ATT. 2 Draft BMTCommissioningPolicy
advertisement
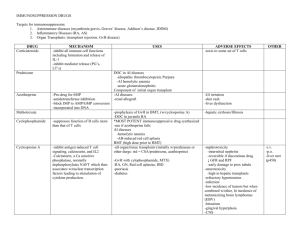
DRAFT Commissioning Guidance for Blood and Bone Marrow Transplants in Wales October 2007. 1 Contents Page 1) Introduction 3 2) Context 3 3) Definitions and Clinical Pathways 3 4) Current Provision in Wales 4 5) Service specification 5 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 5.10 5.11 5.12 JACIE Accreditation Activity Facilities Programme Management MDT Structures and Personnel Support Staff and Facilities Transfusion and Laboratory services Pharmacy service Clinical Policies Follow Up Information Clinical Research 5 5 6 6 7 8 8 9 9 10 10 11 6) Performance and Clinical Information 11 7) Referral Mechanisms 11 8) Patient Selection 11 8.1 8.2 Procedures Supported Clinical Options Panel 11 12 Appendix 1 14 2 1) Introduction The purpose of this document is to build upon the current commissioning policy issued by Health Commission Wales (HCW) in October 2006 and in doing so provide more informed guidance on the governance and performance aspects of a blood and bone marrow transplant (BMT) service. In addition, and in light of developments within what is a rapidly changing field of oncology/haematology recommendations are also made for a more refined process for identifying patients that may be suitable for a blood or bone marrow transplant. 2) Context BMT activity is rising significantly with data from the European Group for Blood and Marrow Transplantation (EBMT) showing that there has been a significant increase in the number of transplants performed in Europe over the past 30 years rising from 14 in 1975 to over 30,000 in 2005 (Gratwohl et al, BMT 2001;27:899-916;Gratwohl et al, BMT 2006; EBMT Annual Surveys 2000 – 2005) This growth is in part due to an increase in the number of diseases found to be improved through BMT, the development of reduced intensity transplants, improvements in tissue typing and the expansion of the donor pool. The majority of transplants (60%) are autologous but allogeneic transplants are increasing significantly, rising in the UK and Eire by 17% between 2004 and 2005; unrelated donor BMTs accounted for 49% of allogeneic activity in 2005. The HCNA indicates an estimated requirement of at least 40 transplants per million population leading to a suggested annual figure for Wales of approximately 120 procedures per annum. Despite the increased activity sufficient evidence for the efficacy of BMT for certain diseases remains open to interpretation, (Carroll, BMT briefing paper, unpublished, 2007). 3) Definitions and clinical pathways For the purpose of this document BMT is defined as the transplantation of blood stem cells derived from bone marrow or blood in order to repopulate the bone marrow and produce new healthy blood cells. Where appropriate a distinction will be made between a procedure where the source is the patient themselves, an autologous transplant or from a donor, an allogeneic procedure. 3.1) Clinical Pathways Clinical pathways will differ by primary disease, type of transplant and location. However understanding some core elements of the clinical pathway is essential to the commissioning process as elements of the pathway can be delivered by different organisations with different levels of service and different commissioning arrangements. 3 As a consequence each pathway should be identified for each part of Wales – see table 1. Table 1. Common elements of a BMT pathway Pathway element Potential location Initial remission induction Unit level chemotherapy Decision to transplant Unit/ centre level Donor selection Harvesting Unit/ centre level Centre Storage Centre Conditioning Re-infusion Centre Centre/unit level Post infusion recovery Centre/unit level Follow up Centre/unit level Notes Depends on primary disease MDT discussion that should be joint with BMT centre Dependent on procedure identified May include donor and procedure. Blood stem cell harvesting may include multiple visits A percentage of stored blood and bone marrow may not be used and may be stored for future use Chemotherapy work up Optimum location is at centre to reduce risks. Dependent on time post infusion, well being post infusion, type of transplant, psychological status and facilities Can be performed in either subject to protocols Providers of BMT services should identify to commissioners annually the clinical pathways for BMT in their locality naming the organisations involved and their role within the pathway. 4) Current Provision in Wales Adults Allogeneic transplants for the South, Mid and West Wales are performed at University Hospital Wales (UHW) within a purpose built 6-bedded unit. Autologous transplants for the same population are also performed within UHW. Approximately 50 BMT are performed within UHW per annum. Swansea NHS Trust do not perform allogeneic transplants but do provide an autologous BMT service for a specified population from West Wales exceeding the required 10 procedures per annum. North West Wales NHS Trust also perform in excess of 10 autologous BMT per annum within their oncology/haematology unit and also provide harvesting and storage facilities 4 for patients to later have their cells re-infused at Conwy & Denbighshire NHS Trust within the confines of the North Wales Cancer Treatment Centre. Access to allogeneic transplant for the North Wales population is via the Christie Hospital in Manchester using their 18 bedded BMT unit. Occasional referral is also made to Bristol for specific cases. North East Wales NHS Trust currently refer all their BMT patients to Manchester though plans have been agreed to use North West Wales Trust for autologous transplantation in the future. Children There is currently no childrens BMT service in Wales with the services at Bristol, Manchester, Newcastle and Great Ormond St providing access. This commissioning guidance does not apply to BMT for children. Other providers It is believed that other providers used in the past for specific adult cases have been Liverpool, Birmingham and Bristol although none have been subject to a commissioning policy. 5) Service specification In order to be commissioned as a provider of a BMT service the following elements of the service must be in place and maintained. Where indicated evidence must be provided on annual basis. Key factors identified below directly relate to the ‘ International Standards for Cellular Therapy Product Collection, Processing and Administration’ FACT –JACIE (3RD Edition – Feb 2007) and are also in line with NICE IOG and the Welsh Cancer Standards. 5.1) JACIE Accreditation It is a key requirement that units providing BMT services should work towards JACIE accreditation (see 5.8). The requirements below are identified as key requirements of a BMT service that assure basic safety and quality and though key elements of JACIE are considered to be elements of a service specification that should be in evidence before final JACIE accreditation is achieved. 5 5.2) Activity A service providing allogeneic transplantation should perform a minimum of 10 new patient procedures per annum with no minimum number for autologous transplants being required if performed within the same unit. A service providing solely an autologous BMT service should perform a minimum of 5 new patient procedures per annum. A breakdown of activity must be provided monthly and a summary provided annually 5.3) Facilities Inpatients Inpatient facilities must be of a nature to minimise airborne microbial contamination with a minimum requirement being single bedded, private accommodation with en suite sanitary facilities. Such facilities must be provided for the remission induction, bone marrow re-infusion and marrow recovery phases of the pathway. Laminar flow, HEPA filtration facilities are desirable for allogeneic BMT services but are not required for an autologous BMT service. All facilities must be supported by a protocol for environmental hygiene e.g. room cleaning, filter cleaning/replacement schedule. Adherence to this protocol should be audited annually. Facilities supporting an allogeneic programme should ideally be able to support mobile renal dialysis facilities. Day case/outpatients Dedicated outpatient and day case facilities should exist that are designed to, minimise infection risk facilitate IV drug and blood product administration - Facilities should be described annually and confirmed year on year. - Audit of environmental hygiene measures should be provided annually. 5.4) Programme Management The Clinical Transplantation Programme must be under the leadership of a single Programme Director with an agreed deputy both of whom are deemed to have adequate experience for the role, as agreed by the relevant Cancer Network. The Clinical Programme Director will 6 Be responsible for the administrative and clinical functions of the service Have oversight of all elements of the clinical programme including quality management, selection and care of patients and donors, cell collection and processing (internal or contracted out) Have oversight of all medical care and the proficiency of those delivering that care Have oversight of the clinical care delivery by the transplant team (MDT) Programme Director confirmed annually 5.5) MDT structures and personnel The BMT service must be supported by a sustainable BMT related multi disciplinary team (MDT) who function both in a virtual and physical manner to identify and deliver the optimum care for the patient. The MDT must identify the following members and the cross cover/deputisation arrangements, Lead clinician and deputy who have adequate clinical experience of BMT ( as indicated by JACIE) Junior and senior clinicians providing 24hr on-call Lead nurse for in and out patient /day case setting Microbiologist Virologist Radiologist Pharmacist Dietician Social worker Psychologist The MDT must ensure that appropriate MDT members convene daily to assess those patients currently under going BMT. The full MDT should meeting regularly to discuss, if appropriate, patients undergoing BMT, patients being worked up for BMT and patients post BMT under follow up. If patients are being followed up at unit level, where appropriate, these patients should be discussed at the request of the unit level team. Patient discussion at the MDT should be supported by a protocol that as a minimum confirms the decision making process and communication of that decision to the patient and clinical team If not meeting to discuss patients the full MDT must meet to discuss outcomes, service issues, audit and the ongoing delivery of the service. The frequency of these review meetings will be at the discretion of the programme lead but must be frequent enough to ensure adequate clinical governance is achieved. 7 Annual confirmation of MDT membership and MDT meeting timetable/attendance 5.6) Support Staff and Facilities A requirement of a service providing allogeneic transplantation must be immediate access to, designated renal expertise and dialysis facilities on site, preferably within the BMT unit accessible HDU/ICU care if not integrated within the BMT unit Mechanical ventilation facilities should be accessible on site and supported by a protocol for the management of patients ventilated off site and away from the BMT setting. For units providing an autologous transplantation service only the above is desirable but not essential. Evidence of access to renal/HDU/ICU facilities and expertise - annually Nursing and Allied Health Professions The nursing team should, Be of a size adequate to ensure that staffing levels are safe and appropriate at all times. Have a greater nurse to patient ratio in allogeneic BMT units Have enough flexibility to ensure 1:1 nursing where patients are severely ill Demonstrate core skills pertaining to IV administration of chemotherapy and other drugs via central lines and management of blood disorders Be proficient in cardio-vascular monitoring Have an adequate skill mix to ensure that experienced, post graduate qualified nurses are in place on each shift Have in place a rolling programme of post graduate education relevant to BMT Those Allied Health Professions involved in the care of BMT patients should as a minimum be designated staff. Post graduate education should be provided for those staff designated to the MDT. Annual self assessment of nursing profile 5.7) Transfusion and laboratory services The service should have the ability to access CMV appropriate blood products as well as irradiated blood products, where indicated, at all times. In the eventuality that such products are not available alternative blood products should only be used according to a previously agreed protocol. 8 In the case of an allogeneic BMT service access should also be made available to HLA DNA – based typing. A protocol must be in place to support the transfusion of patients who, undergoing allogeneic BMT, experience, as a result a change in blood group. - Description of access to transfusion services and details of access to CMV/irradiated blood products and annual confirmation. - Submission of transfusion protocols. 5.8) Pharmacy services Access must be available to pharmacy services at all times. Pharmacy input into the MDT should come from a designated member of staff who is able to respond in an informed way to the themes pertaining to pharmaceutical management of BMT patients. Description of access to pharmacy 5.9) Clinical policies The Programme Director together with key MDT members must ensure that the BMT service is supported by evidence based clinical management and administrative protocols/policies. In addition the Programme Director should ensure that these protocols/policies are audited frequently and re-visited at least every 3 years. As a minimum there must be policies and protocols regarding, Chemotherapy administration and spillage Environmental management of the immuno compromised patient Clinical and laboratory monitoring of the patient Clinical use and management of blood products Use of prophylactic anti infection measures and growth factors Clinical management of neutropaenic sepsis Post discharge precautions It is noted that a prerequisite of JACIE accreditation is evidence of protocols/policies covering a wide range of issues and the list identified above should not be considered exhaustive. All BMT units should be seeking to obtain JACIE accreditation by 2010. 9 Evidence of progress towards JACIE accreditation provided annually. 5.10) Follow up Immediate follow-up (day 0 – 100) should be conducted at the transplant centre in facilities co-terminus with the BMT unit itself. Where follow up is delivered prior to day 100 at a local unit it should only be done so through agreement between the programme director and the local unit level clinician. If this follow up arrangement exists it then should be supported by a suitable protocol. Part of the agreed protocol must ensure that, The unit level clinician is ‘integrated’ into the BMT MDT Immediate access to the BMT services is ensured The unit level facilities are adequate for the management of the patient Long term follow up over and beyond day 100 can be performed at unit level but should be supported by a suitable protocol. Communication between the BMT centre and the unit should be considered of a standard adequate for the unit to Provide follow up in an appropriate, safe and integrated manner Provide emergency interventions as required Provision of protocols for emergency care, immediate and long term follow up Provision of a standard for communication between the BMT centre and units 5.11) Information Data collection must be an integrated part of the BMT service and all MDT personnel should recognise their individual role in collecting adequate data. Data on BMT should equate to the requirements of EBMT FMedA form. The Programme Director should work with colleagues across Wales to ensure common data items are collected. Key items of data that must be collected and reported on annually include, Primary diseases, and phases of diseases transplanted Types of transplants performed Donor selection Length of disease free survival All complications in first 100 days (including episodes of infection) All deaths within first 100 days Long term/delayed side effects Patient support including information for patients from units 10 Information summary should be provided quarterly and a summary annually 5.12) Clinical Research As many patients as possible should be offered the opportunity to be submitted into recognised clinical trials 6) Performance and Clinical Information Commissioners require three sets of performance information, a) A response to the measures identified within this commissioning guidance document - Annual. b) Completion of the annual audit of activity against the Wales Cancer Standards. c) Numbers of patients waiting for BMT identifying primary disease, disease status, time waiting, predicted BMT date, point on clinical pathway ( donor search, bed awaited) - Quarterly. Clinical information should be submitted to the BSBMT data register annually. 7) Referral mechanisms Referral for BMT should be to the BMT Programme Director in those BMT units recognised by the commissioner. Referrals should only be received from recognised Haematology MDT members identified by their local Cancer Network. Table 2. Commissioned Providers of BMT services Oct 2007.North Wales Region S E Cancer Network S W Cancer Network N W Cancer Network 8) Allogeneic BMT UHW UHW Christie/Bristol Autologous BMT UHW UHW/Swansea Christie/NWWT Patient selection process All BMT procedures must be verified by the commissioner in the first instance and submissions for approval must be submitted to the commissioner via the established route by the clinician who first deems the requirement for BMT (this may follow advice from the BMT Programme Director). 8.1) Procedures supported Procedures supported should conform with the standard indication for transplantation as described by EBMT (2005) and be in the category ‘Standard of Care’. See Appendix 1. 11 Additional procedures supported include, Lymphomas – chemosensitive disease using reduced intensity conditioning (RIC) prior to sibling allograft or well matched MUDs. AML high risk and young AML , both in CR1 – allograft sibling or MUD Relapsed AML – allograft or MUD Refractory AML- chronic low disease burden - MUD 8.2) Clinical Options panel The EBMT classification of BMT by disease status (2005) identifies in a number of cases the procedures as a ‘clinical option’ which translates operationally to individual patient assessment, risk and value assessment. In these cases, where an individual clinicians feel BMT is a ‘clinical option’ the commissioner should convene a ‘Clinical Options’ panel the purpose of which will be to assess the appropriateness of BMT through an informed assessment of, Clinical appropriateness Clinical safety and risk Assessment of outcome Value The process is for consideration by the panel is as follows, the referring clinician will complete the referral pro forma which serves to provide clinical information and signify to the commissioner the need to convene the Clinical Options Panel. the commissioner will convene the Clinical Options panel within 10 working days. the Clinical Options Panel will consist, as a minimum, of the following, - referring clinician - national chair for haematology oncology (or nominated deputy) - 1of the 2, or both haematology clinical leads from each of the remaining Networks - medical commissioning lead - finance commissioning lead - relevant Network Director or nominee (optional) the Clinical Options Panel will deliver one of three options - agree to support - agree not to support - request additional information 12 In the case of agreement to or not to support the commissioner will issue the advice within 5 working days and that advice will be agreed by the panel and be binding When further information is required this will be made available within 5 working days and the panel reconvened. The outcome from this second discussion will then follow the process above i.e. agree to support or not support with appropriate rationale. 13 Appendix 1 EBMT Transplant Indication (2005) 14