Full Steam Ahead: Implementation
advertisement

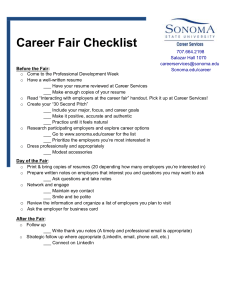
EVENT SUMMARY “Full Steam Ahead: Implementation Opportunities and Challenges for Employers and Consumers” September 8, 2010 The Alliance for Health Reform, with support from the Robert Wood Johnson Foundation, held a discussion about health reform implementation issues facing employers and consumers. The luncheon briefing took place on September 8 from 12:15 to 2 p.m. in Dirksen Senate Office Building, Room G50. Panelists were: Terry Gardiner, Small Business Majority; Steve Finan, American Cancer Society Cancer Action Network; Steve Wojcik, National Business Group on Health; and Janet Trautwein, National Association of Health Underwriters. Ed Howard of the Alliance and Brian Quinn of the Robert Wood Johnson Foundation co-moderated. Ed Howard, executive vice president at the Alliance for Health Reform, welcomed attendees and thanked the speakers for their participation. Mr. Howard also thanked the Robert Wood Johnson Foundation for sponsoring the briefing. After speaking briefly about the disparity between large and small employers offering health insurance to employees, Mr. Howard introduced Brian Quinn of the Robert Wood Johnson Foundation. Brian Quinn, senior program officer at the Robert Wood Johnson Foundation, talked about the role of the Affordable Care Act (ACA) and its effect on the way insurance will be bought and sold. He spoke about the different funding projects through RWJF and how the foundation works to shape health policy. He then thanked Ed Howard and the speakers for their participation. Steven Wojcik of the National Business Group on Health represented the large employer perspective on the legislation. He explained that most large employers tailor self-funded plans, which are then administered through an insurance company rather than offering an off-the-shelf plan available through the insurance company. These plans are subject to an annual renewal cycle; changes are considered in the spring and a final determination is made by late summer. However, the passage of health reform has forced companies off this timeline, and many large employers are struggling to make changes to their 2011 offerings in time. Most companies benchmark their plans with the plans of similar companies in order to maintain competitive employment packages. Additionally, many employers are concerned about possible changes in the cost and quality of the plans they will be able to offer. Indeed, 59 percent of employers believe that administrative costs will go up and cost trends will continue. Mr. Wojcik also talked about steps some companies may take to shift the expense associated with the new regulations. For example, many companies plan to implement a surcharge for all dependants to account for the new requirement that children up to 26 can be covered. Finally, Mr. Wojcik mentioned that there are some provisions of the ACA yet to be addressed, including tax penalties for employers who offer coverage for part-time employees. He hopes these issues will be addressed before 2014. Janet Trautwein of the National Association of Health Underwriters represented small business interests. She spoke of the need to educate small business owners about appropriate use of the legislation. For example, Ms. Trautwein said many small businesses do not know about the modest tax credit available to help them cover employees. Small educational steps like this will facilitate a smoother implementation of the ACA, she said. Cost is the primary concern for small employers and, without the flexibility to create their own plan, they are forced to take off-the-shelf plans offered by insurance companies, the premiums of which are expected to increase by 4-5 percent under this legislation. The new low-deductible caps mandated by the ACA will make some HSAs illegal. This means employers will be forced to spend more for traditional insurance coverage or drop coverage – or employees – altogether. Terry Gardiner of the Small Business Majority also spoke from a small business perspective. He said that state exchanges will promote the enrollment of many more small business employees and sole proprietors. Currently, 28 percent of small business employees do not have coverage. In his view, problems associated with implementation stem from lack of knowledge about options. Additionally, successful implementation will require less premium volatility in the individual market. Mr. Gardiner explained that state exchanges are promising since they allow small employers to offer multiple plans to their employees, creating better coverage and competitiveness. Some changes in the SHOP exchange model must be addressed, but Mr. Gardiner’s primary concern is with the dissemination of information about the ACA to small businesses. Stephen Finan of the American Cancer Society Cancer Action Network spoke about the ACA from the perspective of the consumer. He described the health insurance market as being historically opaque and unfriendly. Mr. Finan explained that most consumer insurance decisions are based on cost, not quality of coverage. He wants to see the construction of a consumer market with four goals: availability, affordability, adequacy and administrative simplicity. He is also looking forward to the elimination of health status as a qualifying factor for coverage, and the revocation of lifetime plan limits. Finally, Mr. Finan discussed institutional changes needed to make reform successful, including plan ratings, assistance for consumers navigating the exchanges, standardization of forms and a focus on prevention. Mr. Finan closed by encouraging consumers to take the time to learn about the bill and ask questions. An informative question and answer session followed.