Antimicrobial-Stewardship-in-small-HSOs-19-Dec
advertisement
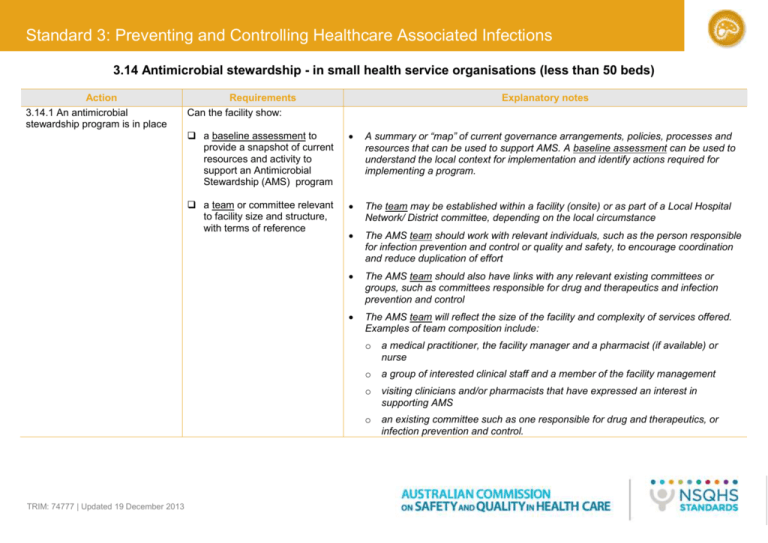
Standard 3: Preventing and Controlling Healthcare Associated Infections 3.14 Antimicrobial stewardship - in small health service organisations (less than 50 beds) Action 3.14.1 An antimicrobial stewardship program is in place TRIM: 74777 | Updated 19 December 2013 Requirements Can the facility show: Explanatory notes a baseline assessment to provide a snapshot of current resources and activity to support an Antimicrobial Stewardship (AMS) program A summary or “map” of current governance arrangements, policies, processes and resources that can be used to support AMS. A baseline assessment can be used to understand the local context for implementation and identify actions required for implementing a program. a team or committee relevant to facility size and structure, with terms of reference The team may be established within a facility (onsite) or as part of a Local Hospital Network/ District committee, depending on the local circumstance The AMS team should work with relevant individuals, such as the person responsible for infection prevention and control or quality and safety, to encourage coordination and reduce duplication of effort The AMS team should also have links with any relevant existing committees or groups, such as committees responsible for drug and therapeutics and infection prevention and control The AMS team will reflect the size of the facility and complexity of services offered. Examples of team composition include: o a medical practitioner, the facility manager and a pharmacist (if available) or nurse o a group of interested clinical staff and a member of the facility management o visiting clinicians and/or pharmacists that have expressed an interest in supporting AMS o an existing committee such as one responsible for drug and therapeutics, or infection prevention and control. 3.14 Antimicrobial stewardship - in small health service organisations (less than 50 beds) Action (Continued) Requirements A governance structure for AMS that includes communication lines with the AMS team and roles and responsibilities of executive/management in supporting the team and stewardship activities a program plan that includes actions for implementation and timeline Explanatory notes The governance structure should incorporate formal structural alignment of the AMS team to relevant committees and be endorsed by the hospital executive While specialist infectious disease clinicians, medical microbiologists and pharmacists may not be onsite in a small facility, access to and involvement of these experts will assist in an effective AMS program Hospital or relevant network district governance arrangements should include processes for seeking external specialist advice to support the local AMS team in the program plan. For example, it may be possible to have a dedicated AMS pharmacist and/or a specialist clinician responsible for coordinating stewardship activities across a number of facilities, working in collaboration with local teams/committees. To establish arrangements for external specialist advice, the program plan should include documented strategies for negotiating such advice, incorporating actions, responsibilities, timelines and a process to review progress. Progress towards implementation should be monitored. The AMS program plan will provide detail of how the program will be implemented, and may be at facility or network/district level. It is essentially an action plan that describes who/which group will be responsible for what actions, when each of the actions will be put into place, the resources required and measures to be used to monitor progress. The priorities should be guided by the results of the baseline assessment. a policy that specifies prescribing clinicians should follow Therapeutic Guidelines: Antibiotic (or state based guidelines based on Therapeutic Guidelines: Antibiotic) 2 3.14 Antimicrobial stewardship - in small health service organisations (less than 50 beds) Action 3.14.2 The clinical workforce prescribing antimicrobials have access to current endorsed therapeutic guidelines on antibiotic usage 3.14.3 Monitoring of antimicrobial usage and resistance is undertaken Requirements prescribing clinicians have access to Therapeutic Guidelines: Antibiotic (may include printed/hard copy or electronic) a system for monitoring antimicrobial usage is documented and included in the AMS program plan a system for monitoring resistance is documented and included in the program plan results of usage and resistance monitoring are reported to and reviewed by the relevant committees Explanatory notes Therapeutic Guidelines: Antibiotic or state based endorsed guidelines Monitoring antimicrobial usage and resistance is critical to understanding antimicrobial prescribing trends and resistance patterns and should be addressed within the program plan The methods of monitoring antimicrobial usage should be relevant to the size and complexity of the facility. Examples could include: o Reviewing the list of stock ordered and used each month, as well as reviewing monthly expenditure of antimicrobials (the supplying pharmacy should be able to provide usage reports) o Monitoring antimicrobial usage in a high risk area, in relation to a specific procedure, clinical condition, or of high risk or broad spectrum antimicrobials and later generation antimicrobials (e.g. 3rd and 4th generation cephalosporin and quinolones). High use or high expenditure can provide a ‘flag’ for facilities to undertake a more detailed analysis of usage such as a clinical audit/drug use evaluation. Methods of monitoring resistance should also be relevant to the facility and could include: o Undertaking surveillance by reviewing the incidence of HAI in a targeted area, or reviewing targeted organisms such as MRSA, VRE or ESBL. 3 3.14 Antimicrobial stewardship - in small health service organisations (less than 50 beds) Action 3.14.4 Action is taken to improve the effectiveness of antimicrobial stewardship Requirements the AMS program plan includes details of how program effectiveness will be monitored and reviewed the plan includes strategies to reduce inappropriate use of antimicrobials and optimise their use For further information please contact: Australian Commission on Safety and Quality in Health Care Phone 1800 304 056 http://www.safetyandquality.gov.au Explanatory notes Monitoring program effectiveness can be achieved through o Expanding usage monitoring to include high risk antimicrobials, or broad spectrum antimicrobials and later generation antimicrobials (e.g. 3rd and 4th generation cephalosporin and quinolones) o Identification and review of adverse events/incidents related to antimicrobial prescribing o Effectiveness can be measured by reviewing usage reports, conducting audits or using indicators from Quality Use of medicines Indicators for Australian Hospitals o Review of Staphylococcus aureus Bacteraemia rates (i.e. data collected for the MyHospitals website) and documentation of actions taken to improve. Strategies to reduce inappropriate use of antimicrobials in small facilities could include : o Implementing antibiotic guidelines for common conditions such as community acquired pneumonia o Implementing antibiotic guidelines for surgical prophylaxis o Developing a process to provide feedback to prescribers o Reviewing duration of use o Implementing an ‘IV to oral’ policy o Including in the program plan future actions for education programs to incorporate content on AMR and AMS for relevant staff (consider available online programs such as antimicrobial prescribing modules www.nps.org.au/health_professionals/online_learning, and ACSQHC Antimicrobial stewardship for nurses e-learning module (latter currently under development). Strategies and resources to assist health care facilities with the implementation of antimicrobial stewardship programs can be found in the Commission publication Antimicrobial Stewardship in Australian Hospitals 2011, available at: http://www.safetyandquality.gov.au/our-work/healthcare- 4 associated-infection/antimicrobial-stewardship/