Perioperative Management of Atrial Fibrillation
advertisement

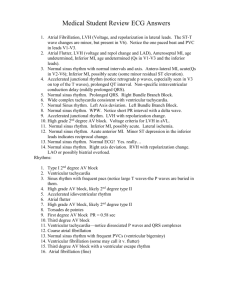
Atrial Fibrillation-An Update William A. Shapiro, M.D. UCSF Department of Anesthesia November 24, 2004 E-mail: shapirob@anesthesia.ucsf.edu Prevalence in the general population, and, after surgery. First described in humans in 1909,1 the prevalence of atrial fibrillation (AF) in the United States population is currently estimated to be 0.4 to 0.9%, or 1-2.2 million cases.2-3 The average age for onset of AF is 70-74 years, and the average survival after onset is 5-6 years.4 The median age of those with AF is 75 years and approximately 10% of patients over 80 years have AF.2 New onset of AF is the most common postoperative arrhythmia after both cardiac surgery (coronary artery bypass graft surgery and valvular surgery5) and lung surgery.6 As the population ages, and increasing numbers undergo anesthesia and surgery, the frequency with which we encounter AF will increase. Anesthetic Considerations Preoperative considerations in patients with AF scheduled for elective surgery AF is a marker for cardiac disease, most commonly associated with chronic hypertension, coronary artery disease, or congestive heart failure, but also with valvular disease, especially abnormalities of the mitral valve, including mitral valve prolapse, and the Wolff-Parkinson-White (WPW) syndrome. AF occurs in 7-10 percent of patients experiencing an acute myocardial infarction.7 Noncardiac risk factors in patients with AF include hyperthyroidism, diabetes, alcohol ingestion, chronic and acute pulmonary disease, hyperadrenergic states, sepsis, and electrolyte disturbances. Most patients in AF will present for surgery already medicated with digitalis for control of ventricular rate. Some with a prior history of AF will be taking drugs to maintain sinus rhythm. Because AF is so intimately associated with cerebral stroke and peripheral emboli, the preoperative evaluation of these patients also must include a careful search for and documentation of any abnormality of the central or peripheral nervous system. Stroke prevention therapy for many will include antithrombotic medication. Is it safe to proceed with surgery? No data are available to suggest an optimal rate of ventricular contraction when patients in AF present for elective surgery. However, a range of 60-100 beats per minute (bpm) seems prudent. Unfortunately, a resting ventricular response between 60-100 bpm Atrial Fibrillation-An Update 2 does not preclude development of tachycardia due to sympathetic stimulation from such events as laryngoscopy or surgical incision. Ideally, optimal drug therapy to control ventricular rate will prevent unwanted, potentially dangerous rates of rapid ventricular contraction during periods of stress. A resting ventricular rate greater than 100 bpm should prompt a search for the cause before beginning anesthesia. If the reason for the elevated heart rate is not apparent, elective surgery probably should be postponed, pending further investigation and adjustment of medication. Digitalis may be administered intravenously or the existing dose increased, but likely will require 30 or more minutes to take effect. If the planned surgery is semi-urgent or emergent, verapamil or a beta-blocking agent also may be given intravenously. However, these agents have negative inotropic effects and require titration, especially if anesthesia is to be induced soon thereafter. Elective cardioversion may terminate AF, restoring sinus rhythm, but fail to improve cardiac output (see below “Does cardioversion to sinus rhythm restore atrial pump function?”). When cardioversion restores sinus rhythm, intraoperative measures to prevent a return to AF with an unacceptably rapid ventricular rate are an essential component of the anesthetic management plan. Intraoperative management of new onset AF Unfortunately, patients undergoing general anesthesia are unable to describe any symptoms related to the acute onset of AF. Therefore, the new onset of AF during general anesthesia requires a dual approach. First, blood pressure must be measured to determine if immediate cardioversion is required. If significant hypotension exists, cardiopulmonary resuscitation (CPR) is indicated until a defibrillator is available. If the first shock (150-200 Joules) is unsuccessful in restoring sinus rhythm, the highest energy level available should be used for all subsequent shocks. If restoration of sinus rhythm is transient, procainamide hydrochloride (5.0-10.0 mg/kg) may be slowly administered intravenously and cardioversion repeated. Hypotension associated with administration of iv procainamide may be treated with iv neosynephrine, 50-100 µg, or ephedrine, 5-10mg. Second, almost simultaneously, the cause for conversion to AF must be identified. Hypoxemia or elevated levels of anesthesia must be immediately excluded as possible causes. As soon as possible, the acid-base and electrolyte status and hemoglobin concentration should be determined. During thoracic or upper abdominal surgery, merely touching the heart with cold surgical equipment may initiate AF. Alterations in venous return also may produce changes in atrial rhythm. While myocardial ischemia may lead to AF, the reverse also is true, making it difficult to determine which came first. If myocardial ischemia is suspected, iv nitroglycerin is indicated. Atrial Fibrillation-An Update 3 Cardioversion of AF The decision to control AF with drugs or cardioversion depends on the patient's hemodynamic status. In awake patients, if the onset of AF is associated with signs or symptoms of angina, congestive failure, dyspnea, or significant hypotension resulting in dizziness or other alterations of mental status, then cardioversion is indicated. A shock of 150-300 Watt sec (Joules) using an anteroposterior pad system successfully restores sinus rhythm in more than 90% of cases. Lower energy levels may be attempted, but often fail, probably because the entire right and left atria are not simultaneously defibrillated. If cardioversion only transiently restores sinus rhythm, then iv procainamide hydrochloride (10-15 mg/kg in awake patients) may be given slowly (over 20-30 minutes) and cardioversion repeated. This drug will prevent atrial premature beats, the usual mechanism of initiation of AF. If the described symptoms do not accompany AF, then pharmacologic therapy, both to control ventricular rate and restore sinus rhythm, may be used. Pharmacologic management of AF Cardioversion is 80-90% effective in restoring sinus rhythm. Unfortunately, without additional drug therapy, only 25% of patients remain in sinus rhythm after one year.8 Medical therapy is first directed at decreasing the ventricular rate, then at converting AF to sinus rhythm. Drugs which prolong AV conduction time are used to control the ventricular rate. Digitalis is the standard, exerting an indirect vagal effect on the AV node at lower doses and an additional direct effect as the dose is increased. IV digitalis has on onset time of 15-30 minutes and the addition of a calcium channel or beta blocking drug may be necessary for initial control of ventricular rate. Calcium channel and beta blocking agents must be used cautiously in patients with decreased cardiac function. Adenosine is a powerful AV node blocking drug that may play a role in the diagnosis and management of some arrhythmias, but has a duration of action too brief to provide long-term management of ventricular rate during AF. In patients who are febrile, hypovolemic, or present with thyrotoxicosis, it may be difficult to control ventricular rate until the underlying medical condition is treated. AV node blocking drugs are contraindicated in patients with WPW whose arrhythmias include irregularly, irregular wide QRS complexes during episodes of AF. Most anti-arrhythmic agents designed to restore sinus rhythm and prevent recurrence of AF are successful for one year in about 50% (range, 40-70%) of treated patients. Quinidine and procainamide, from the Vaughan Williams class 1A agents, are the drugs traditionally given, but both also are associated with an increase in complications, including Atrial Fibrillation-An Update 4 a higher mortality rate, relative to the rate of complications in untreated patients. More recently, class 1C agents, flecainide and propafenone, have been used, but appear to be no more effective than quinidine. Class 3 agents, sotalol and amiodarone9, may offer new alternatives when these other agents are ineffective or contraindicated (see also "Recent Advances" below). Current recommendations acknowledge that an individual approach for each patient will be required to arrive at optimal therapy. Does cardioversion to sinus rhythm restore atrial pump function? In 1964, Braunwald10 postulated that when conversion from AF to sinus rhythm did not improve cardiac hemodynamics, atrial contraction was not effectively restored. Subsequent introduction of two-dimensional and Doppler echocardiography demonstrated that the return of electrocardiographic (ECG) P-wave activity did not necessarily indicate coordinated effective atrial contraction. In some patients, 3-4 weeks may be required for atrial contractile function to return after chronic AF (greater than one-week duration) is converted to sinus rhythm, despite the presence of P-waves on the ECG immediately after cardioversion.11 For this reason, when patients in chronic AF present for elective surgery, cardioversion prior to induction of anesthesia may not result in improved hemodynamic parameters. The reason for this transient atrial dysfunction is not known. However, conversion of recent or new onset AF to sinus rhythm should return full atrial contractile pump function with the resumption of sinus rhythm. Contribution of atrial contraction to cardiac output During sinus rhythm in normal hearts, 70-75% of ventricular filling occurs passively during early diastole and the remaining amount with atrial contraction. The contribution of atrial contraction to the final end-diastolic ventricular volume is therefore relatively small in normal hearts. This response is clinically observed in healthy young individuals during anesthesia when a junctional rhythm takes over at almost the same rate, producing little or no change in blood pressure. As the normal heart ages, compliance of the left ventricle decreases. Consequently, there is less filling during the passive phase of diastole and an increase in the contribution of atrial contraction to left ventricular filling volume. Additionally, diseases that elevate left ventricular end-diastolic pressure or otherwise reduce left ventricular compliance will increase significantly the contribution of atrial contraction to ventricular filling, sometimes by as much as 50% of cardiac output. In such cases, the sudden conversion to AF, independent of the ventricular rate, may herald the onset of congestive failure, angina, or other symptoms associated with heart failure. Common cardiac diseases with which the onset of AF may produce clinical symptoms include mitral or aortic stenosis, left ventricular Atrial Fibrillation-An Update 5 hypertrophy from any cause (most often a result of chronic hypertension), any cardiomyopathy, or an acute myocardial infarction. In these conditions, maintenance of sinus rhythm during induction of anesthesia and throughout surgery is critically important. Mechanism (Electrophysiology) of AF AF is characterized by low amplitude atrial activity that exhibits variability in polarity, amplitude, and cycle length, usually between 300-600 complexes/minute. As a result, there is variability in ventricular rate and blood pressure, because each contraction and subsequent stroke volume depends on the amount of time for ventricular filling available between heart beats. Because AF is chaotic and usually involves both right and left atria, cardiac pacing will be ineffective in terminating it. For the same reason, relatively high energy levels, usually above 150 Joules, are necessary for successful cardioversion. Anesthesia for elective cardioversion Various short-acting anesthetic agents have been used successfully to provide amnesia for cardioversion, including barbiturates, benzodiazepines, and ketamine with or without narcotics. At our institution, we have begun using propofol in bolus doses ranging from 20-100 mg. Our initial dose is determined after evaluation of the patient's cardiac function (left ventricular ejection fraction), age, and overall general medical condition. Subsequent doses are administered if multiple cardioversions are required or the initial dose proves inadequate. We routinely pre-oxygenate our patients and, if necessary after propofol injection, provide positive pressure ventilation. With propofol, our impression is that airway muscle tone is well-maintained during spontaneous ventilation and patients return to pre-anesthesia mental status quickly and without residual drug “hangover”. Recent advances in the management of chronic AF Management of AF is directed in three areas: 1) control of the ventricular rate during AF, 2) conversion to sinus rhythm with subsequent improvement in cardiac output by restoring atrial pump function, and 3) prevention of stroke. Medical strategies The financial impact of AF and associated heart disease and stroke have provided incentive to reduce these health care costs. New strategies fall into two categories — agents to maintain sinus rhythm and drugs to decrease the incidence or the severity of cerebral stroke. Atrial Fibrillation-An Update 6 Oral amiodarone therapy currently offers both a higher rate of maintenance of sinus rhythm and a lower rate of complications than both class 1A and 1C agents.12-13 In most patients, chronic amiodarone therapy does not appear to result in complications during anesthesia, but case reports of possible interactions between amiodarone and anesthesia suggest further studies to evaluate these interactions more completely, particularly in patients with cardiac disease.14 The association of AF, overall cardiac function, and patient age appears to contribute importantly to stroke formation.15-16 Recent FDA approval of Activase,17 a genetically engineered tissue plasminogen activator (TPA), is directed at minimizing the effects of stroke once they present, similar in concept to early TPA intervention in acute myocardial infarction. Unfortunately, the complication rate, 6%, is higher than the placebo complication rate. Another drug, citicoline,18 still in the experimental stages, may offer similar benefits with fewer side effects, and may have beneficial effects even when given up to 24 hours after the onset of a stroke. The implications of some of these agents for patients undergoing anesthesia and surgery are not yet known. When ventricular rate cannot be controlled adequately with pharmacologic agents, or patients are unable or unwilling to take medication, several alternative strategies are available. A-V node ablation Various techniques are available that destroy the AV node permanently, thus preventing propagation of atrial impulses to initiate ventricular contraction. This approach manages ventricular rate by causing complete heart block, then requiring a ventricular pacemaker to control heart rate. Therefore, this technique renders the patient permanently pacemaker-dependent. Although drugs will no longer be required to manage heart rate, the consequences of this therapy will include lifelong cardiac pacing, and atria which remain fibrillating and enlarged, placing the patient at high risk for the development of thrombus and subsequent stroke. Anesthetic considerations for patients with pacemakers are reviewed elsewhere.19 Surgical therapy In 1980, Williams and Cox20 introduced a surgical alternative to the management of AF. Their goal was three-fold: to eliminate AF, to restore effective atrial contraction to boost cardiac output, and to reduce the thromboembolic sequelae associated with AF. The surgery, referred to as the “maze” procedure, is designed to prevent any area of atrial tissue from being large enough to sustain AF. An atrial pathway, or maze, is created for sinus node impulses to weave their way to the AV node.21 The results of more than ten years of research are available in a remarkable series Atrial Fibrillation-An Update of papers that both describe the surgical technique and provide fresh insight into the mechanism of AF in humans.22-25 7 Atrial Fibrillation-An Update 8 Conclusion As the population ages, the number of patients presenting for surgery with AF will increase. These patients will have heart disease and will be taking medication. Some may have undergone AV node ablation, rendering them pacemaker-dependent; others will have undergone cardiac surgery to restore sinus rhythm. As new medications for management of AF and stroke are approved, their interactions with anesthetic agents will require careful evaluation. References 1. Lewis T: Auricular fibrillation: a common clinical condition. Br Med J II:1528, 1909 2. Blackshear JL, Kopecky SL, Litin SC, et al. Management of atrial fibrillation in adults: prevention of thromboembolism and symptomatic treatment. Mayo Clin Proc 71:150-160, 1996 3. National Heart, Lung, and Blood Institute Working Group on Atrial Fibrillation: current understanding and research imperatives. J Am Coll Cardiol 22:1830-34, 1993 4. Movsowitz HD, Lampert C, Jacobs LE, et al. Atrial fibrillation in the elderly: a review. Am J Geriatric Cardiology pgs. 26-40, March/April, 1994 5. Creswell LL, Schuessler RB, Rosenbloom M, et al. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg 56:539-549, 1993 6. von Knoring J, Lepäntalo M, Lindgren L, et al. Cardiac arrhythmias and myocardial ischemia after thoracotomy for lung cancer. Ann Thorac Surg;53:642-647, 1992 7. Cristal N, Szwarcberg J, Gueron M: Supraventricular arrhythmias in acute myocardial infarction. Prognostic importance of clinical setting; mechanism of production. Ann Intern Med 82:35-39, 1975 8. Coplen SE, Antman EM, Berlin JA, et al. Efficacy and safety of quinidine therapy for maintenance of sinus rhythm after cardioversion. Circulation 82:1106-1116, 1990 9. Galve E, Rius T, Ballester R, et. al. Intravenous amiodarone in treatment of recent onset atrial fibrillation: Results of a randomized, controlled study. J Am Coll Cardiol 27:1079-1082, 1996 10. Braunwald E. Introduction to symposium on cardiac arrhythmias with comments on the hemodynamic significance of atrial systole. Am J Med 37:665-669, 1964 11. Shapiro EP, Effron MB, Lima S, et al. Transient atrial dysfunction after conversion of chronic AF to sinus rhythm. Am J Cardiol 62:1202-1207, 1988 12. Gosselink AT, Crijns HJ, Van Gelder IC, et al. Low-dose amiodarone for maintenance of sinus rhythm after cardioversion of atrial fibrillation or flutter. JAMA 267:3289-3293, 1992 13. Hohnloser SH, Klingenheben T, Singh BN. Amiodarone-associated proarrhythmic effects: a review with special reference to torsades de pointes tachycardia. Ann Intern Med 121:529535, 1994 Atrial Fibrillation-An Update 14. 9 Rooney RT, Marijic J, Stommel KA, et al. Additive cardiac depression by volatile anesthetics in isolated hearts after chronic amiodarone treatment. Anesth Analg 80:917-924, 1995 15. Brickner EM. Cardioembolic stroke. Am J Med 100:465-474, 1996 16. Cairns JA and Connolly SJ. Nonrheumatic atrial fibrillation: risk of stroke and role of antithrombotic therapy. Circulation 84:469-481, 1991 17. Fisher LM. Panel recommends approval of drug for stroke treatment. New York Times, p. A12, June 7, 1996 18. Associated Press. Drug found to protect the brain during stroke. New York Times, p. A-18, March 29, 1996 19. Shapiro WA. Practical management of the pacemaker patient. Refresher Course Abstracts. p 19. Society of Cardiovascular Anesthesiologists, 1994 20. Williams MJ, Ungerleider RM, Lofland GK, Cox JL. Left atrial isolation: new surgical technique for the treatment of supraventricular arrhythmias. J Thorac Cardiovasc Surg 80:373-80, 1980 21. Cox JL, Boineau JP, Schuessler RB, et al. Five year experience with the maze procedure for atrial fibrillation. Ann Thorac Surg 56:814-823, 1993 22. Cox JL, Schuessler RB, Boineau JP. The surgical treatment of atrial fibrillation. I. Summary of the current concepts of the mechanisms of atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg 1991;101(3):402-405 23. Cox JL, Canavan TE, Schuessler RB, et al. The surgical treatment of atrial fibrillation. Intraoperative electrophysiologic mapping and description of the electrophysiologic basis of atrial flutter and atrial fibrillation. J Thorac Cardiovasc Surg 1991;101(3):406-426 24. Cox JL, Schuessler RB, D’Agostino HJ, Stone CM, Chang B-C, Cain ME, Corr PB, Boineau JP. The surgical treatment of atrial fibrillation: III. Development of a definitive surgical procedure. J Thorac Cardiovasc Surg 1991;101(4):569-583. 25. Cox JL. The surgical treatment of atrial fibrillation: IV Surgical technique. J Thorac Cardiovasc Surg 1991;101(4):584-592.