Student Learning Guide for Obstructive Pulmonary Diseases
advertisement

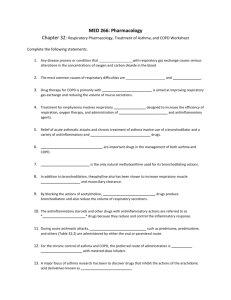
Student Learning Guide for Obstructive Pulmonary Diseases 1. Identify the triggers of asthma. 2. Describe the pathophysiology of asthma. 3. What are the manifestations of asthma? 4. Is the amount of wheezing an indicator of the severity of the attack? 5. What is status asthmaticus and what are the manifestations that differ from those of an asthma attack? 6. Explain why each of the following laboratory test would be abnormal for a client with asthma. 1 7. Complete the following table: Category/Names Anti-inflammatory Systemic o Solu-cortif o SoluMedrol o Prednisone Inhaled o Beclovent o Azmacort o Flovent o Pulmacort Action Suppresses inflammation Mast Cell Stabilizers Cromolyn (Intal) Tilade Anticholinergics Short acting: Atrovent Long acting: Spiriva Inhibit IgE mediated release of inflammatory mediators from mast cells and suppress eosinophils Blocks the bronchoconstricting influence of the parasymphathetic nervous system. Combivent is a combo of anticholinergic and β2 Leukotriene Modifiers: tablets Blockers o Accolate o Singular Inhibitor o Zyflo β2 Adrenergic Agonists Short Acting: Alupent Proventil Blocks the synthesis or action of leukotrienes from mast cells and eosinophils. Leukotrienes are potent bronchoconstrictors Prevent release of inflammatory mediators from mast cells Side Effects Systemic Nursing Considerations Systemic Inhaled Inhaled: 2 Ventolin Maxair Brethine Long Acting: Serevent Foradil Immediate Acting Adrenalin Methylxanthines: theophylline Unknown, but causes bronchodilation 8. Describe the correct way to use metered dose and dry powder inhalers. 9. Why is it necessary for the client with asthma to use both the β2 Adrenergic Agonists inhaler and the long-term therapy of inhaled corticosteriods or cromolyn? 10. Why are the OTC products that contain epinephrine and ephedrine dangerous? 11. List the teaching points for an asthmatic client to prevent asthma attacks. 12. Describe the red flags for a client during an acute asthma attack. 3 13. Describe the care of a client during an asthma attack. 14. Why is a peak flow meter used for clients with asthma and what do the zones mean? 15. What is COPD and what two diseases comprise COPD? 16. Identify the etiological causes of COPD. 17. Describe the pathophysiology of COPD. 4 18. What are the manifestations of COPD? 19. What is cor pulmonale and why does it occur in clients with COPD? 20. What is the treatment of clients with COPD exacerbations? 21. Why do clients with COPD have an increased incidence of peptic ulcer and GERD? 22. Why are COPD clients prone to depression and anxiety? 23. Why is smoking cessation important and what is the relationship between smoking cessation and COPD? 24. Match the nursing diagnosis to the manifestation which would support that nursing diagnosis. 5 A = Impaired gas exchange B = Ineffective breathing pattern C = Ineffective airway clearance _____ Adventitious lung sounds _____ SpO2 _____ shallow respirations _____ copious sputum _____ wheezing _____ cyanosis _____ hypoxemia _____ restlessness _____ tachypnea _____ respiratory acidosis _____ hypoventilation _____ retraction _____ low peak air flow _____ hyperventilation _____ decreased vital capacity _____ inspiratory-expiratory ratio of 1:3 _____ orthopnea 25. For each of the above manifestations establish an outcome criteria addressing that specific manifestation, under the correct nursing diagnoses. Impaired gas exchange: 6 Ineffective breathing pattern Ineffective airway clearance 26. Oxygen should be administered to the client to keep the PaO2 between ________ mm Hg. Consequently, many clients with end stage COPD require high ________ and high _____ concentrations for survival. 27. The major benefit of long term oxygen therapy for the client with COPD is __________ rates and the improved prognosis comes from _______________________ of the disease. 28. What is pursed lip breathing and why is it used for clients with COPD? 29. What is huff coughing and why is it used for clients with COPD? 30. What should the client with COPD be taught about nutrition? 31. Why should clients with COPD attend pulmonary rehabilitation? 32. Why is exercise training important for clients with COPD? 7