RNSG 1341
advertisement

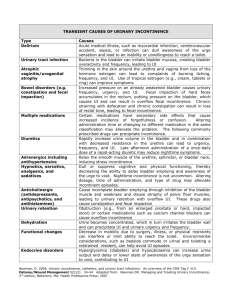
RNSG 1341 Urinary Incontinence Learning Guide Lewis, pp. 1180-1184 1. Describe the incidence of urinary incontinence in the United States. a. Among young adult to middle aged women, prevalence is 30-40% and increases to 30-50% in elderly. Women more frequently experience stress and urge incontinence than men. In young adult men the incidence is 1-5% progressing to 9-34% in elderly men. Urinary incontinence is a common manifestation of benign and malignant prostate enlargement in men. Urinary incontinence in men most often is overflow incontinence due to urinary retention. 2. What are the risk factors for UI? a. Risk factors associated with UI include: immobility, impaired cognition, medications, constipation/fecal impaction, low fluid intake, environmental barriers, diabetes mellitus, and stroke. 3. What are complications of UI? a. Left untreated, incontinence can cause physical and emotional upheaval. Individuals with long-term incontinence suffer from falls, urinary tract infections, and skin irritation leading to pressure ulcers. Incontinence can also affect their self-esteem and cause depression and social isolation. They frequently stop participating in physical activities they once enjoyed because of the risk of embarrassing "accidents." However, with the wide variety of treatment options for incontinence available today, the prognosis for incontinent patients is promising. If incontinence cannot be stopped, it can be improved in the majority of cases. 4. Define stress incontinence. a. Stress incontinence is defined as an involuntary loss of urine associated with activities that increase intra-abdominal pressure. Stress incontinence occurs when pelvic muscles have been damaged, causing the bladder to leak during exercise, coughing , sneezing, laughing, or any body movement which puts pressure on the bladder. Stress UI is more common in women (ex: after multiple childbirth or menopause), but also can be found in older men (ex: post prostatectomy or post urethra/surgery or radiation). Pelvic fracture, radical prostatectomy, or bladder neck surgery can also damage the sphincter muscle and cause stress incontinence. Stress incontinence can be diagnosed with a simple clinical stress test. With a full bladder (at least 200 mls) the resident is asked to stand, relax, and cough vigorously. An instantaneous leak is a positive result. For the mentally intact resident, stress incontinence can often be managed with Kegel exercises. Biofeedback may prove to be a valuable aid in teaching these exercises. For residents who don't respond to the exercises, surgical correction should be considered. 5. Define urge incontinence. a. Urge UI, or overactive bladder, is characterized by an involuntary urine loss associated with a strong desire to void (urgency) and minimal warning. UI is the urgent need to pass urine and the inability to get to a toilet in time. It occurs when nerve passages along the pathway from the bladder to the brain are damaged; causing a sudden bladder contraction of the detrusor muscle that cannot be consciously inhibited. The bladder contracts reflexively, overriding central inhibition. In addition to urgency, signs and symptoms of urge UI most often include urinary frequency, nocturia and enuresis, and UI of moderate to large amounts. Bladder changes associated with aging make older adults particularly prone to this type of UI. Stroke, dementia, Alzheimer's Disease, and Multiple Sclerosis (MS) can all cause urge incontinence. 6. Define overflow incontinence. a. Overflow UI is an involuntary loss of urine associated with over distention of the bladder, and may be caused by an under active detrusor muscle or outlet obstruction leading to over distention and overflow. The quantity of urine produced exceeds the bladder's holding capacity. They do not empty their bladder completely. Individuals with overflow UI often describe dribbling, urinary retention or hesitancy, urine loss without a recognizable urge, or an uncomfortable sensation of fullness or pressure in the lower abdomen. A common condition associated with this type of UI is BPH. It can also result from diabetes, pelvic trauma, extensive pelvic surgery, injuries to the spinal cord, shingles, MS, or polio. Overflow incontinence, especially in men with a urethral blockage, should be referred to an urologist to rule out an enlarged prostate. 7. Define reflex incontinence. a. Individuals with reflex incontinence lose control of their bladder without warning equally during the day and night. They typically suffer from neurological impairment or spinal cord lesions above S2. 8. Define functional incontinence. a. Functional UI is caused by non-genitourinary factors, such as cognitive or physical impairments that result in an inability for the individual to be independent in voiding. It is caused by problems of mobility. For example, acutely ill hospitalized individuals may be challenged by a combination of an acute illness and environmental changes. This, in turn, makes the voiding process too complex resulting in a functional type of UI. . Mobility aids can help remove barriers to self-toileting on a timely basis. Other factors such as arthritis may interfere with managing zippers, buttons, and articles of clothing -- or moving quickly enough to reach the toilet. Some medications such as diuretics, sedative/hypnotics, anticholinergics, alpha blockers, stimulants, and antipsychotics can cause incontinence. 9. List the components of a bladder log or voiding diary. a. Onset of UI, factors that provoke urinary leakage, and associated conditions. Timing of urinations, episodes of urinary leakage and frequency of nocturia. 10. How long is it necessary to keep a bladder log? a. 1-7days 11. List behavioral therapies used to improve urinary incontinence. This is well suited for older women in whom the risks of surgical complications and/or medication side effects may be substantial. a. Lifestyle modifications i. Probably the most important is weight loss if you are overweight. The extra weight a woman may be carrying around puts extra pressure on the bladder at baseline and makes it easier for urine to leak out. Even women who need to lose over 50 -100 pounds may find improvement of incontinence after losing only 10-20 pounds. ii. Decreasing the amount of fluid intake. iii. Decreasing smoking, caffeine, and alcohol intake may be helpful. b. Scheduling Voiding Regimens i. keep a seven-day urinary diary ii. the scheduled toileting with progressive voiding intervals should show results in about 4 weeks. c. Pelvic floor muscle rehabilitation i. Kegel exercises ii. weight training Vaginal Cones and Weights- weighted cones placed into the vagina and you have to use your muscles to hold them in. The main issue with this type of treatment is there has to be a great deal of motivation, and you have to keep up with the exercises long term. biofeedback technique used to help identify the correct muscle groups. iii. d. anti-incontinence devices i. intravaginal pessaries ii. intraurethral occlusive device (plug) iii. penile compression device e. containment devices i. external (penile sheaths) ii. absorbent products (pads and pants) 12. How would you teach a client Kegel exercises? a. This is a common recommendation and is also commonly done incorrectly. You can have the client stop the stream of urine several times during urination and they will get an idea of the muscles involved. 13. Which types of incontinence would this exercise most likely treat? a. Stress, urge, or mixed UI. 14. Describe drug therapy for urinary incontinence. a. Drug therapy is the most common approach for treating urge incontinence. b. The “gold standard” for treatment of urge incontinence has long been oxybutynin, originally trademarked as Ditropan but now available in generic form. It is a short-acting spasmolytic and anticholinergic that works by exerting a direct effect on the contractility of bladder smooth muscle and by blocking acetylcholine at muscarinic parasympathetic receptor sites in the bladder. Unfortunately, its clinical utility is often limited by side effects arising from its influence on other muscarinic receptors: i. dry mouth, due to its effects on the salivary glands ii. increased heart rate, due to its effect on the vagus nerve iii. constipation from slowed peristalsis of the gastrointestinal tract iv. blurred vision from its interference at high doses with the ciliary muscles of the lens of the eye v. occasional drowsiness or confusion, especially in elderly patients, from effects on the central nervous system1,2 The intensity of these side effects is directly related to peak serum levels, due to the short half-life of oxybutynin. Extended-release formulations of oxybutynin were developed to reduce the incidence of these effects, and other anticholinergics, such as tolterodine (Detrol LA), followed suit with long-acting formulations of their own. c. The first major competitor to oxybutynin was tolterodine (Detrol), an anticholinergic agent with a longer half-life and better selectivity for muscarinic receptors in the bladder. Long-acting tolterodine appears to be better tolerated than equivalent doses of oxybutynin, but Ditropan usually controls symptoms more effectively. d. Newer drugs i. solifenacin (Vesicare) muscarinic receptor antagonist with improved bladder selectivity- entered the US market in 2005. Patients have complaints of dry mouth, constipation, and blurred vision ii. darifenacin hydrobromide (Enablex) Like solifenacin, this new drug is a selective M3 muscarinic receptor antagonist iii. trospium chloride (Sanctura) This anticholinergic has been marketed in Europe for several years and was recently introduced in the United States. e. We also have evidence that an antidepressant can improve stress incontinence: duloxetine (Cymbalta) selective serotonin and norepinephrine reuptake inhibitor that is FDA-approved for major depressive disorder in adults, and for diabetic peripheral neuropathic pain. Besides inhibiting serotonin and norepinephrine reuptake in the brain, duloxetine inhibits reuptake in the sacral spinal cord, where the drug exerts an interesting effect on Onuf’s nucleus, which regulates tone of the urethral striated muscle sphincter through the pudendal nerve.16 The accumulation of serotonin and norepinephrine at Onuf’s nucleus (by reuptake blockade) increases efferent activity to the urethra, improving urethral tone. 15. Describe surgical therapy for urinary incontinence. Surgery is not usually done for urge incontinence. It is used to correct stress incontinence. a. Retropubic Suspension- The Marshall-Marchetti-Krantz (MMK) and Burch colposuspension procedures are the most common types of retropubic suspension. This treatment is used when the bladder or urethra has dropped out of place. With this procedure, the bladder neck can be raised back to the correct position. A few stitches are placed in the wall of the vagina and the pelvic fascia. They keep the bladder in place. Doing this also helps support the urethra. These surgeries require hospitalization. Retropubic colposuspension complications include post op voiding dysfunction, urgency and vaginal prolapse. a. Suburethral Sling- A sling, or hammock, may be used when the urethra has dropped out of place or when the sphincter muscle of the urethra is weak. The sling is placed under the urethra. Some slings are held in place by stitches. Others stay in place by friction between the sling and surrounding tissues. The sling is a narrow strap. This is an outpatient, minimally invasive form of sling surgery with a high success rate. Pubovaginal sling placement complications include vascular and bowel injury, urinary retention, mesh/sling erosion, and infection, urgency and bladder perforation. b. Bulking Injections- Bulking injections may be used when the sphincter muscle of the urethra is very weak and extensive surgery is not an option or has not worked. A substance is injected into the tissues around the urethra to add bulk. The urethra becomes narrower and better able to hold urine. Local anesthesia is used for this procedure. The treatment may be done in a doctor's office. More than one injection may be needed. The effect of this type of surgery may last from a few months to a few years. The procedure (injection) may be repeated. c. For men, overflow incontinence caused by enlargement of the prostate (benign prostatic hyperplasia, or BPH) is the form of incontinence most often treated with surgery. 16. Why is it important to use products designed for urinary incontinence? a. Those products are wick away moisture from the skin, prevent soiling of clothing and reduce odor. 17. What are some nursing interventions for the incontinent hospitalized patient? a. Offer urinal or bedpan or assist to the bathroom q 2-3 hours or at scheduled times. Ensures that patient toilets are accessible to patients and there is adequate privacy. b. Avoid medications that may contribute to UI. c. Monitor fluid intake and maintain an appropriate hydration schedule. d. Provide patients with usual undergarments in expectation of continence, if possible. e. Prevent skin breakdown by providing immediate cleansing after an incontinent episode and utilizing barrier ointments. f. Use absorbent products judiciously. g. Consider use of external collection devices for men Sample questions: 1. A 78-year-old patient is admitted to the hospital with dehydration and electrolyte imbalance. The patient is confused and incontinent of urine on admission. In developing a plan of care for the patient, an appropriate nursing intervention for the patient’s incontinence is to a. insert an indwelling catheter. b. apply absorbent incontinent pads. c. assist the patient to the bathroom q2hr. d. restrict fluids after the evening meal. Correct Answer: C Rationale: In older or confused patients, incontinence may be avoided by using scheduled toileting times. Indwelling catheters increase the risk for UTI. Incontinent pads increase the risk for skin breakdown. Restricting fluids is not appropriate in a patient with dehydration. Cognitive Level: Application Nursing Process: Planning Text Reference: pp. 1183-1185 NCLEX: Physiological Integrity 2. After her bath, a 62-year-old patient asks the nurse for a perineal pad, saying that she uses them because sometimes she leaks urine when she laughs or coughs. Which intervention is most appropriate to include in the care plan for the patient? a. Teach the patient how to perform Kegel exercises. b. Demonstrate how to perform Credé’s maneuver. c. Place commode at the patient’s bedside. d. Assist the patient to the bathroom q3hr. Correct Answer: A Rationale: Exercises to strengthen the pelvic floor muscles will help reduce stress incontinence. The Credé maneuver is used to help empty the bladder for patients with overflow incontinence. Placing the commode close to the bedside and assisting the patient to the bathroom are helpful for functional incontinence. Cognitive Level: Application Text Reference: pp. 1181-1184 Nursing Process: Planning NCLEX: Health Promotion and Maintenance 3. Following rectal surgery, a patient voids about 50 ml of urine every 30 to 60 minutes. Which nursing action is most appropriate? a. Use an ultrasound scanner to check for residual urine after voiding. b. Have the patient take small amounts of fluid frequently throughout the day. c. Reassure the patient that this is normal after rectal surgery due to anesthesia. d. Monitor the patient’s intake and output over the next few hours. Correct Answer: A Rationale: An ultrasound scanner can be used to check for residual urine after the patient voids. Because the patient’s history and clinical manifestations are consistent with overflow incontinence, it is not appropriate to have the patient drink small amounts. Although overflow incontinence is not unusual after surgery, the nurse should intervene to correct the physiologic problem, not just reassure the patient. The patient may develop reflux into the renal pelvis as well as discomfort from a full bladder if the nurse waits to address the problem for several hours. Cognitive Level: Application Text Reference: p. 1182 Nursing Process: Implementation NCLEX: Physiological Integrity 4. A patient in the hospital has a history of urinary incontinence. Which nursing action will be included in the plan of care? a. Place a bedside commode near the patient’s bed. b. Use an ultrasound scanner to check urine residual after the patient voids. c. Demonstrate the use of the Credé maneuver to the patient. d. Teach the use of Kegel exercises to strengthen the pelvic floor. Correct Answer: A Rationale: Environmental changes can make it easier for the patient to avoid incontinence for patients with urinary incontinence. Checking for residual urine and performing the Credé maneuver are interventions for overflow incontinence. Kegel exercises are useful for stress incontinence. Cognitive Level: Application Nursing Process: Planning Text Reference: p. 1181 NCLEX: Physiological Integrity 5. Which nursing assessment is most important before beginning bladder retraining with an incontinent client? a. recording the times at which the client is incontinent b. checking the specific gravity of the urine c. monitoring the extent of bladder distention d. observing the color of the client’s urine 6. Which instruction by the nurse is correct when teaching a client to perform Kegel exercises? a. contract and relax the muscles in the vagina b. stand and rock the pelvis back and forth c. push down with the feet and elevate the hips d. pull the abdominal muscles inward, then relax 7. Which response by the nurse is best during bladder retraining? a. encourage the client to restrict his fluid intake b. encourage the client to continue caffeine and alcohol intake c. discourage the client from restricting his fluid d. encourage the use of laxatives