cortisol ria
advertisement
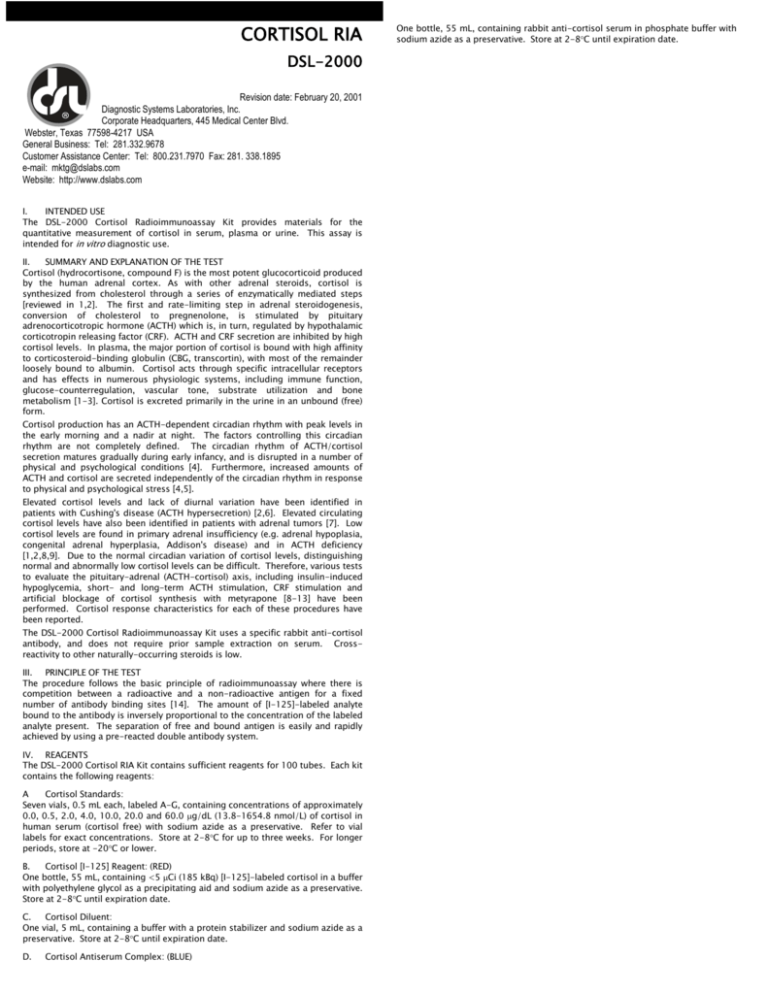
CORTISOL RIA DSL-2000 Revision date: February 20, 2001 Diagnostic Systems Laboratories, Inc. Corporate Headquarters, 445 Medical Center Blvd. Webster, Texas 77598-4217 USA General Business: Tel: 281.332.9678 Customer Assistance Center: Tel: 800.231.7970 Fax: 281. 338.1895 e-mail: mktg@dslabs.com Website: http://www.dslabs.com I. INTENDED USE The DSL-2000 Cortisol Radioimmunoassay Kit provides materials for the quantitative measurement of cortisol in serum, plasma or urine. This assay is intended for in vitro diagnostic use. II. SUMMARY AND EXPLANATION OF THE TEST Cortisol (hydrocortisone, compound F) is the most potent glucocorticoid produced by the human adrenal cortex. As with other adrenal steroids, cortisol is synthesized from cholesterol through a series of enzymatically mediated steps [reviewed in 1,2]. The first and rate-limiting step in adrenal steroidogenesis, conversion of cholesterol to pregnenolone, is stimulated by pituitary adrenocorticotropic hormone (ACTH) which is, in turn, regulated by hypothalamic corticotropin releasing factor (CRF). ACTH and CRF secretion are inhibited by high cortisol levels. In plasma, the major portion of cortisol is bound with high affinity to corticosteroid-binding globulin (CBG, transcortin), with most of the remainder loosely bound to albumin. Cortisol acts through specific intracellular receptors and has effects in numerous physiologic systems, including immune function, glucose-counterregulation, vascular tone, substrate utilization and bone metabolism [1-3]. Cortisol is excreted primarily in the urine in an unbound (free) form. Cortisol production has an ACTH-dependent circadian rhythm with peak levels in the early morning and a nadir at night. The factors controlling this circadian rhythm are not completely defined. The circadian rhythm of ACTH/cortisol secretion matures gradually during early infancy, and is disrupted in a number of physical and psychological conditions [4]. Furthermore, increased amounts of ACTH and cortisol are secreted independently of the circadian rhythm in response to physical and psychological stress [4,5]. Elevated cortisol levels and lack of diurnal variation have been identified in patients with Cushing's disease (ACTH hypersecretion) [2,6]. Elevated circulating cortisol levels have also been identified in patients with adrenal tumors [7]. Low cortisol levels are found in primary adrenal insufficiency (e.g. adrenal hypoplasia, congenital adrenal hyperplasia, Addison's disease) and in ACTH deficiency [1,2,8,9]. Due to the normal circadian variation of cortisol levels, distinguishing normal and abnormally low cortisol levels can be difficult. Therefore, various tests to evaluate the pituitary-adrenal (ACTH-cortisol) axis, including insulin-induced hypoglycemia, short- and long-term ACTH stimulation, CRF stimulation and artificial blockage of cortisol synthesis with metyrapone [8-13] have been performed. Cortisol response characteristics for each of these procedures have been reported. The DSL-2000 Cortisol Radioimmunoassay Kit uses a specific rabbit anti-cortisol antibody, and does not require prior sample extraction on serum. Crossreactivity to other naturally-occurring steroids is low. III. PRINCIPLE OF THE TEST The procedure follows the basic principle of radioimmunoassay where there is competition between a radioactive and a non-radioactive antigen for a fixed number of antibody binding sites [14]. The amount of [I-125]-labeled analyte bound to the antibody is inversely proportional to the concentration of the labeled analyte present. The separation of free and bound antigen is easily and rapidly achieved by using a pre-reacted double antibody system. IV. REAGENTS The DSL-2000 Cortisol RIA Kit contains sufficient reagents for 100 tubes. Each kit contains the following reagents: A Cortisol Standards: Seven vials, 0.5 mL each, labeled A-G, containing concentrations of approximately 0.0, 0.5, 2.0, 4.0, 10.0, 20.0 and 60.0 g/dL (13.8-1654.8 nmol/L) of cortisol in human serum (cortisol free) with sodium azide as a preservative. Refer to vial labels for exact concentrations. Store at 2-8C for up to three weeks. For longer periods, store at -20C or lower. B. Cortisol [I-125] Reagent: (RED) One bottle, 55 mL, containing <5 Ci (185 kBq) [I-125]-labeled cortisol in a buffer with polyethylene glycol as a precipitating aid and sodium azide as a preservative. Store at 2-8C until expiration date. C. Cortisol Diluent: One vial, 5 mL, containing a buffer with a protein stabilizer and sodium azide as a preservative. Store at 2-8C until expiration date. D. Cortisol Antiserum Complex: (BLUE) One bottle, 55 mL, containing rabbit anti-cortisol serum in phosphate buffer with sodium azide as a preservative. Store at 2-8C until expiration date. E. Cortisol Controls: Two vials, 0.5 mL each, Levels I and II, containing low and high levels of cortisol in human serum with sodium azide as a preservative. Store at 2-8C for up to three weeks. For longer periods, store at -20C or lower. VIII. TEST PROCEDURE A. Materials Supplied: Materials supplied in the DSL Cortisol RIA Kit, Catalog No. DSL-2000: MATERIAL NOTE: All reagents and samples must be allowed to reach room temperature (~25°C) and mixed thoroughly by gentle inversion before use. V. Cortisol Standard A Cortisol Standard B Cortisol Standard C Cortisol Standard D Cortisol Standard E Cortisol Standard F Cortisol Standard G Cortisol [I-125] Reagent Cortisol Diluent Cortisol Antiserum Complex Cortisol Serum Control Level I Cortisol Serum Control Level II PRECAUTIONS For in vitro diagnostic use. Radioactive material -- Not for Internal or External Use in Humans or Animals. This radioactive material may be received, acquired, possessed and used only by physicians, clinical laboratories or hospitals and only for in vitro clinical or laboratory tests not involving internal or external administration of the material, or the radiation therefrom, to human beings or animals. Its receipt, acquisition, possession, use and transfer are subject to the regulations and a general license of each country. The following precautions should be observed in handling radioactive material: Store radioactive materials in a designated area. Do not eat, drink, smoke, or apply cosmetics where radioactive materials are being handled. Do not pipet by mouth. Wear gloves when handling radioactive materials and wash hands thoroughly afterwards. Cover working area with disposable absorbent paper. Wipe up all spills immediately and thoroughly and dispose of the contaminated materials as radioactive waste. Dispose of the liquid radioactive waste into the sanitary sewage system if permitted by the local regulations. WARNING: POTENTIAL BIOHAZARDOUS MATERIAL This kit may contain reagents made with human serum or plasma. The serum or plasma used has been tested by an FDA approved method and found to be non-reactive for both the HIV-1/2 Antibodies, HCV and HBsAg. Because no method can offer complete assurance that HIV-1/2, HCV, HBsAg or other infectious agents are absent, these reagents should be handled at the Biosafety Level 2 as recommended for any potentially infectious human serum or blood specimen in the Centers for Disease Control/National Institutes of Health manual "Biosafety in Microbiological and Biomedical Laboratories", 3rd Edition, 1993. CHEMICAL HAZARD: As stated in Section IV, some of the reagents in this kit contain sodium azide as a preservative. For all such reagents, the concentration of sodium azide is ~0.09%. Sodium azide may react with lead and copper plumbing to form explosive metal azides. Dispose of all nonradioactive reagents by flushing with large amounts of water through the plumbing system. VI. SPECIMEN COLLECTION AND PREPARATION Serum or Plasma Serum or plasma may be used and the usual precautions for venipuncture should be observed. Serum or plasma may be stored at 2-8C for up to 24 hours and should be frozen at -20C or lower if stored for longer periods. Because of the diurnal variation in cortisol levels, the time of collection of the specimen should be noted. Do not use grossly hemolyzed or grossly lipemic specimens. Urine B. Extraction Procedure for Urine Specimens: 1. 8. 9. Add 250 L of thoroughly mixed urine to an appropriately marked 12 x 75 mm glass tube. Add 1 mL of methylene chloride. Vortex for 30 seconds. Centrifuge at 2000 rpm for 5 minutes OR allow to stand at room temperature (~25°C) for 30 minutes. Aspirate the upper aqueous layer. Transfer 100 L of methylene chloride extract (lower organic layer) in duplicate to appropriately labeled 12 x 75 mm plastic tubes. Evaporate the extract to dryness by using a gentle stream of air or nitrogen OR by allowing the tube to stand at room temperature. Add 25 L of Cortisol Diluent to each tube of dried urine extract. Proceed with step 3 of the assay procedure. VII. PROCEDURAL NOTES 2. 3. 4. 5. 6. 7. A thorough understanding of this package insert is necessary for successful use of the product. Reliable results will only be obtained by using precise laboratory techniques and accurately following the package insert. A standard curve must be included with each assay. 1. 2. 3. 4. 5. 6. 7. 8. 9. Failure to obtain the appropriate cortisol values for Controls may indicate imprecise manipulations, improper sample handling or deterioration of reagents. Failure to blot tubes adequately following decantation may result in poor replication and spurious values. 2001 2002 2003 2004 2005 2006 2007 2020 2030 2010 2051 2052 Materials Required But Not Supplied: 12 x 75 mm plastic test tubes. 12 x 75 mm glass tubes for urine extraction. Test tube rack for 12 x 75 mm tubes. Deionized water. Precision pipette to deliver 25 L. Precision repeating pipette to deliver 500 L. Vortex mixer. Centrifuge (1500 x g, preferably refrigerated). Sponge test tube rack or similar device for decantation. Waterbath capable of 37 ± 2C. Absorbent material for blotting tubes. Gamma counter. Semi-log graph paper or computer RIA data analysis program. Methylene chloride for urine extraction procedure. Label and arrange tubes in duplicate for Total Count tubes, Standards, Controls and unknowns. Add 25 L of the Standards, Controls or unknowns to the appropriate tubes. Pipet to the bottom of the tubes. Immediately add 500 L of the Cortisol [I-125] Reagent to each tube. Add 500 L of the Cortisol Antiserum Complex to all tubes except Total Count tubes. This reagent should be mixed thoroughly before use. Vortex all tubes. Incubate all tubes in a water bath at 37 ± 2C for 45 minutes. Centrifuge all tubes except Total Count tubes for 15-20 minutes at 1500 x g in a refrigerated centrifuge. Decant all tubes, except Total Count tubes by simultaneous inversion, holding an inversion with a sponge rack into a radioactive waste receptacle. Allow them to drain on absorbent material for 15 - 30 seconds and gently blot the tubes to remove any droplets adhering to the rim before returning them to the upright position. Failure to blot tubes adequately may result in poor replication and spurious results. Count all tubes in a gamma counter for one minute. IX. RESULTS The results in this package insert were calculated using log-linear curve fit. Other data reduction methods may give slightly different results. A. Calculate the mean counts per minute (CPM) for each Standard, Control and unknown. Calculate the % B/T, or %B/Bo for each Standard, Control and unknown as follows: % B/T = % B/Bo = B. C. D. E. F. Do not mix various lots of any kit component within an individual assay. Do not use any component beyond the expiration date shown on its label. After removing assay reagents from the refrigerator, allow them to reach room temperature (~25°C) before pipetting. Unused reagents should be stored as stated in the Reagent Section. Standards and Controls should be mixed before use by inverting or swirling gently rather than vortexing. To insure a homogeneous mixture of the reagents in each assay tube, gentle and thorough shaking or vortexing is essential. CATALOG NO. One Vial One Vial One Vial One Vial One Vial One Vial One Vial One Bottle One Vial One Bottle One Vial One Vial C. Assay Procedure: Allow all reagents to reach room temperature (~25°C) and mix thoroughly by gentle inversion before use. Standards, Controls, and unknowns should be assayed in duplicate. The total volume of urine excreted during a 24 hour period should be collected and mixed in a single container. Preservatives are not required; however, 10 grams of boric acid per liter of urine may be added. Specimens may be stored at room temperature after collection. Urine samples which are not to be assayed immediately should be stored at 2-8C. Urine should be stored at -20C or lower if stored longer than one week. Repeated freezing and thawing of samples should be avoided. QUANTITY Mean Sample Counts Mean Total Counts Mean Sample Counts Mean Counts of 0 g/dL X 100 X 100 Plot a curve of % B/T, or % B/Bo for the Cortisol Standards (y-axis) against the cortisol concentration (x-axis) on log-linear (semi-log) graph paper. Draw a standard curve through the mean of the duplicate points. Determine the cortisol concentration of the means of the duplicate counts of each Control and unknown sample from the standard curve. Any sample reading greater than the highest Standard should be diluted appropriately with the Cortisol Diluent and re-assayed. Any sample reading lower than the lowest Standard should be reported as such. To determine the cortisol concentration in urine, calculate as above and correct for total volume of urine collected in 24 hours: g/dL x 24 hour volume (mL) = g Cortisol/24 hour 100 X. LIMITATIONS This kit should not be used to measure cortisol levels in samples from patients treated with prednisolone or prednisone (prednisone is rapidly converted in vivo to prednisolone [15,16]) because of the high cross-reactivity of the antibody to prednisolone. Hemolyzed and lipemic specimens may give false values and must be avoided. Avoid freezing and thawing of reagents and specimens. XI. QUALITY CONTROL Maximum binding (% bound), or counts bound in the absence of unlabeled antigen is approximately 50% when freshly iodinated tracer is used, and may fall to 25% near the end of expiration date. Maximum binding less than 25% may indicate reagent deterioration, contamination, or poor technique. DSL Controls or other commercial controls should fall within established confidence limits. The confidence limits for DSL Controls are printed on the Control vial labels. TYPICAL CORTISOL STANDARD CURVE DATA TUBE NO. TUBE LABEL BOUND (cpm) MEAN (cpm) 1, 2 TOTAL COUNTS 79112 79819 79466 3, 4 STANDARDS A F 45939 45535 37942 39732 30927 30626 24626 24714 17889 17682 12456 12458 G 5, 6 B 7, 8 C 9, 10 D 11, 12 E 13, 14 15, 16 17, 18 19, 20 CONTROLS Level I Level II B/T (%) B/Bo (%) CORTISOL (g/dL) 45737 57.6 100.0 0 38837 48.9 84.9 0.5 30777 38.7 67.3 2.0 24670 31.0 53.9 4.0 17786 22.4 38.9 10.0 12457 15.7 27.2 20.0 8282 8590 8436 10.6 18.4 60.0 24311 26049 12090 12823 25180 31.7 55.1 3.77 12457 15.7 27.2 20.00 ED50 = 5.1 g/dL CAUTION: The above data must not be employed in lieu of data obtained by the user in the laboratory. XII. EXPECTED VALUES It is recommended that each laboratory establish its own range of normal cortisol values. Results of a normal range study, conducted with the DSL-2000 Cortisol RIA, are as follows: TIME N NORMAL RANGE (g/dL) A.M. P.M. 100 100 5-25 2-12 Because of diurnal variation [4] in normal subjects, serum or plasma cortisol levels are highest in the morning and lowest in the evening. Serum cortisol levels after ACTH stimulation tests normally increase 2-3 times over the basal value. Dexamethasone or Metyrapone suppression tests lower the basal serum cortisol value to 75-90% of normal [8-12]. Assay values for plasma samples (heparin or EDTA) may be approximately 5-10% lower than for serum. Urine normal range: 25-120 g/24 hours (non-extracted urine) XIII. PERFORMANCE CHARACTERISTICS All performance characteristics are stated in g/dL. To convert to nmol/L: g/dL x 27.6 = nmol/L A. Sensitivity: The theoretical sensitivity, defined as the lowest detectable level of cortisol that can be distinguished from the 0 g/dL Cortisol Standard, is 0.11 g/dL at the 95% confidence limit. B. Precision: The intra-assay precision was determined from the mean of 12 replicates each. SAMPLE I II III N 12 12 12 (g/dL) MEAN STANDARD DEVIATION (g/dL) COEFFICIENT OF VARIATION (%) 5.04 18.80 27.32 0.33 0.66 2.26 6.5 3.5 8.3 The inter-assay precision was determined from the mean of average duplicates for 12 separate runs. SAMPLE I II III N 12 12 12 (g/dL) MEAN STANDARD DEVIATION (g/dL) COEFFICIENT OF VARIATION (%) 5.06 18.46 29.68 0.40 1.26 2.76 7.9 6.8 9.3 C. Recovery: Three serum samples containing different levels of endogenous cortisol were spiked with different amounts of an elevated serum sample and assayed. SAMPLE ENDOGENOUS (g/dL) ADDED (g/dL) EXPECTED (g/dL) OBSERVED (g/dL) RECOVERY (%) I 2.27 II 7.94 III 13.11 1.73 3.65 7.49 1.73 3.65 7.49 1.73 3.65 7.49 4.00 5.92 9.76 9.67 11.59 15.43 14.84 16.75 20.60 3.97 6.57 8.95 8.46 11.80 14.26 14.22 14.99 17.94 99 111 92 87 102 92 96 89 87 D. Linearity of Dilution: Three serum samples were diluted with 0 g/dL Cortisol Standard and assayed. SAMPLE I II III DILUTION FACTOR EXPECTED (g/dL) OBSERVED (g/dL) RECOVERY (%) --1:2 1:4 1:8 1:16 --1:2 1:4 1:8 1:16 --9.90 4.95 2.47 1.23 --13.92 6.96 3.48 1.74 19.81 8.68 4.23 1.86 0.95 27.84 13.85 6.54 3.71 1.87 --88 85 75 77 --99 94 107 107 --1:2 1:4 1:8 1:16 --9.87 4.93 2.46 1.23 19.74 9.64 4.49 2.08 1.04 --98 91 85 85 E. Specificity: The cross-reactivity of the cortisol antiserum has been measured against various compounds. The percent cross-reactivity is expressed as the ratio of the cortisol concentration to the concentration of the reacting compound at 50% binding of the 0 g/dL Standard. In most cases, the interference from these compounds is insignificant when compared to the much higher levels of circulating cortisol. The cross-reactivity of the antibody with prednisolone precludes the use of this kit for patients on prednisolone or prednisone therapy (prednisone is rapidly converted in vivo to prednisolone) [16,17]. STEROID Cortisol Prednisolone Corticosterone 11-Deoxycortisol Cortisone Prednisone 17-Hydroxyprogesterone 11-Deoxycorticosterone Dexamethasone Testosterone Progesterone Epiandrosterone Dehydroepiandrosterone Estradiol XIV. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. % CROSS REACTIVITY 100 33.33 9.30 3.80 2.22 1.42 1.00 0.61 0.38 0.14 0.12 0.04 0.02 0.02 Drucker S, New MI: Disorders of adrenal steroidogenesis. Pediatr Clin North Am 34:1055-1066, 1987. Migeon CJ, Lanes RL: Adrenal cortex: hypo- and hyperfunction. IN Lifshitz F (ed): Pediatric Endocrinology, A Clinical Guide, second edition. Marcel Dekker, Inc., New York, 1990, pp. 333-352. Hyams JS, Carey DE: Corticosteroids and growth. J Pediatr 113:249-254, 1988. Kreiger DT: Rhythms of ACTH and corticosteroid secretion in health and disease and their experimental modification. J Steroid Biochem 6:785-791, 1975. Chernow B, Alexander R, Smallridge RC, Thompson WR, Cook D, Beardsley D, Fink MP, Lake R, Fletcher JR: Hormonal responses to graded surgical stress. Arch Intern Med 147:1273-1278, 1987. Crapo L: Cushing's syndrome: A review of diagnostic tests. Metabolism 28:955-977, 1979. Lee PDK, Winter RJ, Green OC: Virilizing adrenocortical tumors in childhood. Eight cases and a review of the literature. Pediatrics 76:437-444, 1985. Leisti S, Ahonen P, Perheentupa J: The diagnosis and staging of hypocortisolism in progressing autoimmune adrenalitis. Pediatr Res 17:861-867, 1983. Alsever RN, Gotlin RW: Handbook of Endocrine Tests in Adults and Children, second edition. Year Book Medical Publishers, Inc., Chicago, 1978. Stewart PM, Seckl JR, Corrie J, Edwards CRW, Padfield PL: A rational approach for assessing the hypothalamo-pituitary-adrenal axis. Lancet i:1208-1210, 1988. Watts NB, Tindall GT: Rapid assessment of corticotropin reserve after pituitary surgery. JAMA 259:708711, 1988. Lashansky G, Saenger P, Fishman K, Gautier T, Mayes D, Berg G, Di Martino-Nardi J, Reiter E: Normative data for adrenal steroidogenesis in a healthy pediatric population: age- and sex-related changes after adrenocorticotropin stimulation. J Clin Endocrinol Metab 73:674-686, 1991. Schlaghecke R, Kornely E, Santen RT, Ridderskamp P: The effect of long-term glucocorticoid on pituitary-adrenal responses to exogenous corticotropin-releasing hormone. New Engl J Med 326:226230, 1992. Yalow R and Berson S: Introduction and general considerations. IN: Odell WD, Daughday WH (eds): Principals of Competitive Protein Binnding Assays. J.B. Lippincott Co., Philadelphia, 1971, pp 1-19. Jenkins J, Sampson P: Conversion of cortisone to cortisol and prednisone to prednisolone. Br Med J 2:205, 1967. Colburn W, Buller R: Radioimmunoassay for prednisolone. Steroids 21:833, 1973. -124-(Synact-hen) on adrenocorticol function. J Endoc 34:411, 1966.