Document 7827686
advertisement

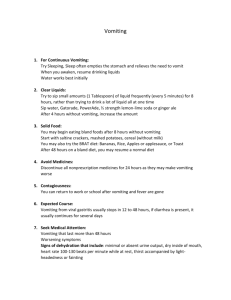
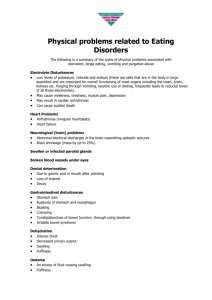
Block 8 Week 1 Mouth and oesophagus Tutor : Prof DF Wittenberg MD FCP(SA) dwittenb@medic.up.ac.za Objectives: To be able to list the causes and discuss the diagnosis and management of a sore mouth in children; know and discuss the epidemiology, aetiology, pathogenesis, pathophysiology, clinical features, diagnosis, complications and detailed management of patients with stomatitis. list and discuss causes of vomiting and regurgitation; recognize by history and examination, common and important causes of vomiting and manage them appropriately; discuss the modes of presentation, clinical features, diagnosis, management and complications of gastro-oesophageal reflux and pyloric stenosis. Illustrative Case Report 1: Mrs Y brings her 10 month old child to you for advice and management of sores in the mouth. Baby Y is a beautiful, healthy baby, growing and developing quite normally. About a month ago, Mrs Y decided to return to work and enrolled him in a day care centre, where he is being cared for together with 6 other babies in one room. It is known that one of those babies had recently been ill. Since 2 days ago, he has developed a mild fever. Yesterday he was quite ‘niggly’. He seemed to be thirsty, but when Mrs Y gave him a bottle with juice, he started to cry after a few mouthfuls and then refused to take the bottle. He seems to be drooling saliva a lot. At night, he slept very fretfully. This morning, mother saw what she thinks are sores in the mouth. On examination, he is a well-nourished febrile, unhappy miserable little boy. His lips appear a little swollen. He is salivating. On the inside of his lips, one can see irregular, very superficial ulcers with a greyish-yellow base and a thin red line surrounding them. The intervening mucosa has a normal appearance. Ulcers are seen on the lips, the inside of the buccal mucosa, the gingival margins and the tongue. The submandibular lymph nodes are enlarged and soft. There are no other abnormalities on clinical examination. Introduction The symptoms of pathology in the mouth are pain (but young babies cannot complain) salivating and drooling feed refusal after a few mouthfuls (differentiate from anorexia) dysphagia (difficulty with swallowing) a) anatomical causes (congenital or acquired obstruction) b) pain (sore mouth and throat) c) neuromuscular (paralysis, incoordination of swallowing muscles) Clinical examination of the mouth: Remember the different structures of the mouth, these need to be inspected in turn: Lips inside and out, angles of the mouth, floor of the mouth, tongue, gingivae and teeth, buccal mucosa, soft and hard palate, uvula, lateral pharyngeal wall, tonsils and the retropharyngeal lymphoid tissue. Stomatitis refers to inflammation of the buccal mucosa; if it extends onto the gingiva it is termed gingivostomatitis. Inflammmation of the buccal muccosa can arise because of Acute infection (measles, herpes, oral candidiasis, coxsackie virus infection, Vincent’s angina) Reactivation of latent infection (herpes, some recurrent acute aphthous stomatitis) Congenital skin conditions involving the oral mucosa (eg pemphigoid) Immune mechanisms (recurrent aphthous stomatitis, allergic phenomena) Inadequate healing after superficial insults (agranulocytosis, protein energy malnutrition) Trauma or chemical injury (caustic burns) Task: Read Coovadia & Wittenberg 264, 320, 667 - 672 Case Analysis and Definition of Learning Needs in Relation to Case Case Summary: 10 month old baby develops fever, followed by feed refusal and salivating a lot. Now has developed sores in the mouth. These are flat ulcers on red base with normal mucosa intervening. They occur on lips, inside mouth, on tongue and on gingival margins. The draining lymph nodes are enlarged Problems: 1. Fever 2. Stomatitis with mouth ulcers Solution: Acute onset with fever, contact with other children, one of whom known to have been ill: This suggests strongly that the patient has an infection. Mouth lesions are discrete and ulcerative rather than diffuse. Pattern suggests acute herpetic stomatitis. Herpes simplex stomatitis Herpes stomatitis Herpes simplex In severe cases of herpes stomatitis, the lesions can extend onto the outside of the lips and the cheeks. The single ulcers can coalesce to form large denuded areas which are very painful. On the outside of the lips, such flat ulcers may also become crusted and bleed. It then becomes difficult to distinguish severe herpes simplex stomatitis from other examples of bad ulcerating conditions of lips and mouth such as shown in the case of Necrotic stomatitis Acute bacterial infection of the pharynx and mouth can give a very bad sore throat. Acute tonsillitis may have just enlarged red tonsils Tonsillitis with follicles Tonsillitis without follicles or the tonsils may be covered with an exudate or with follicles of pus. In very severe cases of bacterial pharyngotonsillitis, the erythema and swelling extends beyongd the tonsils to include the whole of the retropharyngeal wall and the uvula, and a purulent membrane may be seen extending beyond the tonsils. This suggests diphtheria or staphylococcal disease. It is vital to record the immunisation status of such a patient: if there is no record of diphtheria immunisation, such a patient must be treated for diphtheria. Diphtheria Patients infected with streptococci which elaborate an erythrogenic toxin may present with scarlet fever. A flushed red face with paler appearnce of the skin around the mouth (circum-oral pallor) and a strawberry red tongue suggests the diagnosis of scarlet fever. This needs treatment with penicillin. One of the commonest conditions affecting the mouth of very young babies is oral thrush. This is a fungal condition in which the mucosa is covered by a white plaque-like covering made up of candida albicans hyphae. The mouth mucosa is inflamed, and even though the condition is not as painful as acute herpes, it does lead to pain, poor feeding, salivation. Fever is unusual unless due to another co-existing condition. White milk curds on the surface of the buccal mucosa can look a little like the candida plaque. Milk curds can however be wiped off with a spatula and show normal underlying mucosa, while wiping off the layer of thrush will expose pinpoint bleeding sites on an inflamed red mucosa. Oral Thrush A sore mouth does not have to be caused by acute infection only. Recurrent aphthous ulcers are often precipitated by an intercurrent infection and look rather similar to acute herpes simplex stomatitis. In an afebrile child, injury or chemical burns must be considered as a cause of sudden onset of painful mouth. Frenulum injury as part of non-accidental injury Task Study herpes simplex infections, oral candida, measles with Kopliks spots, Vincents angina, aphthous ulcers, agranulocytic stomatitis, mouth burns with corrosive poisons Oesophagus Task Review the anatomy and physiology of the oesophagus. Consider the integration and maturation of the nerve pathways to ensure that the swallowing muscles contract in the correct sequence to propel food content downwards. Be sure to know which muscles and nerves are involved. Review the development of swallowing in the young baby: What enables it to progress from a liquid diet to solids and how does it learn these abilities. Symptoms of the oesophagus and deglutition disorders: 1. Dysphagia including inability to swallow and difficulty with specific types of food eg solids, liquids etc. See above for causes of dysphagia, study the effects of bulbar palsy and pseudobulbar palsy (see textbook of internal medicine) 2. Retrosternal pain. This is poorly localized and sometimes leads to bizarre posturing as for example in the Sandifer syndrome (Gastro-esophageal reflux with acid oesophagitis leading to opisthotonic posturing and bizarre movements, evidently to get away from the pain!) 3. Children do not usually complain of “water brash” the hypersecretion of saliva produced to neutralize acidity, found when there is acid reflux into the oesophagus. 4. Vomiting and regurgitation. Study the difference between the two. (Coovadia & Wittenberg page 437) Vomiting Objectives: 1) To be able to list and discuss causes of vomiting and regurgitation; 2) To be able to recognize by history and examination, common and important causes of vomiting and manage them appropriately; 3) To be able to discuss the modes of presentation, clinical features, diagnosis, management and complications of gastro-oesophageal reflux and pyloric stenosis. Illustrative Case Report: Baby Z is referred from Mamelodi Day Hospital at the age of 9 months because of vomiting, dehydration and failure to thrive. His birth weight was 3.6 Kg at term. He was breastfed for 3 months and seemed to do well. However, he always seemed to regurgitate his feeds. This had become gradually worse after the introduction of formula feeds, and more recently he has been vomiting after most feeds, especially after solids. Over the last few days he has vomited up most of the fluids and food he has received. He has developed a funny sweet smell. He does not have diarrhoea. Since age 6 months the clinic nurse has not been satisfied with been recorded as follows: Birth 3.6 Kg 7 months 3 months 5.8 Kg 8 months 4 months 6.2 Kg 9 months 6 months 7.4 Kg his weight gain. His weights had 7.6 Kg 7.7 Kg 7.8 Kg On examination, he looks dehydrated. He has a ketotic smell, but does not appear to be acidotic. He is obviously underweight for his age. There are no other abnormal features on general examination. His abdomen is not distended. Questions: 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) What is the difference between vomiting and regurgitation? When is regurgitation significant enough to require investigation or intervention? What is a normal pattern of growth? At what stage was this patient’s growth not normal? What are the causes of vomiting? How can one distinguish between vomiting due to central nervous system causes and gut causes? What are the causes of ketosis and which apply to this patient? What are the biochemical effects of severe vomiting? How should this patient be investigated to determine the cause of vomiting? What are the clinical differences between upper and lower gut obstruction? Vomiting is one of the commonest and most important symptoms in childhood. See C&W p 438 for a list of causes according to age. In each case, a careful history goes a long way towards making a diagnosis. Task Study Coovadia & Wittenberg 170 – 171, 437 – 439, 606 - 607 Plot the above patient’s recorded weights on a weight growth chart, as shown below: Percentiles for boys from birth to age 36 months Solution to problem case Always regurgitating after feeds suggests either overfeeding, a feeding problem or simple reflux in a baby who is otherwise well. In this case, overfeeding is not likely because such patients tend to become increasingly overweight. Feeding problems occur when babies are positioned wrongly during feeds or immediately thereafter. Excessive shaking, tickling, movement or abdominal palpation of a baby after a feed will usually result in regurgitation. The commonest form of presentation of GER is simple regurgitation after feeds (C&W page 444. Such babies are not ill and thrive well. In this baby, weight gain became poor after age 6 months. This coincided with worsening vomiting especially with solid feeds. The progressive nature of the vomiting suggests that there is a progressive worsening condition. Over the last few days the baby is vomiting just about everything he has eaten. He is now ketotic and dehydrated. That suggests that he is now not getting enough food or fluid in to maintain his homeostasis. In other words, he appears to have intestinal obstruction. However, his abdomen is not distended, suggesting the obstruction is at the level of the oesophagus. A radiological contrast study must be done. Barium swallow oesophagus stenosis The patient has a hiatus hernia with some of his stomach in the chest. This has resulted in reflux with the vomiting, but also acid oesophagitis with scarring which caused progressive narrowing of the oesophagus to the point of almost complete obstruction. This is a recognized mode of presentation of GER, in which there is a complication of the reflux leading to either dysphagia, blood loss with anaemia, chronic failure to grow because of a lack of food intake. Other modes of presentation of reflux include vomiting with respiratory symptoms from aspiration, or vomiting together with failure to thrive. If this baby had been seen at age 7 or 8 months, the fall-off in weight gain evident on his growth chart at that stage should have prompted evaluation of his post-prandial vomiting. Gastro-oesophageal reflux Abnormal neural control of LES Defective LES Motility Transient Lower Oes. Sphinct. relaxation Gastric distension GER Hiatus Hernia Oesophagitis LES = Lower esophageal sphincter GER = Gastro-esophageal reflux In the diagram above, it can be seen that GER occurs when there is transient relaxation of the lower oesophageal sphincter. This happens when the following conditions apply: Gastric distension after a large feed Abnormal motility of the lower oesophagus Abnormal neural control of the lower oesophageal sphincter Once there is relaxation of the lower sphincter and reflux occurs with acid influx into the lower oesophagus, the resulting peptic oesophagitis results in abnormal motility and interferes with sphincter closure. In this way, significant reflux leads to further reflux.