Drug Classification
advertisement

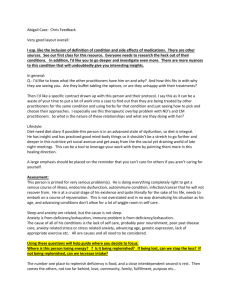
Drug Classification Drugs Action Indications Mast Cell Stabilizers Cromolyn Sodium (Nasalcrom) (Intal) prevents release of histamine from sensitized mast cells. poorly absorbed, action is local long term prophylaxis of allergic disorders, rhinitis, asthma: prevent exercise induced bronchospasm Contraindications < 2 years age; may worsen acute attacks of bronchospasm Not for acute attacks Precautions Adverse Effects Route Nursing implications Patient / family teaching nasal, throat, & trachea irritation; unpleasant taste inhalation - inhaler capsule or nebulizer solution and intranasal spray assess for respiratory function before, during, and after therapy; reduction of dose of other asthma meds may be possible after 2-4 weeks of therapy; pre-treat with bronchodilator to increase delivery of inhalation (if ordered) do not use solution if cloudy or contains precipitate. Must be used routinely. Do not stop abruptly. Teach proper use of inhaler. Gargle & rinse mouth after each dose to decrease dryness and throat irritation. Antimetabolites Methotrexate (others you'll get later) inhibition of DNA synthesis & cell reproduction; immunosuppressive activity kidney transplants; severe psoriasis & RA. unresponsive to other treatments. Unlabeled uses: Crohn's disease, graft rejection, SLE HIGH ALERT: Can be fatal! (High doses used for cancer) Clarify orders, double check all orders and calculations Pregnancy-Category X active infections, renal impairment, bone marrow depression, geriatric/debilitated Anorexia, hepatotoxicity, abdominal pain, N/V, diarrhea, stomatitis, infertility, anemia, bone marrow depression (leukopenia, thrombocytopenia), pulmonary toxicity IM, IV, PO onset 4-7 days, peak 7-14 days Monitor BP, Pulse, Resp. periodically during administration. Quaic stools, urine, & emesis; avoid IM and rectal temps if platelets low. Assess for signs of infection if neutropenic. Assess for fatigue, dyspnea, orthostatic hypotension if anemic. Monitor for symptoms of pulmonary toxicity (dry nonproductive cough) Monitor CBC/diff (Nadir 7-14 days) Monitor renal/hepatic values Monitor serum levels q 12-24 hours with high dose therapy Drink 2L fluid a day; Use antiemetic before dose if N/V Caution about photosensitivity/sunscreen Notify MD immediately if fever, shills, cough, hoarseness, sore throat, bleeding gums, bruising, blood in stools/urine/emesis, fatigue, dyspnea; avoid crowds, sick people use soft toothbrush, electric razor, avoid falls; no alcohol, no ASA or NSAIDs; avoid OTC or herbals (consult MD); use contraception during & 3 months after for men and 1 ovulation cycle for women; no vaccinations without consulting MD. Drug Classification Drugs Adrenergic Sympathomimetics/decongestants Epinephrine (Adrenalin) (EpiPen) inhibits release of hypersensitivity mediators reaction from mast cells; produces bronchodilation, vasoconstriction anaphylactic reaction, severe allergic Indications reactions, croup, upper airway obstruction Contraindications: cardiac disease elderly, pregnancy, lactation, HTN Precautions HIGH ALERT: available in multiple strengths/concentrations for different purposes. (0.1mg/mL & 1 mg/mL) Have 2nd nurse verify orders, dose & route Action Adverse Effects Nervousness, restlessness, tremor, angina, arrythmias, HTN, tacchycardia, paradoxical bronchospasm Route SubC, IV, Inhalation (MDI) 0.1-0.5mg SC onset SC 5-10 mins, peak 20mins (may repeat q 10-15 minutes) Assess lung sounds, respiratory pattern, pulse, and BP before, during and after therapy. watch for paradoxical bronchospasm (wheezing) Use TB syringe 26g ½" needle rotate injection sites massage after injection to enhance absorption shake suspension well before giving MDI - wash mouthpiece after each use & don't spray into eyes Nursing implications Patient / family teaching Corticosteroids Prednisone Cortisone, Dexamethosone (Decadron), Hydrocortisone (Solu-Cortef), Methylprednisolone (Medrol), prednisolone, & others suppresses immune response by reducing levels of leukocytes, monocytes, & esosinophils Tissue/organ transplants, autoimmune disorder, immune disorders, inflammation systemic fungal infections, psychoses, emotional instability, pregnancy, breast feeding. Gi disease, renal disease, HTN, osteoporosis, diabetes, hypothyroidism, thromboembolic history, seizures. Avoid in pediatrics (may stunt growth) Geriatric at risk for increased incidence adverse effects. Cushingoid symptoms, immunosuppression, diabetes, osteoporosis, peptic ulcer, increased appetite, fluid/lyte imbalances, euphoria, insomnia, edema, HTN, GI bleed, elevated glucose, dermatologic PO, IV, IM, Topical Get baseline BP, fluid/lytes, weight & assess regularly. monitor for effectiveness give early in day to mimic circadium rythm give with food to prevent GI irritation. avoid exposure to infections don't stop abruptly Take as prescribed Don't stop suddenly Notify MD if stress level increased (may need increased dose) Take with food Report black tarry stools, bleeding, bruising, blurred vision, emotional changes Drug Classification Drugs Action Immune Modulators Immune Suppressants 1. T & B cell suppressors (Cyclosporine) 2. Interleukin Receptor Antagonist 3. Monoclonal Antibodies Block antibody production by B-cells, inhibit helper T-cell, block inflammatory reaction. Inhibit immune response Cyclosporine - suppress transplant rejection Neoral - psoriasis and RA autoimmune disorders/diseases Contraindications: safety not established in pregnancy & lactation Precautions renal , hepatic impairment no immunizations Flu-like syndrome (fever, chills, malaise) Adverse Effects increased risk for infection, neoplasms, hepatotoxicity, renal toxicity, pulmonary edema due to fluid retention, H/A, tremors, GI, diarrhea, HTN. PO, Sub C, IV, topical Route IV Cyclosporine - dilute with D5 or NS and infuse over 2-6 hours check baseline vital signs, weight, Nursing orientation, ECG, Liver function, CBC implications with differential. Monitor response to therapy Monitor for infection Asses for organ rejection May need protective isolation Indications Patient / family teaching proper administration protect from infection, avoid sick people and those with live vaccinations teach S&S of infection & to report STAT healthy nutrition contraception warn S&S of adverse effects Lifelong therapy for organ transplant Immune Modulators Immune Stimulants 1. Interferons (Interferon Alpha 2b) 2. Interleukins (Aldesleukin) 3. T & B cell modulators (levamisole) interferons naturally produced in response to viral invasion; prevent virus cells from replicating. interleukins stimulate cellular immunity, increase activity of Natural Killer Cells. T & B cell modulators stimulate immune activity. HIV/AIDS, chronic hepatitis, leukemias children, CNS disease, pregnancy/lactating, cardiac disease, myelosuppresion, Flu-like syndrome: HTN, arrythmia, bone marrow suppression, CNS depression, personality changes, lethargy, myalgia, anorexia, nausea, H/A, dizziness, photosensitivity. IM, IV, SC check baseline vital signs, weight, orientation, ECG, liver function, CBC with differential. Monitor response to therapy proper administration protect from infection nutrition contraception warn S&S of adverse effects Drug Classification Drugs Action Indications Antihistamines Diphenhydramine hydrachloride (Benadryl) loratadine (Claritin) cetirizine (Zyrtec) block effects of histamine by competing with histamine for H1-receptor sites on smooth muscle of bronchi, GI tract, uterus and large blood vessels urticaria, pruiritis, allergic rhinitis, allergic reaction Contraindications: Narrow angle glaucoma, breastfeeding, bladder neck obstruction, <6 years age, Precautions elderly, Adverse Effects Route Nursing implications Patient / family teaching anticholinergic effects - constipation, dry eyes & mouth, urinary retention, blurry vision, sedation, hypotension impaired motor function. paradoxical reaction PO, IV, IM assess allergy symptoms monitor pulse and BP with IV route