Dental Nurse Radiation Training
advertisement

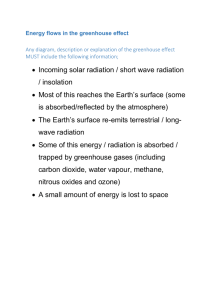
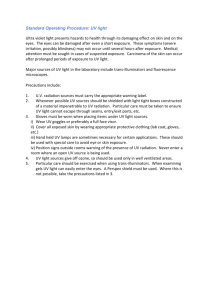
Radiating an interest in IRMER Mark McAlister, FGDP(UK) Yorkshire course organiser In November, FGDP(UK) Yorkshire invited radiation protection adviser Graham Hart to Leeds to present two lectures focusing on IRMER. The evenings were part of a new initiative to provide core CPD topics and relevant lectures at times convenient to the dental team. IRMER expert Graham Hart’s engaging and entertaining style made what many feel is a dry topic both interesting and highly informative. The opening lecture covered radiation, x-rays and radiology, ionising radiation and its effects and digital radiography and specialised techniques. Graham followed this up by focusing on x-rays and the law and practice requirements for the Ionising Radiations Regulations 1999 (IRR99) and IRMER. The following is a snapshot of the basic steps to keep you safe in everyday practice. Radiation in the environment A little background. We are all exposed to small doses of radiation every day from our environment; the food and drink we consume, sunlight, and the ground and buildings around us. More than 50% of the natural radiation we are exposed to derives from naturally occurring radon and thoron found below the earth’s surface. Radon levels depend on where we live. Higher concentrations are found in Cornwall, South Wales, some parts of the Midlands, Aberdeenshire and the Grampians, as well as in the north of England. You can find out if you are in a high radon area by visiting www.ukradon.org According to IRR99, if your practice is in a radon affected area, all occupied below-ground and, potentially, ground floor spaces need to be monitored for radon levels. Levels above 400Bq/m3 require remedial action and further monitoring is mandatory. Radiation and dentistry In comparison with other professions, the dental team has a relatively low level of exposure to radiation. Mean UK radiation doses by occupation*: Aircrew – 2 mSv / yr Nuclear Power – 0.8 mSv / yr Coal miners – 0.6 mSv / yr (radon) Medical workers – 0.14 mSv / yr Dental teams – 0.08 mSv/yr * The International Commission on Radiological Protection recommends that the maximum permissible dose for occupational exposure should be 20mSv per year, averaged over five years, with a maximum of 50mSv in any one year. For public exposure, the maximum permissible dose is limited to 1mSv per year averaged over five years. As Graham points out, just being alive carries a small risk, but all dental practices are required to be vigilant in order to protect both the dental team and patients. The emphasis must be on reducing the risk. The FGDP(UK) standards publication Selection Criteria in Dental Radiography advises that: “No patient should be expected to receive additional radiation dose and risk as part of a course of dental treatment unless there is a likely to be a benefit in terms if improved management of the patient. Notwithstanding the low risk, every effort should be made to undertake the radiography at a minimum dose to the patient.” Practices can minimise risk to the team and patients by following the three basic principles of radiation safety: time, distance and shielding. Time The radiation dose you receive is directly proportional to the time you spend near the radiation source, so it’s important to minimise the time you are close to the patient while radiographs are being taken (ideally you shouldn’t be close to them all). Distance Wherever possible, keep your distance! The way in which x-rays perform depends on the space where the exposure is taking place and the strength of the radiation. X-rays can be focused on a target area but they can scatter if you are not taking them in a contained space. Essentially, the message is to keep as far away as reasonably practicable during the exposure. Shielding Dental radiography uses relatively low amounts of radiation. If your workload is no more than 100 intra-oral or 50 OPT films per week then keeping a wall or a door between you and the patient should be sufficient. Radiation is more strongly absorbed by solid materials so the denser the material, the better the shielding protection. Relatively dense walls of solid brick or concrete construction may be suitable, but if normal structural walls do not afford sufficient shielding additional protective material (such as x-ray protective plaster) should be used. You can consult a Radiation Protection Advisor (RPA) for guidance on compliance with IRR99. Patient and team safety IRMER guidance should help to protect you and your patients from being exposed to excessive levels of radiation. However, if you are concerned about the effects of radiation then you can monitor radiation levels during radiographic procedures. There are a variety of dosimeters that register radiation levels. However, some of them can be limited in terms of sensitivity. Many medical workers who are regularly exposed to radiation wear lead aprons, thyroid shields and even lead glasses. However, these are rarely needed for teams involved in routine dental radiography, due to the low levels of radiation being used. Pregnant tem members and patients It is possible that team members may be concerned about taking radiographs during pregnancy. They should be assured that normal radiation doses should pose no quantifiable risk to a mother and her baby. This is true for team members performing x-rays on a routine basis and patients who require treatments during their pregnancy. It is thought that the average dose of radiation per year for dental team members is 0.08mSv/y. The only time when you may need to take someone’s pregnancy status into account during a radiographic procedure is when taking vertex occlusal projections. In such cases, guidance suggests the use of abdominal lead protection. IRMER in summary IRMER regulations are designed to protect the dental team and patients. Although it may seem a hassle to research the requirements, it’s not just a case of ticking boxes. Being aware of the guidelines and how to monitor your radiographic procedures will protect you, your staff and your patients. Feedback from delegates who attended the lectures was overwhelmingly positive, with many delegates commenting that it was the best IRMER course they had attended. The lectures were free for anyone who attended the FGDP(UK) Yorkshire Division Study Day and enabled local dentists to meet up for CPD and networking. The Yorkshire Division’s next evening lecture event is a radiology course beginning 22 January 2013. FGDP(UK) Yorkshire would like to thank Graham Hart for his excellent lectures and for giving us permission to use his content as the basis for this article. We highly recommend him to other divisions; you can find out more about his work at http://www.dentalrpa.co.uk/