 50-75 to identify modifiable determinants of vaccination. Whites (96%) and African Americans (91%) who were concerned about being infected with influenza were significantly more likely to get immunized compared with those not concerned (45% and 33%). Barriers to vaccination for Latinos were access and cost, for African Americans were issues of mistrust, e.g. – vaccine causes influenza. 4. Undervaccinated african-american preschoolers: a case of missed opportunities, Daniels D, Jiles RB, Klevens RM, Herrera GA, American Journal of Preventive Medicine, May 2001, Vol. 20, Issue 4, Supplement 1, pages 61-68. Results: Among the undervaccinated preschoolers, 63.7% had sufficient number of vaccination visits to have completed the basic series. Of those who were severely undervaccinated, most had three or fewer vaccination visits. For 72.6% of the undervaccinated preschoolers, only one additional vaccination visit was needed to complete the recommended series. Conclusion: 90.5% of African-American preschoolers had enough vaccination visits to complete the series. Providers should assess a child’s vaccination status at every visit. 5. Self-reported immunization practices of pediatricians and family physicians based on bivariate analyses, Archives of Pediatrics & Adolescent Medicine, May 2001, Vol. 155, No. 5. Only 50% of pediatricians and 32% of family physicians ‘routinely’ check the immunization status of adolescent patients at illness related visits and only 55% and 37% check at follow-up visits. Only 23% of pediatricians and 18% of family physicians use a system to track and recall adolescents with delayed immunizations. 6. Immunization barriers and solutions, Burns IT, Zimmerman RK, The Journal of Family Practice, January 2005, Vol. 54, No. 1, pages S58-S62. Summary: This article reviewed a number of studies regarding barriers to immunizations. Barriers for adults included lack of knowledge that the vaccines were recommended as well as concerns about safety were noted. For low-income urban residents in a barrier was “undisclosed shot contents.” A national survey of over 13,500 children showed that there was a correlation of lower immunization rates with confusing vaccination schedules, vaccine expense, religious objections to vaccination, frequent child illness and inconvenience of the vaccination process. Physician barriers include lack of knowledge about immunization schedules, contraindications, side effects. In a study seeking to understand where physicians receive their information about immunizations, pediatricians were likely to refer to the Red Book by AAP Committee on Infectious Diseases. Family physicians and general practitioners cited a wide range of resources. The cost of immunizations as well as storing and handling of immunizations were also sited as barriers. Also, concerns over continuity of patient care was a concern. Of over 1000 physicians surveyed nationally, only 3% used immunization registries. Missed opportunities and missed visits were cited in other studies as barriers. Solutions Suggested: Direct communication between the physician and recipient has shown to improve immunization rates. Enrollment in WIC has improved low-income pediatric populations. This article suggested utilization of web materials but did not cite effectiveness or studies showing effectiveness. Interventions to reduce missed opportunities such as screening children at every visit were met with mixed results due to staffing failures to identify all children. Registries are suggested to provide continuity of care regarding immunizations but the data is incomplete. Reminder/recall systems have been recommended, immunizations as prerequisite for school and childcare enrollment, standing orders for adult immunizations, provision of immunization services in homes and WIC settings and implementation of multicomponent interventions that include expansion of services and education have show to be effective. For inner-city clinics, standing orders, reminders and express vaccination services increased influenza immunization rates. 7. Adolescent immunization practices: a national survey of US physicians, Schaffer SJ, Humiston SG, Shone LP, Averhoff FM, Szilagyi PG, Arch Pediatr Adolesc Med, May 2001, Vol. 155, pages 566-571. Summary: This article reported on a 1997 physician survey with 761 meeting inclusion criteria. Most physicians support adolescent immunizations but face a number of barriers in completing immunizations. The primary reason given by physicians who did not routinely immunize adolescents was lack of insurance coverage for the adolescent patients. 27% of physicians surveyed referred adolescents to alternative sources for immunizations for the following reasons: cost to patients, price of vaccines for physicians, patient or parent request for outside referral, insufficient reimbursement from private insurance plans and insufficient Medicaid reimbursement. Physicians (84%) preferred to have adolescents receive their immunizations in their practices, most find alternative sources such as schools, teen clinics and public health clinics to be acceptable. The authors found that many physicians in the survey missed opportunities to vaccinate teens at illness-related visits in spite of few true contraindications. They also found that very few used any tracking and recall systems and in the case of varicella vaccination, many preferred their adolescent patients to contract wild chickenpox despite high complication rates. Authors recommended that educating family physicians about the importance of adolescent immunizations since pediatricians were significantly more likely to have policies to immunize adolescents. 8. Barriers to adolescent immunization: a survey of family physicians and pediatricians, Oster NV, McPhillips-Tangum CA, Averhoff F, Howell K, JABFP, January-February 2005, Vol. 18, No. 1, pages 13-19. Summary: This study was designed to assess barriers at the provider level that might contribute to low adolescent immunization rates. 210 questionnaires were returned representing a response rate of 59%. Pediatricians access vaccine information from the American Academy of Pediatrics and the Advisory Committee on Immunization Practices. Family physicians refer to the American Academy of Family Physicians. The respondents routinely recommend vaccines for adolescents but percentages vary by vaccine type. The range is 98% for Td toxoids to 60% for varicella vaccine. Pediatricians are more likely than family physicians to routinely recommend all four vaccines. 14% of respondents reported that 75% or more of their adolescent patients were up-to-date on all four vaccines (Td, hep B, MMR and varicella). Physician attitudes towards vaccinations indicated that 77-98% of those surveyed believed it was ‘very important’ to insure that adolescents had all but the varicella toxoids. Physicians cited the following as barriers to vaccinating adolescents: adolescents rarely make preventive health visits, adolescent are not aware of need for immunizations, and adolescent and/or parents underestimate the risk of vaccine-preventable disease. Family physicians listed that it is difficult to obtain verification of previous immunizations as a barrier more than pediatricians. More respondents indicated that there were more barriers for adolescents aged 19-21 than for younger teens. 9. Underimmunization among children: effects of vaccine safety concerns on immunization status, Gust DA, Strine TW, Maurice E, Smith P, Yusuf H, Wilkinson M, Battaglia M, Wright R, Schwartz B, Pediatrics, July 2004, Vol. 114, No. 1, pages e16-e22 Summary: Participants in the National Immunization Survey were surveyed for their knowledge, attitudes and practices. This study documents vaccine safety concern by parents contributes to underimmunization in the U.S. The concerns were significantly more common among parents of under-immunized children but parents of fully immunized children had similar attitudes. Households with highly educated mothers reported asking that their children not receive a vaccine and that school entry laws impacted receipt of vaccines even though parents (11.7% case parents and 6.3% control parents) did not want their children vaccinated. Risk Factors/Determinants of Immunization Status 1. Prevalence and predictors of immunization among inner-city infants: a birth cohort study, Brenner RA, Simons-Morton BG, Bhaskar B, Das A, Clemens JD, NIH-D.C. Initiative Immunization Working Group, Pediatrics, September 2001, Vol. 108 No. 3, pages 661-670. Summary: This study used a prospective study design to identify determinants of immunization status of children up to 7 months of age. 452 mothers were enrolled in the study with 370 completing all components of the study. 65% of the mothers were from households with incomes below the federal poverty level. 98% of the mothers indicated that immunizing their infant was very important and that 100% intended to take their infants to their check-ups. Predictors up-to-date immunization status at 3 months were lower birth order, maternal intention to breastfeed, and participation in WIC. Mothers who felt their were high to medium barriers to immunization were less likely to have their infants up-to-date. Predictors of immunization status at 7 months included maternal employment, lower birth order, intention to use a nonprone infant sleep position and participation in WIC. Predictors of continuation of up-to-date status included lower birth order, maternal employment and lower perception of barriers to immunization. These were significant predictors. When compared to other studies, these authors did not see a significant relationship between health insurance or socioeconomic status and the initiation of immunizations. Best/Promising Practices 1. The impact of computer-generated messages on childhood immunization coverage, Dini EF, Linkins RW, Sigafoos J, American Journal of Preventive Medicine, July 2000, Vol. 19, Issue 1, pages 68-70. Results: Several interventions were used, telephone messages alone, letters only or no notification. Intervention groups received as many as 5 computer-generated phone messages or up to four letters reminding of childhood immunizations that were due. 21% of children whose families received any intervention were more likely to complete the immunization series by 24 months. 2. Impact of financial incentives on documented immunization rates in the inner city: results of a randomized controlled trial, Fairbrother G, Siegel MJ, Friedman S, Kory PD, Butts GC, Academic Pediatrics, July 2001, Vol. 1, Issue 4, pages 206-212. Conclusions: Providing a financial incentive to inner-city physicians produced a significant increase in coverage levels. Researchers attributed the improvement to improved documentation not improved immunization practices. 3. Quality improvement in immunization delivery following an unsuccessful immunization recall, Daley MF, Steiner JF, Kempe A, Beaty BL, Pearson KA, Jones JS, Lowery NE, Berman S, Academic Pediatrics, May 2004, Vol. 4, Issue 3, pages 217-223. Conclusions: A clinic-based quality improvement initiative increased the documentation of upto-date rates in disadvantaged patient populations. The quality improvement component of reminder/recall did not increase up-to-date rates. 4. Addressing immunization barriers, benefits and risks, Kimmel SR, Burns IT, Wolfe RM, Zimmerman RK, Immunization barriers and solutions, Burns IT, Zimmerman RK, The Journal of Family Practice, February 2007, Vol. 56, No. 2, pages S61-S69. Summary: This article outlined similar barriers to immunization as in article #6 in the “barriers” section of this literature review. (Two authors were the same). One additional piece of information was that almost one half of nurses were resistant to giving children 3 or more injections and that parents and physicians had concerns as well. The article also repeated solutions suggested in the article listed above (#6). It also created a chart that compared risk of acquiring disease and risk of fatality and complications with risks from the vaccines. 5. Recommendations regarding interventions to improve vaccination coverage in children, adolescents, and adults, Task Force on Community Preventive Services, American Journal of Preventive Medicine, 2000, Vol. 18, No. 1S, pages 92-96. Recommended interventions by category are: Increasing Community Demand for Vaccinations Client reminder/recall – strongly recommended Mulitcomponent interventions with include education – strongly recommended Vaccination requirements for childcare, school and college attendance – recommended Community-wide education only – insufficient evidence Clinic-based education only – insufficient evidence Client or family incentives – insufficient evidence Client-held medical records – insufficient evidence Enhancing Access to Vaccinations Reducing out-of-pocket costs – strongly recommended Expanding access in health care settings as a part of multicomponent interventions – strongly recommended – by itself – insufficient evidence Vaccination programs in WIC settings – recommended Home visits – recommended Vaccination programs in schools (with no other components) – insufficient evidence Vaccination programs in childcare centers – insufficient evidence Provider-Based Interventions Provider reminder/recall – strongly recommended Assessment and feedback for vaccination providers – strongly recommended Standing orders – strongly recommended Provider education only – insufficient evidence Funding for the Limited Literature Review was provided by MO Department of Health and Senior Services Materials contained in this document are not for publication. Maternal, Child and Family Health Coalition 539 N. Grand Blvd., Ste. 403 St. Louis, MO 63103 www.stl-mcfhc.org 314-289-5680 or 314-289-5658 (Jill Thompson’s direct line)