PATHOLOGY OF SALIVARY GLANDS
advertisement

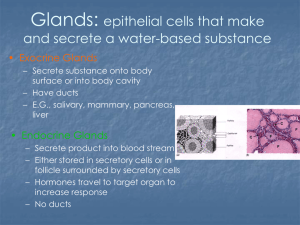
PATHOLOGY OF SALIVARY GLANDS -salivary glands can be classified according to prevailing type of secretory cells -serous glands, mucous glands and mixed seromucous -salivary gland tissue consists of- acinar cells of serous and mucous typemyoepithelial cells- epithelial cells of salivary ducts, mesenchymal cells of the connective tissue (adipose and fibrous, nerves, blood vessels), and inflammatory cells according to the anatomic location- salivary glands include paired major glands (parotid, submandibular, sublingual) and minor glands of upper aerodigestive tract -1.- major glands include parotid- the largest gland, enclosed by capsule, located anterior to the ear, composed of serous acini, secretory ducts -about 20 lymph nodes located in each parotid gland -submandibular-located in the submandibular triangle, seromucous gland -subligual gland, the smallest of major glands, in the floor of mouth, prevailing mucous acini, -2.- minor glands of the oral mucosa -minor glands have mixed serous and mucous acini in varying proportions cellular components: -of particular interest- myoepithelial cells (MEC) - believed to have contractile properties that assist in secretion of saliva -microscopical examination shows that MECs are thin and spindle-shaped cells around acini and intercalated ducts situated between basement membrane and epithelial ductal cells -they display features of both smooth muscle cells and epithelium DISORDERS OF SECRETION Xerostomie- dry mouth-decrease in the secretion of the saliva, it is a symptom and not a disease -xerostomia is important-accompanied by infection, ulceration and rapid dental caries, in addition- there is difficulty in eating, speaking and swallowing -conditions that may lead to xerostomia- 1 -flow rate of saliva may be normal-there is only a feeling of dry mouthbecause of local factors, smoking, mouth breathing, etc -in other cases-real decrease of flow associated with stress, fear as a effect of increased sympathetic activity -common side effect of many drugs, such as sedatives, antihypertensives, and anti-emetics, antihistamines, etc-normal capacity of glands -functional capacity of salivary glands may be reduced due to a loss of secreting cells- irradiation sialadenitis- salivary glands were damaged by therapeutic radiotherapy of head and neck region because of cancer -autoimmune sialadenitis in Sjogren syndrome- permanent and severe xerostomia -other disorders, such as dehydratation, uremia, diabetes mellitus, hypovolemic shock Sialorrhoe (Ptyalism)- true increase in salivary flow is rare -may be present in mercury poisoning, rabies, in some neurological disturbances, epilepsy OBSTRUCTIVE AND INFLAMMATORY DISORDERS These include mucus escape reactions, which are not lined by epithelium, (extravasation mucocoele, ranula), mucus retention cyst (true cyst lined by epithelium), sialolithiasis and a variety of other conditions (e.g. tumours) that can cause obstruction Common to all causes are the effects of obstruction, which are acinar atrophy, stasis, secondary infections, epithelial damage and scarring, and these can aggravate the obstruction. -they occur as a result of stasis of saliva, acute and chronic inflammation and sialolithiasis -sialolithiasis -sialoliths are calcified masses (calculi, stones)- that develop in ductal system of salivary glands - they occur mainly in the large ducts of submandibular gland - (due to thicker mucous secretion than in parotid) -obstruction of salivary duct by stones -chronic sclerosing sialadenitis (Kuttner tumor) - is chronic inflammatory disorder, in most cases secondary to calculi, it can occur at any age, though the mean is about 45 yr, considerably more common than acute sialadenitis 2 - it is most often seen in submandibular gland, patients present with pain and/or sweeling of the gland associated with eating -grossly it is characterized by enlargment and firm consistency of the gland- in the end-stages of the disease there is little remaining glandular tissue- gland is totaly replaced by fibrous tissue - mimic tumor (Kuttner tumor) microscopically: chronic sialadenitis is characterized by fibrosis, progressive atrophy of salivary gland acini and abundant mixed inflammatory infiltrationgerminal centres, some neutrophils, ductal epithelium may show hyperplasia and metaplasma Mucus Escape Reaction. This is defined as pooling of mucus in a cavity in the connective tissue not lined by epithelium- called „extravasation mucocele“. The sites are (minor) lower lip 65%, palate 4%, buccal mucosa 10%, and (major) parotid 0.6%, submandibular 1.2% and sublingual (ranula) 1.1%. -most patients are young - pathogenesis is traumatic damage of a duct, leading to mucus pooling. In the lip, it presents as a raised swelling, which is sometimes blue. The sublingual ranula presents as a swelling of the floor of the mouth. Microscopy shows a well-defined mucin-filled cavity without epithelial lining. There is a mixed inflammatory infiltrate, including foamy histiocytes, and later proliferation of granulation tissue - salivary gland tissue shows chronic sialadenitis, acinar atrophy and fibrosis. The outcome is that recurrences are frequent, especially in sublingual ranula. OTHER INFLAMMATORY DISORDERS 1.- Benign lymphoepithelial lesion and Sjogren syndrome -Sjogren syndrome -is an autoimmune inflammatory exocrinopathy with multisytem manifestations-characterized by lymphocytic infiltration of exocrine glands, particularly the lacrimal and salivary glands resulting in reduced secretion -immunologically, the disease is characterized by B-cell hyperactivity and the production of many circulating auto-antibodies -in over half of cases Sjogren syndrome is accompanied by another autoimmune disorder, such as rheumatoid arthritis, systemic lupus erythematodes, systemic sclerosis, polymyositis, primary biliary cirhosis clinically: glands Sjogren syndrome is characterized by swelling of major salivary -dry eyes- keratoconjunctivitis sicca 3 -dry mouth- xerostomia -rheumatoid arthritis or/and another autoimmune disorder histologically: -the affected lacrimal and salivary glands are diffuselly infiltrated by lymphocytes and plasmacytic cells, there is an atrophy of acinar salivary gland epithelium, accompanied by proliferation of epithelial and myoepithelial cellepi-myoepithelial islands and with fibrosis - called benign lymphoepithelial lesion or lymphoepithelial sialadenitis (LESA) -higher risk of development of malignant lymphoma of MALT type - in salivary gland affected by S. syndrome -miscellaneous inflammatory disorders- there is a variety of noninfectious inflammatory conditions in salivary glands, such as -sarcoidosis -chronic granulomatous inflammatory lesion characterized by epithelioid granulomas with giant cells of Langhans type -Kimura disease (epithelioid hemangioma, angiomatoid lymphoid hyperplasia with eosinophilia)- distinctive lesion particularly affecting soft tissues of head and neck area, characterized by …. SALIVARY GLAND INFECTIONS -mumps virus infection- mumps is an acute infectious disease caused by a paramyxovirus which has predilection for parotid gland -the gland is enlarged, swollen, painful, in most cases bilateral, accompanied with fever and headache -mumps is a self-limited disease, occurs most often in children in school age, there is typically incubation period of 2-3 weeks, -less frequently, other organ may be involved, such as pancreas, testes -cytomegalovirus infection- CMV is a ubiquitous herpes virus detectable in more than 80% of adults -infections may follow debilitating diseases, such as malignant neoplasms, immunosupression, acquired immunodeficiencies, bone marrow transplantations, etc -acute bacterial parotitis- rare, occurs usually in debilitated patients with poor oral hygiene -acute suppurative infiltration, usually with abscess formation 4 -grossly dilated ducts filled with pus cells (neutrophils) and diffuse interstitial acute leukocytic infiltration between acinar cells -focal aggregations of neutrophils may form abscesses- this can only heal by fibrosis- distortion of gland architecture which predispose to further infections NON-NEOPLASTIC NON-INFLAMMATORY LESIONS 1.-Necrotizing sialometaplasia- is a benign self-healing lesion affecting especially the minor salivary glands of the palate -it presents as mucosal ulcer which usually heals spontaneously if left alone, the major problem is that NS clinically and histologically can simulate squamous cell carcinoma -some cases follow surgery or even minor trauma such as from an illfitting denture, the underlying process is considered to be ischemic, the cause is however unknown histology: shows lobular coagulative necrosis of acini, squamous metaplasia of ducts, a chronic inflammatory infiltration and pseudoepitheliomatous hyperplasia of the surface 2.- Sialadenosis- is a non-inflammatory process of the salivary glands due to metabolic and secretory disorders accompanied by painless swelling of the parotid glands -it is related to endocrine dysfunction (thyroid and ovarian insufficiencies) and nerve dysfunction -it is also seen in malnutrition, chronic alcoholism, liver cirrhosis, may be linked to drugs, etc. 3.- Adenomatoid hyperplasia of mucous salivary glands- the lesion is asymptomatic, found accidentally on routine dental examination -grossly- nodular lesion on the palate mimicking benign tumor -most patients –adult, 3-5th decades, etiology is unknown 4.- irradiation changes- salivary glands are very senstitive to irradiation, a xerostomia is a common complication -acute radiation injury-swelling of the gland- necrosis of acinar cells, acute inflammatory response -chronic injury- characterized by fibrosis, loss of acini, and squamous metaplasia -when all glands are involved, loss of saliva is irreversible 5 5.- oncocytic lesions- oncocytic change of salivary glands is relatively common particularly in elderly, it is characterized by cells with abundant granular eosinophilic cytoplasm due to increased number of mitochondria -it is a non-neoplastic metaplastic change, spectrum of lesions -focal and diffuse oncocytic metaplasia -ductal oncocytosis -multifocal oncocytic hyperplasia exact cause is speculative SALIVARY GLAND CYSTS -non-neoplastic cysts and pseudocysts account for about 10% of salivary gland lesions -they can be classified as congenital (dysgenetic) – salivary polycystic dysgenetic disease acquired- true cystic lesions with epithelial lining- salivary duct cyst, lymphoepithelial cyst pseudocysts- without epithelial lining- mucus escape reaction, ranula cystic neoplasms should be distinguished- LG mucoepidermoid carcinoma, Warthin tumor, cystadenoma, etc. mucus escape reaction- is defined as a pooling of mucus in a cavity within the connective tissue that is not lined by epithelium -results from traumatic rupture of a salivary duct of major or minor gland clinically appears as: mucocele- most commonly lesions of lips -more often lower lips ranula- is a type of mucus escape reaction that occurs in the floor of mouth- bluish in color histologic features: -early lesion consists of well-defined cavity in the soft tissue of the oral mucosa - filled with mucinous material with admixture of inflammatory cells and foamy macrophages later, granulation tissue grows organization of the mucocele progressively into the cavity- 6 mucus retention cyst -is a true cyst, less common than mucus escape reaction -clinical presentation is that of slowly growing painless, circumscribed lesion of variable size and location- more often in parotid and submandibular glands salivary duct cyst (sialocyst)- represents true cysts with epithelial lining, it develops as a consequence of duct obstruction. The lesions are unilocular, but rarely they may be multicystic. The absence of lymphoid infiltrate allows to distinguish salivary duct cyst from Warthin tumor, lymphoepithelial cyst and branchial cleft cyst. Cystic lymphoid hyperplasia in AIDS Rarely patients with AIDS present with unilateral or bilateral enlarging cystic masses in parotid glands. These lesions have been reffered to as AIDS-related parotid gland cysts or cystic lymphoid hyperplasia in AIDS (cystic benign lymphoepithelial lesions) -The cysts measure up to 4 cm in diameter and are lined by squamous epithelium. The surrounding parotid gland tissue is replaced by hyperplastic lymphoid tissue with irregular enlarged follicles. -The distinction between AIDS-related parotid gland cysts and benign lymphoepithelial lesion (BLEL) may be difficult, bue well developed cases related to AIDS are characterized by a presence of large irregularly branching cysts with prominent follicular hyperplasia. Benign lymphoepithelial cyst- well circumscribed and predominantly unilocular -Histologically the cyst is lined by stratified squamous epithelium, although mucin producing cells may be also present. -The cyst wall reveals a dense lymphoid tissue with prominent germinal centres of follicles. Salivary Polycystic Dysgenetic Disease. This very rare condition resembles cystic anomalies of other organs, such as the kidney, liver and pancreas, although no association has been described. -Some cases are familial, and almost all cases occurred in females. Most - It only affects the parotid glands, usually bilaterally. Microscopically, the glands maintain their lobular architecture, the cysts vary in size up to a few mm, and they are irregular in shape and often interconnect. The lining epithelium is flat, cuboidal to low columnar, sometimes with an apocrine like appearance. The lumen contains secretion with spherical microliths. Remnants of salivary acini are seen between the cysts, and thick fibrous interlobular septa are often prominent. Inflammation is at most mild Sclerosing polycystic adenosis 7 -rare benign pseudoneoplastic condition of major salivary glands similar to fibrocystic disease of the breast -It affects mainly females, adult -grossly- slow-growing masses in the parotid gland, gland is largely replaced by multiple discrete firm, rubbery nodules. -microscopic examination- well-circumscribed, unencapsulated lesion composed of a lobular arrangement of proliferating ducts and acini with cystic ducts containing viscous secretion There is often intraluminal epithelial proliferation, the lining comprises a spectrum of apocrine, mucous, squamous cells and balooned sebaceous-like cells, although true goblet cells are not seen. There is sometimes nuclear pleomorphism, even occasionally suggesting dysplasia -bening neoplasm, the lesion is monoclonal Clinical features- in 1/3 cases recurrences, benign lesion 8