Treatment of stress response to laryngoscopy and intubation with
advertisement

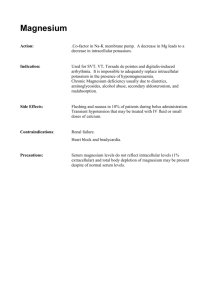
EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ahmed TREATMENT OF STRESS RESPONSE TO LARYNGOSCOPY AND INTUBATION WITH MAGNESIUM SULPHATE By Abbady A. Ahmed Department of Anesthesia and Intensive Care, Sohag faculty of Medicine ABSTRACT: Background: This prospective, randomized double-blinded study was designed to evaluate the efficacy of preoperative administration of magnesium sulphate in reducing stress response to laryngoscopy and intubation. Methods: Fifty adult patients were randomly assigned to one of two groups. The magnesium group (25 patients) received 10% magnesium sulphate and the control group (25 patients) received 0.9% sodium chloride in a double-blind manner. The magnesium group received magnesium sulphate 50 mg kg_1, administered as a slow intravenous bolus over a 10 min period before the induction of anesthesia. The same volume of isotonic saline was administered to the control group. No surgical manipulations were allowed till the end of magnesium sulphate infusion. Heart rate, systolic, diastolic, mean blood pressure, ECG changes and oxygen saturation (SPo2) were measured. Results: Both groups were comparable as regard to the demographic data. In control group there was a statistically significant increase in heart rate, systolic, diastolic and mean arterial blood pressure from the base line, and the maximum increase was at 3 minutes after intubation (p value <0.05). There was statistically significant increase in heart rate, systolic, diastolic and mean arterial blood pressure value in the control group following laryngoscopy and intubation in comparison to the study group (p<0.01). Conclusions: the use of magnesium sulphate attenuates the stress response to laryngoscopy and intubation. KEY WORDS: Magnesium sulphate Laryngoscopy Stress response Intubation. INTRODUCTION: Laryngoscopy and intubation violate the patient's protective airway reflexes and lead to physiological changes involving various systems of the body. Reflex changes in the cardiovascular system are most marked after laryngoscopy and intubation and lead to an average increase in blood pressure by 40-50% and 20% increase in heart rate 1. I.V. magnesium sulphate may be a good agent for deliberate hypotension because magnesium intervenes in the activation of membrane Ca ATPase and Na–K ATPase involved in transmembrane ion exchanges during depolarization and repolarization phases, and thus act as a stabilizer of cell membrane and intracytoplasmic organelles2. 191 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Magnesium also exerts its effects on L-type calcium channels in membranes and the sarcoplasmic reticulum. By inhibiting the calcium activation dependent upon the sarcoplasmic channel, magnesium limits the outflow of calcium from the sarcoplasmic reticulum3. In addition, magnesium sulphate acts as a vasodilator by increasing the synthesis of prostacyclin, as well as inhibiting angiotensin converting enzyme 4 activity . Magnesium sulphate has small, dose dependent myocardial depressant effect 5. In another study, the antagonist effect of magnesium at N-methyl-D-aspartate (NMDA) receptors has led to studies of its adjuvant effect in perioperative analgesia6. Ahmed and the anaesthetist who was in charge of the patients during the operation was unaware of the study medication. The magnesium group received magnesium sulphate 50 mg kg_1, administered as a slow intra-venous bolus over a 10 min period before the induction of anesthesia. The same volume of isotonic saline was administered to the control group. The patients were premedicated with glycopyrolate 0.2 mg I.V. administered just before their entry in the operation theatre. The patients were induced with thiopentone sodium 5 mg/kg after 4 minutes of magnesium sulphate infusion. Succinylcholine was given in a dose of 1-2 mg/kg. Anaesthesia was maintained with nitrous oxide, 50% in oxygen, Isoflurane 1.5% and vecuronium 0.1mg/kg. No surgical manipulations were allowed till the end of magnesium sulphate infusion.. An automatic noninvasive monitor (Nihon Kohden, Japan) was used to monitor Heart rate, systolic, diastolic, mean arterial blood pressure; preoperatively, before induction of anesthesia, and every minute for 5 minutes after laryngoscopy and intubation. ECG changes and oxygen saturation (SPo2) were monitored. Any adverse events or side-effects were recorded during the perioperative and postoperative periods. Data were presented as mean ± SD. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS 10.0). Differences between the two groups were subjected to the independent ttest. Paired t-test was applied to compare values of different observation time points with initial values. A statistical significance was regarded to any difference when p value <0.05. PATIENTS AND METHODS: This is a prospective randomized double-blinded clinical study. After study approval from the ethical committee of Sohag university hospital and written informed consents was taken, fifty patients belonging to ASA grade I, II were included in the study informed consent was obtained from all of them. Exclusion criteria included cardiovascular dysfunction, atrioventricular block, hepatic, renal or known allergy to magnesium sulphate or other study drugs, diabetic neuropathy, haematological disorders, history of neuromuscular disease, morbid obesity, pregnancy, prior treatment with calcium channel blockers, opioids and anticoagulants, and patients receiving magnesium supplementation, or drugs known to have a significant interaction with NMDAs. The patients were divided randomly into two groups. The magnesium group (25 patients) received 10% magnesium sulphate and the control group (25 patients) received 0.9% sodium chloride in a double-blind manner. The solutions were prepared RESULTS: The two groups were comparable with respect to age, body mass index (BMI), sex, and ASA 192 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 physical status (table 1). In magnesium group there was no statistically significant difference in heart rate, systolic, diastolic and mean arterial blood pressure from the base line (p value >0.05) (figure 1, table 2). In control group there was a statistically significant increase in heart rate, systolic, diastolic and mean arterial blood pressure from the base line, and the maximum increase was at 3 minutes after intubation (p value <0.05) (figure 1, table 2). There was statis- Ahmed tically significant increase in heart rate, systolic, diastolic and mean arterial blood pressure value in the control group following laryngoscopy and intubation in comparison to the study group (p<0.01) (figure 1, table 2). The use of magnesium sulphate infusion did not result in any kind of arrhythmias. In patients of control group undergoing laryngoscopy and intubation there was 4 patients (16%) showed ventricular ectopics and 3 patients (12%) showed dropped beats. Table 1: Shows demographic data for magnesium and control patients. MAGNESIUM CONTROL P<0.05 N=25 N=25 33±14 37.7±10 n.s Age (years) 28.5±4 29.1±4 n.s BMI(kg/m2) 15/10 14/11 n.s Sex (male/female) 19/6 20/5 n.s ASA I/II Data are presented as mean±standard deviation; BMI: body mass index. Heart rate changes for Magnesium and Control Patients pr e pr e op er at ive in du ct io n 1 m in ut e 2 m in ut e 3 m in ut e 4 m in ut e 5 m in ut e beat/minuts 140 120 100 80 60 40 20 0 Magnesium group Control group Figure 1: shows heart rate changes for magnesium and control patients. 193 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 Ahmed Table 2: Shows hemodynamic changes for magnesium and control patients. PREOP. PREIND. 1MIN 2 MIN 3 MIN 4 MIN 5 MIN SAP 126 ±7 112 ±9 121±6 145 ± 159±12 138±9 135±9 Control group MAP 95±6 85±7 89±10 116±9 124±7 119±9 112±10 N=25 DAP 80±7 72±8 79±6 97±8 104±8 99±8 88±6 SAP 124±12 104±7 89±6 78±6 82±5 78±7 76±56 Magnesium group MAP 95±7 82±8 70±6 66±7.8 67±6.1 65±5.9 65±6.3 N=25 DAP 81±62 69±74 65±54 59±67 60±64 58±67 55±76 Data presents as mean±SD. SAP; systolic arterial blood pressure, MAP; mean arterial blood pressure, DAP; diastolic arterial blood pressure, Preop; preoperative, Preind; before induction of anesthesia. systolic blood pressure after intubation. Plasma concentrations of epinephrine and norepinephrine were markedly lower after intubation in the magnesium sulphate -treated group10. Puri et al. compared hemodynamic changes during anesthesia induction and intubation after infusion of magnesium sulphate or lidocaine. The group treated with magnesium sulphate showed a slight increase in mean arterial pressure (MAP) and systemic vascular resistance and no decrease in cardiac output, as compared to the lidocaine group, with equally good control of increased heart rate11. In another study, the group treated with magnesium sulphate showed a lesser hypertensive response during induction compared to placebo, whereas early reflex tachycardia was not controlled by magnesium sulphate 12. Ashton et al. found no increase in arterial pressure or heart rate and a moderate decrease of plasma catecholamine concentrations after intubation in a group treated with magnesium sulphate alone before intubation13. Also Elsharnouby1 concluded that continuous infusion of magnesium sulphate led to a useful reduction in MAP and heart rate14. DISCUSSION: Reflex changes in the cardiovascular system after laryngoscopy and intubation are most marked. They manifest themselves in the form of tachycardia, hypertension and cardiac arrhythmias1, ectopics being most common. Less commonly we may encounter bradycardia as a result of vagal stimulation during laryngoscopy. Therefore, the anesthesiologist must be careful so as not to over treat these responses and create more difficulties then the original problem7. A wide variety of pharmacological agents were used to attenuate the hemodynamic responses like esmolol7, Fentanyl8, bupre-norphine4, alfentanyl9 etc. In our study, the magnesium group received magne-sium sulphate 50mg/kg as a slow i.v. bolus in a 10 min period before the induction of anesthesia. This resulted in a steady and smooth reduction in arterial blood pressure and reduced heart rate in with catecholamine release. Magnesium sulphate reduces this release by the adrenal medulla and adrenergic nerve endings. In a similar study, patients received thiopental and Succinylcholine with or without magnesium sulphate 60mg/kg at anesthesia induction. Patients treated with magnesium sulphate showed a lower increase of heart rate and We conclude that the use of magnesium sulphate attenuates the 194 EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 stress response to laryngoscopy and intubation. Ahmed 8. Kindler CH, Schumacher PG, Schneider MC, Urwyler A. Effects of intravenous lidocaine and/or esmolol on haemodynamic responses to laryngoscopy and intubation: a double blind, controlled clinical trial. Journal of Clinical Anaesthesia 1996; Sept; 8(6):491-6. 9. Korenga GM, Kirkpatrick A, Lord JG, Barbaras E et al. Effect of esmolol on tachycardia induced by endotracheal intubation. Anesth Analgesia 1985; 64:185-304. 10. James MFM, Beer RE, Esser JD. Intravenous magnesium sulfate inhibits catecholamine release associated with tracheal intubation. Anesth Analg 1989; 68:772–6. 11. Puri GD, Marudhachalam KS, Chari P, Suri RK. The effect of magnesium sulphate on hemodynamics and its efficacy in attenuating the response to endotracheal intubation in patients with coronary artery disease.J Anesth Analg 1998; 87: 808–11. 12. Yap LC, Ho RT, Jawan B, Lee JH. Effects of magnesium sulfate pretreatment on succinylcholine-facilitated tracheal intubation. Acta Anaesthesiol Sin 1994; 32: 45–50. 13. Ashton WB, James MFM, Janicki P, Uys PC. Attenuation of the pressor response to tracheal intubation by magnesium sulphate with and without alfentanil in hypertensive proteinuric patients undergoing caesarean section. Br J Anaesth 1991; 67: 741–7. 14. Elsharnouby1 N. M, and M. M. Elsharnouby. Magnesium sulphate as a technique of hypotensive anaesthesia. British Journal of Anaesthesia 2006:96 (6): 727–31. REFERENCES: 1. Bruder N, Granthil C, Ortega D. Consequences and prevention methods of hemodynamic changes during laryngoscopy and intubation. Ann Fr Anaesth Reanim 1992; 11(1):57-71. 2. Telci L., Esen F., Akcora D., Erden T., Canbolat A. T. and Akpir K. Evaluation of effects of magnesium sulphate in reducing intraoperative anesthetic requirements. British Journal of Anaesthesia, 2002; 89:594602. 3. Reinhart RA. Clinical correlates of the molecular and cellular actions of magnesium on the cardiovascular system. Am Heart J 1991; 121: 1513–21. 4. Sanders GM, Sim KM. Is it feasible to use magnesium sulphate as a hypotensive agent in oral and maxillofacial surgery? Ann Acad Med Singapore 1998; 27: 780–5. 5. Jee D., Lee D, Yun S. and Lee C. Magnesium sulphate attenuates arterial pressure increase during laparoscopic cholecystectomy. Br J Anaesth. 2009 Oct; 103(4):484-9. Epub 2009 Jul 17. 6. Dube´ L, Granry JC. The therapeutic use of magnesium in anesthesiology, intensive care and emergency medicine: a review. Can J Anesth 2003; 50: 732–46. 7. Saif Ghaus M, Vinita S, Kumar A, Wahal R., Bhatia V K, Agarwal J. A study of cardiovascular response during laryngoscopy and intubation and their attenuation by ultrashort acting b-blocker esmolol.Indian J. Anaesth. 2002; 46 (2) : 104-106p. 195 Ahmed EL-MINIA MED. BULL. VOL. 20, NO. 2, JUNE, 2009 الملخص العربى معالجة رد اإلجهاد إلى منظار الحنجرة وادخال االنبوبة الحنجرية بسلفات الماغنسيوم عبادى عبد الاله أحمد قسم التخدير والعناية المركزة كلية طب سوهاج الهدف من البحث - :إستععمل ستلتلا الملسيست فى تتى عخت تف رد اإلجهتلد إلتى ميرتلر الحيجتر فادخل االيبفبة الحيجر ة. طرق البحث فأدفاعه - :عى إجراء هذا البحث على خمسفن مر ضل بللغتل سستمف بلتع علتفا ى إلى مجمفعع ن. مجمفعة سلتلا الملسيس فى 25مر ض أختذا %01ستلتلا الملسيست فى فالمجمفعتة الي لست ة 25مر ض أخذ ا 1.0علفر د الصفد فى. الي لسلا - :فجد ز لد هلمة بلع إحصل ى تى معد ضربلا اليلت فضتغط التدى االييبلضتى فااليبسلطى فمعفسط ضغط الدى تى المجمفعة الي لس ة بللميلرية بمجمفعة سلتلا الملسيس فى. فجد تى هذه الدراسة أن إسععمل سلتلا الملسيس فى ختف من رد اإلجهلد إلى ميرلر الحيجر ف ادخل االيبفبة الحيجر ة. 196