Cardiopulmonary Resuscitation Policy
advertisement

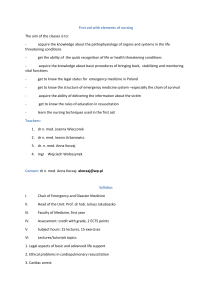
Cardiopulmonary Resuscitation Policy (Including Anaphylaxis and Defibrillation) Version 13 Name of responsible (ratifying) committee Resuscitation Committee Date ratified 24th April 2014 Document Manager (job title) Resuscitation Manager Date issued 25th April 2014 Review date 24th April 2017 (unless requirements change) Electronic location Clinical Policies Related Procedural Documents Do Not Attempt Cardiopulmonary Resuscitation Policy. Neonatal Resuscitation Maternity Policy Medical Devices Management Policy First Aid At Work Policy People Moving and Handling Policy Management of the Deteriorating Patient Key Words (to aid with searching) Cardiopulmonary; resuscitation; CPR; defibrillation; anaphylaxis; heart arrest; cardio respiratory services; bariatric patients Version Tracking Version Date Ratified 12 23rd January 2012 13 Brief Summary of Changes Author Resuscitation Manager Clarity given to the response to non-clinical areas and the Duty Hospital Manager role Clarity given to the response to external buildings Post anaphylaxis reaction actions listed Neonatal Emergency Team/Flat Baby Team name changed to Neonatal Crisis Team References updated including the reference to NHSLA removed and the National Early Warning System and NCEPOD added CONTENTS Cardiopulmonary Resuscitation Issue 13 25th April 2014 th (Review date: 24 April 2017 unless requirements change) Page 1 of 33 QUICK REFERENCE GUIDE ............................................................................................................. 3 1. INTRODUCTION.......................................................................................................................... 4 2. PURPOSE ................................................................................................................................... 4 3. SCOPE ........................................................................................................................................ 4 4. DEFINITIONS .............................................................................................................................. 4 5. DUTIES AND RESPONSIBILITIES ............................................................................................. 7 6. PROCESS ................................................................................................................................... 8 7. TRAINING REQUIREMENTS .................................................................................................... 15 8. REFERENCES AND ASSOCIATED DOCUMENTATION ......................................................... 15 9. EQUALITY IMPACT STATEMENT ............................................................................................ 16 10. MONITORING COMPLIANCE ................................................................................................... 17 APPENDIX 1: Resuscitation Training Needs Analysis for staff with frequent, regular contact with patients…………………………………………………………………………………………………………18 APPENDIX 2: Anaphylaxis algorithm and investigations ….………………………………………….....20 APPENDIX 3: Cardiac Arrest/Medical Emergency Response Teams and equipment availability for non-clinical areas on QAH site…………………………………………..…………………………………..22 APPENDIX 4: Minimum Personnel, Skills and Knowledge Levels for Queen Alexandra Hospital Cardiac Arrest Teams (CAT)………………………………………………………………………………...25 APPENDIX 5: Cardiac arrest record forms…………………………………………………………………28 APPENDIX 6: Electrical equipment safety during defibrillation………………………………………..…32 APPENDIX 7: Defibrillation during renal replacement therapy using vascular access …………….....33 . Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 2 of 33 QUICK REFERENCE GUIDE This policy must be followed in full to ensure that a high-quality and robust resuscitation service is available for patients, staff and visitors at all times. For quick reference the guide below is a summary of actions required. This does not negate the need for all staff to be aware of and follow the detail of this policy. 1. All patients, staff and visitors will receive safe, early and appropriate Cardiopulmonary Resuscitation, including early defibrillation when required 2. All staff with frequent, regular patient contact will attend annual resuscitation training relevant to their role. This training will include, as appropriate, anaphylaxis management, identification and response to the deteriorating patient, DNACPR and post resuscitation care; 3. All in-patient vital signs will be recorded and an early warning score will be generated as per Management of the Deteriorating Patient policy (5). This will indicate whether escalation of care is required and ensure the appropriately skilled healthcare professional is called. This will aid identification and response to patients at risk from cardio-respiratory arrest; 4. All patients having an anaphylactic reaction will be managed following the current Resuscitation Council (UK) guidance (6); 5. All cardiac arrest equipment must be checked on a daily basis and after use by a registered healthcare practitioner to ensure continually availability in clinical areas; 6. All staff using a defibrillator will attend training on an annual basis to demonstrate practical and theoretical competence in the safe use of a defibrillator; 7. To enable the monitoring of compliance to this policy all respiratory and cardiac arrests will be recorded on the current PHT Cardiac Arrest Form. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 3 of 33 1. INTRODUCTION This Cardiopulmonary Resuscitation (CPR) policy is based on the quality standards for cardiopulmonary resuscitation practice and training published by the Resuscitation Council (UK) (Nov 2013) (1). It has been developed to describe the process for managing and mitigating risks associated with resuscitation, by also incorporating the key finding and recommendations from the NECOPD report - Time to Intervene (2012), within Portsmouth Hospitals NHS Trust (the Trust). The Trust must provide a resuscitation service for patients, visitors and staff on its sites. The aim is that all health care staff who have direct patient contact must be able to provide CPR at levels appropriate to their role and healthcare environment in which they are working. As a minimum this is Basic Life Support (BLS). However, some staff e.g. doctors, nurses and technicians must provide elements of Advanced Life Support (ALS), including defibrillation. CPR is undertaken in an attempt to restore breathing (sometimes with support) and spontaneous circulation in a patient in cardiac and/or respiratory arrest. CPR is a relatively invasive medical therapy and it is therefore essential to identify patients for whom cardiac and/or respiratory arrest represents a terminal event in their illness. The Trust has a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) policy which should be read in conjunction with this policy to ensure that CPR is only initiated for patients when it is appropriate and in their best interests. 2. PURPOSE The purpose of this policy is to ensure that: prompt, safe, early and appropriate cardiopulmonary resuscitation and defibrillation occurs within the Trust; the management of anaphylaxis follows the Resuscitation Council (UK) guidelines (6) and appendix 2; 3. SCOPE This policy applies to all staff (including voluntary workers, students, locums and agency) of Portsmouth Hospitals NHS Trust, the MDHU (Portsmouth) and Carillion, whilst acknowledging for staff other than those of the Trust the appropriate line management or chain of command will be followed. In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety. 4. DEFINITIONS Adult Manual Defibrillation Pads Adhesive external pads which are attached to the patient to enable the delivery energy for external pacing, defibrillation or cardioversion purposes. Adult pads are used for all patients over 10kg. Advanced Life Support (ALS) The term ALS describes additional measures aimed at restoring ventilation and a perfusing cardiac rhythm: this is necessary to improve the chance of long term survival. Anaphylaxis is an acute life-threatening hypersensitivity reaction and should be considered when there is an acute onset, life threatening airway and/or breathing and/or circulation problems; especially if skin changes present (Appendix 2). Automated External Defibrillators (AED) The defibrillator itself analyses the cardiac rhythms, and advises whether a shock is indicated or not, and selects the appropriate energy levels according to the current Resuscitation Council (UK) Guidelines (3). AED’s allow staff such as nurses and physiotherapists to defibrillate prior to the arrival of more expert help. AED’s can be used on paediatric patients however attenuated pads Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 4 of 33 that reduce the energy delivered are used for children weighing less than 25kg. Where possible, AED’s should be avoided in the under one year old age group due to potential problems with rhythm recognition. Basic Life Support (BLS) The purpose of BLS is to maintain adequate oxygenation to the vital organs through maintenance of ventilation and circulation. This is continued until the respiratory/cardiac arrest is reversed, and/or the underlying cause treated, or the resuscitation attempt is stopped. It is therefore a "holding measure" until defibrillation and/or advanced life support is available. Failure of the circulation for three to four minutes (less if the victim is initially hypoxaemic) will lead to irreversible cerebral damage. Delay, even within that time, will lessen the eventual chances of a successful outcome. Emphasis must therefore be placed on prevention of cardiac arrest and early access to help then rapid institution of BLS by a rescuer if required. Basic Life Support with Airway Adjunct Basic life support implies that no equipment is employed. When a simple airway device or facemask is used to assist the delivery of ventilations, this is defined as "basic life support with airway adjunct". Cardiac Arrest Cardiac arrest is the sudden cessation of mechanical cardiac activity, confirmed by the absence of a detectable pulse, unresponsiveness, and apnoea or agonal, gasping respiration. Cardiac Arrest Team (CAT) A Cardiac Arrest Team is available on the Queen Alexandra Hospital site at all times and comprises staff trained in ALS. There are different teams for different patient groups as identified in Appendix 7. These teams must achieve a recommended level of training to achieve the required skill set (Appendix 8). Cardiac Rhythms Cardiac rhythms associated with cardiac arrest can be divided into two groups: ventricular fibrillation / pulseless ventricular tachycardia (VF/VT) and other rhythms (Non VF/VT). The latter includes asystole and pulseless electrical activity (PEA). The principle difference in the management of these two groups is the need for defibrillation in those patients with VF/VT. Subsequent actions, including chest compressions, airway management and ventilation, venous access, the administration of adrenaline, and the identification and correction of reversible causes, are common to both groups. Cardiopulmonary Resuscitation (CPR) Cardiopulmonary Resuscitation is a combination of artificial ventilation, chest compressions, drug therapy and defibrillation. Cardioversion This term will be taken to mean synchronised cardioversion i.e. the synchronised button is used to ensure that a DC shock is not delivered on the "T" wave, which in the susceptible heart can lead to VF or VT. Chain of Survival The interventions that contribute to a successful outcome after cardiac arrest can be conceptualised as a chain. The four links of the chain comprise of: early recognition and call for help (i.e. phone 2222), early CPR, early defibrillation and post resuscitation care Clinical Staff A member of trust staff whose job description includes direct patient care. Defibrillation Defibrillation is the definitive treatment for Ventricular Fibrillation (VF) and pulseless Ventricular Tachycardia (VT). It involves the delivery of a DC electric shock to the myocardium. The energy level to be administered is defined in the current ALS guidelines by the Resuscitation Council Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 5 of 33 (UK). For defibrillation to be effective, a critical mass of the myocardium needs to be depolarised to allow the heart’s own pacemakers to resume control. Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) A DNACPR order indicates that in the event of a cardiac arrest, CPR will not be initiated. DNACPR decisions are the overall responsibility of the Consultant/General Practitioner in charge of the patient’s care. Attempts at CPR will not be commenced when it is felt that a patient would not survive or when it is not the patient’s wishes. It is emphasised that a DNACPR decision does not prevent other forms of treatment being provided. See current Trust DNACPR Policy for further detail. Early Warning Score and Escalation Protocols For adult in-patients the early warning system and escalation protocol is incorporated into VitalPAC. This is a tool for bedside evaluation of physiological parameters provides prompts to the clinical staff on when and who to call for additional help. There are adapted early warning systems and escalation protocols for Obstetric and Paediatric in-patients. Further information is in the Trust Management of the Deteriorating Patient Policy. Neonate For the purpose of this policy a neonate is any infant cared for within the Maternity Unit or Neonatal Intensive Care Unit (NICU) regardless of age. For other areas within the organisation the neonate is a baby below 29 days of age. Newborn Resuscitation Policy The newborn resuscitation policy outlines the management of the newborn/neonate infant whilst in Maternity and NICU. Non-clinical staff A member of the Trust staff whose job description does not include direct patient care. Some staff in this group need to attend annual resuscitation training, if their role includes patient contact without clinical staff immediately available, such as reception staff. Paediatric AED defibrillation pads Adhesive external pads used with an automated external defibrillator which itself analyses the cardiac rhythms. The pads are attached to the patient but reduce the energy before the delivery of current for defibrillation or cardioversion is delivered. These are used for paediatric patients under 25kg. Paediatric Manual defibrillation pads Adhesive external pads used for infants under 10kg. Paediatric Resuscitation Guidelines The paediatric resuscitation BLS guidelines are related to size and used for the management of an infant, a baby under one year, and for a child between one year and puberty. The paediatric ALS guidelines are weight related and therefore apply to all babies and pre-puberty children. Patient Group Direction (PGD) Patient Group Directions (PGDs) are documents which make it legal for medicines to be given to groups of patients - for example in a vaccination programme - without individual prescriptions having to be written for each patient. They can also be used to empower staff other than doctors (for example paramedics and nurses) to legally give the medicine in question. Respiratory Arrest Respiratory arrest is the cessation of spontaneous breathing. 2222 is the emergency number for the Cardiac Arrest Response at Queen Alexandra Hospital (QAH), St. Mary’s Community Hospital (SMH) and Gosport War Memorial Hospital (GWMH). Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 6 of 33 5. DUTIES AND RESPONSIBILITIES Resuscitation Manager and the Resuscitation Training Team The Resuscitation Manager and the Team are responsible for ensuring that: Resuscitation Training delivered to Trust staff adheres to the current Resuscitation Council (UK) guidelines and incorporates training on the current early warning system used by the Trust for the identification of patients at risk, including the systems for summoning help, and DNACPR decision making; The delivery of annual resuscitation training updates including the requirement for attendees to be aware of the need to read and implement this policy and the DNACPR policy; All ‘2222’ calls relating to medical emergencies and cardiac arrests are reviewed and relevant data is collected Monday to Friday by a Resuscitation Officer (RO) and entered on the database. All cardiac arrest data from Portsmouth Hospitals NHS Trust is submitted to the National Cardiac Arrest Audit (NCAA) ICNARC - Intensive Care National Audit & Research Centre A Resuscitation Officer will: o Review all returned audit sections of the DNACPR form and ensure key data is entered onto the database; o Lead on collecting data on resuscitation A rolling annual audit of the Cardiac Arrest equipment is undertaken in the Trust clinical areas located on the Queen Alexandra Hospital, St Mary’s Community Hospital, Petersfield Community Hospital and Gosport War Memorial Hospital sites; There are equipment and daily check lists available for the clinical staff to ensure the cardiac arrest equipment is in a state of readiness at all times. The Resuscitation Link Network The Network, which meets quarterly, consists of resuscitation link champions from each clinical area and all the Resuscitation Officers, each of whom chair the Network on a rolling basis. The Network is utilised to cascade information to and from the clinical areas, to support organisational learning and feedback Line Managers Line Managers are responsible for: Ensuring the daily checks are completed on the cardiac arrest equipment to ensure it is in a state of readiness at all times; Taking any unresolvable queries to the link champions or Resuscitation Manager who will take it to the appropriate forum for resolution; Releasing their staff to attend Resuscitation Training, in accordance with the requirements identified in Appendix 1, and monitoring attendance using the monthly reports from Learning and Development. All Clinical Staff All staff are responsible for ensuring that they: Immediately alerting the appropriate response team in the event of a cardiac/obstetric or neonatal emergency (see section 6.2.2); Practice within the current Resuscitation Council (UK) Guidelines and their own Codes of Professional Conduct; Attend the appropriate resuscitation training annually, as in Appendix 1. This will be monitored by the Line Managers and the Clinical Service Centre (CSC) Governance Steering group using the monthly reports from Learning and Development; Participate in the daily checking of cardiac arrest equipment to make sure the equipment is in a state of readiness at all times; Are familiar with the processes to follow if any cardiac arrest equipment fails or is found to be faulty during the daily operational check or when being used. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 7 of 33 Patient Safety Working Group The Committee is responsible, through the receipt of quarterly reports from the Resuscitation Committee, there is continuous and measurable improvement in the quality of the services provided. The Trust Resuscitation Committee The Committee is responsible for ensuring that: This procedural document is up to date, technically accurate, is in line with evidencebased best practice and has been produced following consultation with stakeholders The processes to enable audits of compliance and monitoring of trust standards, as detailed in this policy, are in place and the actions identified as a result of those audits are implemented.; Through the Chair, assurance on the effectiveness of this policy and the Trust’s procedures for CPR, is provided through a quarterly report to the Patient Safety Working Group, including any necessary recommendations to address identified deficits; Cardiac Arrest Teams The Teams consist of four members: a team leader; an airway technician; a circulation technician; and an assistant. Members of the team must respond at the earliest opportunity to any cardiac arrest bleep, including the test call, which is tested at random each day. The members of each team are outlined in Appendix 3. Clinical Engineering Team The Team is responsible for: Responding to reports of any faults with defibrillators and for making arrangements to repair or replace the equipment (24 hour cover via the Queen Alexandra switchboard). 6. PROCESS 6.1 Identification of patients at risk of cardio-respiratory arrest. There is a Trust Management of the Deteriorating Patient Policy (5) developed in response to the key recommendations of the NICE Clinical Guideline 50. The policy describes in full the process for managing and mitigating risks relating to all aspects of the treatment and care of adults who are acutely ill or at risk of physical deterioration and cardio-respiratory arrest. 6.2 Cardiac Arrest Response 6.2.1 CPR should be commenced for all patients/visitors/staff who suffer a cardiac arrest, unless there is a valid DNACPR decision in place. 6.2.2 Queen Alexandra Hospital Site It is the responsibility of the clinical staff to ensure that patients, visitors and staff suffering a respiratory or cardiopulmonary arrest, receive the appropriate treatment as described in current guidelines by the Resuscitation Council (UK) and as per the appropriate site response. The appropriate emergency response/team will be summoned by using the universal number 2222. The precise location of the patient must be communicated promptly and clearly to the switchboard operator Adult patients state Adult Cardiac Arrest Team Obstetric patients state Maternal Crisis Team and Adult Cardiac Arrest Team Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 8 of 33 Paediatric patients state Paediatric Cardiac Arrest Team Neonates state Neonatal Crisis Team All cardiac arrest bleeps are alerted simultaneously by the Queen Alexandra Hospital switchboard operator via a speech channel. Each member of the emergency team that has been called must attend the specified location immediately. ALS will be provided by the responding team. The composition and skills of the teams above are detailed in Appendix 3 and 4. Note: The speech channel is tested at random each day, to ensure that the system and individual bleeps are in working order. All bleep holders must respond to this test call. 6.2.3 St Mary’s Community Hospital and Gosport War Memorial Hospital sites. The response on these sites is BLS, AED and Ambulance. These hospital sites have a switchboard system so use the universal number 2222. This enables switchboard to activate the medical emergency response bleeps and then call the ambulance service. The member of staff should return to the victim to commence BLS. BLS and AED response as per Resuscitation Council (UK) guidelines will be provided by the healthcare staff present and Advanced Life Support will be provided by the ambulance service. All medical emergency response bleeps will be alerted simultaneously by the relevant site switchboard operator via a speech channel. Each member of the site response team must respond at their earliest opportunity. The speech channel will be tested at random each day, to ensure that the system and individual bleeps are in working order, all bleep holders must respond to this test call. 6.2.4 Petersfield Community Hospital and other Community sites such as Health Centres The response on these sites includes BLS, AED and Ambulance. As there is no switchboard facilities at these sites the Trust healthcare staff present should be aware of the site response procedures to enable the ambulance response to be summoned promptly. BLS and AED (if available) response as per Resuscitation Council (UK) guidelines will be provided by the healthcare staff present and Advanced Life Support will be provided by the ambulance service 6.2.5 Resuscitation in non-clinical areas within main buildings The nearest member of staff to the incident must summon help as per site response. If there is a nearby clinical area then they should be contacted to provide clinical expertise and equipment to patients, visitors and staff. The Duty Hospital Manager will attend the cardiac arrest team calls in non-clinical areas. Their role is to co-ordinate the situation in conjunction with the cardiac arrest team leader, and arrange, if appropriate, transfer of the victim to a “Place of Safety”. This is likely to require a clinical member of staff to contact Main Porters via Ext: 6321 for an urgent transfer. Some non-clinical areas/departments will have a designated person responsible for first aid who should also be summoned. See the Trust’s First Aid at Work Policy for further details. See Appendix 6 for details of Cardiac Arrest Equipment cover for non-clinical areas. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 9 of 33 6.2.6 Resuscitation in areas or buildings outside of the main buildings (e.g. Oasis Centre, QuAD Centre, Health Records Building, Victoria House, Residences, grounds, car parks) If the victim has collapsed in an area or building outside of the main hospital buildings staff should dial the normal emergency number for the site using the nearest internal telephone and switchboard will call an ambulance for transfer to a place of safety. If access to an internal phone is not possible, for example the victim is in an isolated place, then staff should call an ambulance directly as they would in the community setting. 6.2.7 Staff Illness For members of staff who have a life-threatening emergency at work the procedures outlined above should be followed. 6.3 Documentation 6.3.1 Cardiorespiratory arrests in Queen Alexandra Hospital All cardiorespiratory arrests in Queen Alexandra Hospital must be recorded on the Cardiac Arrest Record Form (Appendix 5). The inner copy of the Form must be detached and returned to the Trust Resuscitation Department, by the member of staff who completed the form. 6.3.2 Cardiorespiratory arrests in community sites All cardiorespiratory arrests in community sites must be recorded on the Community Sites Audit Form (Appendix 5) and returned to the Resuscitation Department, by the member of staff who completed the form. 6.4 6.5 Post resuscitation care. The healthcare staff responsible for the patient’s care, such as Cardiac Arrest Team Leader or Nurse in Charge or Duty Hospital Manager, must ensure safe continuity of care and where necessary, safe transfer following resuscitation. This may involve one or more of the following steps: Referral to a specialist; Full and complete documentation and hand-over of care; Preparation of equipment, oxygen, drugs and monitoring systems; Intra-hospital or inter-hospital transfer; Liaison with the Ambulance Service; Liaison with staff experienced in patient retrieval and transfer; Informing relatives; Completion of an Adverse Incident Reporting Form if indicated and in accordance with Trust Policy (13). Ensuring continual availability of cardiac arrest equipment 6.5.1 All cardiac arrest equipment must be maintained in a state of readiness at all times and must be checked by a registered healthcare practitioner every day of ward/departments clinical activity and immediately following conclusion of a cardiac arrest event. The defibrillator must be operationally checked in accordance with the instructions issued by the Clinical Engineering Department. Daily check lists must be Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 10 of 33 kept within the clinical areas for the life of the defibrillator and suction machine (which will be on average ten years) plus one year for audit purposes. 6.5.2 If any cardiac arrest equipment fails or is faulty during the daily operational check or when being used, the ward/department based clinical staff must be familiar with the local procedure for this scenario (i.e. the clinical staff would go to the next nearest clinical area and arrange appropriate cover). Defibrillator faults must be reported immediately to the Clinical Engineering Department (24hr cover via Queen Alexandra Hospital switchboard) so arrangements can be made for repair or replacement as soon as possible. Additional information can be found in the Trust Policy and Protocol for Management of Medical Devices (10). 6.5.3 The cardiac arrest equipment held must be stocked in accordance with a standardised list issued by the Resuscitation Committee (8). The current list can be found on the Resuscitation Department intranet page. 6.5.4 Disposable items should be replenished at the earliest opportunity as indicated on the Trust’s ALS equipment lists (8). Non-disposable items should be de-contaminated and/or cleaned in accordance with both the manufacturers’ guidance and the Trustwide infection control guidance and re-instated to the trolley as soon as is practical. Further information can be obtained on the Resuscitation Department intranet page. 6.5.5 On the Queen Alexandra Hospital site the Cardiac Arrest Drug boxes are replaced from pharmacy during normal working hours and outside of this time they are replaced from the Emergency Drug Cupboards (14). The locations of the Emergency Drug cupboards are detailed on the Trust Pharmacy intranet page. 6.6 Manual Handling In situations where the collapsed patient is on the floor, in a chair or in a restricted/ confined space the organisational guidelines for the movement of the patient must be followed to minimise the risks of manual handling and related injuries to both staff and the patient (15). Further information is also available from the Resuscitation Council (UK) who have issued Guidance for Safer Handling During Resuscitation in healthcare settings (Nov 2009) (16). 6.7 Cross Infection 6.7.1 Whilst the risk of infection transmission from patient to rescuer during direct mouthto-mouth resuscitation is extremely rare, isolated cases have been reported. It is therefore advisable that direct mouth-to-mouth resuscitation be avoided in the following circumstances: All patients who are known to have or suspected of having an infectious disease; All undiagnosed patients entering the Emergency Department, Outpatients or other admission source; Other persons where the medical history is unknown. 6.7.2 All clinical areas must have immediate access to a pocket mask, which must be strategically located, to minimise the need for mouth-to-mouth ventilation. However, in situations where airway protective devices are not immediately available, start chest compression only CPR whilst awaiting an airway/ventilation device. 6.8 Anaphylaxis management 6.8.1 The management of suspected anaphylactic reactions must be conducted in accordance with the current Resuscitation Council (UK) Guidelines for the Management of Anaphylaxis (6). See Appendix 2 for the current treatment algorithm. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 11 of 33 6.8.2 All healthcare professionals administering medication will attend mandatory annual Basic Life Support and Anaphylaxis training as a minimum standard. 6.8.3 For governance purposes non-prescribing healthcare professionals should use the Portsmouth Combined NHS Trusts Patient Group Direction for the use of Adrenaline in the Treatment of Anaphylaxis (17). In addition they must complete and maintain the relevant anaphylaxis competency by attendance at annual training (18). Evidence of competency is held on the ward/department in the individual’s personal development records. 6.8.4 Following an anaphylactic reaction: Patients who have had a suspected anaphylactic reaction should be treated and then observed for at least 6 hours in a clinical area with facilities for treating life-threatening ABC problems. To aid diagnosis the post event the blood tests for Mast Cell Tryptase detailed in Appendix 2 must be completed. The adverse reaction must be reported using the current Adverse Incident Reporting mechanism and a MHRA ‘yellow card’ must be completed, see PHT Cardiopulmonary Resuscitation Policy for more information The patient should be reviewed by a senior clinician and a decision made about the need for further treatment or a longer period of observation. 6.8.5 6.9 Before discharge from hospital all patients must be: Reviewed by a senior clinician. Given clear instructions to return to hospital if symptoms return. Considered for anti-histamines and oral steroid therapy for up to 3 days. Considered for an adrenaline auto-injector (see below), or given a replacement. Have a plan for follow-up, including contact with the patient’s general practitioner. Defibrillation 6.9.1 Defibrillators must only be operated by persons specifically trained in their use. The training will be in accordance with the current Resuscitation Council (UK) Guidelines (3). Staff authorised to manually defibrillate or use AED must have demonstrated practical and theoretical competence to the Trust Resuscitation Department or have attended a course recognised by the Trust’s Resuscitation Department such as RC(UK) Advanced Life Support Course. For further recognised courses please call Ext: 6110. 6.9.2 The member of staff must continue to update practical and theoretical competence annually. However for flexibility and to minimise the impact on the clinical areas and patients there is a permitted period of 2 months whereby staff can urgently arrange an update should their certificate have expired. 6.9.3 If a patient who has had an emergency thoracotomy requires defibrillation then the chest should be closed and external defibrillation should be delivered as per current ALS guidelines. 6.9.4 For further information on electrical equipment safety during defibrillation see Appendix 7. 6.9.5 For further for information on defibrillation during haemodialysis see Appendix 8. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 12 of 33 6.10 Procurement For all resuscitation equipment purchasing the Medical Devices Management policy must be followed (10). All resuscitation equipment purchased must be agreed by the Resuscitation Manager prior to ordering. 6.11 Cardiopulmonary Resuscitation for Bariatric Patients Standard Resuscitation Council (UK) Basic Life Support and Advanced Life Support guidelines should be followed with additional consideration given to the following issues: Airway and Breathing Potential Problems Likely to be more difficult to manage airway Increased risk of regurgitation May be more difficult to achieve good seal with pocket mask/Bag Valve Mask Actions Two person technique when using Bag Valve Mask device Early use of airway adjuncts e.g. Oropharyngeal airway Consider early intubation Circulation Potential Problems Intravenous access likely to be more difficult to achieve Intra-osseous may also be more difficult to achieve Actions If unable to achieve access, consider performing cut-down Chest compressions Potential Problems More difficult for chest compression provider to achieve correct hand/arm position (shoulders directly above hands) More difficult to compress adequate depth (5-6 cms) Actions Position bed height to facilitate effective chest compressions. This is likely to be with the bed at or near it’s lowest position Compressions provider to use foot stool if available Consider the height of the person performing chest compressions and if a taller member of staff is available changing the compression person should be considered as the taller person may find it easier to achieve adequate compressions Defibrillation Potential Problem May be more difficult to place pads in correct position The patients body mass may increase transthoracic impedance Actions Use standard defibrillator pad position. Avoid breast tissue if possible. Use Standard defibrillator energy, 150 Joules, escalating to 200 Joules after first shock Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 13 of 33 6.12 Cardiopulmonary Resuscitation for patients with an Implantable Cardioverter Defibrillator (ICD) 6.12.1 Deactivation of an ICD with a magnet is normally indicated when the ICD is providing inappropriate shock therapy or the patient is undergoing emergency surgery out of hours requiring diathermy. In these situations the decision to deactivate the ICD should be advised by appropriately trained SpR or Consultant with Advanced Life Support training. If an ICD has been deactivated the patient should be closely monitored for treatable arrhythmias and an external defibrillator should be attached to patient. A member of staff trained in external defibrillation should remain in attendance. 6.12.2 In event of Cardiac Arrest the effectiveness of ICD should be monitored. If the ICD provides an appropriate shock, that is not successful in correcting VT/VF, ALS should not be delayed. A magnet can be applied during CPR (19) and should remain in situ. Special attention must be given to the person delivering chest compressions following a case report (20) where electrical injury to the rescuers hand was sustained. If any risk to the rescuers is suspected then the ICD should be deactivated with a magnet immediately and standard ALS protocols followed. External pads should be placed 8cm away from the device site preferably use antero- posterior position. The Cardiology SpR or Consultant should be contacted, as soon as possible, for further advice. 6.12.3 The magnets are stored on the cardiac arrest trolleys and should be placed over the ICD using adhesive tape. The ICD site is indicated by scar; usually left infra clavicular or rarely right infra claviclular region. Very rarely ICD may be in abdomen or groin. 6.12.4 Post CPR if there is return of spontaneous circulation leave the magnet in situ until ICD is reprogrammed by a Cardiac Physiologist. If the patient dies then advise mortuary technicians to remove magnet and inform Cardiac Physiologists of patient’s location. 6.12.4 Some ICD devices cannot be deactivated with a magnet. This is rare and if it occurs the patient should be made comfortable with sedation. If it is necessary to identify the device manufacturer the patients are advised to carry information regarding their device at all times. 6.13 Urgent Blood Gas Analysis in Cardiac Arrest And Peri-Arrest Situations on the QAH site For urgent arterial blood gas (ABG) analysis (including potassium) at a cardiac arrest or peri-arrest situation in the East Ward Block (Old Hospital) the blood gas sample can be taken to the Emergency Department for testing. For urgent blood gas analysis (including potassium) at a cardiac arrest or peri-arrest situation in the South Ward Block (New Hospital) the blood gas sample can be taken to the Department of Critical Care (E5) for testing. All non-urgent ABG's should be taken to the Pathology Laboratory (Path Lab) having ensured the samples and forms are fully and correctly labelled at the bedside. The blood gas machine in the Path Lab cannot provide a potassium result and therefore a serum potassium sample should also be taken if required. To save time in emergency situations, there are blank biochemistry/haematology request forms on all the cardiac arrest trolleys. The blood gas syringes compatible with all analyzing machines is the Radiometer PICO70 syringes. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 14 of 33 All non-urgent blood gases should continue to be sent to the Pathology Laboratory in the usual way. 7. TRAINING REQUIREMENTS 7.1 The strategy for resuscitation training embodies the statements and guidelines published by the Resuscitation Council (UK) and the European Resuscitation Council, incorporating the most recent updates to these guidelines. This explicitly incorporates current Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) policy, the identification of patients at risk from cardiac arrest and a strategic approach to implement preventative measures such as Early Warning Systems/ Patient at Risk Systems. The Trust will provide sufficient and appropriate resuscitation training for all clinical staff to attend annually. Profession specific resuscitation training will be directed by their respective functional role and the guidelines and directives issued by their professional bodies (e.g. The Royal College of Anaesthetists). All clinical staff are trained in the identification of the deteriorating and critically ill patients and the use of physiological observation charts to enhance decision making and care escalation. This is included in annual resuscitation training updates to a level relevant to the staff role. The profession specific guidelines for resuscitation training are detailed in the Training Needs Analysis (Appendix 1). The uptake of training monitored monthly through the reports from Learning and Development Department to all Clinical Service Centres (CSC’s). Clinical Staff All doctors, nurses, midwives and Allied Health Professionals must be trained annually in cardiopulmonary resuscitation to a level appropriate to their clinical roles and responsibilities. The level of that training is determined by their respective professional bodies (e.g. General Medical Council) and/or the duties that those staff would be expected to undertake when in attendance at a cardiac arrest/medical/obstetric/neonatal emergency. This is detailed in the Training Needs Analysis (Appendix 1). Non-Clinical Staff All hospital staff with frequent, regular unsupervised (by clinical staff) contact with patients should be trained in basic life support (BLS). 8. REFERENCES AND ASSOCIATED DOCUMENTATION 1. Resuscitation Council (UK) (2013) quality standards for cardiopulmonary resuscitation 2. 3. 4. 5. 6. 7. practice and training. Resuscitation Council (UK) - Quality standards for CPR National Confidential Enquiry into patient Outcome and Death – Time to Intervene (2012) NCEPOD - CAP: Time to Intervene? Report (2012) Resuscitation Guidelines (UK) 2010. http://www.resus.org.uk/pages/guide.htm PHT Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) Policy. Located on the intranet under clinical policies. http://pht/PoliciesGuidelines/ClinicalPolicies/default.aspx PHT Management of the Deteriorating Patient Policy. Located on the intranet under clinical policies. http://pht/PoliciesGuidelines/ClinicalPolicies/default.aspx Resuscitation Council (UK) (2008) Emergency treatment of anaphylactic reactions. Guidelines for healthcare providers. Resuscitation Council (UK): London http://www.resus.org.uk/pages/mediMain.htm PHT Neonatal Resuscitation Maternity Policy. Located on the intranet. Departments – Maternity – Maternity Services Guidelines Neonatal Resuscitation Maternity Services Policy Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 15 of 33 8. Current PHT Resuscitation BLS & ALS equipment Recommendations and daily checklists are located on PHT Resuscitation intranet site. Departments – Resuscitation. Resuscitation Equipment Lists and Forms 9. Procedural Documents Development And Management Policy. Located on the intranet under management policies. http://pht/PoliciesGuidelines/ManagementPolicies/default.aspx 10. PHT Medical Devices Management Policy. Located on the intranet under management policies. http://pht/PoliciesGuidelines/ManagementPolicies/default.aspx 11. NICE Clinical Guideline 50. Acutely ill patients in hospital. Recognition of and response to acute illness in adults in hospital. July 2007. http://guidance.nice.org.uk/CG50 12. PHT First Aid at Work Policy. Located on the intranet under health and safety policies. http://pht/PoliciesGuidelines/HealthandSafetyPolicies/default.aspx?PageView=Shared 13. PHT Adverse Incident and Near Misses Management policy. Located on the intranet under management policies. http://pht/PoliciesGuidelines/ManagementPolicies/default.aspx 14. Emergency Drug Cupboard List is located on PHT intranet – Departments – Pharmacy - Out of hours. http://pharmweb/Closed/emergencydrugcupboards.asp 15. PHT People Moving and Handling policy. Located on the intranet under clinical policies. http://pht/PoliciesGuidelines/ClinicalPolicies/default.aspx 16. Resuscitation Council (UK) (2009) Guidance for Safer Handling during Resuscitation in healthcare settings. http://www.resus.org.uk/pages/mediMain.htm 17. Portsmouth Hospitals Trust. Patient Group Directions for Adrenaline (Epinephrine) Injection BP 1:1000 PGD Ref No: RSS 003. Current version is located on the intranet – Departments – Pharmacy – PGD’s http://pharmweb/FMG/PGD/Database/ 18. PHT Competency Statements on Adult and Paediatric Anaphylaxis. PHT intranet. Learning and Development Zone, Nursing and Midwifery. Generic Nursing and Midwifery Competency Framework 19. Nolan JP et al. Part 1: Executive summary: 2010 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2010;81:e1-e25. 20. Stockwell B., Bellis G., Morton G., Chung K., Merton W. L., Andrews N. P., Smith G. B. Case report. Electrical injury during “hands on” defibrillation—A potential risk of internal cardioverter defibrillators? Resuscitation 2009;80;832-4 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 16 of 33 10. MONITORING COMPLIANCE The document will be monitored to ensure it is effective and to assurance compliance. As a minimum, the following elements will be monitored. Minimum requirement to be monitored Lead Tool Frequency of Reporting of Compliance 100% of Cardiac Arrest are audited using the Cardiac Arrest Record Form and entered in to the National Cardiac Arrest Audit (NCAA) Resuscitation Manager PHT Cardiac Arrest Record Form based on the Utstein Template (Appendix 5) Annually Continual availability of resuscitation equipment: equipment will be available at all times Resuscitation Manager Current Resuscitation Equipment Standards (8) Annually 85% of staff will attend Basic Life Support training annually as set out in training needs analysis Learning and Development Business Manager Audit of Electronic Staff Record Annually Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Reporting arrangements Policy & NCAA Audit Report Resuscitation Committee quarterly Patient Safety Working Group quarterly Policy Audit Report to Page 17 of 33 Resuscitation Manager Resuscitation Manager Resuscitation Committee Policy Audit Report Lead(s) for acting on recommendations Resuscitation Committee CSC Heads of Nursing / Chiefs of Service Resuscitation Training Needs Analysis for staff with frequent, regular contact with patients Appendix 1 Minimum standard for all clinical staff and non-clinical staff with frequent, regular contact with patients As a minimum standard all clinical staff with direct Adult patient contact must attend Adult Basic Life Support (BLS) annually. As a minimum standard all clinical staff with direct Paediatric patient contact must attend Paediatric Basic Life Support (BLS) annually. As a minimum standard all clinical staff with direct Newborn patient contact must attend Newborn Life Support annually. As a minimum standard all clinical staff with direct Maternal patient contact must attend Maternal Basic Life Support (BLS) annually. Annual Resuscitation Training for Registered Nursing/Midwifery/AHP’s with Direct Patient Contact PHT Adult BLS PHT Paed BLS PHT CSSD PHT Adult BLS & AED Anaphylaxis Training if administering medicines RC (UK) ALS Provider Course Registered Staff in M D M D Adult Critical Care Every 2 Areas years Registered Staff in M D M Acute Adult Ward Every 2 Areas years Registered Staff in M M M Community Hospitals Registered Staff in M M Adult non-ward clinical areas Registered Staff in M M M Paediatric Areas Registered Staff in M M Newborn Areas Registered staff in M M Maternity Areas BLS = Basic Life Support CSSD = Critical Skills Study Day ILS = Immediate Life Support EPLS = European Paediatric Life Support NICU = Neonatal Intensive Care Unit M = Mandatory on an annual basis Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) RC (UK) ILS Course EPLS/ APLS Course RC (UK) pILS Course RC (UK) Newborn Life Support Course PHT NICU Resuscitation Training Programme PHT Maternal BLS and anaphylaxis PHT Newborn Life Support Update D D D D D M M M AED = Automated External Defibrillation APLS = Advanced Paediatric Life Support D = Desirable Page 18 of 33 M ALS = Advanced Life Support pILS= Paediatric Immediate Life Support Blank = Not Applicable Appendix 1 cont. Annual Resuscitation Training for Medical Staff with Direct Patient Contact Adult BLS Paed BLS PHT Adult ALS Anaphylaxis Training if administering medicines RC (UK) ALS Provider Course M M FY1(D) M D D D M M PHT Adult Manual/AED Defibrillation EPLS/ APLS Course Medical Staff On Adult Cardiac Arrest Team All Other Medical Staff with direct adult patient contact Anaesthetists M M M M Medical Staff On Paediatric Cardiac Arrest Team All Other Medical Staff with direct paed patient contact Medical Staff On Neonatal Emergency Response Team All Other Medical Staff with direct Neonatal patient contact Medical Staff On Maternal Emergency Response Team All Other Medical Staff with direct Maternal patient contact M M M M M M M D M RC (UK) pILS Course PHT Paed Manual Defibrillation and Anaphylaxis RC (UK) Newborn Life Support Course NICU Resuscitation Training Programme Maternal BLS M D D D D D D D M M M M M M M M M M D M M = Mandatory on an annual basis M D = Desirable Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Blank = Not Applicable Page 19 of 33 M Appendix 2 Resuscitation Council (UK) Anaphylaxis Treatment Algorithm Cardiopulmonary Resuscitation Issue 13 25th April 2014 th (Review date: 24 April 2017 unless requirements change) Page 20 of 33 Appendix 2 cont Investigations post anaphylactic/severe allergic reaction When a patient experiences an adverse event that is thought to be a possible anaphylactic or anaphylactoid reaction, ensure that the following basic samples are obtained: An EDTA plasma (purple top) or serum sample (red or yellow top) for tryptase estimation (one bottle will suffice) Sample As soon as possible after, or within one hour of, onset of the reaction. 1 Sample 2 3 hours post-reaction Sample 3 24 hours post-reaction (required to act as a baseline to exclude mastocytosis). Sample transport These samples can be transported at room temperature to the laboratory where they will be stored until the series is received. Interpretation of results Peak tryptase level Systolic BP (mmHg) >50ug/L Unrecordable Type I Hypersensitivity (drug history required for allergen specific IgE studies). 2050ug/L 20-80 Non-immune anaphylactoid reaction either (i) direct release by pharmacologically active drugs or (ii) complement activation. 2-20ug/L 100-120 Probable bronchospasm NB: It is very important to tell the lab when samples were taken in relation to the precipitating event. Sometimes, they will add a total IgG, which should not change acutely. Any changes in IgG over a short period of time, may indicate that a peak tryptase might be underestimated following any acute fluid administration. There will be occasions when this protocol is unworkable and a single blood sample taken post mortem for example, may still be of value in the investigation of underlying causative pathology. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 21 of 33 Appendix 3 Cardiac Arrest and Emergency Response Teams Table 1. ADULT Cardiac Arrest Team at Queen Alexandra Hospital Team Medical SpR/ST3 and above Resuscitation Committee recommended minimum training standard ALS & PHT ALS Medical SHO/FY2/ST1 & 2 ALS & PHT ALS Medical FY1/FY2 PHT ALS/ILS (ALS desirable) Doctor from DCCQ PHT ALS Department Nurse / AHP BLS/CSSD/ILS Specialty Nurse Bleep Holder CSSD/ILS Emergency Number 2222 State Cardiac Arrest Team and location Table 2. PAEDIATRIC Cardiac Arrest Team at Queen Alexandra Hospital Team Paediatric SpR/ST3 and above Resuscitation Committee recommended minimum training standard APLS/EPLS Paediatric SHO/ ST1&2 pILS/EPLS SpR from DCCQ EPLS/APLS Paediatric Nurse Bleep Holder pILS Department Nurse / PAM Adult & Paed BLS/CSSD/ILS Emergency Number 2222 State Paediatric Cardiac Arrest Team and location Table 3: NEONATAL Crisis Team at Queen Alexandra Hospital Team Resuscitation Committee recommended minimum training standard Neonatal Consultant NLS Neonatal SpR/ST3 and above NLS Neonatal SHO/FY2/ST1&2 NLS NLS or NICU Resuscitation Training programme NLS or NICU Resuscitation Training programme & Adult BLS Department Nurse Nurse in Charge of each Shift Cardiopulmonary Resuscitation Issue 13 25th April 2014 th (Review date: 24 April 2017 unless requirements change) Emergency Number 2222 State Neonatal Crisis Team Page 22 of 33 Table 4: Response to Maternal Cardiac Arrests at Queen Alexandra Hospital Team Resuscitation Committee recommended minimum training standard Emergency Number Medical SpR/ST3 and above ALS & PHT ALS Medical SHO/FY2/ST1 & 2 ALS & PHT ALS Medical FY1 PHT ALS/ILS (ALS desirable) 2222 State Maternal Crisis Team and Cardiac Arrest Team and location Doctor from DCCQ PHT ALS Adult Cardiac Arrest Team Maternity Crisis Team Department Midwife/AHP Maternal BLS Maternity Bleep Holder Maternal BLS Maternity Anaesthetist ALS & PHT ALS Gynaecology SpR BLS & Defib Obstetric SpR BLS & Defib Anaesthetic ODP BLS If requested the Neonatal Crisis Team Neonatal Consultant NLS Neonatal SpR/ST3 and above NLS Neonatal SHO/FY2/ST1&2 NLS ALS = Resuscitation Council (UK) Advanced Life Support Course Provider PHT ALS= PHT Advanced Life Support for the Cardiac Arrest Team CSSD= PHT Critical Skills Study Day ILS= Resuscitation Council (UK) Immediate Life Support Course APLS = Advanced Paediatric Life Support Course Provider EPLS= Resuscitation Council (UK) European Paediatric Life Support Course Provider pILS = Resuscitation Council (UK) Paediatric Immediate Life Support Course NLS = Resuscitation Council (UK) Newborn Life Support Course NICU = PHT Neonatal Intensive Care Unit Table 5: Emergency Response in PHT Community sites Team Resuscitation Committee recommended minimum training standard Emergency Number Clinical areas BLS & AED Site specific Non-clinical areas BLS Site specific Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 23 of 33 Table 6: Availability of Cardiac Arrest equipment to non-clinical areas on the Queen Alexandra Hospital Site. Equipment Provided By: For A, B & C Level corridors in the East Ward Block (‘Old Hospital’) the Emergency Department (ED) staff will respond with cardiac arrest equipment For D, E, F & G Level corridors in the East Ward Block (‘Old Hospital’) the nearest clinical area will provide the equipment For A, B, C, D, E, F and G Level corridors in the South Ward Block (‘New Hospital’) the nearest clinical area will provide the equipment Main Entrance, Retail Shop and Coffee Shop, A Level North Entrance, C Level Education Centre, E Level Place of Safety Emergency Department (ED) The nearest clinical area. The clinical staff and cardiac arrest team would then arrange the continuing care and carry out safe transfer if required. The nearest clinical area. The clinical staff and cardiac arrest team would then arrange the continuing care and carry out safe transfer if required. Adult BLS equipment including an AED & oxygen have been placed behind Main Reception. A Cardiac Arrest trolley can be obtained from Paediatric Outpatient Department. The cardiac arrest team would then arrange the continuing care and carry out safe transfer if required. Adult BLS equipment including an AED & oxygen are in Medical OPD. A Cardiac Arrest trolley can be obtained from Orthopaedic Outpatients. The cardiac arrest team would then arrange the continuing care and carry out safe transfer if required. Adult BLS equipment including an AED is held at the Education Centre reception. A Cardiac Arrest trolley can be obtained from E8 Ward. The cardiac arrest team would then arrange the continuing care and carry out safe transfer if required. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 24 of 33 Appendix 4 Minimum Personnel, Skills and Knowledge Levels for Queen Alexandra Hospital Cardiac Arrest Teams (CAT) The CAT should consist of 4 members – a team leader, airway technician, circulation technician and one assistant (1). Team Leader: must • Possess a current Resuscitation Council (UK) Advanced Life Support course certificate • Be able to recognise cardiac arrest • Be able to provide basic life support • Possess a thorough understanding of the current RC (UK) guidelines for the treatment of cardiac arrest • Possess basic and advanced airway management skills to include use of: o Use of simple airway opening manoeuvres o Use of oral and nasopharyngeal airway adjuncts o Use of laryngeal mask airway o Tracheal intubation (preferred) o Suction of the upper and lower airway • Possess following skills relating to breathing: o Use of pocket mask o Use of bag /valve / mask devices (manual resuscitators) o Use of oxygen therapy in emergency care • Possess following skills relating to the circulation: o Peripheral intravenous (IV) cannulation o Central vein cannulation (preferred) o Defibrillation and synchronised cardioversion • Possess an understanding of current drug therapy for cardiac arrest • Possess an understanding of current treatments for peri-arrest arrhythmias • Be able to organise and co-ordinate the efforts of the cardiac arrest team • Understand the ethics of resuscitation, including “Do not attempt cardiopulmonary resuscitation” and “treatment limitation” decisions • Know and understand current Portsmouth Hospitals Trust policies relating to resuscitation: o Cardiopulmonary Resuscitation policy o Do not attempt cardiopulmonary resuscitation policy • Must possess good communication skills permitting the transfer of information to staff, the relatives of cardiac arrest victims and, where appropriate, the victims themselves. • Must complete a Cardiac Arrest Record Form for each cardiac arrest event • Must lead the organisation of the following o Post arrest investigations o Post arrest transfer to coronary care unit and critical care o Inter hospital transfer Team member (Airway & Breathing technician) • Must be able to recognise cardiac arrest • Must be able to provide basic life support • Must possess an understanding of the current RC (UK) guidelines for the treatment of cardiac arrest • Must possess basic and advanced airway management skills to include use of: o Simple airway opening manoeuvres o Oral and nasopharyngeal airway adjuncts o Laryngeal mask airway o Tracheal intubation, including the use of intravenous sedative and paralysing drugs o Suction of the upper and lower airway • Must possess following skills relating to breathing: o Use of pocket mask o Use of bag /valve / mask devices (manual resuscitators) Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 25 of 33 • • • • • o Use of oxygen therapy in emergency care Must understand the ethics of resuscitation, including “Do not attempt cardiopulmonary resuscitation” and “treatment limitation” decisions Must know and understand current Portsmouth Hospitals Trust policies relating to resuscitation: o Cardiopulmonary Resuscitation policy o Do not attempt cardiopulmonary resuscitation policy Must possess good communication skills permitting the transfer of information to staff, the relatives of cardiac arrest victims and, where appropriate, the victims themselves. Must participate in the completion a Cardiac Arrest Record Form for each cardiac arrest event Must participate in the organisation of the following o Post arrest investigations o Post arrest transfer to coronary care unit and critical care o Inter hospital transfer Team member (Circulation technician) • Must be able to recognise cardiac arrest • Must be able to provide basic life support • Must possess an understanding of the current RC (UK) guidelines for the treatment of cardiac arrest • Must possess basic airway management skills to include use of: o Use of simple airway opening manoeuvres o Use of oral and nasopharyngeal airway adjuncts o Suction of the upper and lower airway • Must possess following skills relating to breathing: o Use of pocket mask o Use of bag /valve / mask devices (manual resuscitators) o Use of oxygen therapy in emergency care • Must possess following skills relating to the circulation: o Peripheral intravenous (IV) cannulation o Central vein cannulation (preferred) o Defibrillation and synchronised cardioversion • Must understand the ethics of resuscitation, including “Do not attempt cardiopulmonary resuscitation” and “treatment limitation” decisions • Must know and understand current Portsmouth Hospitals Trust policies relating to resuscitation: o Cardiopulmonary Resuscitation policy o Do not attempt cardiopulmonary resuscitation policy • Must possess good communication skills permitting the transfer of information to staff, the relatives of cardiac arrest victims and, where appropriate, the victims themselves. • Must participate in the completion a Cardiac Arrest Record Form for each cardiac arrest event • Must participate in the organisation of the following o Post arrest investigations o Post arrest transfer to coronary care unit and critical care o Inter hospital transfer 1 other Team Member (assistant) • Must be able to recognise cardiac arrest • Must be able to provide basic life support • Must possess an understanding of the current RC (UK) guidelines for the treatment of cardiac arrest • Must possess basic and advanced airway management skills to include use of: o Use of simple airway opening manoeuvres o Use of oral and nasopharyngeal airway adjuncts o Suction of the upper and lower airway • Must possess ability to assist airway technician (see above) • Must possess following skills relating to breathing: Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 26 of 33 • • • • • • o Use of pocket mask o Use of bag /valve / mask devices (manual resuscitators) o Use of oxygen therapy in emergency care Must possess ability to assist circulation technician (see above) Must possess an understanding of current drug therapy for cardiac arrest Must understand the ethics of resuscitation, including “Do not attempt cardiopulmonary resuscitation” and “treatment limitation” decisions Must know and understand current Portsmouth Hospitals Trust policies relating to resuscitation: o Cardiopulmonary Resuscitation policy o Do not attempt cardiopulmonary resuscitation policy Must possess good communication skills permitting the transfer of information to staff, the relatives of cardiac arrest victims and, where appropriate, the victims themselves. Must participate in the completion of a Cardiac Arrest Record Form for each cardiac arrest event Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 27 of 33 Appendix 5 Queen Alexandra Site Cardiac Arrest Record Form Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 28 of 33 Appendix 5 cont Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 29 of 33 Appendix 5 cont Community Sites Cardiac Arrest Record Form Cardiopulmonary Resuscitation Issue 13 25th April 2014 th (Review date: 24 April 2017 unless requirements change) Page 30 of 33 Appendix 5 cont Community Sites Cardiac Arrest Record Form cont Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 31 of 33 Appendix 6 Electrical equipment safety during defibrillation Electrical equipment safety during defibrillation is important for its effectiveness, the rescuers safety and to avoid potential damage to machinery. Electrical current predominantly takes the path of least resistance. During defibrillation the intended destination of the current is from one pad, through the thorax and the myocardium to the other pad. If another route is available, i.e. there is equipment attached to the patient, the current may follow that route. In addition, the intended current pathway can be disturbed by the presence of other devices connected to the patient. If aberrant pathways are taken this may lead to insufficient depolarisation of the myocardium and as a consequence defibrillation may not be successful. It is recommended that all equipment (For example ECG machines, IV pumps, haemodialysis machines etc) is disconnected from the patient receiving defibrillation, but this must not delay the shock being given. Medical equipment that has some degree of protection from defibrillation is marked with either of the bottom two symbols however it is still recommended that this equipment be detached for the reasons identified above. If medical equipment has been attached to the patient during defibrillation and you are concerned about it’s function, contact the Clinical Engineering Department for advice. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 32 of 33 Appendix 7 Defibrillation during renal replacement therapy using vascular access This guidance outlines the specialty specific actions to be taken by Health Care Professionals, should a patient have a cardiopulmonary arrest during haemodialysis (RRT) or any other renal replacement therapy using vascular access (RRT). This should be used in conjunction with the PHT Cardiopulmonary Resuscitation Policy (1), the Wessex Renal Transplant Service (WRTS) Access management for Haemodialysis (packs 1 and 2) (2) and DCCQ Dialysis Catheter Care Guideline (3) RRT therapy and defibrillation treatment plan Immediately stop the fluid loss on the RRT machine and disconnect patient (2&3). Defibrillation must not be delayed by attempting to return the blood held in the extra corporeal circuit If the patient does not require defibrillation: Immediately stop the fluid loss on the RRT machine. Discontinue the RRT as soon as possible (2&3) Rationale 1. Disconnection from RRT machine removes risk of aberrant current pathways & associated risks to staff, patient and machinery. 2. Blood held in the extra corporeal circuit can be returned back to the patient (2&3).This process must not delay defibrillation. 3. If blood is not returned, the patient may be affected by hypovolaemia. However this can be managed with fluid replacement therapy during the cardiac arrest. Care of Vascular access During the cardiac arrest maintain vascular access patency (2&3). Leave one lumen of the central venous catheter free for immediate use or leave a fistula needle in situ if no other iv access can be obtained. Ensure the lumen to be used is flushed with normal saline, clamped, and the end closed between uses. The lumen of the central venous catheter that is not used needs to be flushed and locked as per the Renal Standard Operating Procedure for the Medical Device Duralock – c (Trisodium citrate) Renal PGD’s . Ensure the fistula needle to be used is flushed and kept patent as per the Renal Patient Group Direction for Sodium Chloride Injection B 0.9% for flushing Renal PGD’s , then clamped and closed with a cap. Community Haemodialysis (HD) If the fistula needle is left in situ or the HD line lumen is being used as access, this must be handed over to the paramedic staff. A care sheet should be sent to the hospital to inform the staff looking after the patient. Continuing Care Continue Care as per Portsmouth Hospitals NHS Trust Cardiopulmonary Resuscitation Policy (including Anaphylaxis and Defibrillation) (1). References 1. Current PHT Cardiopulmonary Resuscitation 2. Wessex Renal Transplant Service (WRTS) Access management for Haemodialysis (packs 1 and 2). Authors Sarah Kattenhorn & Siobhan Gladding (contact PHT Renal Unit). 3. Current PHT DCCQ Dialysis Catheter Care Guideline DCCQ Dialysis Catheter Care Guideline. Cardiopulmonary Resuscitation Issue 13 25th April 2014 (Review date: 24th April 2017 unless requirements change) Page 33 of 33