Equipment in Regional Anesthesia
advertisement
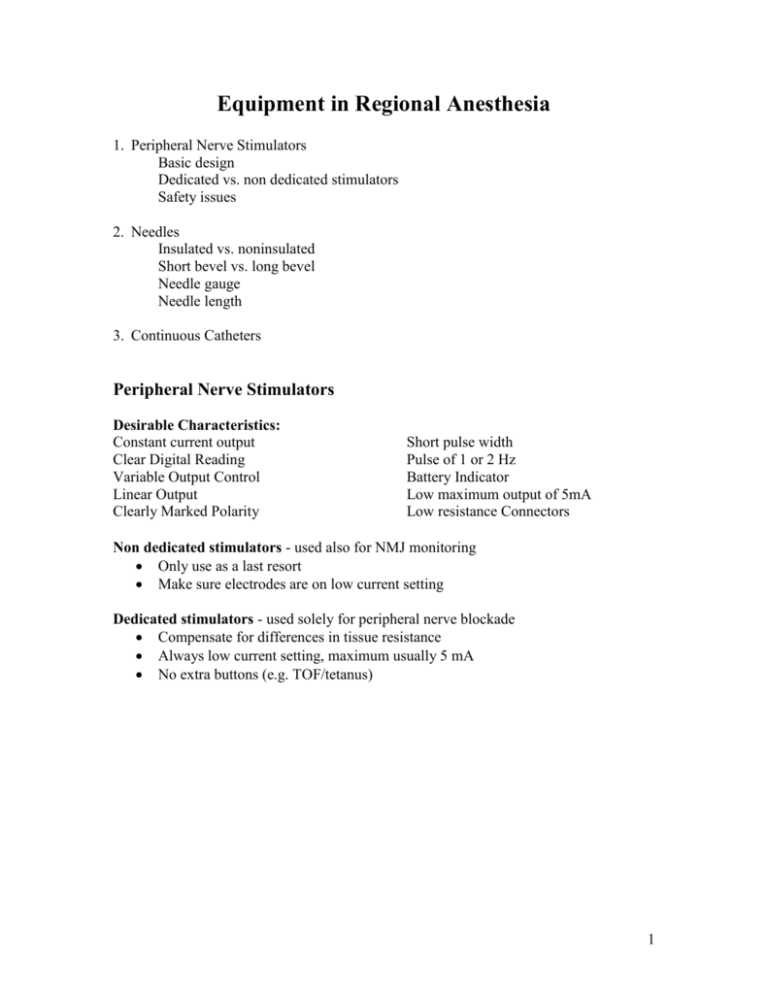
Equipment in Regional Anesthesia 1. Peripheral Nerve Stimulators Basic design Dedicated vs. non dedicated stimulators Safety issues 2. Needles Insulated vs. noninsulated Short bevel vs. long bevel Needle gauge Needle length 3. Continuous Catheters Peripheral Nerve Stimulators Desirable Characteristics: Constant current output Clear Digital Reading Variable Output Control Linear Output Clearly Marked Polarity Short pulse width Pulse of 1 or 2 Hz Battery Indicator Low maximum output of 5mA Low resistance Connectors Non dedicated stimulators - used also for NMJ monitoring Only use as a last resort Make sure electrodes are on low current setting Dedicated stimulators - used solely for peripheral nerve blockade Compensate for differences in tissue resistance Always low current setting, maximum usually 5 mA No extra buttons (e.g. TOF/tetanus) 1 Ideal Stimulator: 4. Safety Tips a. Electrode connections: Negative to Nerve / Needle (Black to block) Positive to Patient / EKG Pad (red) If the positive electrode is connected to the needle, the nerve is slightly hyperpolarized. At any given current the twitch response will be less. This will predispose the patient towards nerve injury as the needle will be too close to the nerve in order to achieve an acceptable twitch endpoint. Most dedicated nerve stimulators are designed to avoid this by using an alligator clip on the positive electrode and a male connector on the negative electrode. b. Check that circuit is complete prior to needle insertion and just after skin penetration. c. Ideal = 0.3-0.5 mA Acceptable twitch: 0.5 mA – 1.0 mA ? Too close 0.1mA – 0.2 mA d. What if a paresthesia occurs before an optimal twitch? Accept it if: reliable patient reliable distribution you didn’t move!!! the patient didn’t move!!! 2 e. If your assistant is unfamiliar explain the stimulator PRIOR to needle insertion. Start at 1.5 mA. Advance needle -- stop --- nerve stim adjusted -- stop --- advance needle---see what happens to the twitch ---stop --- nerve stim adjusted ….. Bottom line: Do NOT move needle while stimulator is being adjusted and vice versa. f. Do not inject if burning pain/constant paresthesias/or resistance to I injection. STOP, withdraw the needle 1-2 mm and try again. If symptoms persist remove needle!! g. Aspirate and inject every 3-5 mL Needles 1. Insulated vs non-insulated: Non-insulated less reliable as shaft can also stimulate Can be used if employ 2 Hz, lower current, and move needle slowly 2. Short bevel (30-45 degrees) vs long bevel (12-15 degrees): Inconclusive. Nerve penetration less likely with short bevel, damage may be more severe and delayed with short bevel if nerve is penetrated? Will feel fascial "pops" better with blunt/short bevel 3. Needle gauge: Usually 24-21 gauge Smaller gauge - the increased resistance to injection may make it difficult to tell if the injection is intraneural. Larger gauge (18/20) will require a local skin wheal. Used mainly for catheter techniques. 4. Needle length: 1 inch for interscalene/supraclavicular/axillary Generally need longer needles for the lower extremity. Exception - Infraclavicular approach -- need 2-4 inch needle 3 Femoral/popliteal should be OK with 2 inch needle unless the patient is obese. Sciatic - generally need 4 inch needle Continuous Catheters 1. Approaches: Upper Extremity: Interscalene, Infraclavicular, Axillary Lower Extremity: Femoral, Sciatic, Popliteal Fossa Trunk: Paravertebral, intercostals 2. Catheter Needle sets: 18-21G, Insulated Short beveled, Touhy, Sprotte Catheter through needle sets usually 18G Cannula over needle sets usually 20G – 21G More recently – stimulating catheter sets 40% secondary block failure rate with catheters Catheter stimulated prior to initiation of block Stimulating catheters ideal for ambulatory patients 3. Technique Peripheral Nerve Stimulation Paresthesia techniques not used due to larger sizes of needles 4. Helpful Hints Pay strict attention to sterile technique (prep/drapes) i.e. similar to epidurals Orient the needle bevel along the axis of the nerve sheath If the cannula/catheter won’t thread make sure that the neural sheath has been distended with 3-5mL of local or saline before threading. If the catheter/cannula still won’t thread try rotating the bevel/lowering the angle Secure the catheter with mastisol/steri strips/ tegaderm (similar to epidurals). Catheters can also be tunneled to increase longevity. Make sure the catheter connector is easily accessible Ensure the efficacy of the nerve block by appropriate bolus of local anesthetic before starting the infusion Common infusion 0.2% ropivacaine , or bupivacaine 0.125% , 4-10 ml/h 4 References: 1. Pither, C. Review Article: The Use of Peripheral Nerve Stimulators for Regional Anesthesia in Reg. Anesth pp 49-58, Apr 1985 2. Hadzic A and Volka J. Peripheral Nerve Stimulators for Nerve Blocks from www.nysora.com 3. Selander, D. Peripheral Nerve Injury after Regional Anesthesia in Complications of Regional Anesthesia Ed Finucane B. pp110-111, 1999 4. Enneking F. Catheter Placement for Continuous Regional Anesthesia in Peripheral Nerve Blocks: A Color Atlas Ed Chelly J. p140, 1999 5. Pham-Dang, C. Continuous Peripheral Nerve Blocks with Stimulating Catheters. Reg. Anesth pp. 83-88, Apr 2003 5