DB_SP_Disposal of Dead Bodies
advertisement

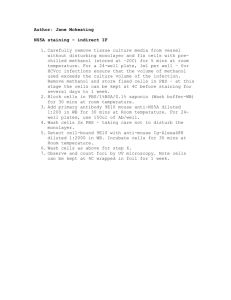
WASH Cluster – Management of Dead Bodies DB Session Plan DB- Management of Dead Bodies Timetable DB – Management of dead bodies 1hr 30 mins Session-at-a-Glance Session Activities Introduction and Objective setting Discussion on the public health importance of dead bodies in terms of risks to the public and those responsible for handling the dead Approx. Time 5 mins 30 mins Instructional Activity Powerpoint presentation Plenary discussion and powerpoint Group exercise on managing dead bodies 20 mins Group Work Presentation of group work 10 mins One group to present back using flipchart paper Presentation by facilitator on key aspects of managing dead bodies with focus on protecting body handlers, methods of disposal and selection of burial sites. 10 mins Powerpoint Presentation by facilitator on management of highly infectious bodies ie Cholera or Ebola 10 mins Powerpoint Discussion to establish if session objectives have been met 5 mins Powerpoint Total time 1 hr 30 mins Session Aims To put the issue of dead bodies into a public health perspective (including psycho-social aspects) and understand the basics of managing dead bodies in the first phase following a disaster. Session Objectives By the end of the session participants will be able to: Describe the relative importance of dead bodies in an emergency (health risks to the public and those handling the dead) Develop an action plan to manage dead bodies in a practical sense following a disaster List 3 extra precautions needed in dealing with those who have died from a highly infectious disease such as cholera or Ebola. 1 WASH Cluster – Management of Dead Bodies DB Session Materials Computer and projector Flip chart paper and pens Handout - Special Precautions for dealing with dead bodies in relation to Cholera, Ebola, SARS, Typhus/Plague, Tuberculosis and HIV/AIDS. Key Learning Points Dead bodies are generally speaking not a major public health risk in the immediate aftermath of a disaster Dead bodies require careful management and those that have died from highly infectious causes need extra special attention in their management. Facilitator Guidance • PAHO et al, Management of Dead Bodies after Disasters: A field manual for first responders, 2006 • MSF, Infection Control in Health Care Settings, First Edition, 2006. • Harvey, Peter., Baghri, Sohrab., and Reed, Bob., Emergency Sanitation, Assessment and Programme Design, WEDC, Loughborough University 2002 • UNHCR, Handbook for Emergencies, Third Edition, February 2007. (Pg 277) • Davis, Jan., and Lambert, Robert., Engineering in Emergencies, A practical guide for relief workers. 2nd Edition, RedR/IT, 2002 (Pg 182-183) • Disposal of Dead Bodies in emergency conditions, WHO, Technical Note No. 8 Draft Revised 7.1.05 Session plan Read the slide Read the slide Read the slide Session Plan – DB 2 WASH Cluster – Management of Dead Bodies DB Read the slide Read the slide Generate discussion to see who in the group would prioritise the needs of survivors over the disposal of the dead. In general the dead do not pose a major physical public health risk no matter what the type of emergency be it a complex emergency, earthquake or flood when the victims have died from some sort of trauma such as injury, drowning or fire and not from a disease. Seek to establish if any of the group identify those who have died from highly infectious diseases (a disease epidemic type of emergency) such as cholera as of major public health importance. Seek to establish what other highly infectious diseases are important in this regard – examples include Cholera, Ebola, Typhus, Plague and Marburg. Read the Quote Note: There is the potential risk to drinking water supplies contaminated by faecal matter released from dead bodies. However this risk is as yet undocumented. Ask the question The psychological trauma of losing loved one and witnessing death on a large scale is at the very least distressing. Therefore the collection of corpses following a disaster is an important consideration to minimise this distress. The hasty collection and disposal of corpses (in the mistaken belief that these dead will create an epidemic) can also have severe long term mental health consequences and legal problems for the relatives of the victims. It can be traumatic for relatives if they don’t know if a person has died or not and if they have died where there remains are buried. If they can’t prove someone is dead this may cause legal problems. Read the quote It is not necessary to rush the disposal of bodies (burials or cremations). This does not allow for the correct identification and record taking of the details of the dead. Nor does it give the time for the bereaved to carry out the ceremonial and cultural practices, which would normally occur after a death. This is important in helping people deal with the psychological impact and allowing time for such practices to take place helps the process of disaster recovery. (Source: Dispoal of Dead Bodies in emergency conditions, WHO, Technical Note No.8, Draft revised Session Plan – DB 3 WASH Cluster – Management of Dead Bodies DB 7.1.05) Ask the question Purpose of slide is to get group to think about the specifics of dealing with the dead if they have a responsibility for it regardless of where it fits within the general list of public health priorities. Read the slide Individuals handling remains have a small risk through contact with blood and faeces (bodies often leak faeces after death) Note: most infectious organisms do not survive beyond 48 hours in a dead body. An exception is HIV, which has been found six days post mortem. There are non-infectious risks such as injury from working in collapsed buildings. Tetanus is another risk from working in such hazardous environments. Organise group into their working groups While groups are working they should be directed to think about the specifics of collecting dead bodies. In particular they should be asked to provide details on how staff collecting dead bodies are protected from health and safety risks. This would include personal protective equipment such as heavy duty gloves and boots, facilities to wash their hands with soap and water after handling dead bodies, the availability of first aid for team members who may have an accident and tetanus vaccination for workers with vaccination cover. The hot season factor will bring added urgency to the task and with the population being Christian this will raise questions about the method of disposal The following page outlines the key steps to managing dead bodies and group can be referred to PAHO manual for greater detail. Read the slide These are the key steps to be followed as outlined in the PAHO Manual The affected people in scenario were Christian and therefore burial would have been the method of disposal utilised. Next slide will focus more specifically on Disposal, an issue of major concern for WASH people. Session Plan – DB 4 WASH Cluster – Management of Dead Bodies DB Read the slide Ask the question Group should identify burial as the preferred option over cremation for the reasons outlined on Pg 21 of PAHO manual. Burial helps preserve evidence for future forensic investigation if required. Cremation will destroy evidence for future identification, large amounts of fuel are needed, logistically difficult to arrange the cremation of large numbers of dead bodies. May largely depend on cultural and religious norms of the population affected. Ask the question Key points to refer to are sufficient space, soil conditions and highest point of the water table. Again see Pg 21 of PAHO manual. You may also make reference to the distance of burial sites from water sources and specific aspects around grave construction Ask the question Group should be asked to consider their work as WASH people not only in the general environment as in the Goma example but also the work they may undertake if working on WASH at a Health Care setting specifically like an isolation centre for Cholera victims. Read the slide and distribute handout Group to receive handout on the Special Precautions for dealing with dead bodies in relation to Cholera, Ebola, SARS, Typhus/Plague, Tuberculosis and HIV/AIDS. Read this summary of key recommendations for WASH people Question group to ask if the specific objectives of the session have been met and if there are any final questions. Session Plan – DB 5 WASH Cluster – Management of Dead Bodies DB Read the slide and ask group if objective has been met Refer to these key references Session Plan – DB 6