Obstetric case exam case
advertisement
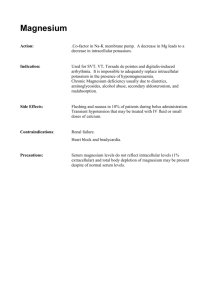
Case Commentary An 18-year-old, 62 kg lady is admitted in labor, she is 6-cm dilated and screaming. Her BP is 170/100, HR 100, R 24, and temp 37,5°C. ECG & CXR attached 1 2 Preoperative questions: Q: Which labs will you want and why? Hematocrit -Want to know where we're starting in case blood loss gets problematic. Her blood pressure may be that high due to the pain of contractions, but that pressure does qualify for preeclampsia, so I'd want a PT, PTT, and platelet count, LFTs and urea & creatinine . Q: What is the utility of a bleeding time? Bleeding time supposedly ties it all together, but the bother of doing it, plus the variability of the technician’s interpretation, renders the test of little use. I wouldn't get one. Q: What special considerations do you have in the airway exam? The pregnant patient has a swollen, friable airway. If she has preeclampsia on top of that, then the airway will be even worse. Large breasts may interfere with the laryngoscope handle. The gravid uterus reduces FRC and will lead to rapid desaturation. Finally, the stomach is full, posing an aspiration risk. Q: if between contractions, her blood pressure falls to 110/65, Does this patient have preeclampsia? Preeclampsia encompasses the triad of hypertension, edema, and proteinuria. Edema may be hard to tell from the generalized swelling of pregnancy, but a urine dipstick will show if there is proteinuria. As this patient's blood pressure is not sustained, then she most likely does not have preeclampsia. Her blood pressure was most likely up from the pain of contractions. Q: What is the upper limit of normal blood pressure? What is the classification of hypertension during pregnancy? A blood pressure of 130/80 is the upper limit of normal at any time during pregnancy. There are three types of hypertension: •Pregnancy-induced hypertension (PIH) Preeclampsia Eclampsia Gestational hypertension (late or transient hypertension of the 3rd trimester) •Coincidental hypertension (chronic hypertension preceding pregnancy) •Chronic hypertension with superimposed PIH Superimposed preeclampsia Superimposed eclampsia Q: Define gestational hypertension and chronic hypertension? Gestational hypertension is hypertension without proteinuria or generalized edema during the last weeks of pregnancy or immediately after delivery. 3 Chronic hypertension is persistent hypertension, regardless of etiology, before the 20th week of gestation or beyond 6 weeks after delivery. 8. What is the difference between preeclampsia and eclampsia? Eclampsia means preeclampsia plus seizures. 9. Discuss the characteristics of convulsions in eclampsia. Eclampsia can develop in the presence of either mild or severe preeclampsia. The convulsion is grand mal in character and appears before, during, or after delivery. Any seizure that occurs more than 48 hours postpartum is due to other CNS lesions. Q: Discuss the pathophysiologic alterations of preeclampsia in different organs? The underlying condition is vasoconstriction caused by circulating levels of renin, angiotensin, aldosterone, and catecholamines. Hematologic Changes •There is a decrease in circulating blood volume, primarily plasma, in spite of excess total body sodium and water, resulting in hemoconcentration. •Increased blood viscosity aggravates the existing decreased perfusion. •Despite increased hematocrit and hemoglobin, relative anemia usually exists; these patients tolerate blood loss poorly. •A disseminated intravascular coagulopathy is characterized initially by reduction in platelet count; later by a rise in fibrin degradation product, a fall in fibrinogen level, and prolongation of partial thromboplastin time and prothrombin time. Cerebral Changes •Hyperreflexia and CNS irritability increase. •Coma can occur without eclampsia. •Increased intracranial pressure can be exacerbated by hypercarbia, metabolic acidosis, and hypoxia. Respiratory Changes •Upper airway and laryngeal edema occurs. •Overloading with fluid can lead to pulmonary edema with left ventricular failure. •The oxyhemoglobin dissociation curve may shift to the left, decreasing the availability of oxygen to the fetus. Cardiovascular Changes Arteriolar constriction and peripheral resistance increase, leading to increase in blood pressure. Volume expansion may cause ventricular overloading and cardiac failure. Ophthalmic Changes •There is retinal arteriolar spasm. Bilateral retinal detachment, owing to massive edema in the retina, occurs in severe cases and can result in blindness. 4 Uterine Changes •The uterus is hyperactive and markedly sensitive to oxytocin. Rapid labor and painful contractions are common. The placenta shows signs of premature aging and has infarcts, fibrin deposits, calcifications, and/or abruption. Renal Changes •Decreased urate clearance results in the well-recognized increase in serum uric acid concentration. This occurs earlier than reduction of the glomerular filtration rate. •There is a reduction in filtration fraction (glomerular filtration rate/renal plasma flow). •Renal lesions consist of glomerular capillary endothelial swelling with narrowing of glomerular capillaries owing to severe swelling of endothelial cells. There is deposition of fibrin in glomeruli, which is pathognomonic of the disease. •Proteinuria results from increased permeability of damaged renal glomeruli. Hepatic Changes •In severe cases, there is hepatocellular damage owing to periportal hemorrhage from vasospasm. There have been subcapsular hematomas. Rupture of the liver is a rare occurrence. The hepatic swelling produces epigastric pain. •Elevation of liver enzymes has been reported. •Hemolysis occurs as jaundice secondary to hepatocellular damage and heme pigment deposited in body stores. This may progress to fatty metamorphosis of the liver and ultimately to death. Q: What is the contraction stress test (oxytoxin stress test)? Oxytoxin is given to mimic labor. Three uterine contractions in 10 minutes without fetal rate decelerations related to the contractions is considered a negative test. If 3 consecutive contractions are followed by a "late" deceleration, there is evidence of uteroplacental insufficiency and delivery is indicated. Q: What is the first line of treatment for preeclampsia? Discuss its actions. Magnesium sulfate is the initial therapy for the prevention of convulsions and hypertension. Eclamptic convulsions are prevented at a plasma magnesium level of 4 to 6 mEq/liter. Actions of magnesium are: •Magnesium is a central nervous system depressant and anticonvulsant. •Magnesium inhibits the release of acetylcholine at the neuromuscular junction, decreases the sensitivity of the motor end-plate to acetylcholine, and decreases muscle membrane excitability. •Magnesium decreases uterine hyperactivity by its mild relaxant effect on vascular and uterine smooth muscle, thereby improving uterine blood flow. •It diminishes fibrin deposition and improves renal and hepatic circulation, therefore relieving hepatic pain. •It is a mild vasodilator and has a mild antihypertensive effect. 5 Q: What is the suggested regimen using magnesium sulfate? An initial bolus of 4 to 6 g in a 20% solution is given intravenously over 5 minutes followed by continuous infusion of 2 g/hr. If the initial treatment of 4 g does not control convulsions, an additional 2 g to 4 g can be administered intravenously. If seizures persist, 10 mg of diazepam should be slowly given intravenously. Q: How would you judge the therapeutic effects of magnesium sulfate? Clinical signs, such as knee jerks (present but hypoactive) and respiratory rate (more than 10 to 12 per minute), are helpful in monitoring its administration. The absence of deep tendon reflex indicates impending magnesium toxicity, which occurs at about 10 mEq/liter. If urine output is less than 30 cc/hr, decrease or stop magnesium administration. The therapeutic range of plasma level of magnesium is 4 to 8 mEq/liter. (Normal plasma level is 1.5 to 2 mEq/liter.) Q: What precautions should be taken in using magnesium sulfate? •Magnesium is excreted by the kidneys. It must be used cautiously in patients with preexisting renal disease. Intake and urine output must be monitored with an indwelling Foley catheter. •Magnesium potentiates nondepolarizing and depolarizing muscle relaxants. A nerve stimulator must be used. During surgery, muscle relaxants must be used in smaller doses. •Magnesium potentiates the effect of sedatives and narcotics; therefore, their doses must be reduced Q: If the patient is having an eclamptic fit, what is the immediate therapy? •Initially, intravenous administration of thiopental, 50 mg to 100 mg, to terminate the convulsion. Further convulsions are treated with diazepam or magnesium sulfate. •Maintain adequate airway. Give oxygen to prevent hypoxia. Turn the patient to her left side, with head-down tilt, and elevate the chin. An endotracheal tube should be placed following administration of succinylcholine and cricoid pressure. •Bicarbonate may be needed after arterial blood gases and pH are determined, because convulsions are often associated with metabolic acidosis. Q: A toxicology screen shows cannabis in the blood, any further workup needed given these findings? Just look for other, more disturbing findings in the toxicology screen. If, for example, cocaine shows up, then the mother may suffer from hypertension or cardiac problems from long-term cocaine abuse. Nose bleeds, infectious hepatitis, and HIV could accompany IV abuse. The baby may be born addicted to cocaine and require NICU. 6 8. Physical exam reveals a 2/6 systolic murmur but no other findings, Do you need an echo? The high flow state of pregnancy often produces a "flow murmur." I would order an echo only if she had other symptoms, such as shortness of breath, orthopnea, or drop in exercise tolerance. Admittedly, each of these are hard to tell from the baseline state of advancing pregnancy. Intra-operative Questions: Q:What is your choice of anesthesia for PIH patients? Continuous lumbar epidural anesthesia is the best technique for managing patients with PIH. Q: To place the epidural, do you have her on her side or sitting up? Why? Sitting up. The advantage is the ease of finding the midline. On the side, the midline can sag away from you and you can get lost. Disadvantages: The struggle to get the patient sitting up Also, in the sitting position, the BP can drop or the fetal heart rate can drop. "The baby doesn't like it when she sits up," Also, if Be something goes toxic when the patient is sitting up, the patient will fall down, which is no fun. On their sides, there is no place to fall down But as I'm going for ease of insertion, I'd go with the sitting position. Q:What is the advantage of an epidural in this case? And disadvantage? An epidural provides an ongoing source of pain relief and path for C-section. A disadvantage is a less dense block if the case goes to C-section. Another disadvantage is the large dose of local anesthetic you need to use. If this large dose goes intravascular, you will have prolonged cardiac collapse. Q: First pass elicits a clear, gushing liquid not entirely unrelated to some CSF. Do you place a catheter and do a continuous spinal? Why or why NOT? I would NOT place a continuous spinal, as this has been associated with nerve root irritation. Better to pull out, go to another level. Note this patient's name, as you will be back to treat spinal headache later on. Explain, as best you can, what happened so she will know what to expect. Q:How would you manage total spinal anesthesia? •Maintain venous return by left uterine displacement, Trendelenburg position, and cystalloid intravenous fluids. •Ventilate with oxygen and intubate after oxygenating. •Give ephedrine for hypotension. (Phenyl ephrine or adrenaline) •Give anesthesia when stable (if necessary). 7 •Within 10 to 20 minutes after stabilization of ventilation and circulation, withdraw CSF using the epidural catheter (twice the volume of local anesthetic that was accidentally injected). At least 10 ml should be withdrawn; replace with 2 to 3 times the volume of preservative-free normal saline or lactated Ringer's solution. Q: You place the epidural elsewhere and aspirate blood. What will you do? Aspirating blood means pull the catheter out. Flushing a little and pulling back a little may just land you in the epidermis, so better to pull out and try again. Q:What level of epidural anesthesia should be reached in preeclamptic patients? The level of epidural for preeclamptic patients is not different from that for normotensive patients. For labor pain, the segmental band of T10 to L1 provides analgesia for uterine contractions. As the second stage of labor is entered, the block can be extended to the perineum (S1 to S5). Fentanyl, 50 to 75 mcg, is added to the local anesthetic. For cesarean section, the block is extended gradually to T2 to T4; the blood pressure must not drop suddenly. Left uterine displacement should be maintained at all times until delivery. Q: At 8 cm, the fetal heart rate drops to 60. While they're preparing for a Csection, you try to buy some time. The patient is on Pitocin. What measures can you take? Fix the basic stuff first; left uterine displacement. If that fails, she may be in the 10% that need right uterine displacement. Stop the Pitocin, this may be making the uterus contract too vigorously and cause uteroplacental insufficiency. Give supplemental oxygen. Treat hypotension with fluids and ephedrine. Q: Heart rate stays down, now it's time perform a "Caesarean delivery." What steps do you take in preparation? Do you give antacids? If so, which and why? In this quick, quick, quick to the OR, there is no time for antacids. Get the epidural dosed up if you can. Two percent lidocaine injected as you go down the hall can and does get you a level. The goal is to avoid a general if you can, especially since you have a working epidural in Q: Incision is made and the patient screams. What do you do? You have inadequate surgical anesthesia and surgery has begun. Perform a general anesthetic. Limping through on ketamine is a halfway attempt at salvaging a regional is NOT a good idea Q: You induce and can't intubate but can ventilate. What do you do? I would proceed with maintained cricoid pressure. If you attempt to wake her up and do an awake intubation, she will be in agony from the incision and cooperation will be hard to come by. I would call for extra anesthesia hands, place an LMA. I would tell 8 the obstetrician my troubles and ask for their help, specifically, avoid externalizing the uterus. Q: Why in pregnancy there is increased risk of Regurgitation and Aspiration? A: . Delayed gastric emptying . Incompetent lower oesophageal sphincter . Placental Gastrin increase HCL secretion . Progesterone decreases gastrointestinal Motility Q: What are the modifications of a standard general anesthesia technique in PIH patients? •Use a smaller endotracheal tube because of the exaggerated edema of the upper airway. •Defasciculation prior to succinylcholine is not necessary if the patient is receiving magnesium sulfate. •Administer lidocaine, 100 mg IV, 3 to 5 minutes before induction to prevent rise of blood pressure during intubation. •Administer succinylcholine, 1.5 mg/kg, to ensure rapid complete relaxation for intubation. •Titrate the dose of muscle relaxants, nondepolarizing and depolarizing, because of the interactions with magnesium sulfate. Use a nerve stimulator before injecting additional muscle relaxant. •Avoid potentiating nephrotoxic or hypertensive drugs, such as methoxyflurane or ketamine exceeding 0.75 mg/kg. •Use a low dose (i.e., two-thirds minimum alveolar concentration) of halothane, enflurane, or isoflurane to prevent intraoperative hypertension. •Magnesium sulfate should not be discontinued during the intraoperative and postoperative period. •Antihypertensive drugs can be given as required. Q: if the Placenta failed to separate and Uterine Atony resulted with uncontrolled Bleeding that necessitate massive blood transfusion 1- How to define Massive Blood Transfusion? 2- What are the complications? 3- If you noticed bleeding from puncture sites as well as Haematuria What will be your differential diagnosis? A: 1- Massive blood transfusion is - ONE total blood volume replacement - Transfusion of more than 10 units PRBCs 2- Complications - Dilutional Coagulopathy ( Platelets and Clotting factors ) - Hypocalcaemia ( Citrate Binding ) 9 - Metabolic Alkalosis ( that could compensate for the metabolic acidosis Resulted from Hypoperfusion ) 3- Differential Diagnosis - Disseminated intravascular Coagulopathy - Dilutional Thrombocytopenia or clotting factors V and VIII - Acute hemolytic reaction Q: How to confirm your diagnosis? A: 1- Platelet count rules out Dilutional Thrombocytopenia 2. Prolonged PTT . Low Fibrinogen level . High level of Fibrin degradation products ( FDPs ) All confirm Diagnosis of DIC 3- In Acute Hemolytic reaction . Under Anaesthesia Haematuria is diagnostic rather than bleeding disorders . Haematuria manifested earlier . Simultaneous tachycardia and hypotension ( Not Reliable ) Q: What are the Main lines of Management ? A: I - For Dilutional Thrombocytopenia and DIC Replacement Transfusion - Platelet Concentrate - Fresh Frozen Plasma - Cryoprecipitate II- If confirmed Acute Hemolytic Reaction . Stop blood transfusion . Enhance Diuresis . Alkalinization of Urine ( NaHCO3 50 meq/Kg ) . Re- Crossmatch of the remaining blood units . Maintain ABP Q: What is the HELLP syndrome and what is its importance? HELLP is the syndrome of hemolysis, elevated liver enzyme, and low platelets presented by a unique group of preeclamptic/eclamptic patients with or without the usual clinical findings of PIH. It is often misdiagnosed as a disorder unrelated to pregnancy. It can occur antepartum or postpartum. The recognition of this syndrome is important to prevent maternal and neonatal death. Findings include: •Hemolysis (H)-The peripheral blood smear shows microangiopathic hemolytic anemia with "burr" cells (contracted, distorted RBCs with spiny projections along the periphery); schistocytes (small, irregularly shaped RBC fragments. There is normal PT, PTT and fibrinogen in 96% of patients. •Elevated liver enzymes (EL)-abnormal function tests with elevated SGOT, SGPT, and hyperbilirubinemia (especially indirect bilirubin); elevated BUN and creatinine in half the cases. 10 •Low platelets-of less than 100,000/mm3 The main symptoms are malaise, nausea, epigastric pain, and edema. Hypertension may not be seen. Q: Discuss the postpartum care of preeclamptic patients. •Continue magnesium sulfate for 24 hours and, for eclamptic patients, for another 24 hours after the last postpartum convulsion. Twenty-five percent of eclampsia occurs in the puerperium; therefore, continuous monitoring is required. •Continue hydralazine or substitute with another long-acting antihypertensive agent, such as methyldopa. •Pain medications are required to avoid further convulsions; avoid Ergotrate or aspirin. Epidural narcotic (e.g., morphine) can provide sustained postoperative analgesia. •Maintain intravenous fluids-lactated Ringer's solution with 5% dextrose at 60 to 150 ml/hr, unless there is unusual fluid loss from vomiting, diarrhea, diaphoresis, or excessive blood loss. An appreciable fall in blood pressure very soon after delivery is due to excessive blood loss and not to miraculous dissolution of the vasospastic disease. When oliguria follows and the hematocrit decreases, then blood transfusion is indicated. 11