Substance Misuse Prescribing Mini Manual
advertisement

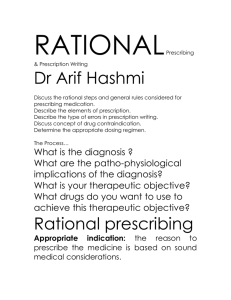
Prescribing in Substance Misuse Aide-memoire CONTENTS Page Principles of Good Prescribing Introduction Aims of Prescribing Care Coordination Care Plan Ongoing care and monitoring 2 3 3 4 5 5 Safety and Good Practice Appointments and Review Procedures Driving 6 6 6 Pharmacy liaison Wording a prescription correctly Supervised Consumption Policy Managing “on top” use Holiday Prescription Guidelines Recording cancelled prescriptions Discontinuation of a prescription 7 7 8 9 9 10 10 Methadone Prescribing Buprenorphine (Subutex & Suboxone) Prescribing Choosing between methadone and buprenorphine Benzodiazepine Prescribing Lofexidine Prescribing Naltrexone Prescribing Prescribing In Pregnancy and Breastfeeding 12 13 14 15 17 19 20 V. 1.2 June 2009 Page 1 Principles of Good Prescribing (Summary) Prescribing should take place within a framework. Address co-existing physical, emotional, social and legal problems at the same time. Prescribe with a firm harm reduction approach. Before prescribing, assess the patient fully, screen to confirm substance use and agree a care plan. Regularly monitor and review during treatment including screening. See patients usually on a three monthly basis. Inform patients about driving regulations and the need to contact the DVLA. Pharmacy liaison is very important as the pharmacist is usually the only health care professional who will have daily contact with the patient. Ensure prescriptions are written correctly to achieve continuity of treatment. Discontinuation of a prescription is a serious intervention and should ideally be a multi-disciplinary decision. Continued illicit drug/or alcohol use will lead to a review of the prescription. Decisions to work outside the prescribing policy should be a multi-disciplinary decision but must ultimately be supported by the prescriber. Document all decisions. On top use should not be ignored. It can be dealt with through psychological therapy, pharmacological therapy or a mixture of both. V. 1.2 June 2009 Page 2 Introduction Prescribing is a component of a treatment package rather than being a treatment on its own. Community prescribing may comprise: Stabilisation or maintenance on substitute opioids. Withdrawal from opioids with non-opioid medication e.g. lofexidine. Stabilisation and withdrawal from sedatives, benzodiazepines and alcohol. Relapse prevention prescribing with acamprosate or disulfiram. Symptomatic and maintenance prescribing for stimulant users. Cornwall Drug Services operate with a firm harm reduction approach in line with Department of Health and NTA guidelines. Aims of Prescribing Prescribe substitute medication to stabilise patient’s withdrawal symptoms. Reduce or eliminate the use of illicit/non-prescribed drugs. Reduce the dangers associated with drug misuse e.g. reducing injecting and sharing of injecting paraphernalia. Reduce criminal activity associated with drug misuse. Reduce the risk of prescribed drugs being diverted. Improve the patients’ overall functioning from a personal, social, family and community perspective. In the case of alcohol and benzodiazepines, achieve safe detoxification minimising adverse events. Engage and retain drug users in their treatment programme. V. 1.2 June 2009 Page 3 Care Co-ordination Care co-ordinator’s responsibilities: To co-ordinate the monitoring of the patient for signs of over-sedation during titration and treatment. This will be supplemented by the pharmacist, who will withhold doses in accordance with an agreed protocol if the patient presents to the pharmacy intoxicated To request the prescription via a letter or written request (handwritten is acceptable) with start date, pharmacy and details of the prescription. All such details must also be recorded in the case file. To ensure that appointments are booked with the prescriber and to keep the prescriber informed of patient’s presentation. Action Completed? 4-way information-sharing agreement in place? Patient registered with a GP? Dispensing pharmacy identified and contacted? Tier 3 comprehensive assessment performed? Patient’s general health status assessed? Objective proof of dependent substance misuse? Assessment undertaken and toxicological screening documented? Treatment programme agreed with care co-ordinator? Written care plan agreed and signed by patient? Patient clear on service policy on missed appointments etc? Patient’s literacy confirmed? Patient medication choice fully informed and side effects explained? Patient’s own GP informed of prescribing plan? Patient’s own GP informed of final dose after titration? Patient registered with National Drug Treatment Monitoring System? V. 1.2 June 2009 Page 4 The Care Plan The care plan forms the basis for treatment and sets out the expectations of both the service user and the service. It should include other appropriate agencies and carers. Agreed treatment goals are central to care planning. Treatment goals Engagement with service Harm reduction Health promotion Stabilisation of drug use Maintenance on medication Detoxification Abstinence Treatment outcome measures Attending appointments Modified injecting behaviour Reduced drug use Hepatitis B /C /HIV testing Hepatitis A&B vaccination Safer sex Increased knowledge of drug use/ harm reduction Aware of overdose prevention and management Engagement with GP re health problems Improved social relationships Improved housing Reduced debt Increased daily activity Reported cessation of problem drug use. Negative toxicology Cessation of substitute prescribing Cessation of drug use Drug free after 1,3,6 months Completing relapse prevention intervention Where supplementary prescribing by a non-medical prescriber is intended, a clinical management plan must be in place. This can be incorporated within the care plan to reduce duplication. Ongoing care and monitoring Provide the following information to the patient with the written care plan: Information on the drug prescribed, its effects and side effects Warnings about overdose and how to manage others who overdose. Information regarding help and advice regarding blood borne virus screening, safer injecting and sexual practices. Those who are Hepatitis B or C positive should be provided with information about alcohol usage. V. 1.2 June 2009 Page 5 Safety and Good Practice Monitor during treatment with regular random urine screening and/or oral fluid tests. This should be at least two screens per year but will be more for patients who are not stable or in early treatment. Appropriate dispensing arrangements should be in place. Send prescriptions to pharmacies and only give directly to patients in exceptional circumstances. Pharmacies may collect prescriptions. Advise the patient on safe storage of their prescription especially if children live at or visit the same premises. Review ineffective prescriptions with the multi-disciplinary team and, if necessary, stop them. Keep records of the prescription including date issued, dates to start, drugs prescribed, dosage and prescription numbers. Only the patient should collect the medication from the pharmacy. If a third party needs to collect the prescription the care co-ordinator or the prescriber must authorize this in writing (e.g. by fax to the pharmacy) Appointments and Review Procedures The patient will usually be seen by the prescriber three monthly. This may be less frequent for stable patients with the agreement of the multi-disciplinary team, while for patients with complex needs it will need to be more frequent. The care co-ordinator should see patients at least three monthly if a patient is completely stable on their prescription. After initiation of prescribing, the patient should be seen at least weekly for the first fortnight and after this typically every 2-4 weeks depending on the agreed care plan. If the patient misses two consecutive appointments (without good reason) it is a strong indicator for stopping the prescription, or putting it ‘on hold’. Consult the multi-disciplinary team before reaching a decision. Continued illicit drug use will lead to a review of the prescription and/or the psychological approach adopted. Driving - (See the CD-rom for patient and prescriber information) V. 1.2 June 2009 Page 6 Pharmacy liaison The prescriber or care co-ordinator should help the patient find a pharmacy as pharmacies are not obliged to supervise the consumption of controlled drugs and those that do may have reached capacity. Liaise regarding start dates and other relevant details Communicate in good time to allow the Pharmacist an adequate period to secure stocks. Prescription regulations The doctor who signs the prescription carries ultimate responsibility for prescribing. Prescriptions must be: Signed by the prescriber with his/her usual signature. Dated, but a computer generated date is acceptable. Post-dating of prescriptions may be necessary but a prescription for a controlled drug must be dispensed within 28 days of the date it is signed or the commencement date if the prescriber specifies one. The prescription for CD schedules 2 and 3 should also state: The form and where appropriate the strength of the preparation. The total quantity or the number of dose units, in words and figures. The dose. Instructions to cover when the pharmacy is closed e.g. Sundays and Bank Holidays. Missed Collections of Instalments Where instalments to be dispensed are for more than one day, prescribers are advised to include the phrase: ‘if a collection is missed the remainder of the instalment [i.e. the instalment less the amount prescribed for the day(s) missed] may be supplied’ This will allow the pharmacist to dispense the remaining day(s) doses to a patient who fails to collect on the designated day but attends the following day. Without this phrase the whole instalment would be forfeited. However should a patient fail to pick-up the instalments for more than 2 consecutive days then the prescription should be suspended and the care-coordinator contacted. Missed doses can lead to loss of tolerance and prescribers should be kept informed of missed doses. Patients who repeatedly miss doses should have their treatment reviewed. If on less than daily dosing the first step would be to revert to daily dispensing. V. 1.2 June 2009 Page 7 Supervised Consumption Policy (Summary) Supervised consumption should occur for a minimum of three months at the start of treatment unless there are exceptional circumstances. Restart supervised consumption if a patient resumes a prescription after a break, receives a significant increase in their dose or transfers to daily collection from less frequent pick-up arrangements. Certain patient groups should remain in supervised consumption during their treatment programme. Supervised consumption is only available for methadone mixture and buprenorphine tablets. In certain circumstances e.g. women near term or with infants younger than 3 months, those with verified employment or in full time education special arrangements may be made to allow take home doses before three months have elapsed. As this is outside policy discuss at a multi-disciplinary team meeting and note the decision to prescribe in the patient’s records. After three months review the need for supervision and the collection interval with the care co-ordinator. Before offering a patient take home doses, ensure: a) Patients must demonstrate consistent negative screens for illicit drugs (at least three consecutive negative screens - excluding cannabis), b) Regular attendance at pharmacy and appointments, c) Achievement of care plan goals. d) No criminal activity, e) No other users in household, f) No evidence of injecting and / or high-risk poly drug use through selfreporting, physical examination and/or testing. Exclusion criteria: Continue supervised consumption if: Patients demonstrate continued drug misuse outside their care plan. Patients have a significant unstable psychiatric illness. There is concern that the prescribed drug is being diverted or used inappropriately. There are child protection issues. V. 1.2 June 2009 Page 8 During the initial titration of a methadone or buprenorphine prescription it is vital that post contact arrangements are in place to assess the patient. This will allow the assessor to determine: Whether the dose is adequate using an appropriate withdrawal symptoms assessment tool. Whether the dose is too high. Managing “on top” use Try to ascertain whether use is indeed in addition to the prescription. Sometimes the prescription is traded for street drugs. Reconsider daily supervised consumption. Clarify the treatment aims and dosing strategy with the patient. Those who are clearly motivated to cease on top use or who report heroin use to manage withdrawal symptoms may benefit from higher dose regimes. Weigh potential benefit of higher doses against additional risk. Refer clients on 100mg methadone but still unstable, or using on top, to secondary care for review and probable subsequent treatment. Alcohol misuse contributes to overdose risk and enhances the respiratory depressant effects of heroin. In the face of alcohol misuse weigh risks versus benefits and only continue prescribing together with interventions targeted at alcohol. Benzodiazepine use is linked to poorer treatment outcomes and overdose risk. Benzodiazepines and allied hypnotics should be prescribed with caution including, when necessary, daily dispensing. Treatment will usually be short-term. Holiday Prescription Guidelines (Summary) The patient should give at least 7 days notice if a holiday prescription is required for UK travel and 14 days for international travel. A bulk prescription should not usually exceed two weeks’ supply because safe prescribing demands regular contact with patients. Large volume prescribing should be subject to a risk assessment. Establish safe storage in transit and at the destination. In UK, where possible continue current arrangements by using a suitable pharmacy at the holiday location. Contact the local DAAT (www.addaction.org.uk/?page_id=1691) to find a pharmacy. Export licences are required for some quantities of certain drugs. V. 1.2 June 2009 Page 9 Some countries prohibit importation of certain drugs. The patient should check with the appropriate consulate (contact details at http://www.drugs.gov.uk/publication-search/drug-licences/embassy-list) Give a letter of authority detailing the medication the patient is carrying. If a patient leaves the country for more than the period covered by their prescription, they need reassessment and drug screening on their return, prior to the initiation of a new prescription. Recording cancelled prescriptions When a prescription already issued to a pharmacy needs to be changed: The care co-ordinator phones the pharmacy with details of the prescription to be cancelled. It should be made clear whether the new prescription supplements an existing prescription, or replaces it (e.g. if a patient is receiving 8mg buprenorphine, and a new prescription is issued for 4mg, is that an increase to 12mg or a reduction to 4mg?) The cancellation of any prescription and any replacement is recorded in the client’s prescription record The care co-ordinator is responsible for informing the prescriber about any prescriptions that are suspended or cancelled. This includes when patients are admitted to hospital. Discontinuation of prescription When there is a disagreement between a patient and the team over prescribing issues, aim to negotiate a new treatment agreement whenever possible. If agreement cannot be reached, a unilateral decision to reduce or stop a prescription may result. Reasons for this might be: Compromised safety, either of the patient or others. This risk can usually be addressed by a return to supervised consumption. On top use of alcohol or illicit drugs at a level which, when combined with a regular prescription, puts them at risk of dangerous side effects. The discontinuation of substitute prescribing is a serious matter. The following steps should be undertaken: The care co-ordinator will discuss the team view with the patient. It may be appropriate to do this together with the prescriber. If the patient does not attend appointments, this may have to be done by phone or by letter. V. 1.2 June 2009 Page 10 If a patient does not attend two consecutive appointments, they are informed by letter that if they do not attend a third appointment they may be discharged from the service. All decisions to end prescribing should be communicated to the service user’s GP where they are not the prescriber and the dispensing pharmacy. V. 1.2 June 2009 Page 11 Methadone Prescribing Policy (Summary) Methadone maintenance is most effective at a daily dose of 60-120mg. Prescribe methadone as the standard 1mg/1ml dose. Sugar free formulations and tablets have a greater potential for injection, and are more expensive. Start substitute prescribing with methadone at 20-30mg a day depending on initial assessment and tolerance and titrate the dose in 10mg increments (not exceeding 30mg in a week) until withdrawal symptoms are controlled; start low and go slow. Steady state plasma levels are reached about 5 days following the last dose increase. Deaths have occurred following doses as low as 20mg. Prescribe supervised consumption for a minimum of 12 weeks. Methadone has a clinically significant interaction with benzodiazepines and alcohol. Reassess patients who continue to misuse these drugs. Discuss decisions to prescribe over 100mg daily in patients who are still unstable with a Consultant in case a move to secondary care is indicated. The higher the dose the more important it is that the patient is tightly interval dispensed. For example a patient on 100mg or more should never pick-up once a week, and equally patients should never, or very rarely, have more than 1000mg in their possession at any one time (e.g. for a holiday prescription). Methadone use may be a risk factor for developing torsades de pointes / QT prolongation. Monitoring (ECG) is recommended in doses above 100mg daily or where there are other risk factors for QT prolongation including: heart disease liver disease electrolyte imbalances pimozide erythromycin clarithromycin quinidine amiodarone chloroquine mefloquine clozapine lithium risperidone Methadone maintenance therapy has the most cumulated evidence as safe to use in pregnancy and breast-feeding. Injectable methadone should only be initiated by a Consultant. V. 1.2 June 2009 Page 12 Buprenorphine (Subutex & Suboxone) Prescribing Policy Buprenorphine is a “safer” alternative to methadone due to its partial agonist properties and appears to have an easier withdrawal phase. Buprenorphine will provide a blockade effect against other opioids at doses of 12mg or above. Unlike methadone, buprenorphine as Subutex is easily soluble, allowing it to be dissolved and injected. Suboxone cannot be so easily misused in this way because it contains naloxone. Suboxone and Subutex are the same price and assumed to be the same efficacy. Suboxone is therefore recommended for all new clients, and transfer of clients from Subutex to Suboxone should be considered, especially if there is evidence of misuse of the former. Wait at least 6-8 hours after the last heroin dose or 24-48 hours after the last dose of methadone before initiating buprenorphine. Do not transfer patients from methadone doses above 30mg to buprenorphine without specialist advice. Introduce buprenorphine by titration, commonly 4mg (day 1), 8mg (day 2) and 12mg (day 3 onwards) to reduce the risk of precipitating withdrawal and allow monitoring of withdrawal symptoms against dose. Sublingual dissolution can take several minutes, and if not fully supervised during this time, client can leave the pharmacy with a partially dissolved tablet under their tongue which can be diverted. Buprenorphine is not contra-indicated in pregnancy. Discuss pregnant patients with a specialist in the field of substance misuse. Contra-indicated in acute respiratory depression, children under 16, severe hepatic insufficiency, Acute alcoholism or delirium tremens and breast-feeding Caution in Respiratory Depression, Liver Disorders, Renal insufficiency, Pregnancy, patients transferring from methadone treatment at doses of greater than 30mg Draft v. 1.1 June 2009 Page 13 Choosing between methadone and buprenorphine Methadone is cheaper than buprenorphine. Where there is no patient preference or convincing clinical reason to favour buprenorphine, methadone should be first line treatment for opioid maintenance therapy. Buprenorphine is the clear drug of choice for patients under the age of 18, although it should be noted that the licence is for patients of 16 years plus. The Royal College of General Practice suggests that you should take into consideration: Patient’s preference. Previous treatment history. Whether a sedating (methadone) or less sedating opiate (buprenorphine) would be advantageous. Prefer methadone if there is a risk of psychological decompensation. Buprenorphine is more appropriate for detoxification as withdrawal appears to be easier than for methadone if used for < 4-6 months. Naltrexone can be started sooner if buprenorphine is used (3-7 days). Buprenorphine is less affected by interactions with anticonvulsants, rifampicin and ribavirin. Buprenorphine is safer in overdose. The blockade effects of buprenorphine may be better suited to patients who wish to cease using heroin completely. Buprenorphine should not be continued if patients continue to use illicit opiates on a regular basis (risk of precipitated withdrawal). Buprenorphine is contra-indicated in acute respiratory depression, children under 16, severe hepatic insufficiency, Acute alcoholism or delirium tremens and breast-feeding Buprenorphine should be used with caution in Respiratory Depression (particularly when used in combination with benzodiazepines), Liver Disorders, and Renal insufficiency. Patients in methadone treatment at doses of greater than 30mg: Transferring to buprenorphine is likely to be associated with precipitated withdrawal Pregnancy Draft v. 1.1 June 2009 Page 14 Benzodiazepine Prescribing Policy There is little or no evidence that long-term benzodiazepines prescribing reduces harm, and increasing evidence that prescribing more than 30mg diazepam may actually cause harm. Discuss with a Consultant in Substance Misuse or GPwSI before exceeding 30mg. Benzodiazepines are indicated for short-term use only. They are not licensed as substitutes for long-term dependency but benzodiazepine withdrawal states can be treated (though the BNF specifies alcohol withdrawal only). Assess the patient fully and confirm use with urine or saliva testing on at least two occasions before issuing a prescription. Adequate methadone reduces illicit benzodiazepine use. Consider increasing doses of methadone and buprenorphine rather than introducing benzodiazepines. Insomnia and anxiety in opiate users are most likely to be explained by their street-drug use, and can be used as a reason to promote motivation for change. Arrangements to prevent diversion should be in place – supervised consumption and interval dispensing should be the same frequency as any substitute medication being prescribed. Diazepam can be prescribed on blue MDA forms, but on a separate prescription to methadone or buprenorphine. Other benzodiazepines must be on green FP10 forms with a covering instalment dispensing form. Diazepam is the drug of choice. Its long half-life helps reduce withdrawal symptoms. In severe liver dysfunction, lorazepam may be safer, but seek expert advice. Withdrawal symptoms: The incidence of convulsions is about 1–2%. Clients on higher doses (>50mg/day) appear to be able to reduce quickly with little risk of fits. Clients presenting with a history of excessive intake (>100mg diazepam daily) can be started on 40% of their reported dose with no serious ill-effect. Some authorities maintain that there is no indication for prescribing more than 60mg diazepam daily, regardless of the client’s stated intake. Consider hospital admission. In any of these scenarios, do not prescribe without expert advice. Detoxification - (see CD-rom for examples of reducing regimes) Keep any opiate substitute unchanged while reducing benzodiazepines. Try to avoid increases in dose once reduction has commenced Agree any change to the original plan with the client. DoH guidelines require review of any benzodiazepine prescription at least every three months. Draft v. 1.1 June 2009 Page 15 Many clients have a very negative view of their ability to withdraw from benzodiazepines. This can legitimately be challenged, as up to 40% of clients can stop usage without undue difficulty. Risks of Benzodiazepine Usage Pregnancy & lactation – see special section Liver disease impairs the metabolism of most benzodiazepines, lorazepam or oxazepam appearing safest in these circumstances. Contra-indications to benzodiazepine use are: Conditions causing respiratory depression, including COPD and sleep apnoea Severe renal impairment Malnutrition and hypoproteinaemia (benzodiazepines bind to plasma proteins) Severe muscular impairment, e.g. myasthenia gravis or motor neurone disease Porphyria. Drug interactions – the list of interactions is extensive. Check BNF appendix 1. “Z drugs” (zopiclone, zolpidem and zaleplon) are equally potent and as liable to dependency and illicit use as benzodiazepines. They confer no proven advantage. Draft v. 1.1 June 2009 Page 16 Lofexidine Prescribing (Summary) Lofexidine is useful as a detoxification regime for adult patients using up to 50mg methadone or <1g of heroin a day, short drug histories and nonpolydrug users who want abstinence as a goal of treatment. Lofexidine can cause hypotension. Monitor blood pressure before and during treatment and discontinue lofexidine gradually over 2 – 4 days to avoid rebound hypertension. Supplementary “when required” doses may be given. Caution is advised in pregnancy and breast-feeding. Offer the patient “The Detox Handbook” or the “Britlofex (lofexidine) - Home detoxification programme. A users’ guide.” (Available from Britannia Pharm.) Patients who may be excluded from a lofexidine treatment programme: Patients with severe heart disease, recent myocardial infarction, cerebrovascular disease or chronic renal failure. Patients who use other CNS depressants excessively, chaotically, in binges or in other dangerous ways. Patients with blood pressure below 80/40 at baseline. If blood pressure is between 90/50 and 80/40 discuss with the consultants. Patients with marked bradycardia (less than 55 bpm). Patients with congenital long QTc or the simultaneous use of 2 drugs that prolong the QTc interval, unless ECG monitoring is being performed and the lowest effective dose of lofexidine is being used (maximum lofexidine dose is 0.4 mg four times a day). Patients on methadone doses above 80mg daily. If the patient is on doses of methadone greater than 50mg or using more than 1 gram of heroin a day then the case should be discussed with the Consultant. Patients who are pregnant or breast-feeding. Patients currently being prescribed tricyclic antidepressants or who have taken them within the last 2 weeks, or other drugs such as anti-hypertensives which are active at the alpha–2 adrenergic receptors. Patients suffering from an underlying psychosis or severe health problem or suicidality requiring admission to hospital. Patients under the age of 16 years. Draft v. 1.1 June 2009 Page 17 Dose Regimes Initially, one tablet (0.2mg) twice daily increased by increments of one to two tablets (0.2-0.4mg) a day up to a maximum of twelve tablets (2.4mg) a day in response to withdrawal symptoms. Duration of treatment of 7-10 days is recommended but longer treatment may be warranted. The daily dose should be given in 2-4 doses with one dose at bedtime to offset insomnia and peak dose should coincide with the expected onset of severe withdrawal symptoms. Draft v. 1.1 June 2009 Page 18 Naltrexone Prescribing (Summary) Potential candidates for naltrexone treatment include: o Patients who want to achieve abstinence as a treatment goal. o Patients who have been clean but recently relapsed. o Patients currently abstinent but afraid of relapse because of stress Naltrexone is a useful adjunct to treatment if patients are motivated. Treatment should be supervised and supported by psychosocial therapy to achieve best results. Liver function tests should be carried out both before and during treatment. Do not prescribe in patients with acute hepatitis or liver failure. Caution in patients with impaired hepatic or renal function, pregnancy and breastfeeding. The safe use of naltrexone in children has not been established. Patients must be opiate-free for at least 7-10 days before treatment. The patient should not manifest withdrawal signs or report withdrawal symptoms. Typical wash-out periods are: Heroin Methadone Buprenorphine (>2mg, >2weeks) Buprenorphine (<2mg, <2 weeks) Up to 7 days Up to 10 days. Up to 7 days. Up to 3 days. Warn patients to avoid opioid containing medication while on naltrexone and that an attempt to overcome the block can result in acute opioid intoxication. Initiation of Treatment Screen for opioid use with a naloxone challenge test. Verify self-reporting of abstinence from opioids with urine analysis. Where a naloxone challenge test cannot be performed the patient should give informed consent for naltrexone treatment confirming they have been opiate free for the required number of days. Initiate treatment at a dose of naltrexone 25mg. Observe the patient for 30-60 minutes for withdrawal symptoms. Lofexidine should also be available for withdrawal symptoms on the first day of naltrexone dosing. If no withdrawal signs occur continue on 50mg a day thereafter. Maintenance 50mg per day is appropriate for many patients. However, a flexible regimen (100mg Monday, 100mg Wednesday, 150mg Friday) is possible to improve compliance No standard duration of treatment can be recommended. Plan an initial period of three months but prolonged administration may be necessary. Prescribe on FP10 (green) prescription forms, not in instalments. Draft v. 1.1 June 2009 Page 19 Prescribing In Pregnancy and Breast-Feeding (Summary) The treatment of pregnant substance misusers should be co-ordinated by or have input from a specialist working in the field of substance misuse. Monitor more frequently (every 6 weeks; key worker review every 1-2 weeks). Pregnant women should be offered a course of hepatitis B vaccination if not immune. Screen for HIV, hepatitis B and C. All babies should be routinely immunised against hepatitis B regardless of the mother’s hepatitis B status. Prescribing In Pregnancy Drug Methadone Maintenance Treatment (MMT) Methadone Reduction Buprenorphine Benzodiazepines Alcohol Lofexidine Naltrexone Stimulants Draft v. 1.1 June 2009 Comments MMT has the most robust evidence base and results in improved maternal and foetal health. Maintain pregnant patients on methadone on the same dose. In the third trimester an increase may be needed due to increased blood volume in pregnancy, increased liver metabolism and increased glomerular filtration rate. This should be judged on withdrawal signs with small incremental increases if necessary. Split dosing may be required in the third trimester. Stability is more important than reduction but some women strongly prefer to detoxify. Avoid detoxification in the first trimester (due to risk of miscarriage) and in the second trimester reduce at a rate of no more than 2.5-5mg methadone weekly, fortnightly or monthly or 1mg/day. Detox with caution in the third trimester (risk of foetal stress and premature labour) only after informed consent has been obtained regarding the lack of clear guidance. The evidence is less robust than for methadone and therefore buprenorphine is not a first line treatment in pregnancy. It may be appropriate to continue buprenorphine in patients established on treatment but this necessitates informed consent from the client and a wish not to transfer to methadone. Its partial agonist action may interfere with opioid analgesia in labour. First-trimester exposure may be associated with an increased risk of oral clefts in newborns, although the magnitude of this risk is uncertain. Third-trimester use is associated with floppy baby syndrome. Benzodiazepines are best avoided in pregnancy and antenatal detoxification carried out using a controlled reduction schedule (see CD-rom). Discuss with a GPwSI or consultant working in the field of substance misuse. Patients with symptomatic withdrawal should be offered benzodiazepine withdrawal, ideally as an inpatient. Discuss with a GPwSI or consultant working in the field of substance misuse. Medication to sustain abstinence i.e. acamprosate and disulfiram should not be given in pregnancy or breast-feeding. Moderate drinking has not been shown to harm the foetus. Manufacturers recommend caution. Assess risk-benefit before prescribing. Manufacturers recommend caution. Animal studies do not suggest a teratogenic effect. Assess risk-benefit before prescribing. Recommend abstinence from stimulants during pregnancy. If streetuse continues, seek specialist advice. Page 20 Prescribing in Breastfeeding Drug Methadone and buprenorphine Benzodiazepines Alcohol Lofexidine Naltrexone Stimulants e.g. cocaine and amphetamines Draft v. 1.1 June 2009 Comments These enter breast milk but encourage breastfeeding because of the usual advantages it confers and the reduction in severity of any withdrawals the baby is experiencing. Only continue after discussion with a GPwSI or consultant working in the field of substance misuse. Any infant exposed to benzodiazepines in breast milk should be monitored for CNS depression and apnoea. Occasional light drinking has not been shown to harm the breastfeeding baby. Moderate to heavy drinking is inadvisable as it can interfere with the mother’s “let down” reflex and/or cause drowsiness in the infant resulting in the baby taking in less milk. No data available. Give to breastfeeding women only when the potential benefits outweigh the possible risks. Encourage mothers to stop stimulant use, but if use continues and the mother wishes to feed then encourage her since the more vulnerable babies have more to gain from it. Warn mothers about the dangers of continued use including possible delay in cognitive development, risk of seizure or stroke, cerebral palsy, mental retardation, vision and hearing impairment, urinary tract abnormalities and autism. Page 21