EXERCISE #8: Automation MLAB 1415 Hematology HEMATOLOGY
EXERCISE #8: Automation MLAB 1415 Hematology
HEMATOLOGY AUTOMATION
LAB OBJECTIVE
1.
Cite the electrical impedance principle of cell counting.
2.
Identify instruments that utilize electrical impedance.
3.
State the principles of light scatter used in cell counting.
4.
Identify instruments that utilize light scatter for analysis.
5.
Categorize cell parameters as directly measured and whether they are derived from
a histogram, scattergram or calculation.
6.
Identify and interpret CBC parameters and correlate patient results with various
disease states.
HISTORY
Automated cell counts began in the mid 1950’s. Blood cell counters replaced manual hematocytometer blood cell counts, spun hematocrits, spectrophotometrically determined hemoglobins and peripheral blood smear preparations. The major advantage of these instruments was they provided data with increased reliability, precision and accuracy. The two main principles of blood cell counting currently used by hematology instruments are impedance and optical light scatter.
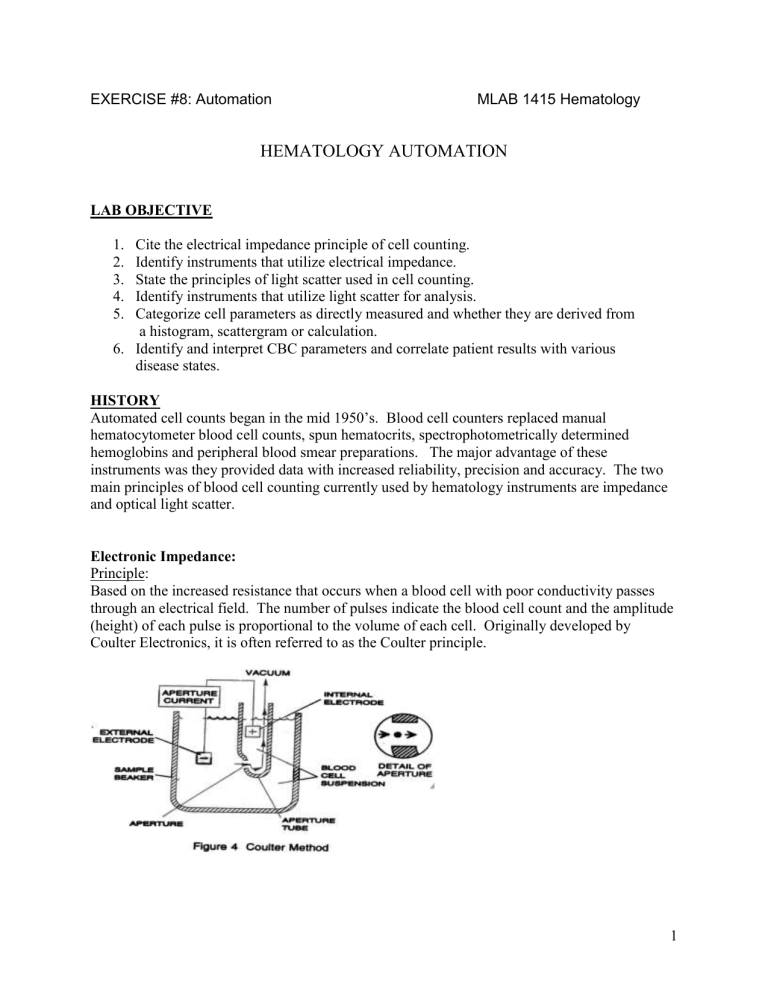
Electronic Impedance:
Principle:
Based on the increased resistance that occurs when a blood cell with poor conductivity passes through an electrical field. The number of pulses indicate the blood cell count and the amplitude
(height) of each pulse is proportional to the volume of each cell. Originally developed by
Coulter Electronics, it is often referred to as the Coulter principle.
1
EXERCISE #8: Automation MLAB 1415 Hematology
Procedure:
1. EDTA sample is divided into four aliquots. The first aliquot is delivered to the RBC/platelet dilution chamber where blood cells are diluted in an electrically conductive diluent. Within the dilution chamber is an external electrode and three apertures, each of which has an internal electrode. As the individual cells pass through the aperature, there is an increase in the resistance between the two electrodes proportional to the volume of the cell. In the chamber that counts RBCs and platelets, particles that are between 2-20 fL are counted as platelets and those greater than 36 fL are counted as RBCs. A steady stream of diluent flows behind each aperature to prevent cells from re-entering the aperature- this is called the sweep flow .
2. Since there are three aperatures within the chamber, three erythrocyte counts are obtained.
These counts are compared and evaluated. If there is agreement, the reported RBC count represents the average of the counts from these three aperatures.
3. At this point, an erythrocyte histogram is created. The erythrocyte histogram (size distribution curve) is based on cell volume and relative cell number. Each pulse of the X axis represents size in fL, the Y-axis is the relative number of cells.
The histogram allows the visualization of changes in size within the RBC population. In a homogeneous cell population, the curve assumes a symmetrical bell-shaped or Gaussian distribution. A wide or more flattened curve is seen when the standard deviation from the mean is increased. Histograms provide information about erythrocyte, leukocyte and platelet frequency and distribution as well as depict the presence of subpopulations. Shifts in one direction or another can be of diagnostic importance.
Larger than normal cells will cause the histogram to shift to the right and smaller than normal cells will cause the histogram to shift to the left. A bimodal peak illustrating a dimorphic
RBC population (camel humps) can be seen in such situations as cold agglutinin disease, after transfusion of red blood cells into a person with abnormally sized RBCs, treated iron deficiency anemia, as well as other conditions.
The RBC histogram displays cells as small as 24fL, but only those between 36-360 fL are counted as RBCs.
2
EXERCISE #8: Automation MLAB 1415 Hematology
This histogram represents a normal red cell distribution. The small tail to the right of the curve represents coincidence , multiple cells passing through the aperture at the same time.
4. The platelet count is also obtained from the RBC/platelet dilution chamber. In the electrical impedance system, the analyzer’s computer classifies particles that are greater than 2 fL or less than 20 fL as platelets. The raw platelet histogram is electronically smoothed and extrapolated over 0 to 70 fL. The final platelet count is derived from this extrapolated histogram. The MPV
(mean platelet volume) and the PDW (platelet distribution width) are obtained from the platelet histogram as well.
Platelet Histogram
5. The second aliquot is delivered to the WBC/hemoglobin dilution chambers . The WBC count is directly measured by electronic impedance from the leukocyte dilution after lytic agent is added. The lytic agent lyses the RBCs and converts hemoglobin to cyanmethemoglobin and shrinks the leukocyte cell membrane and cytoplasm. Therefore, the WBC count represents a measure of cell volume not native cell size. Particles greater than 35 fL are counted as WBCs.
The WBC count is obtained from three aperatures and averaged.
6.The WBC histogram represents the size distribution curve for the leukocyte data and allows for
3
EXERCISE #8: Automation MLAB 1415 Hematology visualization of subpopulations based on their relative sizes. The leukocyte histogram is the basis of the three-part differential identifying cells on the following:
lymphocytes between 35 and 90 fL
mononuclear cells as cells between 90 and 160fL
granulocytes as cells between 160 and 450 fL
7.
The instrument examines the WBC histogram for the presence of interferences and uses a system of flags to alert the technologist. A valley or depression should be seen between each population. Abnormal sized cells or abnormal particles can cause abnormal patterns and the instrument will print an alert specific for the region where the abnormal pattern exists.
8.
The hemoglobin concentration is determined by measuring the absorbance of cyanmethemoglobin in the WBC/hemoglobin chamber at 525 nm.
9.
The third aliquot is delivered to the orbital mixing chamber . Here blood is lysed to remove the erythrocytes and leave the leukocytes in their native state. This dilution is sent to the VCS (volume,conductivity, scatter) flow cell for determination of the five-part differential.
Volume Analysis –Determined by impedance as they pass through the aperture.
Conductivity - Cell walls act as conductors to high-frequency current. As the current
passes through the walls and through each cell interior, it detects differences in the
insulating properties of cell components. It characterizes the nuclear and granular
constituents and the chemical composition of the cell interior.
Scatter - Leukocytes are hydrodynamically focused and passed in a steady stream through a sensing zone on which a laser light is focused. As each cell passes through the sensing zone of the flow cell, it scatters and reflects the focused light which is detected by a
4
EXERCISE #8: Automation MLAB 1415 Hematology photodetector. The patterns of scatter are measure at various angles (forward scatter at
180
and right angle scatter at 90
). Scattered light provides information about cell structure, shape and reflectivity. The characteristics are used to differentiate the various types of WBCs and to produce scatterplots with a five-part differential.
10.
The fourth aliquot is used to measure reticulocytes .
Examples of instruments using electronic impedance: a.
Beckman-Coulter (Gen-S, LH-750) b.
Sysmex XE-2100 c.
Abbott CELL_DYN Sapphire
Optical Light Scatter :
Principle:
Based on light scattering measurements obtained as a single blood cell passes through a beam or light (optical/laser). Blood cells create forward scatter and side scatter that photodetectors detect. These light signals are converted into electrical signals. The number of signals indicates the number of cells. The degree of forward scatter is a measurement of cell size. The degree of side scatter is a measurement of cell complexity and granularity.
Procedure:
1. Instrument has five measurement channels:
Erythrocyte/platelet channel: determined by light scattering measurements as cells pass
through a helium-neon laser beam
Hemoglobin channel: Cyanmethemoglobin determined at 546 nm
Peroxidase channel: Id of neutrophils, monocytes and eosinophils by the degree of
peroxidase activity and degree of forward light scatter. Lymphs and unstained larger
cells not stained by peroxidase
Basophil/lobularity channel: Basophils retain cytoplasm after diluent lyses other cells
Reticulocyte channel
Examples of Instruments using Light Scatter: a.
Siemens ADVIA- 120 b.
Siemens ADVIA 2120
5
EXERCISE #8: Automation MLAB 1415 Hematology
Parameter = a statistical term that refers to any numerical value that describes an entire population.
Parameters and their derivation for the Beckman-Coulter System
Parameter Unit of reporting
Derivation Calculation
WBC
RBC n x 10
3 cells/
μ
L n x 10 6 cells/
μ
L
Hemoglobin g/dL
# of leukocytes measured directly, multiplied by the calibration factor
# of red cells measured directly, multiplied by the calibration factor
NA
NA
MCV fL
A beam of white light shines through the lysed
WBC solution and then through an optical filter.
The transmittance of light (525 nm) as compared to a reagent blank is converted to absorbance, then converted to g/dL using a calibration factor
NA
Derived from the RBC histogram by multiplying the # of RBCs by the size of RBCs and multiplied by a calibration constant.
NA
Hematocrit % Calculated
MCH
MCHC
RDW
Platelet
MPV pg g/dL
% n x 10
3 cells/
μ
L fL
Calculated
Calculated
Derived from RBC histogram
# of platelets derived from the Plt histogram and multiplied by a calibration constant
Derived from the platelet histogram
RBC x MCV
10
Hgb X 10
RBC
Hgb X 100
Hct
NA
NA
NA
6
EXERCISE #8: Automation MLAB 1415 Hematology
Instrument manufacturers and their websites are listed below:
Manufacturer Instruments available Web address
Abbot Cell-Dyn 1200, 3200, 4000 abbot.com
Siemens Diagnostics (Bayer) Advia 60 and 120
Beckman-Coulter STKS, Gen-S bayerdiag.com beckmancoulter.com
Sysmex SE-Series Sysmex.com
SPECIMEN
EDTA-anticoagulated blood
QUALITY CONTROL
1. Commercial low, normal and high controls
Monitor the CBC and differential parameters. Latron controls monitor the performance
2. of the volume, conductivity and light scatter for the automated differential. Control values are stored in the instrument computer and can be monitored with the generation of a Levey-Jennings graph for each parameter.
X
B
analysis
Patient results are monitored with continuous X
B
analysis (weighted moving averages), which uses the patient’s own data to monitor population values and instrument performance. Batches of 20 samples are used to track MCV, MCH, and MCHC values.
This method can be used to detect changes in sample handling, reagents, or instrument performance. Batches of 20 are automatically printed out. The analyzer is considered to be in control when the MCV, MCH and MCHC determined on a batch of 20 patients by
3.
4. use of the X
B
algorithm are within 3% of the expected mean indices of the population.
Delta Checks
Another method of quality control is the use of delta checks (delta means “difference”) which compares a patient’s own values with their most previous results. If the difference between the two is greater than laboratory-set limits, the current result is immediately flagged for review. These can only be used if the instrument is interfaced with a host
Laboratory Information System (LIS).
Mode to Mode
A selected specimen is run in both primary and secondary mode and results must fall within a specified limit.
7
EXERCISE #8: Automation MLAB 1415 Hematology
REFERENCE RANGES
REPORTING RESULTS
Parameter Normal Range
WBC
RBC
3.0-9.0 x 10
3
/
μ
L
Male 4.5-5.5 x 10
6
/
μ
L
Female 4.0-5.0 x 10
6
/
μ
L
Hemoglobin Male 14-17.4 g/dl
Female 12-16 g/dl
Hematocrit
MCV
MCH
MCHC
RDW
Platelets
MPV
Male 42-52%
Female 36-46%
80-100 fl
28-34 pg
32-36 g/dl or %
12.0-14.6%
150,000 - 450,000/
μ
L
6.8-10.2 fl
8
EXERCISE #8: Automation MLAB 1415 Hematology
Code
+++++
H
LINEARITY LIMITS
The instrument will be accurate as long as the results fall within a certain range known as the linearity range. Linearity ranges very by instrument.
Linearity Range Table
Parameter Coulter STKS Bayer Advia
WBC
RBC
Hgb
0-99.9 x 10
3
/
μ
L
0-7.0 x 10
6
/
μ
L
0-18 g/dL
0.02-400 x 10
3
0.0-7.0 x 10
6
0-22.5 g/dL
/
μ
L
/
μ
L
MCV
Plt
MPV
50-200 fL
0-999 x 10
3 μ
L
5-20 fL
NA
5.0-3500 x 10
3 μ
L
NA
INSTRUMENT CODES
Cause
Result exceeds printable range
Action indicated
Dilute 1:2 and rerun.
Continue further dilutions if necessary until the result falls within the linearity range (See
“Handling Abnormal Results)
Result is higher than the laboratory-set patient high action limit
Review result
L Result is lower than the laboratory-set patient low action limit
Review result
9
EXERCISE #8: Automation MLAB 1415 Hematology
INTERFERENCES THAT MAY CAUSE ERRONEOUS RESULTS
Parameter Interfering agent
WBC Unusual RBC abnormalities that resist lysis
Nucleated RBCs
Fragmented WBCs
Unlysed particles greater than 35 fL
Very large or aggregated plts
Specimens containing fibrin, cell fragments or other debris (esp pediatric/oncology specimens
RBC
Hgb
Very high WBC (greater than 99.9)
High concentration of very large platelets
Agglutinated RBCs, rouleaux will break up when Istoton is added
RBCs smaller than 36 fL
Specimens containing fibrin, cell fragments or other debris (esp pediatric/oncology specimens
Very high WBC count
Severe lipemia
Heparin
Certain unusual RBC abnormalities that resist lysing
Anything that increases the turbidity of the sample such as elevated levels of triglycerides
High bilirubin
MCV
RDW
Very high WBC count
High concentration of very large platelets
Agglutinated RBCs
RBC fragments that fall below the 36 fL threshold
Rigid RBCs
Very high WBC
High concentration of very large or clumped platelets
RBCs below the 36 fL threshold
Two distinct populations of RBCs
RBC agglutinates
Rigid RBCs
10
EXERCISE #8: Automation MLAB 1415 Hematology
Parameter Interfering agent
Plt Very small red cells near the upper threshold
Cell fragments
Clumped platelets
Cellular debris near the lower platelet threshold
MPV
Hct
MCH
Known factors that interfere with the platelet count and shape of the histogram
Known effects of EDTA
Known factors that interfere with the parameters used for computation,
RBC and MCV
Known factors that interfere with the parameters used for computation,
Hgb and RBC
MCHC Known factors that interfere with the parameters used for computation,
Hgb, RBC and MCV
Diff parameters
Known factors that affect the WBC count as listed above, high triglycerides that affect lysing
HANDLING ABNORMAL RESULTS
Plts < 40,000 Check the integrity of the specimen (look for clots, short draw, etc.)
Confirm count with smear review for clumps, RBC fragments, giant platelets, very small RBCs
WBC ++++ Dilute 1/2 with Isoton or further until count is within linearity (for final result, multipy diluted result by dilution factor); subtract final WBC from RBC; perform spun hct, calculate MCV from correct RBC & Hct (MCV = Hct/RBC x 10), do not report HGB, MCH, MCHC. Plt counts are not affected by high
WBC. Add comment, “Unable to report Hgb, MCH, MCHC due to high
WBC.”
Plt ++++ Check smear for RBC fragments or microcytes.
1. If present, perform plt estimate. If they do not agree, perform manual plt count.
2. If not present, dilute specimen 1:2 with Isoton or further until count is within linearity, multiply diluted result by dilution factor.
11
EXERCISE #8: Automation MLAB 1415 Hematology
RBC > 7.0 Dilute 1:2 with Isoton or further until count is within linearity, multiply dilution result by dilution factor; perform spun hct, review Hgb, recalculate
MCH, MCHC
MCHC >
36.5
Perform manual hct.
1. If it stays the same, check plasma for lipemia, icteremia or other color interference. If present, perform Isoton replacement. Pour 3 ml blood into
10x75 tube. Mark level of top of blood. Centrifuge at high speed for 10 minutes. Pipette off plasma being careful not to disturb red cells. Replace plasma with Isoton to mark. Mix well and rerun to obtain correct Hgb and
MCH, MCHC. RBC should be within
0.2 of previous result. Add comment, “ results corrected for lipemia”.
2. If it is significantly higher, check the specimen for cold agglutinin by looking for RBC clumping. If present, warm the specimen at 37C for 5 minutes, mix well and repeat. If results are acceptable, report. If cold agglutinin persists, report the spun hct and mark through the RBC, MCV,
MCH, MCHC results. Add comment, “ specimen warmed before running”.
3. If the above conditions are not found, check the smear for spherocytes or lyse-resistant red cells. If present, ensure correct instrument operation by running controls and report result.
MCHC <
36.5
Perform spun hct. Verify proper instrument operation by running a previous patient. Decreased MCHC may be caused by swollen hyperglycemic red cells. Perform isoton replacement or correct values using spun hct.
Low plts,
“Giant plts” or EDTA clumpers
Confirm with smear review.
1. If clumps are present, check with phlebotomist to see if the phlebotomy was difficult. If not, recollect in blue top tube (Na citrate anticoagulant). If platelet clumps disappear and platelet count is acceptable, multiply plt result by 1.1 to account for the dilution factor.
2. If there are no clumps, but giant platelets are present, perform plt estimate from smear. Perform manual platelet count if smear estimate and instrument count do not agree.
12
EXERCISE #8: Automation MLAB 1415 Hematology
PROCEDURE NOTES
1. The approximate relationship of the hemoglobin level to hematocrit is 1:3, a ratio that may vary with the cause of the anemia and the effect of that cause on the RBC indices, particularly the MCV. This is referred to as the rule of 3.
Hct (
2) = 3 x Hgb
Also, the RBC is usually about a the hemoglobin. If the ratios are not appropriate, there is either something wrong with the instrument or there is something unusual with the specimen which must be resolved before reporting results. Some typical instrument problems that cause the H&H not to match include inadequate delivery of lysing reagent, inadequate delivery of diluent, clogs in tubing or blood sampling valve, inadequate draining of baths, etc. To differentiate between an instrument problem and a specimen problem, run a control or repeat a specimen from earlier in the day.
REFERENCES
Harmening., Denise, Clinical Hematology and Fundamentals of Hemostasis, 3 rd edition, pp.
593-599.
Turgeon, Mary Louise, Clinical Hematology - Theories and Procedures, 3 rd
edition, pp373, 376-
382.
Rodak, Bernadette, Diagnostic Hematology, 1 st
edition, p.605-606.
Coulter STKS Operating Manual
McKenzie, Shirlyn, Clinical Laboratory Hematology, 2 nd
edition,pp 813-829.
13
EXERCISE #8: Automation MLAB 1415 Hematology
3.
2.
STUDY QUESTIONS
Name ________________________________
Date_________________________________
1.
State the principle of electronic impedance. (2 pts)
Label the cell populations on the following histograms: (6 pts)
Sketch the appearance of histograms associated with each of the following: (6 pts) macrocytosis MCV 120 fl
Microcytosis MCV 65 fl
Dimorphic red cell population
14
EXERCISE #8: Automation MLAB 1415 Hematology
4. List the parameters provided by automated analysis and the derivation (direct measurement or calculated). (10 pts)
5.
6.
What is coincidence correction? (2 pts)
How is the RDW derived? List three causes of an increased RDW. (5 pts)
For each of the following conditions, state whether the test would be falsely ↑,
or not affected at all:
7. WBC count (6 pts)
15
EXERCISE #8: Automated CBC MLAB 1315 Hematology
NRBCs giant plts clumped plts hemolysis lipemia
↑ RBC
LAB EXERCISES MLAB 1315
EXERCISE #6: Automated CBC MLAB 1415 Hematology
8. RBC count (6 pts)
EXERCISE #8: Automated CBC MLAB 1315 Hematology cold agglutinin rouleaux lipemia greatly ↑ WBC clotted specimen
↑ background count
LAB EXERCISES MLAB 1315
EXERCISE #8: Automated CBC MLAB 1315 Hematology
9. Hemoglobin (4 pts)
LAB EXERCISES MLAB 1315
EXERCISE #8: Automated CBC MLAB 1315 Hematology lipemia icteremia greatly ↑ WBC
↑ background count
LAB EXERCISES MLAB 1315
EXERCISE #8: Automated CBC MLAB 1415 Hematology
EXERCISE #8: Automated CBC MLAB 1415 Hematology
10. Calculate indices from the following results and state the expected RBC morphology
(macro, micro, normocytic and hypo or normochromic). (24 pts)
Show your calculations below and on back.
.
RBC
X 10
6
/
L
Hgb g/dL
Hct
%
MCV fL
MCH pg
MCHC
%
Expected RBC morphology
A 4.66 17.7 52.3
B
C
2.95
3.64
9.1
10.8
29.9
32.0
D
E
F
4.90
3.50
5.04
15.1
8.0
10.0
43.8
26.2
30.1