TOXICOLOGY
advertisement

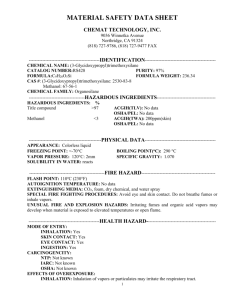
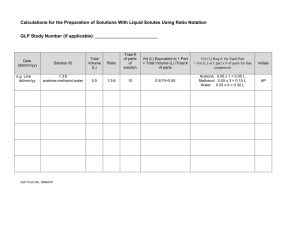
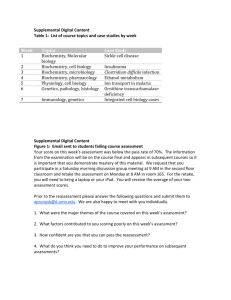
Alcohol withdrawal Hydroflouric acid burns Methanol poisoning Poisoned patients ALCOHOL WITHDRAWAL Alcohol withdrawal is a complex syndrome, which usually presents with more than one of: tremor, seizures, hallucinations, perspiration, hyperthermia, anxiety or agitation. Though there is a large spectrum of individual susceptibility it usually peaks at 48 hours post withdrawal. ASSESSMENT ABCs Assess symptoms and signs of withdrawal as per “Alcohol Withdrawal Rating Scale” at least 4 hourly Assess hydration. Nutritional Status INVESTIGATIONS Electrolytes and Creatinine Glucose LFTs FBC MANAGEMENT Keep in a quiet area Detoxification with diazepam as per “Guidelines for the Management of Alcohol Withdrawal in Hospital” IV fluids if dehydrated but avoid overhydration Thiamine 100mg IV (Decreases risk of Wernicke’s but does not alter seizures or delirium) In the elderly or those with severe liver dysfunction consider using oxazepam rather than diazepam, which has no active metabolites and therefore less risk of accumulation. DISPOSITION 1. HOME – if mild symptoms, with information regarding eg GP Review CADs (Community Alcohol & Drug Service Ph: 6232323 Central 8366166 West 5882701 North 2778080 South Home Detox Service / Inpatient Unit 50 Carrington Road, Pt Chevalier Ph: 8155830 Social Detoxification Centre 203 Federal Street Ph: 3033016 Alcoholcs Anonomous PO Box 5373, Wellesley St, Auckland Ph: 366 6688 Consider a short-term prescription for diazepam prior to GP or Detox review if withdrawal symptoms. If not withdrawing suggest continue drinking enough alcohol to prevent symptoms prior to GP / CAD’s review. 2. ADMISSION TO HOSPITAL 3. Hepatic decompensation Infection or fever >38.5 Severe dehydration Acute haematemesis / malaena Malnutrition Cardiovascular collapse / cardiac arrhythmias Wernicke’s encephalopathy Recent head injury with loss of consciousness Acute alcohol poisoning ADMISSION TO A DETOXIFICATION SERVICE. Contact Admissions Coordinator Grafton Regional Detoxification Service 88 Grafton Rd, Grafton Phone: 377 0370 Fax: 377 0380 Admission indicated if there is a high risk of medical danger eg: History of withdrawal seizures Medical problems – IDDM, IHD Severe symptoms – but not requiring hospital admission Pregnant especially first trimester Detox will not consider a patient for a crisis admission solely on the basis of social issues unless the patient is the primary care giver of children whose safety is at risk If there are no detoxification beds available, discuss with Medical team regarding hospital admission. REFERRENCES 1. Pharmacological management of Alcohol Withdrawal. A meta- analysis and Evidence Based Guidelines. American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA. 278(2):144 – 51. 1997 2. Guideline for the Management of Alcohol Withdrawal in Hospital. Professional Practice Manual. Auckland Healthcare. ALCOHOL WITHDRAWAL RATING SCALE GUIDELINES FOR MANAGEMENT OF ALCOHOL WITHDRAWAL IN HOSPITAL HYDROFLUORIC ACID BURNS INTRODUCTION Hydrofluoric acid (HF) is one of the strongest inorganic acids. A severe burn can be considered if: 1. 2. 3. HF of 50% concentration or greater burns >1% body surface area HF of any concentration to >5% body surface area Inhalation of >60% HF concentration Mechanism of toxicity: 1. 2. 3. Local tissue damage secondary to hydrogen ions Local tissue damage secondary to fluoride ions forming insoluble salts with calcium and magnesium Systemic effects of hypocalcemia, hyperkalaemia, hypomagnesaemia, including cardiac arrhythmias / sudden death Burn manifestations: 1. 2. 3. Relatively little surface reaction. Delayed severe pain in the region. Time of onset is related to the concentration of HF. MANAGEMENT OF HYDROFLOURIC ACID BURNS ABC's ECG IV access Bloods, including urgent Ca, K, Mg Monitoring Systemic Hypocalcaemia - long QT - low serum Ca 2 - clinical Local burn Decontamination Remove clothing Copious irrigation with water 20ml 10% Ca Gluconate stat continue with 10ml aliquots as per response May require very large dose 2.5% Calcium Gel* topically e.g. fill a glove applied over the hand Liaise with DCCM regarding admission Symptomatic at 30 minutes FURTHER TREATMENT Upper Limb: - Bier's block using 10mls of 10% calcium gluconate and 5,000 units heparin diluted to 40mls in normal saline rather than prilocaine. Duration 20 minutes with gel reapplied post-treatment Elsewhere: - Subcutaneous infiltration of 0.5ml / square cm of burn of 10% Ca gluconate. Extend 0.5cm beyond the margin of obviously burned tissue. - Local intra-arterial infusions may be considered Liaise with Plastic surgery in large lifethreatening burns. Surgical debridement may be live saving * If gel not available dissolve 10% calcium gluconate in 3 times the volume of KY jelly. METHANOL POISONING Background The vast majority of methanol poisonings seen in Auckland ED are due to ingestion of methylated spirits (95% ethanol, 2-5% methanol). Those consuming methylated spirits are often chronic methanol/ethanol abusers. There is good evidence that in this subgroup of patients significant methanol toxicity does not occur regardless of methanol level. This subgroup of patients can simply be treated as if drunk and discharged as soon as they are safely sober. Those who are not chronically alcohol tolerant and those who consume preparations containing fractions of methanol above 5% are at risk of developing significant toxicity. Relevant history Formulation of methanol ingested (usually methylated spirits as above) Time of ingestion Amount ingested Any coingestions Reasons for ingesting (recreational, self harm) Significant medical conditions Physical findings The initial presenting signs of methanol toxicity are similar to ethanol intoxication. Significant toxic signs and symptoms develop after a latency of between 10 and 30 hours in general appearing sooner with larger poisonings. Gastrointestinal effects due to chemical irritation of mucosa Ocular disturbances due to direct and preferential toxicity of the optic nerve (blurred vision, whiteout) Severe metabolic acidosis manifest as dyspnoea, tachypnoea, Kussmaul’s respiration and cardiovascular collapse Laboratory investigation U&E’s, glucose, ethanol and methanol levels ABG Consider paracetamol/salicylate levels if self harm suspected (methanol toxicity may mask symptoms of salicylate poisoning) Management Is treatment indicated. See background note above Attend to ABC’s as required. Decontamination ineffective unless significant coingestants Aggressive correction of metabolic acidosis with Sodium Bicarbonate (Doses >500mmol in first few hours commonly required) Antidotal therapy with ethanol (ethanol level > 20mmol/L will completely inhibit methanol metabolism). If initial ethanol level is greater than 20mmol/L a loading dose is not required 10% ethanol loading dose 10ml/kg 10% ethanol maintenance dose @1ml/kg/hr in non alcohol tolerant @2.5mg/kg/hr in alcohol tolerant Check ethanol levels after 4 hours and adjust. Ethanol infusion should continue until methanol levels are <6mmol/L and acidosis has completely resolved Consider haemodialysis in anyone who has any of the following (discuss with consultant) 1. 2. 3. 4. Disposition Metabolic acidosis of any degree and visual disturbance Severe metabolic acidosis (base deficit > 15 mmol/L) Ingestions of methanol estimated at > 40mls Methanol level. 20mmol/L Discharge if treatment not indicated and ingestion not due to attempted self-harm. Psychiatric referral if medically clear and self harm suspected Medical admission if significant poisoning in susceptible patient requiring ethanol infusion DCCM admission if significant metabolic abnormality either on arrival or during initial assessment and treatment. References Martensson E. et al. Clinical and Metabolic Features of EthanolMethanol Poisonings in Chronic Alcoholics. Lancet Feb 13 1988 Pg. 327-328 Kruse J.A. Methanol Poisoning (review). Intensive Care Medicine 1992 18:pg 391-397 Methanol/methylated spirits. Substance Abuse Database POISONED PATIENTS 1. INITIAL RESUSCITATION 2. RELEVANT HISTORY 3. RELEVANT EXAMINATION Identify drug/s Quantity Time taken and route Any remedial treatment to date Reason for taking Significant medical conditions Most acute toxicity presents as cardiorespiratory or neurological symptoms or signs Consider possibility of co-existent physical injuries 4. MINIMUM INVESTIGATION SET FOR DELIBERATE SELF HARM Airway – ensure / procure Breathing 1. Supplemental 02 if any alteration of LOC 2. Ventilatory assistance if required Circulation – IV access and fluids in initial management of hypotension 1. 2. 3. 4. U&E’s, glucose, ethanol, paracetamol, salicylate ECG – if history of ingestion of cardiovascular drugs, drug with known cardiovascular side effects, or any patient with altered LOC or abnormal vital signs Carboxyhaemoglobin level in suspected CO poisonings with signs or history of decreased LOC Additional investigations such as blood drug levels only useful if likely to alter management i.e. digoxin, Li+, Fe++ Refer to Substance Abuse Database for advice regarding these 5. DECONTAMINATION 1. 2. 3. 6. MONITORING Activated charcoal 50G to be given to all patients with significant poisoning presenting within 1 hour of ingestion. Ensure intact or protected airway. Gastric lavage should only be considered in the severely poisoned patient presenting within 1 hour of ingestion (discuss with Consultant). Surface decontamination – with soap and water for dermal poisonings (i.e. organophosphate sprays). Ensure staff barrier precautions. In general asymptomatic patient with normal examination and investigation as above should be observed for 6 hours from the time of poisoning and may safely be medically 7. VIOLENT UNCO-OPERATIVE PATIENTS 8. ANTIDOTAL / ANTAGONIST THERAPIES 9. ENHANCED ELIMINATION 10. PSYCHIATRIC ASSESSMENT 11. RECREATIONAL DRUG ABUSE 12. DISPOSITION cleared after this time. Exceptions to this rule include those who have taken delayed release preparations, and those with significant comorbidities (discuss with Consultant) You have a legal mandate/obligation to detain and treat suicidal patients and those whose mental competence to refuse treatment is impaired by drugs or concurrent illness. Chemical sedation is the preferred method of patient restraint. Appropriate drug regimens (unless prior allergy noted) include: 1. Clonazepam 1mg aliquots IM / IV repeated as required 2. Midazolam 5mg aliquots IM / IV repeated as required 3. Haloperidol 5mg aliquots IM / IV repeated as required Available for a limited number of poisons Refer to Substance Abuse Database for information regarding indications for, and methods of use Rarely required Discuss possible indications with Consultant Mandatory for all deliberate self poisonings prior to discharge once medically cleared. Contact: Psych Liaison 0800 – 2300 On Call Psych Reg 2300 – 0800 Offer contact details of appropriate drug addiction services prior to discharge (information is available at nurses station) Likely dispositions include: 1. Discharge – medically and psychiatrically cleared. 2. Medical Admission – symptoms and signs of toxicity persist >6 hours from time of poisoning or ongoing antidotal treatment required. 3. DCCM – severe poisoning requiring ongoing support of cardiorespiratory, neurological or renal function 4. Psychiatric Admission – committal / voluntary References: 1. Position Statement American Academy of Clinical Toxicology : European Association of Poisons Centres and Clinical Toxicologists. Clinical Toxicology, 35(7) 699-762 (1997) 2. Medicolegal Aspects of Managing Deliberate Self Harm in The Emergency Department. NZ Med J 1998; 110 255-258.