Nutr. Res. & Ethics Paper - Tamara Belhomme-Wint
advertisement
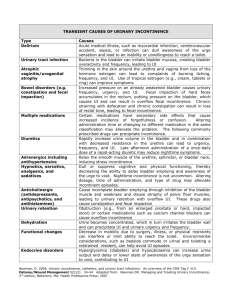
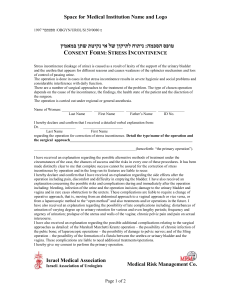
1 Caffeine Consumption and Nocturnal Enuresis Belhomme, Tamara HUN3800 Jones November 26, 2012 2 Does the reduction of chocolate & caffeine (during the day as well as near bedtime) effectively reduce/cease the occurrence of bed-wetting (also called nocturnal enuresis/urinary incontinence) in adults? To receive insight into this question I researched many facts about nocturnal enuresis first. It is also called bladder or urinary incontinence (UI), or simply bedwetting. Many people struggle with this disorder, especially those of close friends and family members, that fail to share this information for fear of ridicule. I have a profoundly personal experience with this as I have suffered from nocturnal enuresis since childhood and have yet to find a reasonable cure for this issue (I feel that it could be onset by emotional disturbances but that is another topic of research and study that I plan to do in the near future), so I have a vested interest in this subject and finding out the solution to this private yet embarrassingly public and common issue. At least 2% of adults show lack of bladder control (bedwetting) at night, (1, 2) and surprisingly, more than a million Canadians suffer from urinary incontinence. In almost all cases, family physicians are the first health professionals contacted by patients. 7 A historical account of nocturnal enuresis and its treatment was found in 1974 in a section of the History of Medicine by a Michael A Salmon, MRCP, DCH, in the Stoke Mandeville Hospital in Aylesbury, Buckinghamshire in Southeast England. It is the only one that could be found during my research and offers some interesting insight. The first found reference of enuresis was found in the Ebers papyrus of 1550 BC. 9 There are some outlandish, but possibly effective treatments suggested back in history, that include Pliny’s (whom wrote a piece of literature called “Natural History”), which calls for “giving boiled mice in their (infants) food,” 9 to woodlice and the urine of spaded swine, and a few other wild suggestive cures for enuresis. During the Victorian era, suggested 3 treatments for enuresis included fluid restriction (which we know today is a good suggestion, as long as the daily intake requirements for fluids are met), enemata [a procedure in which liquid or gas is injected into the rectum, typically to expel (evacuate) its contents. (Google dictionary)], the use of an alarm clock, cold or warm baths, splashing cold water towards the inguinal area and lower spine douches (p.443). 9 Jacobi (1891) mixed Strychnine and sheep fat into a bean-sized suppository [a solid medical preparation to be inserted into the rectum or vagina to dissolve (Google dictionary)] and inserted into the rectum of enuretic patients multiple times daily to supposedly strengthen a weak bladder, sometimes injecting strychnine into the perineum/inguinal area (p.443). 9 The medical suggestions continue with further noted doctors and scientists, such as Ruddock (1878), Corrigan (1844), Slade (1855), Rex (1893), Trousseau (1870), Simmons (1880), Baruch (1889), Nye (1881) and so forth. One study that particularly interested me was Powers 1879 review of Goltz experiments performed on dogs (p.445). In these experiments, “while cleansing dogs with divided spinal cords, Goltz found that when the wet sponge touched the perennial area, micturition (voiding of urine) occurred.” 9 Powers believed that the urinary voiding of liquids was stimulated by the sacral nerves when ‘higher mental influences were suspended,’ as during sleep. Ruddock’s (1878) thoughts were that “hypertrophy (enlarging of an organ due to abnormal increase of cells) of the bladder muscles with increased contractility” may be responsible for enuresis. 9 These studies, be they dated to some extent, are quite pertinent to the relationship between caffeine, ADH and the bladder, which will be discussed in further detail. There are two different types of enuresis that exist: the first is Persistent Primary Nocturnal Enuresis (PPNE), which begins during childhood and is a condition when 4 “nighttime dryness has not been achieved for longer than six months” (About 2-3% of male and female adults older than 18 suffer from this type and this would be the type that I suffer from). 1 The second is Adult Onset Secondary Enuresis (AOSE): nocturnal enuresis when “nighttime dryness has been achieved and maintained for years,” but then interrupted by nocturnal enuresis at an older age. 1 A few additional key terms crucial to the comprehension of nocturnal enuresis include ADH, which is the Anti-Diuretic Hormone, produced and secreted by the hypothalamus and posterior pituitary gland of the body (in the inferior region of the brain, superior to the spinal cord). Upon release, this hormone decreases the bladder’s activity by relaxing the detrusor muscle, which is the muscle that controls the bladder. Those with bladder incontinence (nocturnal enuresis or bedwetting) have trouble producing sufficient amounts of this hormone, or their body isn’t as reactive to it as the normal human body would be, causing bladder/urinary instability and incontinence (bedwetting). Functional bladder capacity is the limit of the bladder to hold in urine before releasing due to pressure. Patients can suffer from small FBC (Functional Bladder Capacity), which means that their bladder fills with less than the normal human body before it gets the signal to alleviate the pressure and release the urine.1 Caffeine (as well as alcohol) is a diuretic, so it opposes ADH, is known as a “bladder irritant” 1 and “can also contribute to detrusor instability, as well as increase urine production.” 3 Many chocolates contain caffeine, so decrease in these can also decrease detrusor instability and therefore decrease the risk of bladder incontinence. 5 In a study conducted with nine women and three men (21-40 years of age) with OAB symptoms, each drank 8 ml/kg water with and without caffeine at two separate sessions and bladder tests were performed 30 minutes post-intake. 8 Findings suggest that high but not lower caffeine intake is associated with a modest increase in the incidence of frequent and urgent urgency incontinence. (5, 8) The majority of the studies and research have been done on women with incontinence, and the results show positive correlation between high caffeine intake and detrusor instability as seen in women with urinary incontinence. 6 When adequate research methods are followed, dieticians will become more knowledgeable with these issues and more equipped to assist patients: suggesting lifestyle modifications such as cessation of smoking, bladder training, a low caffeine or caffeine-free intake plan to decrease occurrences of bladder incontinence, as well as advising patients to set alarms at different times during the night, to consciously void bladder in restroom as opposed to unconsciously while sleeping. 7 Patients with OAB should try to avoid or be overly cautious of caffeine intake within food and/or drink in order to prevent detrusor instability. Some extra information that I found regarding resolving the issue or urinary incontinence consists of the use of DDAVP (Desmopressin) before bedtime, which can decrease/cease the rate of occurrence in bladder incontinence with correct dosage; also adequate fluid intake during the day (40% in the morning, 40% in the afternoon and 20% in the evening4) with decrease in the evening keeps the body well hydrated throughout the day in order to perform its natural functions. By setting alarms at different times every night, you can empty your bladder without it getting used to a specific time and 6 emptying out while you are asleep. Also, bladder volume training1, in which you increase you bladder capacity by drinking large amounts of fluids and holding it for 2-3 hours, can strengthen the detrusor muscle and decrease the occurrence of bladder incontinence. So, in conclusion, with a decrease in caffeine consumption, conditioning your bladder (strengthening it by holding your bladder for 2-3 hours after a heavy liquid consumption), and drinking less fluids in the evening (staying well-hydrated throughout the day and night using the 40:40:20 method/rule), the occurrence of bladder incontinence can be decreased and/or ceased. As for an application to dietetic practice: Larger studies are needed to determine whether the association between caffeine and UI is causal, but dieticians can safely suggest that patients decrease caffeine consumption. Patients are NEVER to dehydrate themselves to cease bedwetting; by drinking adequate amounts of fluids during the day and less during the evening (amongst other health factors), your body is kept well-hydrated and its functions regulated. 7 References 1 National Association for Continence (NAFC) Website. http://www.nafc.org/bladder-bowel- health/bedwetting-2/adult-bedwetting/. Accessed October 14, 2012. 2 Baykara, M., S. Yucel, O. Kutlu, and E. Kukul. "Impact of Urodynamics in Treatment of Primary Nocturnal Enuresis Persisting Into Adulthood." Urology 64, 5 (2004): 1020-1025. Abstract. http://www.ncbi.nlm.nih.gov/pubmed/15533498. Accessed October 15, 2012 Pan, Cynthia. “Urinary Incontinence and Bed-Wetting.” Pediatric Rounds. 2005. Children's 3 Hospital of Wisconsin. 28 July 2006 www.chw.org/ Yeung, C. K., J. D. Sihoe, F. K. Sit, M. Diao, and S. Y. Yew. "Urodynamic Finding in Adults with Primary Nocturnal Enuresis." Journal of Urology 171: 2595-2598. PubMed. Duke University, Charleston, SC. 28 July 2006 www.ncbi.nlm.nih.gov/. 4 Jalkut MW, Lerman SE, Churchill BM, Enuresis. 2001 Dec; 48(6):1461-1488. http://www.ncbi.nlm.nih.gov/pubmed/11732125. Accessed October 15, 2012. 5 Yura, YH, Townsend MK, Curhan GC, Resnick NM. Grodstein F. "Caffeine Intake, and the risk of stress, urgency and mixed urinary incontinence." J Urol. 2011 May; 185(5): 1775-1780. Epub 2011 Mar 21. Abstract. http://www.ncbi.nlm.nih.gov/pubmed/21420114. Accessed October 22, 2012 6 Arya LA, Myers DL, Jackson ND. Dietary caffeine intake and the risk for detrusor instability: a case-control study. Obstet Gynecol. 2000 Jul;96(1): 85-89 http://www.ncbi.nlm.nih.gov/pubmed/12790272. Accessed October 22, 2012. 8 7 Moore KN, Saltmarche B, Query A. Urinary incontinence. Non-surgical management by family physicians. Can Fam Physician. 2003 May;49:602-610. http://www.ncbi.nlm.nih.gov/pubmed/12790272. Accessed October 22, 2012. 8 Lohsiriwat S, Hirunsai M, Chaiyaprasithi B. Effect of caffeine on bladder function in patients with overactive bladder symptoms. 2011 Jan;3(1): 14-18. http://www.ncbi.nlm.nih.gov/pubmed/21346827. Accessed October 22, 2012. 9 Salmon, MA. An historical account of nocturnal enuresis and its treatment. Proc R Soc Med. 1975 July; 68(7): 443–445. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1863929/?page=1. Accessed October 22, 2012.