September 25, 2015
advertisement

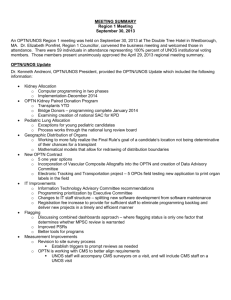
AGENDA Region 4 Meeting Marriott Suites Market Center, Dallas, Texas September 25, 2015 (Note: All times except the start time are approximate. Actual times will be determined by the amount of discussion.) 8:45- Registration and Continental Breakfast 10:15 9:00- Liver Program Directors meeting (Salon 1) 10:00 Thoracic Program Directors meeting (Austin room) Histocompatibility Laboratory Directors meeting (San Antonio room) 10:15 Welcome/Opening Remarks (15 minutes) Kenneth Washburn, MD Region 4 Councillor UTHSC at San Antonio Non-Discussion Agenda (5 minutes) Dr. Washburn ** As a reminder, the following proposals require a vote but will not be presented or discussed** Proposal to Update the Human Leukocyte Antigen (HLA) Equivalency Tables (Histocompatibility Committee) Policy 4.7: HLA Antigen Values and Split Equivalences, states; “The Histocompatibility Committee must review and recommend any changes needed to the tables on or before June 1 of each year.” The Board of Directors approved the most recent updates to the Equivalency Tables in November 2013. Since that time, additional equivalencies have been proposed which should be incorporated into the tables in policy. This proposal also adds alleles to the Human Leukocyte Antigen (HLA) dropdown options in UNetSM to increase access to transplant for sensitized candidates. The Histocompatibility Committee (the Committee) also proposes updating references to these HLA loci in policy to HLA-DPB1, HLA-DQA1, and HLA-DQB1 to distinguish them from other similar HLA loci. Revising Kidney Paired Donation Pilot Program Priority Points (Kidney Transplantation Committee) This proposal seeks to improve how the OPTN Kidney Paired Donation Pilot Program (OPTN KPD) prioritizes candidate-donor matches identified in KPD exchanges (2-way, 3-way, and chains) to increase the likelihood of finding matches for difficult-to-match candidates. UNOS performs a match run on a regular basis to identify all possible exchanges. The match run often identifies more than one possible exchange for the same candidate-donor pair. Since each donor can only donate once, the OPTN KPD uses an optimization algorithm to select a single set of exchanges in which no pair is included more than once. The optimization algorithm searches for the combination of exchanges that maximizes the total number of “priority points” according to current OPTN KPD policy (Table 13-2). As of June 16, 2015, the OPTN KPD system consisted of 56% of candidates with a calculated panel reactive antibody (CPRA) of greater than or equal to 80%, also known as highly sensitized candidates. A candidate with a CPRA of 80% is immunologically incompatible with 80% of donors making it difficult to find matches for these candidates. It is even more difficult to find matches for candidates with a CPRA of 98% or higher because these candidates are only compatible with about 2% of donors. Current policy does not take into account the vast difference in matching a candidate with a CPRA of 80% compared to one with a CPRA of 98% or higher. Furthermore, seemingly easy to match candidates (e.g., non-O blood type with low level of HLA sensitization) that enter the OPTN KPD are often not receiving match offers. While these “easy to match” candidates may match with many potential donors, matches are seldom or never found because the candidate’s paired donor is difficult-to-match due to non-O blood type or other factors. Currently, the optimization algorithm used to find OPTN KPD exchanges is based on a set of priority points that does not include either the candidate or paired donor’s blood type, both of which affect the likelihood of a finding a match. The proposed revisions to the priority points include both a sliding point scale for CPRA and candidate and paired donor blood type to reflect the increased difficulty in matching candidates based on these traits. The proposal also includes other changes to the priority points intended to update a system developed in 2006. As a part of the revision to the OPTN KPD priority points, the proposed policy changes will also provide a remedy for OPTN KPD candidates that are part of a failed exchange. A failed exchange happens when a KPD candidate does not receive a transplant after their paired donor has donated. This proposal refers to these candidates as “orphan candidates.” The OPTN KPD does not currently have a remedy in place for failed exchanges outlined in policy. Although the OPTN KPD has not had any failed exchanges as of June 2015, this proposal outlines a remedy for failed exchanges in the event that one occurs. The Kidney Transplantation Committee (Kidney Committee) and KPD Work Group believe that these changes will improve equity in access to highly sensitized candidates and pairs with difficult to match blood types by increasing the number of priority points given to these pairs and increase the number of transplants in the OPTN KPD by increasing the number of matches found. Changes to Transplant Program Key Personnel Procurement Requirements (Membership and Professional Standards Committee) Some transplant program key personnel requirements in OPTN/UNOS Bylaws involving organ procurement experience stand to be updated. Specifically, the Bylaws addressed in this proposal are unnecessary due to the evolution of transplantation, unenforceable as currently written, inconsistent across the different transplant programs, or include periods to obtain necessary procurement experience that have been restrictive and problematic for some members. This proposal recommends Bylaws changes that address these issues and update transplant program key personnel procurement requirements. Proposed changes include deleting multi-organ procurement requirements for all key personnel, requiring that all primary transplant physicians must (as compared to “should”) observe three procurements of the organ that corresponds to the transplant program they are applying to be the primary physician of, removing “selection and management of the donor” requirements from the primary liver transplant surgeon pathways, and extending the time period for performing the requisite number of procurements in each primary transplant surgeon training pathway. Clarifying and updating these Bylaws primarily supports the OPTN strategic plan key goal of promoting the efficient management of the OPTN. Proposal to Reduce the Documentation Shipped with Organs (Organ Procurement Organization Committee) OPTN/UNOS Policy 16.5.A (Organ Documentation) states that members must send the complete donor record in the container with each transported organ. These requirements originated prior to the availability of electronic medical records and the functionality to upload information into DonorNet®. The OPO Committee discussed strategies to reduce the amount of documentation that is packaged and shipped with each organ, to allow OPO transplant coordinators more time to focus on donor management. The OPO Committee proposes limiting the required documentation to blood type source documentation and infectious disease testing results. OPOs will continue to provide all other pertinent donor information electronically. 10:35 OPTN/UNOS Update (20 minutes) Stuart Sweet, MD, PhD OPTN/UNOS Vice-President 10:55 OPTN/UNOS Committee Reports and Voting on Public Comment Proposals Moderator: Kenneth Washburn, MD ** Lunch will be served at 12:30** Data Advisory Committee Dr. Sweet Proposal to Revise OPTN/UNOS Data Release Policies (15 min) page 99 Current OPTN/UNOS policy restricts the release of organ procurement organization (OPO)- and hospitalidentified data, even though the OPTN Final Rule (the Final Rule) requires the OPTN to release data in response to “reasonable requests from the public for data needed for bona fide research or analysis purposes” and “reasonable requests from the public for data needed to assess the performance of the OPTN or Scientific Registry, to assess individual transplant programs, or for other purposes.” The Health Resources and Services Administration (HRSA) clarified that this portion of the Final Rule applies to release of data that is identified by transplant hospital or OPO, and therefore OPTN/UNOS policy is not consistent with the Final Rule. The OPTN/UNOS Data Advisory Committee (DAC) is proposing changes in response to this interpretation of the Final Rule. This proposal revises the OPTN/UNOS Data Release policy to better align with the Final Rule by removing restrictions on the release of OPTN data. This will allow the OPTN contractor to release more data than are currently released, including any non-confidential data by institution (e.g., data identifiable by transplant hospital, histocompatibility lab, or OPO). As allowed in the Final Rule, UNOS staff will still evaluate data requests for reasonableness, but the process for doing so will not reside in OPTN policy. Pediatric Transplantation Committee Gregory Abrahamian, MD UTHSC at San Antonio Proposal to Establish Pediatric Training and Experience Requirements in the Bylaws (15 min) page 9 The National Organ Transplant Act (NOTA) requires that the OPTN “recognize the differences in health and in organ transplantation issues between children and adults throughout the system and adopt criteria, policies, and procedures that address the unique health care needs of children.” Although pediatric transplantation is an accepted subspecialty within the field of transplantation, the current OPTN Bylaws do not include any requirements in order for programs to be approved to perform pediatric transplants. As early as 1993, the Membership and Professional Standards Committee (MPSC) has sought guidance from the Pediatric Transplantation Committee in establishing pediatric requirements so it could better assess key personnel applications. The Committee proposes that a designated transplant program must have an approved pediatric component in order to perform transplants in patients less than 18 years old. To be approved for a pediatric component, a program must identify a qualified primary pediatric surgeon and a qualified primary pediatric physician to serve as key personnel. By establishing pediatric membership requirements, this proposal contributes to the OPTN Strategic Goals of improving transplant outcomes and promoting patient safety, while protecting access to transplantation. Thoracic Organ Transplantation Committee Mark Drazner, MD, MSC UT Southwestern Medical Center Committee Update (10 min) Proposal to Modify Pediatric Lung Allocation Policy (10 min) page 200 On May 31, 2013, former Secretary of Health and Human Services, Kathleen Sebelius, requested that the OPTN review lung allocation policy, with “particular attention to the age categories used in allocation” and the “intent of identifying any potential improvements to this policy that would make more transplants available to children, consistent with the requirements of the OPTN final rule.” As an immediate measure, the OPTN/UNOS Board of Directors approved the Adolescent Classification Exception for Pediatric Candidates, which allowed lung candidates less than 12 years old to request an exception from the Lung Review Board to be classified as an adolescent candidate for the purposes of prioritization by Lung Allocation Score (LAS). Following its passage, the Thoracic Organ Transplantation Committee conducted a more comprehensive review of lung allocation policy and identified two additional opportunities for improving access to transplant for all pediatric candidates less than 18 years old. The Committee proposes broader geographic sharing of pediatric donor lungs. This will give candidates less than 18 years old better access to properly sized donors, which aligns with Goal 2 of the OPTN Strategic Plan. The Committee also proposes establishing eligibility criteria for candidates registered prior to their second birthday to receive a deceased donor lung of any blood type. This will increase utilization of the smallest donor lungs and decrease waiting list mortality among infants, which supports Goals 1 and 3 of the OPTN Strategic Plan. Transplant Administrators Committee Update (5 min) Susan Zylicz, MHA, BSN, RN, CCTC The Methodist Hospital Kidney Transplantation Committee Steven Potter, MD, FACS East Texas Medical Center Committee Update (15 min) Simultaneous Liver Kidney (SLK) Allocation Policy (20 min) page 236 Current OPTN policy prioritizes candidates seeking a simultaneous liver kidney (SLK) transplant before pediatric and adult transplant candidates who are listed only for a kidney (“kidney alone candidates”) when the liver candidate and the deceased donor are in the same Donation Service Area (DSA). Unlike kidney alone allocation, in SLK allocation, the kidney is not allocated based on medical criteria assessing the kidney function of the candidate. Instead, geographic proximity between the liver-kidney candidate and the donor is the single factor for allocating the kidney with the liver. Organ Procurement Organizations (OPOs) are not required to allocate the kidney with the liver to a regional SLK candidate, although they have the discretion to do so. The Kidney Transplantation Committee (“the Committee”), has identified several problems with this current policy: The current policy for SLK allocation is counter to requirements in the OPTN Final Rule (“Final Rule”) specifying that organ allocation policies be based on sound medical judgment and standardized criteria. These requirements are in place to ensure equity and efficiency in the U.S. organ allocation system—to promote a system where all candidates are assessed and organs are allocated equitably based on some level of medical need. The lack of medical criteria results in the allocation of high quality kidneys to liver candidates who may regain renal function after liver transplant and decreased access for kidney alone candidates who would otherwise be highly prioritized in deceased donor kidney allocation. The lack of consistency for regional SLK allocation has been a tremendous concern for the liver transplant community, as deceased donor liver allocation prioritizes candidates with a certain medical urgency status or Model End Stage Liver Disease Score (MELD) score or Pediatric End Stage Liver Disease (PELD) score for regional allocation but regional SLK allocation is not required. In order to provide more clarity and consistency in the rules for SLK allocation, the Committee is proposing the following new policies: Establish medical eligibility criteria for candidates seeking an SLK transplant. Because there is somewhat limited data to establish new rules, the Committee has relied on clinical consensus and feedback from experts in kidney and liver transplantation to establish the criteria. Establish a “safety net” (some match classification priority on the kidney alone waiting list for liver recipients with continued dialysis dependency or kidney dysfunction in the first year after liver transplant) as an added element to address concerns about limitations associated with the SLK medical eligibility criteria. This proposal reflects feedback from the 11 OPTN regions, several professional transplant societies, patient advocacy groups, and various OPTN/UNOS committees. The proposal is intended to further the OPTN strategic goal to “provide equity in access to transplants” by addressing the objective to “establish clearer rules for allocation of multiple organs to a single candidate, especially liver-kidney candidates.” Because there is a tremendous amount of transplant community interest in the development of this policy and a need to ensure a high level of consensus for the final product, the Committee may utilize the Fall 2015 and Spring 2016 public comment periods to receive input on these changes, with an expectation that the OPTN/UNOS Board of Directors will consider final adoption at the June 2016 Board meeting. HRSA Workplace Partnership for Life Hospital Campaign (5 min) Beth Hannan LifeShare Transplant Donor Services of Oklahoma Donate Life America Update (5 min) Suzy Miller Donate Life Texas Membership and Professional Standards Committee Adam Bingaman, MD, PhD Methodist Specialty and Transplant Hospital Committee Update (5 min) Addressing the Term “Foreign Equivalent” in OPTN/UNOS Bylaws (15 min) page 127 OPTN/UNOS Bylaws’ transplant program key personnel requirements use the term “foreign equivalent.” Specifically, transplant program key personnel are required to have current American board certification or the “foreign equivalent,” and cited experience must have been obtained at a designated transplant program or the “foreign equivalent.” This term is unclear for members when assessing if certain staff are qualified to serve as transplant program key personnel and for the OPTN/UNOS Membership and Professional Standards Committee (MPSC) when evaluating membership applications and determining if a board certification or case experience performed outside the United States should be considered equivalent. To address this problem, and after consideration by a Joint Societies Working Group, the MPSC proposes deleting the term “foreign equivalent” from the Bylaws (except for vascularized composite allograft (VCA) program key personnel); permitting board certification by the Royal College of Physicians and Surgeons of Canada in addition to American board certification; and establishing a new process for those individuals who are not American or Canadian board certified to qualify as transplant program key personnel. These proposed changes are anticipated to advance the OPTN Strategic Plan key goals of promoting living donor and transplant recipient safety and the efficient management of the OPTN. Changing the Bylaws to better reflect the training and experience expected of transplant program key personnel should contribute positively to increased transplant recipient safety. Additionally, removing the ambiguous term “foreign equivalent” and providing a detailed option to qualify as key personnel for those who do not possess American board certification should help promote the efficient management of the OPTN. Pancreas Transplantation Committee Richard Ruiz, MD Baylor-Simmons Transplant Institute Committee Update (5 min) Proposal to Revise Facilitated Pancreas Allocation Policy (10 min) page 225 The Pancreas Transplantation Committee offer a proposal that will expedite organ placement by updating the mechanics of facilitated pancreas allocation. Such changes will combat a troubling trend of growing pancreas underutilization rates by shifting facilitated pancreas allocations from a list of volunteer programs to one of programs with a recent record of frequently importing pancreata external to their Donation Service Area (DSA). This proposal calls for the revision of Policy 11.7 by splitting it into two subsections; Policy 11.7.A: Transplant Program Qualifications outlines eligibility requirements for programs to participate while 11.7.B: Facilitated Pancreas Offers explains the process by which an organ procurement organization (OPO) or the Organ Center can use facilitated pancreas allocation. This proposal coincides with the first goal of the Organ Procurement and Transplantation Network’s (OPTN) Strategic Plan to increase the number of transplants by offering imported pancreata to those programs most likely to use them. Operations and Safety Committee Update (5 min) Nicole Johnson, MBA, BS, RN Baylor-Simmons Transplant Institute Policy Oversight Committee Jeffrey Orlowski, MS, CPTC LifeShare Transplant Donor Services of OKlahoma Proposal to Increase OPTN/UNOS Committee Terms to Three Years (10 min) page 191 Most OPTN/UNOS committee members currently serve terms of two years, with the exception of the Patient Affairs (PAC), Transplant Administrators (TAC), and Ethics committees, who serve three-year terms. Committee members and committee leadership have expressed that it would be beneficial for all committee members to serve three-year terms to decrease committee turnover, enable members to continue work on long-term projects, and retain needed historical knowledge and expertise for a longer period. Living Donor Committee Shannon Edwards UNOS Regional Administrator Proposal to Establish and Clarify Policy Requirements for Therapeutic Organ Donation (10 min) page 114 This policy proposal would establish or clarify which policy requirements apply for the informed consent, psychosocial and medical evaluation and follow-up reporting for therapeutic donors. Liver and Intestine Committee Update (5 min) Vivek Kohli, MD, FACS INTEGRIS Baptist Hospital Histocompatibility Committee Update (5 min) Chantale Lacelle, PhD UT Southwestern Medical Center 3:00 Adjournment