Pharmacology 15 – Anti – Emetics
advertisement

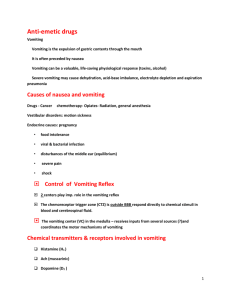
Pharmacology 15 – Anti-Emetics Anil Chopra 1. To describe, in broad terms, the control of vomiting 2. To state the receptor specificity, the main sites of action and the specific antiemetic uses of promethazine, metoclopramide, hyoscine and ondansetreon (see Fig.). 3. To list the main pharmacokinetic features and unwanted actions of specific drugs. Anti emetics are used only when the cause of nausea/vomiting is known. Stimuli include: - Peripheral organs o Pharynx o Stomach o Duodenum o Heart o Bladder o Uterus o Viscera o Testicles - Endogenous Toxins o Infections o Cancer o Chemotherapeutic agents o Radiation damage o Morphine o Cardiac glycosides, o Estrogen (early pregnancy) o Recovery from general anaesthesia - Motion sickness - Emotional - There are 4 main stimuli for the vomiting pathway: Peripheral Organs – e.g. pharynx, stomach, duodenum, heart, testicles, bladder, uterus etc Endogenous Toxins – e.g. drugs, infections, cancer, radiation damage, morphine, chemotherapeutic agents, cardiac glycosides, estrogen (early pregnancy) and recovery from general anaesthesia Motion Sickness Pain etc - repulsive sights and smells, and emotional factors All of these inputs feed to the vomiting centre (lower medulla, reticular formation, dorsal Vagal nucleus) which gives a co-ordinated response to nerves supplying somatic and visceral receptors (e.g. respiratory and abdominal muscles) to allow for vomiting - Receptors and neurotransmitters involved: o AChM = Muscarinic ACh receptor o H1 = Histamine receptors o 5-HT3 = Serotonin receptors o D2 = Dopamine Receptor Inducing Vomiting Stimuli from peripheral organs VISCERAL AFFERENTS Endogenous toxins, drugs Release of emetogenic agents 5-HT3 R Blood AchM, H1 R STIMULI Labyrinth Vestibular nuclei AchM, H1 R CSF? Nucleus of the solitary tract Pain, repulsive sights & smells, emotional factors. Motion sickness CHEMORECEPTOR TRIGGER ZONE Floor V, IV, medulla, area postrema INPUT to CNS SENSORY AFFERENTS & CNS PATHWAYS HIGHER CENTRES D2, 5-HT3, R AchM, H1 R VOMITING CENTRE Lower medulla, reticular formation, dorsal vagal nucleus INTE GRATION AchM, H1 R NERVES TO SOMATIC AND VISCERAL RECEPTORS Co-ordination of somatic respiratory & abdominal muscles & g.i.t. smooth muscle OUTPUT Name: Promethazine Uses - Motion sickness Disorders of labyrinth e.g. Meniere’s disease Hyperemesis gravidarium (morning sickness in pregnancy) Pre and post operatively (sedative and anti muscarinic actions useful) Relief of allergic symptoms Anaphylactiv emergency Night Sedation (in insomnia) Mode of Action It acts as a competitive antagonist at histaminergic (H1) cholinergic (muscarinic, M) and dopaminergic (D2). Potency H1 > M > D2 receptors. It also acts on the labyrinth, NTS (nucleus of the solitary tract), vomit centre to block its activation. Side-Effects Dizziness Tinnitus Fatigue Sedation (‘do not drive or operate machinery') Excitation in excess Convulsions (children more susceptible) Antimuscarininc side-effects Pharmacokinetics Administer orally Onset of action 1-2 hours Maximum effect circa 4 hours Duration of action 24 hours Name Metoclopramide Uses Used to treat nausea and vomiting associated with: uraemia (severe renal failure) radiation sickness gastrointestinal disorders cancer chemotherapy (high doses) eg. cisplatin (intractable vomiting) Mode of Action It is also a dopamine receptor antagonists. Order of antagonistic potency: D2 > H1 > Muscarinic receptors. It acts centrally at the chemoreceptor trigger zone and on the gastrointestinal tract by increasing smooth muscle motility (from oesophagus to small intestine), accelerating gastric emptying and accelerating transit of intestinal contents (from duodenum to ileo-coecal valve). Side Effects As it increases GI motility, it can cause reduce nutrient supply and effectiveness of certain drugs such as digoxin. In CNS drowsiness dizziness anxiety extrapyramidal reactions; children more susceptible than adults (Parkinsonian-like syndrome: rigidity, tremor, motor restlessness) NOTE: No anti-psychotic actions In the endocrine system hyperprolactinaemia galactorrhoea disorders of menstruation Pharmacokinetics may be administered orally; rapidly absorbed; extensive first pass metabolism may also be given i.v. crosses Blood brain barrier crosses placenta Name Hyoscine Uses Prevention of motion sickness Has little effects once nausea/emesis is established In operative pre-medication NOTE: Atropine is less effective Also has sedative properties unlike atropine which is exctiatory Mode of Action It is an anti-muscarinic drug but also acts in the vestibular nuclei, nucleus of the solitary tract, and vomiting centre to block activation. Side Effects Typical anti-muscarinic side-effects: drowsiness dry mouth, cycloplegia mydriasis constipation (not usually at anti-emetic doses) Other Can be administered orally (peak effect in 1-2 hours), i.v., transdermally Name Ondansetron Uses main use in preventing anticancer drug-induced vomiting, especially cisplatin radiotherapy-induced sickness post-operative nausea and vomiting Mode of Action Acts to block transmission in visceral afferents and chemoreceptor trigger zone. Side Effects headache sensation of flushing and warmth increased large bowel transit time (constipation) Other Administer orally; well absorbed, excreted in urine.