Physicians link heart arrhythmias to calcium, sodium ions
advertisement

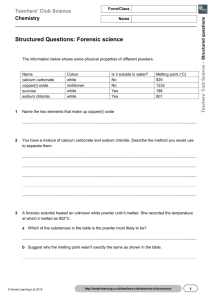
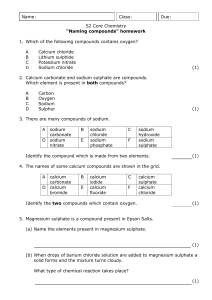
Physicians link heart arrhythmias to calcium, sodium ions By Mary Beth Gardiner February 20, 2002 Research published in the journal Nature has identified the first functional linkage between two key ions -- calcium and sodium -- within heart cells, a finding that could lead to therapeutic prevention of life-threatening arrhythmias, the primary cause of sudden cardiac death in the United States. “These findings provide the previously missing link between the electrical spark that starts the contractile cycle and the contraction itself,” says Jeffrey R. Balser, James Taloe Gwathmy Clinician-Scientist Professor and Chair of Anesthesiology, who directed of the study that produced the results published in the Jan. 24 issue of the scientific journal. The heart pumps blood to all the vital organs in the body, and it does so by both mechanical and electrical means. Mechanical contractions squeeze the heart repeatedly while electricity flowing through heart cell membranes creates a rhythm. The major spark for the rhythmic excitation of the heart, which ignites roughly every second –normal heart rate is about 60 to 70 beats per minute – is created by the sodium current flowing through special pores – sodium channels – in heart cell membranes. And the squeeze – the mechanical contraction that expels the blood – is due to elevation of intracellular calcium that triggers the contractile mechanism in the heart. The study clarifies that calmodulin, a calcium-sensing protein, binds to the tail end of the sodium channel protein inside heart cells and modulates electrical signaling in response to calcium levels in the cell. Balser and his colleagues found that the sodium channel protein has a tail that hangs down inside the cell like a hook. It’s on the C-terminus of that hook-shaped protein that lies a special domain – called an IQ domain – where calmodulin binds. The researchers discovered the calmodulin-binding site by studying a Dutch patient flagged as having an unusual electrocardiogram. Through collaboration with an Amsterdam cardiologist, Dr. Arthur Wilde, Balser learned of this special patient who has Brugada Syndrome, a rare condition characterized by irregular cardiac electrical activity caused by malfunctioning sodium channels. “These people normally have life-threatening arrhythmias usually at night while they are asleep,” says Balser. “The only thing that keeps them alive is an implanted defibrillator.” This patient, however, was different. He had all the electrical abnormalities typical of a Brugada patient, but never experienced arrhythmias. When Balser studied the sodium channels in the cells of this patient, he found a mutation squarely in the middle of the IQ domain. By studying this mutation, the investigators learned that in the normal heart calcium binding at the IQ domain causes the sodium channel to open less readily. “It gets a little sluggish,” says Balser. “That makes intuitive sense because if intracellular calcium goes up from excess activity, you would anticipate negative feedback that would slightly reduce the activity of the sodium current.” Moreover, during conditions that evoke life-threatening arrhythmias, such as during a “heart attack,” intracellular calcium may be exceedingly high. This effect of calcium on sodium channels, called slow inactivation, was altered by the mutation found in the Dutch patient. The mutation diminished the ability of calmodulin to increase slow inactivation when calcium bound to the channel — and the heart — to be more electrically active. -1- “So we have a person with Brugada syndrome, but insensitive to the insult of increased intracellular calcium,” he says. “We suspect that’s why this patient doesn’t have arrhythmias.” According to Balser, the electrocardiographical abnormalities in Brugada Syndrome are reminiscent of those seen in patients who have cardiac ischemia, or decreased blood flow. Arrhythmias due to cardiac ischemia are the leading cause of sudden death in this country. Balser admits that the connection between the situation in the Brugada patient and other arrhythmias is speculative at this point. Nevertheless, he is encouraged by the findings. “It’s provocative, and suggests that we may be focusing on the mechanism of sudden death through a better understanding of the linkage between calcium and sodium channel function,” he says. “We don’t know for sure, but it’s possible that this mutation lies in a key sodium channel domain that is capable of eliminating the arrhythmia susceptibility of a patient who ought to be having ventricular fibrillation and sudden death. The arrhythmia susceptibility of a patient who ought to be having ventricular fibrillation and sudden death but doesn’t. That makes us feel like we’re onto something.” Future studies will be aimed at determining the full three-dimensional structure of the C-terminus of the sodium channel protein to identify other calcium-binding domains located there. Knowing the structural features and their functions will be key to developing targeted therapeutic interventions. “If you could develop a drug that would bind to the C-terminus and prevent the interaction with calcium or calmodulin, that might keep the sodium channels working normally in spite of the raised intracellular calcium,” Balser says. “Perhaps you could prevent arrhythmias in the cases where the cell is calcium overloaded – and we suspect ischemic cells are overloaded.” Balser is quick to acknowledge the contribution of co-author Mark E. Anderson, associate professor of medicine and associate professor of pharmacology, in linking calcium to sodium channel function. “This was a real collaborative effort with Mark,” he says. “Mark has been studying calmodulin and calcium binding proteins for years, and he got me interested in looking at how they interact with the sodium channel, which is my area of expertise. This never would have gotten done without our synergy.” Other Vanderbilt collaborators on the study include Dan M. Roden, professor of medicine and director of clinical pharmacology; Sabina Kupershmidt, assistant professor of pharmacology; Rong Zhang, research instructor in cardiovascular medicine; Svetlana Stepanovic, research coordinator in anesthesiology research; and Hanno L. Tan, former cardiology fellow in Balser’s lab, currently with the Experimental and Molecular Cardiology Group at the Academic Medical Center, University of Amsterdam. Funding for the study was provided by a grant from the National Institutes of Health, and by the Dutch Heart Foundation. - VU - -2-