SEA cases - learning points
advertisement
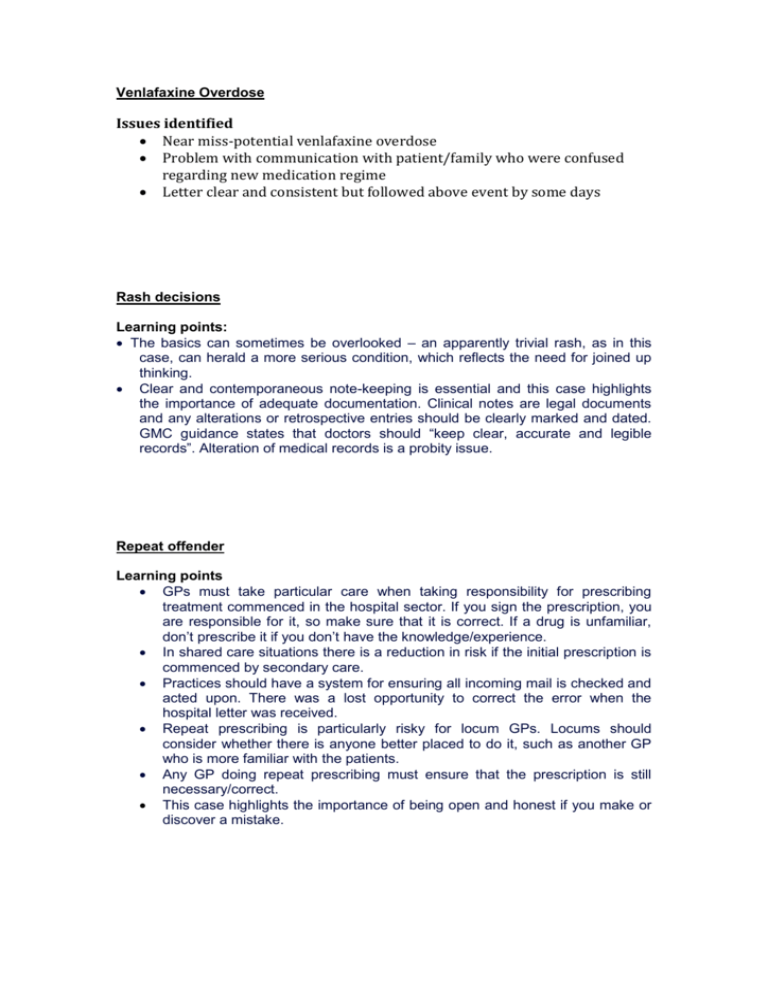
Venlafaxine Overdose Issues identified Near miss-potential venlafaxine overdose Problem with communication with patient/family who were confused regarding new medication regime Letter clear and consistent but followed above event by some days Rash decisions Learning points: The basics can sometimes be overlooked – an apparently trivial rash, as in this case, can herald a more serious condition, which reflects the need for joined up thinking. Clear and contemporaneous note-keeping is essential and this case highlights the importance of adequate documentation. Clinical notes are legal documents and any alterations or retrospective entries should be clearly marked and dated. GMC guidance states that doctors should “keep clear, accurate and legible records”. Alteration of medical records is a probity issue. Repeat offender Learning points GPs must take particular care when taking responsibility for prescribing treatment commenced in the hospital sector. If you sign the prescription, you are responsible for it, so make sure that it is correct. If a drug is unfamiliar, don’t prescribe it if you don’t have the knowledge/experience. In shared care situations there is a reduction in risk if the initial prescription is commenced by secondary care. Practices should have a system for ensuring all incoming mail is checked and acted upon. There was a lost opportunity to correct the error when the hospital letter was received. Repeat prescribing is particularly risky for locum GPs. Locums should consider whether there is anyone better placed to do it, such as another GP who is more familiar with the patients. Any GP doing repeat prescribing must ensure that the prescription is still necessary/correct. This case highlights the importance of being open and honest if you make or discover a mistake.