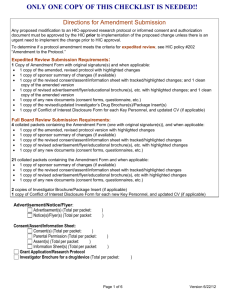
100FR17PediatricProtocol_Application_Form_BioMed3-6
advertisement
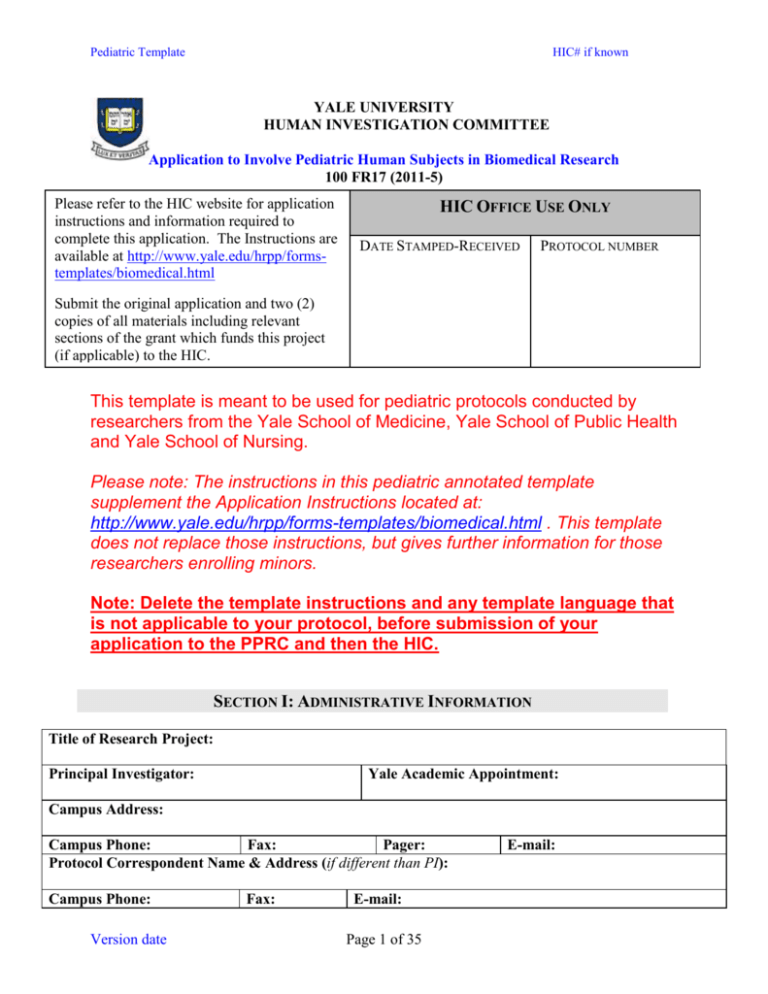
Pediatric Template HIC# if known YALE UNIVERSITY HUMAN INVESTIGATION COMMITTEE Application to Involve Pediatric Human Subjects in Biomedical Research 100 FR17 (2011-5) Please refer to the HIC website for application instructions and information required to complete this application. The Instructions are available at http://www.yale.edu/hrpp/formstemplates/biomedical.html HIC OFFICE USE ONLY DATE STAMPED-RECEIVED PROTOCOL NUMBER Submit the original application and two (2) copies of all materials including relevant sections of the grant which funds this project (if applicable) to the HIC. This template is meant to be used for pediatric protocols conducted by researchers from the Yale School of Medicine, Yale School of Public Health and Yale School of Nursing. Please note: The instructions in this pediatric annotated template supplement the Application Instructions located at: http://www.yale.edu/hrpp/forms-templates/biomedical.html . This template does not replace those instructions, but gives further information for those researchers enrolling minors. Note: Delete the template instructions and any template language that is not applicable to your protocol, before submission of your application to the PPRC and then the HIC. SECTION I: ADMINISTRATIVE INFORMATION Title of Research Project: Principal Investigator: Yale Academic Appointment: Campus Address: Campus Phone: Fax: Pager: Protocol Correspondent Name & Address (if different than PI): Campus Phone: Version date Fax: E-mail: Page 1 of 35 E-mail: Pediatric Template HIC# if known Faculty Advisor:(required if PI is a student, resident, fellow or other trainee) NA Yale Academic Appointment: Campus Address: Campus Phone: Fax: Pager: E-mail: Does the principal investigator, co-investigator, or any other responsible research team member, or any of their family members (spouse, child, domestic partner) have an incentive or interest, financial or otherwise, that may be viewed as affecting the protection of the human subjects involved in this project, the scientific objectivity of the research or its integrity? See Disclosures and Management of Personal Interests in Human Research http://www.yale.edu/hrpp/policies/index.html#COI Yes No If yes, list names of the investigator or responsible person: The Yale University Principal Investigator and all Yale University and Yale New Haven Hospital individuals who are listed as co-investigators on a protocol with a Yale University Principal Investigator must have a current financial disclosure form on file with the University’s Conflict of Interest Office. Conflict of Interest Office. If this has not been done, the individual(s) should follow this link to the COI Office Website to complete the form: http://www.yale.edu/coi/ NOTE: The requirement for maintaining a current disclosure form on file with the University’s Conflict of Interest Office extends primarily to Yale University and Yale-New Haven Hospital personnel. Whether or not they are required to maintain a disclosure form with the University’s Conflict of Interest Office, all investigators and individuals deemed otherwise responsible by the PI who are listed on the protocol are required to disclose to the PI any interests that are specific to this protocol. SECTION II: GENERAL INFORMATION 1. Performing Organizations: Identify the hospital, in-patient or outpatient facility, school or other agency that will serve as the location of the research. Choose all that apply: a. Internal Location[s] of the Study: Magnetic Resonance Research Center (MR-TAC) Yale Cancer Center/Smilow Yale Cancer Center/Clinical Trials Office Yale-New Haven Hospital Specify Other Yale Location: Yale University PET Center YCCI/Church Street Research Unit (CSRU) YCCI/Hospital Research Unit (HRU) YCCI/Keck Laboratories Cancer Data Repository/Tumor Registry b. External Location[s]: APT Foundation, Inc. Connecticut Mental Health Center Clinical Neuroscience Research Unit (CNRU) Other Locations, Specify: location(s)): Haskins Laboratories John B. Pierce Laboratory, Inc. Veterans Affairs Hospital, West Haven International Research Site (Specify Version date Page 2 of 35 Pediatric Template HIC# if known c. Additional Required Documents (check all that apply): N/A *YCCI-Scientific and Safety Committee (YCCI-SSC) Approval Date: *Pediatric Protocol Review Committee (PPRC) Approval Date: *YCC Protocol Review Committee (YRC-PRC) Approval Date: *Dept. of Veterans Affairs, West Haven VA HSS Approval Date: *Radioactive Drug Research Committee (RDRC) Approval Date: YNHH-Radiation Safety Committee (YNHH-RSC) Approval Date: Magnetic Resonance Research Center PRC (MRRC-PRC) Approval Date: YSM/YNHH Cancer Data Repository (CaDR) Approval Date: Dept. of Lab Medicine request for services or specimens form *Approval from these committees is required before final HIC approval is granted. See instructions for documents required for initial submission and approval of the protocol. Allow sufficient time for these requests. Check with the oversight body for their time requirements. 2. Probable Duration of Project: State the expected duration of the project, including all follow-up and data analysis activities. The numbers of subjects need to match in all documents (e.g. parental permission and consent form if you have participants > 18 years of age) as well as within this HIC application, especially if you have different groups participating in the study. It is important for PPRC to know how many minors are being exposed to the observation or intervention. The number of subjects should be minimized consistent with good study design. Also, this is the place to indicate if you think that you need to enroll more subjects or have more subjects sign the consent form because there will be a certain drop-out or non-completion rate. 3. Research Type/Phase: (Check all that apply) a. Study Type Single Center Study Multi-Center Study Does the Yale PI serve as the PI of the multi-site study? Yes Coordinating Center/Data Management Other: b. Study Phase Pilot Other (Specify) N/A Phase I Phase II Phase III 4. No Phase IV Area of Research: (Check all that apply) Note that these are overlapping definitions and more than one category may apply to your research protocol. Definitions for the following can be found in the instructions section 4c: Clinical Research: Patient-Oriented Clinical Research: Outcomes and Clinical Research: Epidemiologic and Behavioral Health Services Translational Research #1 (“Bench-to-Bedside”) Interdisciplinary Research Translational Research #2 (“Bedside-to-Community”) Community-Based Research Version date Page 3 of 35 Pediatric Template HIC# if known 5. Is this study a clinical trial? Yes No NOTE the current ICMJE (International Committee of Medical Journal Editors) definition of a clinical trial: “any research study that prospectively assigns human participants or groups of humans to one or more health-related interventions to evaluate the effects on health outcomes.” Health-related interventions include any intervention used to modify a biomedical or healthrelated outcome (for example, drugs, surgical procedures, devices, behavioral treatments, dietary interventions, and process-of-care changes). Health outcomes include any biomedical or health-related measures obtained in patients or participants, including pharmacokinetic measures and adverse events” If yes, where is it registered? Clinical Trials.gov registry Other (Specify) Registration of clinical trials at their initiation is required by the FDA, NIH and by the ICMJE. If this study is registered on clinicaltrials.gov, there is new language in the consent form and compound authorization that should be used. For more information on registering clinical trials, including whether your trial must be registered, see the YCCI webpage, http://ycci.yale.edu/researchers/ors/registerstudy.aspx or contact YCCI at 203.785.3482) 6. Will this study have a billable service as defined by the Billable Service Definition? Yes No If you answered "yes", this study will need to be set up in Patient Protocol Manager (PPM) http://medicine.yale.edu/ymg/systems/ppm/index.aspx 7. Are there any procedures involved in this protocol that will be performed at YNHH or one of its affiliated entities? Yes ___ No ___ If Yes, please answer questions a through c and note instructions below. If No, proceed to Section III. a. Does your YNHH privilege delineation currently include the specific procedure that you will perform? b. Will you be using any new equipment or equipment that you have not used in the past for this procedure? c. Will a novel approach using existing equipment be applied? If you answered “no” to question 7a, or "yes" to question 7b or c, please contact the YNHH Department of Physician Services (688-2615) for prior approval before commencing with your research protocol. SECTION III: FUNDING, RESEARCH TEAM AND TRAINING Version date Page 4 of 35 Pediatric Template HIC# if known 1. Funding Source: Indicate all of the funding source(s) for this study. Check all boxes that apply. Provide information regarding the external funding source. This information should include identification of the agency/sponsor, the funding mechanism (grant or contract), and whether the award is pending or has been awarded. Provide the M/C# and Agency name (if grantfunded). If the funding source associated with a protocol is “pending” at the time of the protocol submission to the HIC (as is the case for most NIH submissions), the PI should note “Pending” in the appropriate section of the protocol application, provide the M/C# and Agency name (if grant-funded) and further note that University (departmental) funds support the research (until such time that an award is made). PI Title of Grant Name of Funding Source Funding Federal State Non Profit Industry Other For Profit Other Federal State Non Profit Industry Other For Profit Other Federal State Non Profit Industry Other For Profit Other Funding Mechanism Grant-M# Contract# Contract Pending Investigator/Department Initiated Sponsor Initiated Other, Specify: Grant-M# Contract# Contract Pending Investigator/Department Initiated Sponsor Initiated Other, Specify: Grant-M# Contract# Contract Pending Investigator/Department Initiated Sponsor Initiated Other, Specify: IRB Review fees are charged for projects funded by Industry or Other For-Profit Sponsors. Provide the Name and Address of the Sponsor Representative to whom the invoice should be sent. Note: the PI’s home department will be billed if this information is not provided. Send IRB Review Fee Invoice To: Name: Company: Address: 2. Research Team: List all members of the research team. Indicate under the affiliation column whether the investigators or study personnel are part of the Yale faculty or staff, or part of the faculty or staff from a collaborating institution, or are not formally affiliated with Version date Page 5 of 35 Pediatric Template HIC# if known any institution. ALL members of the research team MUST complete Human Subject Protection Training (HSPT) and Health Insurance Portability and Accountability Act (HIPAA) Training before they may be listed on the protocol. See NOTE below. Name Affiliation: Yale/Other Institution (Identify) NetID Principal Investigator Role: Role: Role: Role: Role: Role: NOTE: The HIC will remove from the protocol any personnel who have not completed required training. A personnel protocol amendment will need to be submitted when training is completed. SECTION IV: PRINCIPAL INVESTIGATOR/FACULTY ADVISOR/ DEPARTMENT CHAIR AGREEMENT As the principal investigator of this research project, I certify that: The information provided in this application is complete and accurate. I assume full responsibility for the protection of human subjects and the proper conduct of the research. Subject safety will be of paramount concern, and every effort will be made to protect subjects’ rights and welfare. The research will be performed according to ethical principles and in compliance with all federal, state and local laws, as well as institutional regulations and policies regarding the protection of human subjects. All members of the research team will be kept apprised of research goals. I will obtain approval for this research study and any subsequent revisions prior to my initiating the study or any change and I will obtain continuing approval of this study prior to the expiration date of any approval period. I will report to the HIC any serious injuries and/or other unanticipated problems involving risk to participants. I am in compliance with the requirements set by the University and qualify to serve as the principal investigator of this project or have acquired the appropriate approval from the Dean’s Office or Office of the Provost, or the Human Subject Protection Administrator at Yale-New Haven Hospital, or have a faculty advisor. I will identify a qualified successor should I cease my role as principal investigator and facilitate a smooth transfer of investigator responsibilities. _____ PI Name (PRINT) and Signature Version date Date Page 6 of 35 Pediatric Template HIC# if known As the faculty advisor of this research project, I certify that: The information provided in this application is complete and accurate. This project has scientific value and merit and that the student or trainee investigator has the necessary resources to complete the project and achieve the aims. I will train the student investigator in matters of appropriate research compliance, protection of human subjects and proper conduct of research. The research will be performed according to ethical principles and in compliance with all federal, state and local laws, as well as institutional regulations and policies regarding the protection of human subjects. The student investigator will obtain approval for this research study and any subsequent revisions Prior to initiating the study or revision and will obtain continuing approval prior to the expiration of any approval period. The student investigator will report to the HIC any serious injuries and/or other unanticipated problems involving risk to participants. I am in compliance with the requirements set forth by the University and qualify to serve as the faculty advisor of this project. ___________ ______ _____ Advisor Name (PRINT) and Signature Date ______ Department Chair’s___________ Assurance Statement _____ Advisor Name (PRINT) and Signature Date Do you know of any real or apparent institutional conflict of interest (e.g., Yale ownership of a sponsoring company, patents, licensure) associated with this research project? Yes (provide a description of that interest in a separate letter addressed to the HIC.) No As Chair, do you have any real or apparent protocol-specific conflict of interest between yourself and Signature of PI Date the sponsor of the research project, or its competitor or any interest in any intervention and/or method tested in the project that might compromise this research project? Yes (provide a description of that interest in a separate letter addressed to the HIC.) No I assure the HIC that the principal investigator and all members of the research team are qualified by education, training, licensure and/or experience to assume participation in the conduct of this research trial. I also assure that the principal investigator has departmental support and sufficient resources to Version date Page 7 of 35 Pediatric Template HIC# if known conduct this trial appropriately. ____________________________ Chair Name (PRINT) and Signature Date _________________________________ Department YNHH Human Subjects Protection Administrator Assurance Statement Required when the study is conducted solely at YNHH by YNHH health care providers. As Human Subject Protection Administrator (HSPA) for YNHH, I certify that: I have read a copy of the protocol and approve it being conducted at YNHH. I agree to notify the IRB if I am aware of any real or apparent institutional conflict of interest. The principal investigator of this study is qualified to serve as P.I. and had the support of the hospital for this research project. ______________________________________ YNHH HSPA Name (PRINT) and Signature Date For HIC Use Only Date Approved Human Investigation Committee Signature SECTION V: RESEARCH PLAN 1. Statement of Purpose: State the scientific aim(s) of the study, or the hypotheses to be tested. Explain the purpose or aim(s) of the study clearly so that the reviewer(s) are able to justify the inclusion of a pediatric population. The reviewer needs to understand the PI’s justification for the inclusion of children; therefore, the rationale should be clear and fully explained. The reviewer(s) should also be able to ascertain if the question(s) or the study/aim(s) or purpose is clinically meaningful, scientifically sound, significant, and with value to children in general, and in most cases, to the individual child subject. 2. Background: Describe the background information that led to the plan for this project. Provide references to support the expectation of obtaining useful scientific data. Version date Page 8 of 35 Pediatric Template HIC# if known Provide all relevant studies to your research (adult and pediatric), especially any pediatric studies that are relevant. If no pediatric studies have been performed, state so. If no pediatric studies have been performed, include the literature from as many adult studies as possible, preferably studies in which research of the test article has reached Phase III and beyond. Depending upon the severity of the disease and the availability of an analogous disease or test article being used in adults, include a justification for the study of this test article in this pediatric population at this point in its development. The research problem needs to be one of true scientific uncertainty; that is, the investigator should explain his/her level of true uncertainty and that of the literature about which of the treatments or drugs, etc. being compared (in a comparative study) is superior. 3. Research Plan: Summarize the study design and research procedures using non-technical language that can be readily understood by someone outside the discipline. Be sure to distinguish between standard of care vs. research procedures when applicable, and include any flowcharts of visits specifying their individual times and lengths. In addition to providing an orderly description of each research procedure or observation that the minor will undergo, state if the procedure/test/assessment is standard of care or research-related. Include all visits and procedures and not just a summary of the procedures. The extent to which children are exposed to an intervention is important for a pediatric review. This helps reviewers to assess the risk to the child/adolescent. If there are different groups, provide this description for all groups, especially noting which procedures will NOT be performed on/with the control group. If blood is to be drawn, include the amount and the route, e.g. drawing off an IV, venipuncture, finger stick. Also include the circumstances around the blood draw, e.g. where possible drawn with necessary clinical specimens, only drawn with clinical specimens, etc. Also include the amount of blood to be drawn at each visit and cumulatively, where indicated. (This may also be included in the risks section.) Note (per NIH Guidelines; revised June 5, 2009): Maximum blood volumes for the pediatric patient are as follows: No more than 5ml/kg in a single day (24 hour period) and no more than 9.5 ml/kg to be drawn over any 8 week period. For adolescents the amount drawn may not exceed the maximum amount of blood to be drawn in adults (550 ml over any 8 week period.) For infants (less than one year of age), the weight, medical condition, and the physiological status of the infant or neonate needs to be considered when proposing the amount of blood to be drawn per 24 hour and/or 8 week period. (The Committee will review these blood draw amounts on a case by case basis.) Include the approximate time for each visit or test/procedure. Also disclose this to the parent/child in the permission/assent documents. Include a mechanism for follow-up of research subjects, as applicable, especially with regard to studies of test articles without predicted side/adverse effects. Version date Page 9 of 35 Pediatric Template HIC# if known 4. Genetic Testing N/A A. Describe i. the types of future research to be conducted using the materials, specifying if immortalization of cell lines, whole exome or genome sequencing, genome wide association studies, or animal studies are planned ii. the plan for the collection of material or the conditions under which material will be received iii. the types of information about the donor/individual contributors that will be entered into a database iv. the methods to uphold confidentiality B. What are the conditions or procedures for sharing of materials and/or distributing for future research projects? C. Is widespread sharing of materials planned? D. When and under what conditions will materials be stripped of all identifiers? E. Can donor-subjects withdraw their materials at any time, and/or withdraw the identifiers that connect them to their materials? i. How will requests to withdraw materials be handled (e.g., material no longer identified: that is, anonymized) or material destroyed)? F. Describe the provisions for protection of participant privacy G. Describe the methods for the security of storage and sharing of materials 5. Subject Population: Provide a detailed description of the types of human subjects who will be recruited into this study. Children--Definition Specific conditions are cited in the federal regulations regarding the inclusion of children into research. Children include all persons who have not attained the legal age to consent for themselves to treatments or procedures under the applicable law of the jurisdiction in which the research will be conducted. In Connecticut, this legal age is 18 years, except for children seeking treatment for substance abuse, mental health, and reproductive health, or when the child is emancipated. Investigators should note that in the State of Connecticut, pregnancy does not qualify a child as being emancipated. Emancipated minor: According to CT State Statute, Sec. 46b-150 at http://www.cga.ct.gov/2009/pub/Chap815t.htm#Sec46b-150.htm. “Any minor who has reached such minor’s sixteenth birthday and is residing in this state, or parent or guardian of such minor may petition the superior court for juvenile matters or the probate court for the district…for a determination that the minor named in the petition be emancipated.” The order of emancipation (Sec. 46b-150b.) may be granted by the Superior Court or Probate Court, after a hearing if the court finds that: (1) The minor has entered into a valid marriage, whether or not the marriage has been terminated by dissolution; or (2) the minor is on active duty with any of the armed forces of the United States of America; or (3) the minor willingly lives separate and apart from his parents or guardian, with or without the consent of the parents or guardian, and that the minor is managing his own financial affairs, regardless of the source of any lawful income; or (4) Version date Page 10 of 35 Pediatric Template HIC# if known for good cause shown, it is in the best interest of the minor, any child of the minor or the parents or guardian of the minor, the court may enter an order declaring that the minor is emancipated.” The statute continues with regard to the effect of emancipation (Sec. 46b-150d.) which states that, “(1) The minor may consent to medical, dental, or psychiatric care, without parental consent, knowledge, or liability; (2) the minor may enter into a binding contract…” Investigators should take care to check for the court order of emancipation before treating the minor as emancipated for consenting or other research purposes. See the statute for further information. Institutionalized children: These children should be rarely considered for inclusion in research studies, because institutionalization may deprive them of some of the safeguards necessary for the conduct of ethical investigations. These children may be involved in studies of special conditions unique to them or to the type of institution in which they reside. They should also have access to experimental drug therapy when the research therapy is the only treatment available for the illness that affects them. The IRB may require that the PI consult and document the consultation with an advocacy group that will assist with the overall design of the study as it relates to the rights, clinical condition, and needs of such a targeted population. Explain these conditions in the HIC application. Provide a description of the minors to be included, items like age and, in cases where drugs are being given or large amounts of blood drawn, average weight or range of weight for inclusion are important. 6. Subject classification: Check off all classifications of subjects that will be targeted for enrollment in the research project. Will subjects who may require additional safeguards or other considerations be enrolled in the study? If so, identify the population of subjects requiring special safeguards and provide a justification for their involvement. Children Non-English Speaking Decisionally Impaired Yale Students Healthy Fetal material, placenta, or dead fetus Prisoners Economically disadvantaged persons Employees Pregnant women and/or fetuses Females of childbearing potential NOTE: Is this research proposal designed to enroll children who are wards of the state as potential subjects? Yes No (If yes, see HIC Application Instructions section VII #2 for further requirements) Check off all appropriate populations. 7. Inclusion/Exclusion Criteria: What are the criteria used to determine subject inclusion or exclusion? The inclusion/exclusion criteria should take into account the unique physiology, anatomy, psychology, pharmacology, social situation and special needs of children and their families (as indicated by the study.) Version date Page 11 of 35 Pediatric Template HIC# if known List, in sufficient detail, in this section, inclusion/exclusion, criteria so that the reviewer can assess if the minors are being protected by appropriate selection. For example, screening for pregnancy for females of childbearing potential for interventional drug studies, appropriate frequency and pertinent parameters for baseline and follow-up laboratory values for certain tests or procedures, (based upon the clinical condition of the patient and the purpose of the research), and the subject’s weight for certain amounts of blood to be drawn. If you are drawing the maximum amount of blood within an 8 week period, the child/parent should be advised not to participate in other studies where blood is drawn and young adults (over 17 years of age) should be advised not to donate blood for a period of 8 weeks after study participation (American Red Cross Blood Donation Guidelines). (See Research Plan section for maximum amounts of blood to be drawn.) 8. How will eligibility be determined, and by whom? 9. Risks: Describe the reasonably foreseeable risks, including risks to subject privacy, discomforts, or inconveniences associated with subjects participating in the research. List all foreseeable risks and inconveniences to the minor and to his/her parents. Since all research has some risk, it can be stated that the research has “minimal” risks or “no physical risks” depending upon the situation. These risks should include the known and predictable risks of the drug/test article being studied as determined from previous human (adult and pediatric) and animal studies in addition to the inherent risks of the procedures themselves. These risks should match internally within this document and with the consent/permission/assent documents. List risks of all procedures performed, where applicable. Blood drawing: list the risks of the blood draw, depending upon the method, (e.g. IV or venipuncture), such as pain, bleeding at site, redness, inflammation, ecchymosis; rarely phlebitis, infection and fainting. As per the research plan, list the risks of all procedures, noting those that are for research purposes only. For example, if it would be standard of care to obtain a chest xray once per year in the population you are studying, but you want to obtain an x-ray every 6 months, this should be clearly noted as a risk with the amount of radiation cited for that risk. If the radiation utilized in the protocol is for research purposes, complete the Radiation Safety Committee application located at http://rsc.med.yale.edu. 10. Minimizing Risks: Describe the manner in which the above-mentioned risks will be minimized. Overall, the plan to minimize risks and monitor safety needs to be robust. The type and number of invasive tests should be minimized and scientifically sound, and creative methods to obtain needed information non-invasively should be sought. Version date Page 12 of 35 Pediatric Template HIC# if known Denote how each risk listed above will be minimized. For example, for blood drawing, it is preferable to include whether a topical anesthetic will be utilized prior to the blood draw or intravenous placement. Include the types of topical anesthetic in the HIC application and the consent documents. The methods of administration of these anesthetics include intradermal and topical, e.g. creams and/or patches. Include the pediatric protections and opt out clause for pregnancy, as applicable. Investigators may refer to http://www.ct.gov/dph/lib/dph/Sec19a-216.pdf, which is generally used as a guideline for dealing with the issue of confidentiality of pregnancy testing in minors. If the minor is less than 13 years of age, the facility or physician is advised to report the name, age, and address of the pregnant minor to the Commissioner of Children and Families or his designee. Also, in an opinion written by the Attorney General (September 30, 2002), Attorney General Blumenthal stated, “The Department has taken the position that a mandated reporter is obliged to report any sexual relations involving a minor less than the age of 13 [years]…” See this opinion for further information with regard to mandatory reporting of abuse or neglect. The pregnancy language to be included in each document is as follows: (Modify for your protocol procedures for the patient population of interest, as applicable.) Protocol: Female subjects of childbearing potential will require urine/serum pregnancy testing prior to enrollment in the protocol. Because full confidentiality regarding pregnancy cannot be entirely guaranteed, these testing requirements and the limited scope of confidentiality will be made known to all subjects during the consent procedure. In this manner, young women who would not be comfortable with pregnancy testing or sharing the results of such testing can “opt out” of the study at the time of the initial consent, without having to declare specific reasons. According to CT state statutes for mandatory reporting, pregnancy in females less than age of 13 years, will be reported to parent(s) and to the State of Connecticut Department of Children and Family Services (DCF). Confidentiality with regard to pregnancy test results will be maintained for females > 13 years. Parental Permission: Female subjects of childbearing potential will require urine/serum pregnancy testing prior to proceeding with the protocol. Only your daughter, if she is at least 13 years of age, will be told the results. We will, of course, counsel your daughter to seek appropriate healthcare and the support of an adult if she were found to be pregnant. A positive pregnancy test means that your daughter cannot participate in this study. Because she will be asked to leave the study, you may find out that she is pregnant. If you and/or your daughter are uncomfortable with pregnancy testing, then we would recommend that your daughter does not participate. If a positive pregnancy test is found in a minor less than 13 years of age, we will need to report this to you and to the State of Connecticut, Department of Children and Family Services (DCF). Assents may be structured as per developmental age of the patient population versus chronological age. If the patient population of interest is of childbearing Version date Page 13 of 35 Pediatric Template HIC# if known age, then it is advisable that the assent include pregnancy language, if indicated by the study procedures. For the assent form(s), the information about females less than 13 years of age does NOT need to be included, unless it is warranted by the developmental characteristics of patient population under study (in bold type below). Adolescent Assent: We will ask you to have a pregnancy test before you start this study. Only you will be told the results, if you are at least 13 years old. If you are pregnant, we will advise you to get care for your pregnancy and also to get the support of an adult. You will be asked not to participate or you will be removed from the study if your pregnancy test is positive. You need to know that your parents may ask you why you cannot participate or why you were asked to leave the study. So if there is any chance that you are pregnant or you might become pregnant during the time of this study, we would recommend that you think carefully about whether you should participate. It is okay if you decide that you do not want to participate or to stay in this study. You do not need to give a reason for not participating. If you are less than 13 years old, we will need to report a positive pregnancy test to your parents and to the proper authorities, called DCF. We will explain all of this to you and help you to get the care that you need. Precautions with regard to confidentiality of questioning about drugs or drug testing: (Should also be added to confidentiality section of consent form or section where drug testing is discussed in research plan.) Investigators may refer to http://www.ct.gov/dph/lib/dph/practitioner_licensing_and_investigations/plis/psychology/psych_s tatelawstudyguide.pdf for general guidance regarding the confidentiality of questioning about “illicit” drugs or drug testing/treatment in research protocols. In general, the confidentiality of drug testing, questioning about substance abuse history, and mental health treatment is considered confidential between the researcher and the minor, unless the researcher believes that the minor is in imminent risk of serious harm or that maintaining this confidentiality would be associated with serious detriment to the minor’s well-being. Investigators are encouraged to assess adolescents as per their developmental level and their psychiatric or psychological condition. In general, the guidelines of breeching confidentiality and disclosing to parents positive drug testing in a younger adolescent (less than 13 years of age) is accepted practice. For those minors (of any age) who are considered to be exhibiting behavior that the investigator believes may be of harm to the subject or others, the investigator is encouraged to refer these subjects to a licensed psychologist or psychiatrist, who will provide evaluation and treatment, as needed. Note: Judgment with regard to the confidentiality of drug screening may be made by the investigator and the PPRC on a case by case basis, depending upon the nature of the research and the clinical condition/developmental age of the subject. General guidelines and examples of pertinent language are presented throughout this section. Suggested language with regard to confidentiality of drug testing/treatment to be included in each document is as follows: (Modify for your protocol procedures, as applicable.) Version date Page 14 of 35 Pediatric Template HIC# if known For the HIC protocol: In order to participate in this protocol, the pediatric subject will need to be asked questions about his/her prior and/or current illicit drug use or undergo drug testing (urine or blood). Because drug use will exclude the minor from participating, the parent may ask why the child was asked not to participate or to leave the study. Therefore, parents and/or minors who are uncomfortable with questions about drug use can "opt out" of the study at the time of initial consent, without having to declare specific reasons. Drug use information (in the adolescent > 13 years of age) will not be shared with parents unless the study team feels that the minor is exhibiting behaviors that would pose an immediate threat to the minor or to others. The PI or co-investigator will ask the minor if the study team can share the drug testing results with parents. If the minor declines, the study team will refer the minor for evaluation based upon the clinical judgment of the Principal Investigator. In all cases, the safety and well-being of the minor will be protected. We will explicitly inform parents and minors, in the permission and assent documents, and orally with regard to these guidelines. Parental permission form language for confidentiality of drug use: We will need to ask your child/adolescent about current or past use of illicit "street" drugs (or this could be testing if you were going to do urine testing). If he/she is using drugs now or has a history of using drugs, he/she may not be able to participate in this study (or you can make this stronger--he/she will not be able to participate.) If your child is 13 years of age or older, we will keep this information confidential. If your child is 12 years of age or younger, we will notify you and refer your child for an evaluation for substance abuse. If your child is of any age, and in immediate danger of hurting him/herself or someone else, then we will notify you and refer your child for an evaluation. If you or your child is uncomfortable with drug testing or discussing drug use, then we would recommend that your son/daughter does not participate in this study. Adolescent Assent (for > 13 years of age): We will ask you about/or test you for (any past or) current use of “street” drugs. If you are using drugs now or have a history of using drugs, you may not be able to participate in this study. You need to know that your parents may ask you why you cannot participate or why you were asked to leave the study. So if there is any chance that you are using drugs or have used drugs, we would recommend that you think carefully about whether you should participate. It is okay if you decide that you do not want to participate or to stay in this study. You do not need to give a reason for not participating. If your urine is positive for drugs, then you cannot participate in this study. We will ask you if we can discuss your positive drug screening results with your parents. If you decline, we will keep the results of your drug test confidential and we will give you a referral for an evaluation. However, if we feel that you are in danger of hurting yourself or someone else, then we will need to tell your parents and also refer you for help. Adolescent Assent (for 12 years of age and younger), if necessary, for the population of your study: We will ask you for a urine/blood sample or we will ask you about your use of “street drugs.” We will give you a container that you can use in a private bathroom or need to Version date Page 15 of 35 Pediatric Template HIC# if known explain the blood draw. We will check your urine/blood for drugs. These drugs will include “street drugs.” If you are positive for drugs, then you cannot participate in this study. We will discuss these results with you first, and then we will need to discuss these results with your parent(s). This is so we can get you some help. This age group may also be offered the “opt out” of testing or questioning as noted in the adolescent assent section above. . Blood amounts: include the calculation of blood amounts so as to prove that they do not exceed the maximum allowable/approvable limits, e.g. Maximum blood volumes for pediatric patients are as follows: No more than 5ml/kg in any single day (24 hour period) and no more than 9.5 ml/kg to be drawn over any 8 week period. For adolescents, the amount drawn may not exceed the maximum amount of blood to be drawn in adults (550 ml over any 8 week period.) For infants (less than one year of age), the weight, medical condition, and the physiological status of the infant or neonate needs to be considered when proposing the amount of blood to be drawn per 24 hour and/or 8 week period. (The PPRC will review these blood draw amounts on a case by case basis.) As noted in the inclusion/exclusion criteria section, the baseline Hematocrit or hemoglobin of the child should be based upon the clinical condition of the patient and the purpose of the research. The child/parent should also be advised not to participate in other studies where blood is drawn and young adults (over 17 years of age in CT) should be advised not to donate blood for a period of 8 weeks after study participation. (The American Red Cross Blood Donation Guidelines are that minors must be 17 years of age in CT, weigh 110 lbs, and not have given whole blood, i.e. 550 ml of blood, within an eight week period.) For children who are ill and/or hospitalized, investigators should be especially cognizant of the hematocrit and hemoglobin values at which drawing blood for research purposes should be terminated. Investigators should also be noting the number of studies in which children are enrolled, in order to minimize blood drawing anemia states. Another method to minimize blood loss in children with a closed intravenous catheter system, in which blood is to be removed, is to re-infuse the “waste” from the indwelling catheter, provided that the “waste” is kept sterile and the practitioner has followed the institutional policy for re-infusion of such “waste” blood from an indwelling intravenous (peripheral and/or central) catheter. For policies regarding peripheral intravenous therapy in the pediatric subject, the YNHH Policy for Peripheral Intravenous Therapy may be consulted at http://intranet/ynhh/policies/CPM/homepage.html. Blood amounts may be further minimized by combining the need for pharmacokinetic and safety data with pharmacodynamic data (drug studies), the use of sensitive assays, use of pediatric specific laboratories, and population pharmacokinetic approaches. With this in mind, if it would be detrimental for the child to be enrolled in more than one study for blood drawing reasons, other safety reasons, or due to confounding scientific validity, this should be explicitly stated in the protocol and monitored for by the investigator and study staff. Version date Page 16 of 35 Pediatric Template HIC# if known If you will monitor the patient for certain side/adverse effects, explain how this will be done and any stopping rules for either the intervention or the research procedure. For example, it should always be noted that if children need a break from testing one will be provided; if children want to stop a procedure at any time, it will be stopped; if children want to be removed from a scanner/MRI, they will be removed. With regard to MRI scanning or any procedure in which minors need to be still, the method for keeping children quiet and/or still should be noted, as necessary. If this involves sedation, the method for the sedation should be clearly explained, with how the child will be monitored and any other necessary precautions. Utilize the “YNHH Policy for Sedation/Analgesia for Diagnostic and Surgical Procedures Multi-Disciplinary Protocol” when explaining the monitoring and precautions. A copy of the policy may be obtained from the Yale-New Haven Hospital, Clinical Administrative Policy and Procedure Manual” located on the YNHH clinical work station. Clinical problems not previously known to the parent/subject and communication with other care providers (pediatricians, etc): If there are tests or procedures that are completed as part of the research that are appropriate for clinical care (diagnostic or treatment use), the plan to communicate these results to the caregiver (parents) and health care providers should be noted in the HIC application and in the parental permission form. If these tests or procedures are purely for research purposes, but could indicate a clinical problem, then the plan to notify the family/care givers should be noted with the provisions for re-testing or referral to the appropriate provider noted. An example of this wording may be found in the MRRC templates: This MR study is for research purposes only and is not in any way a clinical examination. The scans performed in this study are not designed to find abnormalities. The primary investigator, the lab, the MR technologist, and the Magnetic Resonance Research Center are not qualified to interpret the MR scans and are not responsible for providing a diagnostic evaluation of the images. If a worrisome finding is seen on your child’s scan, a radiologist or another physician will be asked to review the relevant images. Based on his or her recommendation (if any), the primary investigator or consulting physician will contact you, inform you of the finding, and recommend that you seek medical advice as a precautionary measure. The decision for additional examination or treatment would lie solely with you and your child’s physician. The investigators, the consulting physician, the Magnetic Resonance Research Center, and Yale University are not responsible for any examination or treatment that your child receives based on these findings. The images collected in this study are not a clinical MR exam and for that reason, they will not be made available for diagnostic purposes. 11. Data and Safety Monitoring Plan: Include an appropriate Data and Safety Monitoring Plan (DSMP) based on the investigator’s risk assessment stated below. (Note: the HIC will make the final determination of the risk to subjects.) For more information, see the Instructions, page 24. a. What is the investigator’s assessment of the overall risk level for subjects participating in this study? b. If children are involved, what is the investigator’s assessment of the overall risk level for the children participating in this study? Version date Page 17 of 35 Pediatric Template c. HIC# if known Copy and paste, and then tailor an appropriate Data and Safety Monitoring Plan from http://www.yale.edu/hrpp/forms-templates/biomedical.html for i. Minimal risk ii. Greater than minimal/moderate risk iii. High risk There are 4 possible risk assessments for children participating in pediatric studies, according to The Code of Federal Regulations, Title 45, Volume I, Subpart D-Additional Protections for Children Involved as Subjects in Research: (1) 45 CFR 46.404: Research not involving greater than minimal risk (2) 45 CFR 46.405: Research involving greater than minimal risk, but presenting the prospect of direct benefit to individual subjects (3) 45 CFR 46.406: Research involving greater than minimal risk and no prospect of direct benefit to individual subjects, but likely to yield generalizable knowledge about the subject’s disorder or condition. 45 CFR 46.407: Research not otherwise approvable which presents an opportunity to understand, prevent, or alleviate a serious problem affecting the health or welfare of children. HHS will conduct or fund research that the IRB does not believe meets the requirements of Sec. 46.404, Sec. 46.405, or Sec. 46.406 only if: A. The IRB finds that the research presents a reasonable opportunity to further the understanding, prevention, or alleviation of a serious problem affecting the health or welfare of children; and B. The Secretary of DHHS (Department of Health and Human Services) after consultation with a panel of experts in pertinent disciplines (for e.g., science, medicine, education, ethics, law) and following opportunity for public review and comment, has determined that certain conditions have been met and the research may be approvable. (See 45 CFR 46.407 for further information.) There are analogous risk determinations in the Federal Drug Administration Regulations for children participating in pediatric studies (that involve test articles such as investigational drugs, devices, and any other articles regulated by the FDA), according to Subpart D Additional Safeguards for Children in Clinical Investigations of Title 21Food and Drugs, Chapter I-Food and Drug Administration, Department of Health and Human Services, Part 50 Protection of Human Subjects. These may be found at http://www.accessdata.fda.gov/SCRIPTs/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=5 0&showFR=1&subpartNode=21:1.0.1.1.19.4 The Data and Safety Monitoring Plan should include a plan to terminate the study should an unexpected hazard be identified. Data and Safety Monitoring Boards: It is recommended (AAPGuidelines, 2010) that an independent data and safety monitoring committee or board be created for all Phase III Version date Page 18 of 35 Pediatric Template HIC# if known drug/test article trials conducted in children. A data and safety monitoring committee or board may be necessary as well for some Phase I and II trials, especially those that include blinding. In Phase I and II trials with a DSMB/C, a robust data monitoring plan must be in place. Utilize the DSMP template examples at http://www.yale.edu/hrpp/resources/docs/420FR1DSMPTemplate.pdf as per the risk assessment. The moderate risk template may be used for those protocols that are deemed greater than minimal risk. Especially note the language with regard to the reporting of serious adverse events to the HIC: (This is only one part of the DSMP. Utilize the entire template (as appropriate to the level of risk of your protocol) located on the HRPP website at: http://www.yale.edu/hrpp/resources/docs/HICProtocol_Application_Instructions02-1210.doc) Plan for reporting serious AND unanticipated AND related adverse events, anticipated adverse events occurring at a greater frequency than expected, and other unanticipated problems involving risks to subjects and others to HIC: The investigator will report the following types of adverse events to HIC: a) serious AND unanticipated AND possibly, probably, or definitely related events; b) anticipated adverse events occurring with greater frequency than expected; and c) other unanticipated problems involving risks to subjects or others. d. For multi-site studies for which the Yale PI serves as the lead investigator: ii. How will adverse events and unanticipated problems involving risks to subjects or others be reported, reviewed and managed? iii. What provisions are in place for management of interim results? iv. What will the multi-site process be for protocol modifications? 12. Statistical Considerations: Describe the statistical analyses that support the study design. In particular, sample size justification, proposed analyses for your primary and secondary outcomes (including adverse events, if possible), and considerations for missing values should be included. Outcomes should be meaningful and measurable, with adequate control or normative data for comparison and there should be appropriate power analysis to ensure enrollment of an adequate number of subjects to answer the research question. For complex statistical elements of study design and/or assistance with pilot study design in which preliminary data may be limited, you may find it useful to contact the Yale Center for Analytical Sciences (YCAS) at ycas@yale.edu. Version date Page 19 of 35 Pediatric Template HIC# if known SECTION VI: RESEARCH INVOLVING DRUGS, BIOLOGICS, PLACEBOS AND DEVICES If a drug/substance is being used in a study and it is NOT approved by the FDA for minors (children or adolescents), indicate the IND number(s) below and answer the questions 1.a and 1.b. If the drug being studied is FDA approved, then indicate this and the indication for the use of the drug/device in this section. If you or the sponsor have not filed for an IND with the FDA and you are not planning to file for an IND, complete the appropriate exemption information below. If the study does not meet the criteria indicated in the exemption categories below, then an IND may be indicated. The IRB (HIC) will determine whether application for an IND is necessary. A. DRUGS and BIOLOGICS 1. Identification of Drug or Biologic: What is (are) the name(s) of the drug(s) or biologic(s) being used? Identify whether FDA approval has been granted and for what indication(s). All protocols which utilize a drug or biologic not approved by, but regulated by, the FDA must provide the following information: What is the Investigational New Drug (IND) number assigned by the FDA? Who holds the IND? All protocols which utilize a radiotracer not approved by, but regulated by the FDA must provide the IND number: _______________ Alternatively, use of the investigational radiotracer may be under RDRC/RSC oversight: (check if appropriate)_____________ For all investigational radiotracers, attach a copy of the RDRC/RSC application ( for radioisotopes used in the PET Center, PET Center personnel may complete this step) Go to http://rsc.med.yale.edu/login.asp?url=myApps.asp. When you have logged in, complete the application and attach a copy to this submission Alternatively, an exemption from IND filing requirements may be sought for a clinical investigation of a drug product that is lawfully marketed in the United States. If there is no IND and an exemption is being sought, review the following categories and complete the category that applies (and delete the inapplicable categories): Exempt Category 1 The clinical investigation of a drug product that is lawfully marketed in the United States can be exempt from IND regulations if all of the following are yes: i. The intention of the investigation is NOT to report to the FDA as a well-controlled study in support Version date Page 20 of 35 Pediatric Template HIC# if known of a new indication for use or to be used to support any other significant change in the labeling for the drug. Yes No ii. The drug that is undergoing investigation is lawfully marketed as a prescription drug product, and the intention of the investigation is NOT to support a significant change in the advertising for the product. Yes No iii. The investigation does NOT involve a route of administration or dosage level or use in populations or other factor that significantly increases the risks (or decreases the acceptability of the risks) associated with the use of the drug product. Yes No iv. The investigation will be conducted in compliance with the requirements for institutional (HIC) review and with the requirements for informed consent of the FDA regulations (21 CFR Part 50 and 21 CFR Part 56). Yes No v. The investigation will be conducted in compliance with the requirements regarding promotion and charging for investigational drugs. Yes No Exempt Category 2 (all items i, ii, and iii must be checked to grant a category 2 exemption) i. The clinical investigation is for an in vitro diagnostic biological product that involves one or more of the following (check all that apply): Blood grouping serum Reagent red blood cells Anti-human globulin ii. The diagnostic test is intended to be used in a diagnostic procedure that confirms the diagnosis made by another, medically established, diagnostic product or procedure; and iii. The diagnostic test is shipped in compliance with 21 CFR §312.160. Exempt Category 3 The drug is intended solely for tests in vitro or in laboratory research animals if shipped in accordance with 21 CFR 312.60 Exempt Category 4 A clinical investigation involving use of a placebo if the investigation does not otherwise require submission of an IND. 2. Background Information: Provide a description of previous human use, known risks, and data addressing dosage(s), interval(s), route(s) of administration, and any other factors that might influence risks. If this is the first time this drug is being administered to humans, include relevant data on animal models. Include any previous studies in minors (children or adolescents), if they exist. If no studies have been done with minors, indicate this. Be clear about how this substance will be used in minors, e.g. “the first time the substance will be given by this route for this particular indication,” or “the first time it will be given in minors altogether.” Include the pediatric dose per unit of measure, e.g. dose per kg or dose per m 2. Justify the dose if it is not computed via such a measure. Version date Page 21 of 35 Pediatric Template HIC# if known 3. Source: a) Identify the source of the drug or biologic to be used. b) Is the drug provided free of charge? If yes, by whom? Yes No 4. Storage, Preparation and Use: Describe the method of storage, preparation, stability information, and for parenteral products, method of sterilization and method of testing sterility and pyrogenicity. Note: If the YNHH IDS (or comparable service at CMHC or WHVA) will not be utilized, explain in detail how the PI will oversee these aspects of drug accountability, storage, and preparation. Check applicable Investigational Drug Service utilized: YNHH IDS Yale Cancer Center CMHC Pharmacy West Haven VA PET Center None Other: Note: If the YNHH IDS (or comparable service at CMHC or WHVA) will not be utilized, explain in detail how the PI will oversee these aspects of drug accountability, storage, and preparation. 5. Use of Placebo: Not applicable to this research project Provide a justification which addresses the following: a. Describe the safety and efficacy of other available therapies (if any). b. State the maximum total length of time a participant may receive placebo while on the study. c. Address the greatest potential harm that may come to a participant as a result of not receiving effective therapy (immediate or delayed onset.) d. Describe the procedures that are in place to safeguard participants receiving placebo. Fully describe the conditions of placebo use and provide the justification as noted above. It is necessary to understand the use of placebo in minors to further assess risk in this population. The risk to subjects from the placebo arm should be minimized. The conditions under which placebos may be ethically used in children are as follows: 1. When there is no commonly accepted therapy for the condition and the agent/test article under study is the first one that may modify the course of the disease process. 2. When the commonly used therapy is of questionable efficacy; 3. When the commonly used therapy for the condition carries with it a high frequency of undesirable adverse effects and the risks may be significantly greater than the benefits; 4. When the placebo is used to identify incidence and severity of adverse effects produced by adding a new treatment to an established regimen; or 5. When the disease process is characterized by frequent, spontaneous exacerbations and remissions and the efficacy of the therapy has not been demonstrated. These conditions, as applicable to the plan of study, should be included in the HIC application. 6. Use of Controlled Substances: Will this research project involve the use of controlled substances in human subjects? Version date Page 22 of 35 Pediatric Template Yes HIC# if known No See HIC Application Instructions to view controlled substance listings. If yes, is the use of the controlled substance considered: Therapeutic: The use of the controlled substance, within the context of the research, has the potential to benefit the research participant. Non Therapeutic: Note, the use of a controlled substance in a non therapeutic research study involving human subjects may require that the investigator obtain a Laboratory Research License. Examples include controlled substances used for basic imaging, observation or biochemical studies or other non-therapeutic purposes. Note, the use of a controlled substance in a non-therapeutic research study involving human subjects may require that the investigator obtain a Laboratory Research License. Examples include controlled substances used for basic imaging, observation or biochemical studies or other non-therapeutic purposes. See HIC Application Instructions for further information. 7. Continuation of Drug Therapy After Study Closure Not applicable to this project Are subjects provided the opportunity to continue to receive the study drug(s) after the study has ended? Yes If yes, describe the conditions under which continued access to study drug(s) may apply as well as conditions for termination of such access. No If no, explain why this is acceptable. Respond to this section. Especially for conditions for which there are no established FDAapproved therapies for children, it is important for the reviewer to know if a therapy that works may be continued and if not, why not, or what other options may or may not be available to the child/parents. B. DEVICES If the device being studied is FDA approved, then indicate this and the indication for the use of the device in question 2. If a device is being used in the study and it is NOT approved by the FDA for minors (children or adolescents), indicate the IDE number(s) below and answer the question 3. If you or the sponsor have not filed for an IDE with the FDA and you are not planning to file for an IDE, complete the appropriate exemption information below in question 6. If the study does not meet the criteria indicated in the exemption categories below, then an IDE may be indicated. The IRB (HIC) will determine whether application for an IDE is necessary. 1. Are there any investigational devices used or investigational procedures performed in a YNHH Operating Room? Yes No If Yes, please be aware of the following requirements: a. A YNHH OR New Product/Trial Request Form must be completed. Please contact the OR Materials Manager, Chris Baillargeon, at 203-688-8912 for more information on this requirement; b. Your request must be reviewed and approved by the Operating Room New Technology Committee before patients may be scheduled; and Version date Page 23 of 35 Pediatric Template HIC# if known c. The notice of approval from the OR New Technology Committee must be submitted to the HIC for the protocol file. Please contact Gina D’Agostino, gina.d’agostino@ynhh.org or 688-5210, to initiate the process. 2. What is the name of the device to be studied in this protocol? Has this device been FDA approved? If yes, state for what indication. Yes No 3. Background Information: Provide a description of previous human use, known risks, and any other factors that might influence risks. If this is the first time this device is being used in humans, include relevant data on animal models. Include any previous studies in minors (children or adolescents), if they exist. If no studies have been done with minors, indicate this. Be clear about how this device will be used in minors, e.g. “the first time the device will be used for this particular indication,” or “the first time it will be used in minors altogether.” If this is a device to be used in the pediatric population and the sponsor or PI has not filed for an IDE because the sponsor states that the device is substantially equivalent or is already approved in another country for an indication that may meet Class I (General Controls, e.g. elastic bandages, surgical instruments) or Class II designation (e.g. infusion pumps, specific types of imaging machines, etc.) provide enough information about the device in the background section for the HIC to make a determination of significant vs. non-significant risk. (In some instances, the risk determination may need to be referred to the FDA, but this will give the HIC an initial understanding.) The HIC will determine whether or not the device presents non-significant risk to subjects. 4. Source: a) Identify the source of the device to be used . b) Is the drug provided free of charge? If yes, by whom? Yes No 5. What is the PI’s assessment of risk level (significant or non-significant) associated with the use of the device? Significant Risk (SR) Device Study: A study of a device that presents a potential for serious risk to the health, safety, or welfare of a participant and 1) is intended as an implant; 2) is used in supporting or sustaining human life; or otherwise prevents impairment of human health; 3) is of substantial importance in diagnosing, curing, mitigating or treating disease, or otherwise prevents impairment of human health; or 4) otherwise presents a potential for serious risk to the health, safety, or welfare of a participant. Significant Risk Devices require an Investigational Device Exemption (IDE) issued by the FDA. Version date Page 24 of 35 Pediatric Template HIC# if known a. What is the IDE number assigned by the FDA? b. Did the FDA approve this IDE as Category A (experimental/investigational) or as Category B (non-experimental/investigational)? c. Who holds the IDE? Non-Significant Risk (NSR) Device Study: A study of a device that does not meet the definition for a significant risk device and does not present a potential for serious risk to the health, safety, or welfare of participants. Note that if the HIC concurs with this determination, an IDE is not required. 6. Abbreviated or Exempt IDE: There are abbreviated requirements for an IDE and there also are exemptions to the requirement for an IDE. See the criteria in the HIC Application Instructions, Section VI.B.4 at http://www.yale.edu/hrpp/forms-templates/biomedical.html to determine if these pertain to this study. Abbreviated IDE or Exempt IDE – If criteria set forth in the HIC Application Instructions are met, copy and paste the completed relevant section from the Instructions into this application. 7. Investigational device accountability State how the PI, or named designee, ensures that an investigational device is used only in accordance with the research protocol approved by the HIC, and maintains control of the investigational device as follows: a. Maintains appropriate records, including receipt of shipment, inventory at the site, dispensation or use by each participant, and final disposition and/or the return of the investigational device (or other disposal if applicable): b. Documents pertinent information assigned to the investigational device (e.g., date, quantity, batch or serial number, expiration date if applicable, and unique code number): c. Stores the investigational device according to the manufacturer's recommendations with respect to temperature, humidity, lighting, and other environmental considerations: d. Ensures that the device is stored in a secure area with limited access in accordance with applicable regulatory requirements: e. Distributes the investigational device to subjects enrolled in the IRB-approved protocol: SECTION VII: RECRUITMENT/CONSENT/ ASSENT 1. Targeted Enrollment: Give the number of subjects: a. targeted for enrollment at Yale for this protocol___ Version date Page 25 of 35 Pediatric Template HIC# if known b. If this is a multi-site study, give the total number of subjects targeted across all sites___ 2. Indicate recruitment methods below. Attach copies of any recruitment materials that will be used. Flyers Posters Letter Medical Record Review Departmental/Center Newsletters YCCI Recruitment Database Other (describe): Internet/Web Postings Radio Mass E-mail Solicitation Telephone Departmental/Center Website Television Departmental/Center Research Boards Newspaper Web-Based Clinical Trial Registries Clinicaltrials.gov Registry (do not send materials to HIC) 3. Recruitment Procedures: a. Describe how potential subjects will be identified. b. Describe how potential subjects are contacted. c. Who is recruiting potential subjects? Strategies should be included for dealing with potential problems of recruitment and retention. There needs to be a sufficient number of subjects to answer the research question. 4. Screening Procedures: A. Will email or telephone correspondence be used to screen potential subjects for eligibility prior to the potential subject coming to the research office? Yes No B. If yes, identify any health information and check off any of the following HIPAA identifiers to be collected and retained by the research team during this screening process. If you have answered yes to this question, complete question 9, Request for HIPAA waiver. HEALTH INFORMATION TO BE COLLECTED: HIPAA identifiers: Names All geographic subdivisions smaller than a State, including: street address, city, county, precinct, zip codes and their equivalent geocodes, except for the initial three digits of a zip code if, according to the current publicly-available data from the Bureau of the Census: (1) the geographic unit formed by combining all zip codes with the same three initial digits contains more than 20,000 people, and (2) the initial three digits of a zip code for all such geographic units containing 20,000 or fewer people is changed to 000. Telephone numbers Fax numbers E-mail addresses Social Security numbers Medical record numbers Health plan beneficiary numbers Account numbers Version date Page 26 of 35 Pediatric Template HIC# if known All elements of dates (except year) for dates related to an individual, including: birth date, admission date, discharge date, date of death, all ages over 89 and all elements of dates (including year) indicative of such age, except that such ages and elements may be aggregated into a single category of age 90 or older Certificate/license numbers Vehicle identifiers and serial numbers, including license plate numbers Device identifiers and serial numbers Web Universal Resource Locators (URLs) Internet Protocol (IP) address numbers Biometric identifiers, including finger and voice prints Full face photographic images and any comparable images Any other unique identifying numbers, characteristics, or codes 5. Assessment of Current Health Provider Relationship for HIPAA Consideration: Does the Investigator or any member of the research team have a direct existing clinical relationship with any potential subject? Yes, all subjects Yes, some of the subjects No If yes, describe the nature of this relationship. If you choose any other response, than “Yes, all subjects,” consider how recruitment will take place. Consider how you will know/gain access to the Personal Health Information (PHI) of the subjects, as needed, for recruitment. If subjects will refer themselves to the study via posters or flyers, then this is not an issue. If a study team member is not the treating clinician and will initiate contact with potential participant, then consider filling out no. 9, entitled, “Request for waiver of HIPAA authorization.” 6. Request for waiver of HIPAA authorization: (When requesting a waiver of HIPAA Authorization for either the entire study, or for recruitment purposes only. Note: if you are collecting PHI as part of a phone or email screen, you must request a HIPAA waiver for recruitment purposes.) Choose one: For entire study: ______ For recruitment purposes only: ______ i. Describe why it would be impracticable to obtain the subject’s authorization for use/disclosure of this data; ii. If requesting a waiver of signed authorization, describe why it would be impracticable to obtain the subject’s signed authorization for use/disclosure of this data; By signing this protocol application, the investigator assures that the protected health information for which a Waiver of Authorization has been requested will not be reused or disclosed to any person or entity other than those listed in this application, except as required by law, for authorized oversight of this research study, or as specifically approved for use in another study by an IRB. Researchers are reminded that unauthorized disclosures of PHI to individuals outside of the Yale HIPAA-Covered entity must be accounted for in the “accounting for disclosures log”, by subject name, purpose, date, recipients, and a description of information provided. Logs are to be forwarded to the Deputy HIPAA Privacy Officer. Version date Page 27 of 35 Pediatric Template HIC# if known 7. Required HIPAA Authorization: If the research involves the creation, use or disclosure of protected health information (PHI), separate subject authorization is required under the HIPAA Privacy Rule. Indicate which of the following forms are being provided: Compound Consent and Authorization form HIPAA Research Authorization Form 8. Consent Personnel: List the names of all members of the research team who will be obtaining consent/assent. 9. Process of Consent/Assent: Describe the setting and conditions under which consent/assent will be obtained, including parental permission or surrogate permission and the steps taken to ensure subjects’ independent decision-making. Parents of children can only provide “permission” for their minor child. Only an individual with full decision-making capacity can give consent for him/herself. According to the American Academy of Pediatrics criteria, children > 7 years of age may provide written assent. Children younger than 7 years of age should provide verbal assent for participation, as developmentally appropriate. See Section VII, no. 3 Inclusion/Exclusion Criteria: Children, for a full list of those considerations for Children. A parent is defined as a child’s biological or adoptive parent, and a guardian is defined as an individual who is authorized under applicable state law to consent on behalf of a child to general medical care. As appropriate to the protocol, the clarification of legal guardianship may need to be elucidated. If the investigator or consenting personnel has reason to believe that the legal guardianship of the person signing consent is at issue, possible methods of verification include: (a) child’s birth certificate to establish biological parents; (b) divorce decree to establish custody; (c) court order which may validate a transfer of legal guardianship to a relative or transfer custody to another entity such as DCF; (d) calling the court. If the legal guardianship cannot be established, then it may be advisable to state that in these instances, the child will not be enrolled in the study. Foster parents cannot provide consent for foster children to participate in research, because they are not considered their legal guardians. However, foster parent(s) may need to be consulted with as the research may require their commitment; for example, driving the child to and from research appointments. Refer to 45CFR46.406 at http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm#46.406 with regard to the adequate provisions for obtaining permission of parents when research is deemed to be greater than minimal risk and no prospect of benefit to individual subjects, but likely to yield generalizable knowledge about the subject’s disorder or condition. Where the research is covered under Sec. 46.406 and permission is to be obtained from parents, both parents must give their permission unless one parent is deceased, unknown, incompetent, or not reasonably available, or when only one parent has legal responsibility for the care and custody of the child. Version date Page 28 of 35 Pediatric Template HIC# if known Finally, consider whether or not the child will remain in the study once he/she reaches the age of majority (18 years). If yes, then describe the process of obtaining the consent of the young adult to continue participation (or allow continued use of his/her study information/sample(s), especially applicable to repository studies or those studies in which samples are requested to be used for future research) in this study. 10. Evaluation of Subject(s) Capacity to Provide Informed Consent/Assent: Indicate how the personnel obtaining consent will assess the potential subject’s ability and capacity to consent to the research being proposed. Explain how you will assess the decision making capacity of parents and children. Parents should be free of duress enough to be able to give permission for their minor child to participate in the proposed study. If you will enroll children who are less than 7 years of age (the youngest “intellectual” age for which written assent is recommended by the American Academy of Pediatrics), you do not need an assent form. Also explain any special circumstances in which it might be justified for children (> 7 years) not to provide a written assent. For example, if you will enroll children with severe autism and it is assessed that even though they are above the chronological age of 7 years, they will be developmentally incapable of providing assent, this should be explained in this section. Another example might be children who are hospitalized in the Pediatric Intensive Care Unit. They will not be able to assent for themselves, but parents should be able to give permission (unless they are under too much emotional distress.) In addition to limited intellectual capabilities, the IRB may also waive the provision of assent if the intervention or procedure involved in the research holds out the prospect of direct benefit to the health or well being of the child and is available only in the context of the research, e.g. some chemotherapy protocols, or if the research meets the same conditions as those for waiver or alteration of consent in research involving adults. In the case of parents who may be under duress due to their child’s emergent hospital admission or surgery, etc., the option of asking the parent to provide permission prior to the “index” event is acceptable or at any other time that the parent is not considered to be under stress. For example, children with sickle cell that may have frequent vaso-occlusive crisis. Perhaps parents can provide permission at a routine clinic visit and then the permission can be verified or confirmed with the parent when the hospitalization occurs. The same may hold true for elective surgeries, etc. It is preferable for parents to give permission when they have the time to review the permission form and to understand all study procedures, risks, and benefits. For research in which the researcher cannot anticipate the “index” or the “stressful” event, it is possible to do the research, if conditions for seeking permission are justified. It is important for the study team to acknowledge the parent’s emotional state, lack of medical knowledge, and inexperience with clinical trials. During the consent process (and throughout the trial), research staff need to educate parents about the child’s disease and how clinical trials work. Potential risks should be enumerated and described without overstating benefits. Version date Page 29 of 35 Pediatric Template HIC# if known 11. Documentation of Consent/Assent: Specify the documents that will be used during the consent/assent process. Copies of all documents should be appended to the protocol, in the same format that they will be given to subjects. If you will enroll participants who are 18 years or older, include a Compound Authorization and Consent Form or a Consent Form and a HIPAA Authorization Form. For minors, include a Compound Authorization and Parental Permission Form or a Parental Permission Form and a HIPAA Authorization Form. If you will include all minors capable of providing assent, i.e. 7 years to 17 years of age, include 2 assent forms: One assent form should be developed for children ages 7 to 12 years of age and a separate assent form developed for adolescents 13 to 17 years of age. The form for 13 year olds generally includes pregnancy/contraception precautions and drug use precautions as necessary for your study. If you are enrolling a smaller span of ages, then one assent form may be considered developmentally appropriate. All forms should be written according to the grade level of the above age groups. If only children younger than 7 years of age will participate or it is assessed that the children who are participating will not be able to provide written assent, then only a Compound Authorization and Parental Permission Form or a Parental Permission Form and HIPAA Research Authorization Form may be provided. Include an explanation of this fact in the section above entitled, “Evaluation of Subject(s) Capacity to Provide Informed Consent/Assent.” For example, if you will enroll children with severe autism and it is assessed that even though they are above the chronological age of 7 years, they will be developmentally incapable of providing assent, this should be explained in this section. See also the Application to Involve Human Subjects in Research Instructions in Biomedical Research (http://www.yale.edu/hrpp/formstemplates/biomedical.html ) for further information about parental permission and assent. 12. Non-English Speaking Subjects: Explain provisions in place to ensure comprehension for research involving non-English speaking subjects. Translated copies of all consent materials must be submitted for approval prior to use. If you will not include Non-English speaking families, i.e., usually families whose primary language is Spanish, provide a justification for this decision here. 13. Consent Waiver: In certain circumstances, the HIC may grant a waiver of signed consent, or a full waiver of consent, depending on the study. If you will request either a waiver of consent, or a waiver of signed consent for this study, complete the appropriate section below. Not Requesting a consent waiver Requesting a waiver of signed consent Version date Page 30 of 35 Pediatric Template HIC# if known Requesting a full waiver of consent A. Waiver of signed consent: (Verbal consent from subjects will be obtained. If PHI is collected, information in this section must match Section VII, Question 6) Requesting a waiver of signed consent for Recruitment/Screening only If requesting a waiver of signed consent, please address the following: a. Would the signed consent form be the only record linking the subject and the research? Yes No b. Does a breach of confidentiality constitute the principal risk to subjects? Yes No OR c. Does the research activity pose greater than minimal risk? Yes If you answered yes, stop. A waiver cannot be granted. Please note: Recruitment/screening is generally a minimal risk research activity. No AND d. Does the research include any activities that would require signed consent in a nonresearch context? Yes No Requesting a waiver of signed consent for the Entire Study (Note that an information sheet may be required.) If requesting a waiver of signed consent, please address the following: a. Would the signed consent form be the only record linking the subject and the research? Yes No b. Does a breach of confidentiality constitute the principal risk to subjects? Yes No OR c. Does the research pose greater than minimal risk? Yes If you answered yes, stop. A waiver cannot be granted. No AND d. Does the research include any activities that would require signed consent in a nonresearch context? Yes No B. Full waiver of consent: (No consent from subjects will be obtained.) Requesting a waiver of consent for Recruitment/Screening only a. Does the research activity pose greater than minimal risk to subjects? Yes If you answered yes, stop. A waiver cannot be granted. Please note: Recruitment/screening is generally a minimal risk research activity No b. Will the waiver adversely affect subjects’ rights and welfare? Yes No c. Why would the research be impracticable to conduct without the waiver? d. Where appropriate, how will pertinent information be returned to, or shared with subjects at a later date? Version date Page 31 of 35 Pediatric Template HIC# if known Requesting a full waiver of consent for the Entire Study (Note: If PHI is collected, information here must match Section VII, question 6.) If requesting a full waiver of consent, please address the following: a. Does the research pose greater than minimal risk to subjects? Yes If you answered yes, stop. A waiver cannot be granted. No b. Will the waiver adversely affect subjects’ rights and welfare? Yes No c. Why would the research be impracticable to conduct without the waiver? d. Where appropriate, how will pertinent information be returned to, or shared with subjects at a later date? Note: parental permission may not be modified or waived, under federal regulations, in protocols that involve an FDA-regulated product. There are two situations in which parental permission may be modified or waived. These include: (a) research that involves only minimal risk, does not negatively affect the welfare of subjects, and cannot be practically performed without the waiver; (b) research in which obtaining permission will not function to protect the child. The IRB may determine and PPRC may agree that the protocol is designed for conditions or a specific population for which parental permission or guardian permission is not a reasonable requirement to protect the subjects, e.g. neglected or abused children. This situation is conditional, provided that an appropriate mechanism for protecting the children who are targeted for participation is substituted, and the waiver is not inconsistent with federal, state, or local law. If you are asking for a waiver of signed consent, note that “Information Sheets” as noted above (in the documentation of consent section) for the parent/subject/minors are needed. Include their provision in the section (above) and also include these forms with your PPRC submission. [They basically follow the same format as consent/permission or assent forms, but do not include a signature page.] The only waiver of parental permission that the FDA considers is for research involving emergent and life-threatening situations. Waivers of permission for emergency research with minors may be granted when the following conditions are met: (All applicable conditions need to be explained in this HIC application.) 1. Patients must have specific life-threatening medical conditions and the family/parents are not available to provide informed consent or permission. 2. The research must hold out the prospect of individual benefit to the subject. 3. The minor must have a life-threatening condition for which available treatments are unproven or unsatisfactory. 4. For the treatment to be effective, it must be initiated before consent/permission can be obtained by the subject’s parent, guardian, or legally authorized representative. 5. An IND or an IDE is required. 6. The sponsor of the study must have received written authorization from the FDA. 7. The IRB needs to document that these specific conditions have been met. Version date Page 32 of 35 Pediatric Template HIC# if known 8. The development and implementation of a plan for community consultation and public disclosure before the start of the study. 9. A mechanism for contacting and providing information to the subject’s legally authorized representative or family member/parent within the therapeutic window or at the earliest feasible opportunity. 10. Opportunity for family members/parents to object to a subject’s continued participation in the study. SECTION VIII: PROTECTION OF RESEARCH SUBJECTS Confidentiality & Security of Data: a. What protected health information (medical information along with the HIPAA identifiers) about subjects will be collected and used for the research? b. How will the research data be collected, recorded and stored? c. How will the digital data be stored? CD DVD Flash Drive Portable Hard Drive Secured Server Laptop Computer Desktop Computer Other d. What methods and procedures will be used to safeguard the confidentiality and security of the identifiable study data and the storage media indicated above during and after the subject’s participation in the study? Do all portable devices contain encryption software? Yes No e. What will be done with the data when the research is completed? Are there plans to destroy the identifiable data? If yes, describe how, by whom and when identifiers will be destroyed. If no, describe how the data and/or identifiers will be secured. f. Who will have access to the protected health information (such as the research sponsor, the investigator, the research staff, all research monitors, FDA, Yale Cancer Center Data and Safety Monitoring Committee (DSMC), SSC, etc.)? (please distinguish between PHI and deidentified data) g. If appropriate, has a Certificate of Confidentiality been obtained? h. Are any of the study procedures likely to yield information subject to mandatory reporting requirements? (e.g. HIV testing – reporting of communicable diseases; parent interview incidents of child abuse, elderly abuse, etc.). Please verify to whom such instances will need to be reported. If by state statute you belong to a profession (e.g. physicians, nurses, social workers), that is considered a mandatory reporter of abuse and/or neglect (child, domestic, elderly) and/or a reporter of communicable diseases in the State of CT, then the answer to this question is that you will report these incidences to the proper authorities, even though in some studies this may be a rare occurrence or an incidental finding. SECTION IX: POTENTIAL BENEFITS Potential Benefits: Identify any benefits that may be reasonably expected to result from the research, either to the subject(s) or to society at large. (Payment of subjects is not considered a benefit in this context of the risk benefit assessment.) Clearly state the benefit of the research and/or the research procedures/assessments/tests to the individual subject or to the population at large Version date Page 33 of 35 Pediatric Template HIC# if known either at present or in the future. The benefit statement should be consistent in all documents, internally in the HIC application and match with the parental permission/consent/assents. Especially for studies of greater than minimal risk, it is important to be clear if the individual subject will benefit or if the population at large (that the subject belongs to) will benefit. SECTION X: RESEARCH ALTERNATIVES AND ECONOMIC CONSIDERATIONS 1. Alternatives: What other alternatives are available to the study subjects outside of the research? If this is a study providing any type of treatment, list what alternatives are available to parents/minors. Other alternatives, as appropriate to your study, may include: (1) other research protocols if similar ones are offered at this site; (2) the intervention may be provided as standard of care (outside of the protocol, e.g. an FDA approved drug, if applicable). If not a treatment study or the other alternatives as noted above do not apply, then the option may simply be not to participate. 2. Payments for Participation (Economic Considerations): Describe any payments that will be made to subjects, the amount and schedule of payments, and the conditions for receiving this compensation. If there are separate payments for parents and children, explain this here and in the parental permission documents. If there is only one payment or gift, etc, indicate to whom this payment will be given. For an example, consider the following: a gift certificate to a music or book store for the adolescent and money for transportation given to the parent/guardian. The American Academy of Pediatrics (2010) advises that payments are to be reasonable and minimal to either the child or the parent. The IRB must be certain and the PPRC may advise as to whether the payment is fair and does not become an undue inducement for participation of the child. 3. Costs for Participation (Economic Considerations): Clearly describe the subject’s costs associated with participation in the research, and the interventions or procedures of the study that will be provided at no cost to subjects. Differentiate those procedures/tests/assessments that are standard of care and will be billed to parent’s insurance versus those procedures that are research related and will be paid for by the study. This should also be consistent and clear in the parental permission and/or consent form (depending upon the ages to be enrolled.) Any potential financial costs should also be outlined for parents. 4. In Case of Injury: This section is required for any research involving more than minimal risk. a. Will medical treatment be available if research-related injury occurs? b. Where and from whom may treatment be obtained? Version date Page 34 of 35 Pediatric Template c. d. e. HIC# if known Are there any limits to the treatment being provided? Who will pay for this treatment? How will the medical treatment be accessed by subjects? References: Blumenthal, R. (2002). Attorney General’s Opinion written to the Honorable Kristine Ragaglia, Commissioner of Children and Families. September 30, 2002, accessed from http:///www.ct.gov/ag/cwp/view.asp on April 14, 2007. Code of Federal Regulations. Subpart D Additional Safeguards for Children in Clinical Investigations of Chapter 1 Food and Drug Administration, DHHS; 21 CFR 50.51 to 21 CFR 50.54. Code of Federal Regulations, Subpart D Additional Protections for Children Involved as Subjects in Research of Title 45—Public Welfare, Subtitle A—Department of Health and Human Services, Part 46 Protection of Human Subjects, DHHS; 45 CFR 46.404 to 45 CFR 46.407 CT State Statutues. The following Sections: Section 17a-101, Section 17a-101a, Section 19a-14c, Section 46b-150. Shaddy, R. E., Denne, S.C. (2010). Clinical report guidelines for the ethical conduct of studies to evaluate drugs in pediatric populations. Pediatrics, 125, 850-860. (Pediatrics is the Official Journal of the American Academy of Pediatrics.) Version date Page 35 of 35