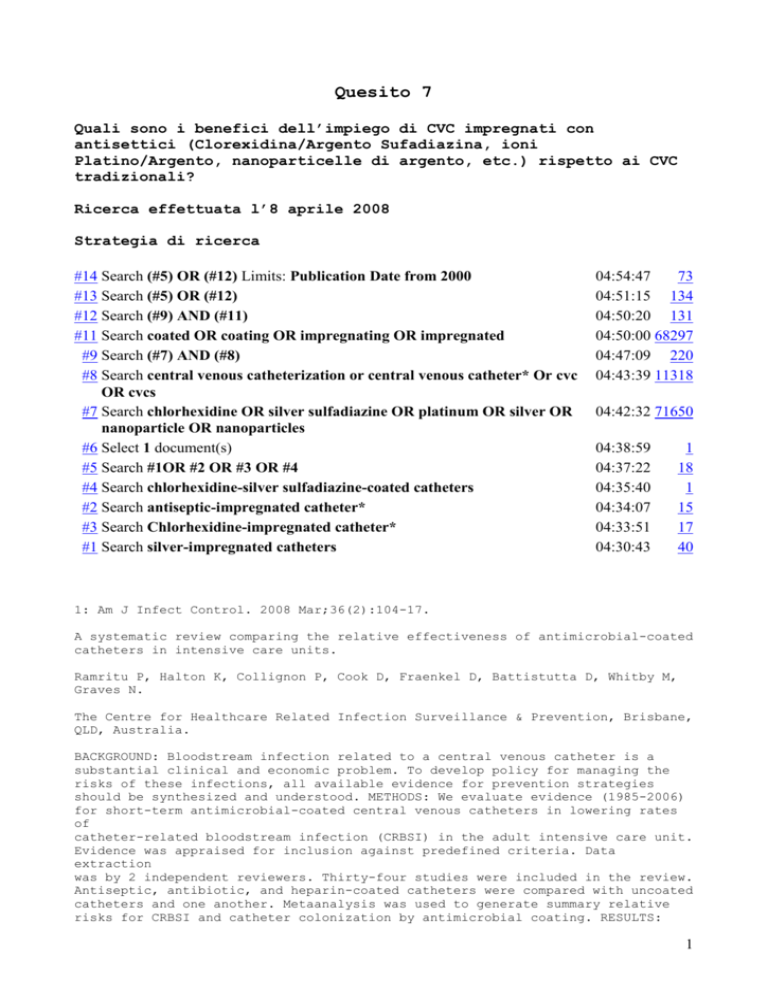
Quesito 7
Quali sono i benefici dell’impiego di CVC impregnati con
antisettici (Clorexidina/Argento Sufadiazina, ioni
Platino/Argento, nanoparticelle di argento, etc.) rispetto ai CVC
tradizionali?
Ricerca effettuata l’8 aprile 2008
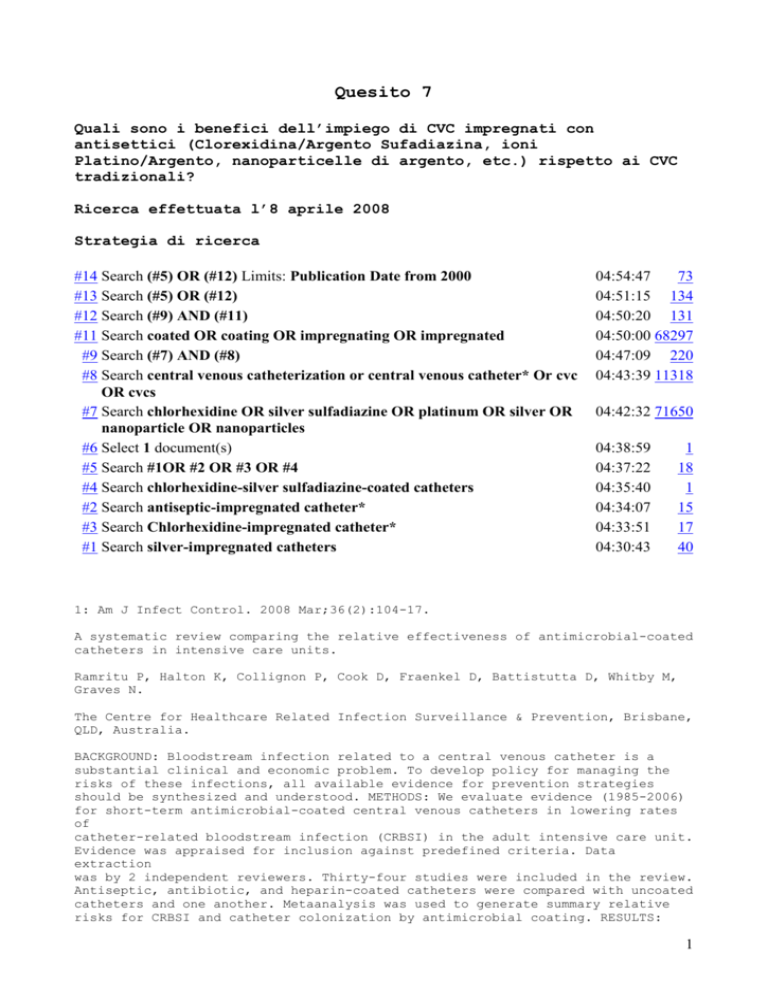
Strategia di ricerca
#14 Search (#5) OR (#12) Limits: Publication Date from 2000
#13 Search (#5) OR (#12)
#12 Search (#9) AND (#11)
#11 Search coated OR coating OR impregnating OR impregnated
#9 Search (#7) AND (#8)
#8 Search central venous catheterization or central venous catheter* Or cvc
OR cvcs
#7 Search chlorhexidine OR silver sulfadiazine OR platinum OR silver OR
nanoparticle OR nanoparticles
#6 Select 1 document(s)
#5 Search #1OR #2 OR #3 OR #4
#4 Search chlorhexidine-silver sulfadiazine-coated catheters
#2 Search antiseptic-impregnated catheter*
#3 Search Chlorhexidine-impregnated catheter*
#1 Search silver-impregnated catheters
04:54:47
73
04:51:15 134
04:50:20 131
04:50:00 68297
04:47:09 220
04:43:39 11318
04:42:32 71650
04:38:59
04:37:22
04:35:40
04:34:07
04:33:51
04:30:43
1
18
1
15
17
40
1: Am J Infect Control. 2008 Mar;36(2):104-17.
A systematic review comparing the relative effectiveness of antimicrobial-coated
catheters in intensive care units.
Ramritu P, Halton K, Collignon P, Cook D, Fraenkel D, Battistutta D, Whitby M,
Graves N.
The Centre for Healthcare Related Infection Surveillance & Prevention, Brisbane,
QLD, Australia.
BACKGROUND: Bloodstream infection related to a central venous catheter is a
substantial clinical and economic problem. To develop policy for managing the
risks of these infections, all available evidence for prevention strategies
should be synthesized and understood. METHODS: We evaluate evidence (1985-2006)
for short-term antimicrobial-coated central venous catheters in lowering rates
of
catheter-related bloodstream infection (CRBSI) in the adult intensive care unit.
Evidence was appraised for inclusion against predefined criteria. Data
extraction
was by 2 independent reviewers. Thirty-four studies were included in the review.
Antiseptic, antibiotic, and heparin-coated catheters were compared with uncoated
catheters and one another. Metaanalysis was used to generate summary relative
risks for CRBSI and catheter colonization by antimicrobial coating. RESULTS:
1
Externally impregnated chlorhexidine/silver sulfadiazine catheters reduce risk
of
CRBSI relative to uncoated catheters (RR, 0.66; 95% CI: 0.47-0.93). Minocycline
and rifampicin-coated catheters are significantly more effective relative to
CHG/SSD catheters (RR, 0.12; 95% CI: 0.02-0.67). The new generation
chlorhexidine/silver sulfadiazine catheters and silver, platinum, and
carbon-coated catheters showed nonsignificant reductions in risk of CRBSI
compared with uncoated catheters. CONCLUSION: Two decades of evidence describe
the effectiveness of antimicrobial catheters in preventing CRBSI and provide
useful information about which catheters are most effective. Questions
surrounding their routine use will require supplementation of this trial
evidence
with information from more diverse sources.
Publication Types:
Meta-Analysis
Research Support, Non-U.S. Gov't
PMID: 18313512 [PubMed - indexed for MEDLINE]
2: Int Wound J. 2008 Jan 18 [Epub ahead of print]
Use of chlorhexidine-impregnated patch at pin site to reduce local morbidity:
the
ChIPPS Pilot Trial.
Wu SC, Crews RT, Zelen C, Wrobel JS, Armstrong DG.
Scholl’s Center for Lower Extremity Ambulatory Research (CLEAR), Rosalind
Franklin University of Medicine, Chicago, IL 60064, USA.
Pin tract infection is one of the most common complications associated with the
use of external fixation. While some studies have identified the potential
benefit of chlorhexidine gluconate-impregnated polyurethane dressings to reduce
the incidence of catheter-related bloodstream infections, we are unaware of any
published studies that evaluate the effectiveness of similar technologies in
reducing the risk for external-fixation-related pin tract infections. Therefore,
the purpose of this study was to evaluate the effectiveness of chlorhexidine
gluconate-impregnated polyurethane dressing in reducing
percutaneous-device-related skin colonisation and local infections. In this
initial retrospective cohort, data were abstracted for two groups of consecutive
patients undergoing surgery involving external fixation at an interdisciplinary
foot and ankle surgical unit. All patients received surgical treatment of their
foot/ankle pathology along with application of a hybrid external fixator. Twenty
patients (45% male, age 54.5 +/- 3.69 years) received chlorhexidine
gluconate-impregnated polyurethane dressing and twenty (55% male, age 55.8 +/3.22 years) received standard pin care. There was a significantly higher rate of
pin tract infection in patients who received standard pin care compared with
those who received chlorhexidine gluconate-impregnated polyurethane dressings
(25% versus 0%, P = 0.047). There was no significant difference in any of the
descriptive study characteristics (age, gender, diabetes and presence of
neuropathy). The results of this initial study suggest that chlorhexidine
gluconate-impregnated polyurethane dressing may be effective to reduce the
incidence of pin tract infections and help decrease morbidity associated with
external fixation.
PMID: 18205786 [PubMed - as supplied by publisher]
3: Surg Infect (Larchmt). 2007 Aug;8(4):445-54.
Effect of chlorhexidine/silver sulfadiazine-impregnated central venous catheters
in an intensive care unit with a low blood stream infection rate after
implementation of an educational program: a before-after trial.
2
Schuerer DJ, Zack JE, Thomas J, Borecki IB, Sona CS, Schallom ME, Venker M,
Nemeth JL, Ward MR, Verjan L, Warren DK, Fraser VJ, Mazuski JE, Boyle WA,
Buchman
TG, Coopersmith CM.
Department of Surgery, Washington University School of Medicine, St. Louis,
Missouri 63110, USA.
BACKGROUND: Current guidelines recommend using antiseptic- or
antibiotic-impregnated central venous catheters (CVCs) if, following a
comprehensive strategy to prevent catheter-related blood stream infection
(CR-BSI), infection rates remain above institutional goals based on benchmark
values. The purpose of this study was to determine if chlorhexidine/silver
sulfadiazine-impregnated CVCs could decrease the CR-BSI rate in an intensive
care
unit (ICU) with a low baseline infection rate. METHODS: Pre-intervention and
post-intervention observational study in a 24-bed surgical/trauma/burn ICU from
October, 2002 to August, 2005. All patients requiring CVC placement after March,
2004 had a chlorhexidine/silver sulfadiazine-impregnated catheter inserted
(post-intervention period). RESULTS: Twenty-three CR-BSIs occurred in 6,960
catheter days (3.3 per 1,000 catheter days)during the 17-month control period.
After introduction of chlorhexidine/silver sulfadiazine-impregnated catheters,
16
CR-BSIs occurred in 7,732 catheter days (2.1 per 1,000 catheter days; p = 0.16).
The average length of time required for an infection to become established after
catheterization was similar in the two groups (8.4 vs. 8.6 days; p = 0.85).
Chlorhexidine/silver sulfadiazine-impregnated catheters did not result in a
statistically significant change in the microbiological profile of CR-BSIs, nor
did they increase the incidence of resistant organisms. CONCLUSIONS: Although
chlorhexidine/silver sulfadiazine-impregnated catheters are useful in specific
patient populations, they did not result in a statistically significant decrease
in the CR-BSI rate in this study, beyond what was achieved with education alone.
Publication Types:
Clinical Trial
Research Support, N.I.H., Extramural
Research Support, U.S. Gov't, P.H.S.
PMID: 17883361 [PubMed - indexed for MEDLINE]
4: Curr Opin Infect Dis. 2007 Aug;20(4):360-9.
Prevention of intravascular catheter infection.
Eggimann P.
Department of Adult Intensive Care Medicine and Burn Centre, Centre Hospitalier
Universitaire Vaudois (CHUV), Lausanne, Switzerland. philippe.eggimann@chuv.ch
PURPOSE OF REVIEW: To review recent evidence supporting the guidelines for
preventing catheter-related and catheter-associated infections. RECENT FINDINGS:
A series of studies has confirmed, over the past few years, that education-based
preventive programmes can reduce these infections by one half to two thirds. The
evidence supporting some specific measures has increased for the optimal timing
for set replacement, for catheter-site dressing with chlorhexidine-impregnated
devices, and for the use of some coated or impregnated intravascular devices.
SUMMARY: Catheter-related and associated infections are largely preventable and
should not be viewed as an unaffordable tribute to technical medicine.
Improvements in existing techniques and new technologies should all be
integrated
into a structured process of continuous improvement in the quality of care.
3
Publication Types:
Review
PMID: 17609594 [PubMed - indexed for MEDLINE]
5: Curr Opin Crit Care. 2007 Aug;13(4):411-5.
Prevention of catheter-related blood stream infection.
Byrnes MC, Coopersmith CM.
Department of Surgery, Washington University School of Medicine, St. Louis,
Missouri, USA.
PURPOSE OF REVIEW: Catheter-related blood stream infections are a morbid
complication of central venous catheters. This review will highlight a
comprehensive approach demonstrated to prevent catheter-related blood stream
infections. RECENT FINDINGS: Elements of prevention important to inserting a
central venous catheter include proper hand hygiene, use of full barrier
precautions, appropriate skin preparation with 2% chlorhexidine, and using the
subclavian vein as the preferred anatomic site. Rigorous attention needs to be
given to dressing care, and there should be daily assessment of the need for
central venous catheters, with prompt removal as soon as is practicable.
Healthcare workers should be educated routinely on methods to prevent
catheter-related blood stream infections. If rates remain higher than benchmark
levels despite proper bedside practice, antiseptic or antibiotic-impregnated
catheters can also prevent infections effectively. A recent program utilizing
these practices in 103 ICUs in Michigan resulted in a 66% decrease in infection
rates. SUMMARY: There is increasing recognition that a comprehensive strategy to
prevent catheter-related blood stream infections can prevent most infections, if
not all. This suggests that thousands of infections can potentially be averted
if
the simple practices outlined herein are followed.
Publication Types:
Review
PMID: 17599011 [PubMed - indexed for MEDLINE]
6: Crit Care Med. 2007 Apr;35(4):1197-9.
Comment on:
Crit Care Med. 2007 Apr;35(4):1032-9.
Antimicrobial coating of central venous catheters: show me the data.
Anaissie E.
Publication Types:
Comment
Editorial
PMID: 17413788 [PubMed - indexed for MEDLINE]
7: J Infus Nurs. 2007 Mar-Apr;30(2):105-12; quiz 120-1.
Implementing evidence-based nursing practice in the pediatric intensive care
unit.
Morgan LM, Thomas DJ.
Nova Southeastern University, Miami, FL, USA. Anchoredsoul@aol.com
4
With the widespread use of central venous catheters in children, the incidence
of
catheter-related bloodstream infections (CR-BSIs) is increasing. Current
evidence-based practice strategies to decrease CR-BSIs include using maximum
barrier techniques during insertion, practicing good hand hygiene, performing
skin antisepsis with 2% chlorhexidine, using a chlorhexidine-impregnated patch
(CIP) covered by a semipermeable polyurethane dressing, and promptly removing
catheters when no longer needed. Implementation of evidence-based practice
bundles, along with monthly monitoring of infection surveillance, has resulted
in
significant decreases in the average rates of CR-BSIs per 1,000 catheter days in
many pediatric intensive care units.
PMID: 17413495 [PubMed - indexed for MEDLINE]
8: Crit Care Med. 2007 Apr;35(4):1032-9.
Comment in:
Crit Care Med. 2007 Apr;35(4):1197-9.
Comparison of silver-impregnated with standard multi-lumen central venous
catheters in critically ill patients.
Kalfon P, de Vaumas C, Samba D, Boulet E, Lefrant JY, Eyraud D, Lherm T, Santoli
F, Naija W, Riou B.
Service de Réanimation Polyvalente, Hôpitaux de Chartres, Chartres, France.
pkalfon@ch-chartres.fr
OBJECTIVES: To evaluate a new silver-impregnated multi-lumen central venous
catheter for reducing catheter-related colonization in intensive care patients.
DESIGN: Multicenter, prospective, randomized, controlled clinical study.
SETTING:
Ten adult intensive care units (multidisciplinary, medical and surgical,
university and nonuniversity hospitals) in eight institutions. PATIENTS: A total
of 577 patients who required 617 multi-lumen central venous catheters between
November 2002 and April 2004 were studied. INTERVENTIONS: Intensive care adult
patients requiring multi-lumen central venous catheters expected to remain in
place for >or=3 days were randomly assigned to undergo insertion of
silver-impregnated catheters (silver group) or standard catheters (standard
group). Catheter colonization was defined as the growth of >or=1,000
colony-forming units in culture of the intravascular tip of the catheter by the
vortexing method. Diagnosis of catheter-related infection was performed by an
independent and blinded expert committee. RESULTS: A total of 320 catheters were
studied in the silver group and 297 in the standard group. Characteristics of
the
patients, insertion site, duration of catheterization (median, 11 vs. 10 days),
and other risk factors for infection were similar in the two groups.
Colonization
of the catheter occurred in 47 (14.7%) vs. 36 (12.1%) catheters in the silver
and
the standard groups (p = .35), for an incidence of 11.2 and 9.4 per 1,000
catheter days, respectively. Catheter-related bloodstream infection was recorded
in eight (2.5%) vs. eight (2.7%) catheters in the silver and the standard groups
(p = .88), for an incidence of 1.9 and 2.1 per 1,000 catheter days,
respectively.
CONCLUSION: The use of silver-impregnated multi-lumen catheters in adult
intensive care patients is not associated with a lower rate of colonization than
the use of standard multi-lumen catheters.
Publication Types:
Comparative Study
Multicenter Study
5
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 17334256 [PubMed - indexed for MEDLINE]
9: BMJ. 2007 Feb 17;334(7589):362-5.
Reduction of bloodstream infections associated with catheters in paediatric
intensive care unit: stepwise approach.
Bhutta A, Gilliam C, Honeycutt M, Schexnayder S, Green J, Moss M, Anand KJ.
Department of Pediatrics, University of Arkansas for Medical Sciences, Arkansas
Children's Hospital, 800 Marshall Street, Slot 512-3, Little Rock, AR 72202,
USA.
bhuttaadnant@uams.edu
PROBLEM: Bloodstream infections associated with catheters were the most common
nosocomial infections in one paediatric intensive care unit in 1994-7, with
rates
well above the national average. DESIGN: Clinical data were collected
prospectively to assess the rates of infection from 1994 onwards. The high rates
in 1994-7 led to the stepwise introduction of interventions over a five year
period. At quarterly intervals, prospective data continued to be collected
during
this period and an additional three year follow-up period. SETTING: A 292 bed
tertiary care children's hospital. KEY MEASURES FOR IMPROVEMENT: We aimed to
reduce our infection rates to below the national mean rates for similar units by
2000 (a 25% reduction). STRATEGIES FOR CHANGE: A stepwise introduction of
interventions designed to reduce infection rates, including maximal barrier
precautions, transition to antibiotic impregnated central venous catheters,
annual handwashing campaigns, and changing the skin disinfectant from
povidone-iodine to chlorhexidine. Effects of change Significant decreases in
rates of infection occurred over the intervention period. These were sustained
over the three year follow-up. Annual rates decreased from 9.7/1000 days with a
central venous catheter in 1997 to 3.0/1000 days in 2005, which translates to a
relative risk reduction of 75% (95% confidence interval 35% to 126%), an
absolute
risk reduction of 6% (2% to 10%), and a number needed to treat of 16 (10 to 35).
LESSONS LEARNT: A stepwise introduction of interventions leading to a greater
than threefold reduction in nosocomial infections can be implemented
successfully. This requires a multidisciplinary team, support from hospital
leadership, ongoing data collection, shared data interpretation, and
introduction
of evidence based interventions.
PMID: 17303886 [PubMed - indexed for MEDLINE]
10: J Antimicrob Chemother. 2007 Mar;59(3):359-69. Epub 2007 Jan 25.
Rifampicin-impregnated central venous catheters: a meta-analysis of randomized
controlled trials.
Falagas ME, Fragoulis K, Bliziotis IA, Chatzinikolaou I.
Alfa Institute of Biomedical Sciences (AIBS), Athens, Greece. m.falagas@aibs.gr
BACKGROUND: The use of antimicrobial-impregnated central venous catheters (CVCs)
for the prevention of CVC microbial colonization and catheter-related
bloodstream
infection (CRBSI) remains controversial. METHODS: We performed a meta-analysis
of
randomized controlled trials (RCTs) evaluating CRBSI and colonization of CVCs
6
impregnated with rifampicin-based antimicrobial combinations. Our main analysis
compared the occurrence of CRBSI with rifampicin/minocycline-impregnated CVCs
with that of non-rifampicin-impregnated CVCs. The PubMed and Cochrane Central
Register of Controlled Trials databases were searched (until October 2006).
RESULTS: Eight RCTs were included in the analysis. The main analysis (seven
RCTs)
demonstrated that rifampicin/minocycline-impregnated CVCs were associated with
fewer CRBSIs compared with catheters not impregnated with rifampicin/minocycline
(OR 0.23, 95% CI 0.14-0.40). The same was true regarding colonization (OR 0.46,
95% CI 0.31-0.69). Further analysis, comparing rifampicin-based CVCs with
non-rifampicin-impregnated CVCs, demonstrated superiority of rifampicin-based
CVCs in reducing colonization (OR 0.38, 95% CI 0.24-0.62) and CRBSI (OR 0.24,
95%
CI 0.14-0.40). Similar results, suggesting superiority of
rifampicin/minocycline-impregnated CVCs, were noted in a subgroup analysis of
colonization and CRBSIs in which rifampicin/minocycline-impregnated CVCs were
compared with simple, non-tunnelled, non-antimicrobially impregnated CVCs, a
subgroup analysis that was performed by excluding low quality RCTs, and a
subgroup analysis for colonization comprising studies in which the sonication
technique was used. No serious adverse events and no difference in mortality
between the two treatment groups were reported. No clear conclusions can be made
regarding the impact of the use of rifampicin/minocycline-impregnated CVCs on
the
development of antimicrobial resistance based on the available data.
CONCLUSIONS:
The available evidence suggests that rifampicin/minocycline-impregnated CVCs are
safe and effective in reducing the rate of catheter colonization and CRBSI.
Further research should focus on the possible development of resistance and on
pharmacoeconomic issues related to the use of rifampicin/minocycline-impregnated
CVCs.
Publication Types:
Meta-Analysis
PMID: 17255143 [PubMed - indexed for MEDLINE]
11: Antimicrob Agents Chemother. 2006 Oct;50(10):3283-8.
Erratum in:
Antimicrob Agents Chemother. 2007 Apr;51(4):1586.
Comparative in vitro efficacies and antimicrobial durabilities of novel
antimicrobial central venous catheters.
Hanna H, Bahna P, Reitzel R, Dvorak T, Chaiban G, Hachem R, Raad I.
University of Texas MD Anderson Cancer Center, Department of Infectious
Diseases,
Infection Control and Employee Health, Houston, TX 77030, USA.
hhanna@mdanderson.org
We investigated the efficacies and durability of novel antimicrobial central
venous catheters (CVCs) in preventing the adherence of microbial organisms to
the
surfaces of the CVCs. Novel antimicrobial CVCs investigated in this in vitro
study were impregnated with antibiotics (minocycline and rifampin), with Oligon
agent (silver, platinum, and carbon black), with approved antiseptics
(chlorhexidine and silver sulfadiazine), or with a novel antiseptic agent,
gendine, which contains gentian violet and chlorhexidine. When tested against
methicillin-resistant Staphylococcus aureus (MRSA) and Pseudomonas aeruginosa,
gendine-coated CVC segments provided protection against bacterial adherence
significantly more than all other types of tested CVCs (P < 0.05). Gendinecoated
7
CVCs also provided better protection against Candida albicans and Candida
parapsilosis than CVCs impregnated with antibiotics or with silver, platinum,
and
carbon (P < 0.02). After 28 days of being soaked in serum, the CVCs impregnated
with chlorhexidine and silver sulfadiazine and the CVCs impregnated with silver,
platinum, and carbon had lost antimicrobial activity against MRSA, P.
aeruginosa,
and C. parapsilosis, and the CVCs impregnated with minocycline and rifampin had
lost activity against P. aeruginosa and C. parapsilosis. The CVCs impregnated
with gendine maintained antimicrobial activities against MRSA, P. aeruginosa,
and
C. parapsilosis after 28 days of being soaked in serum. Central venous catheters
impregnated with the novel investigational antiseptic gendine showed in vitro
efficacy and provided protection against bacterial adherence more than other
approved novel antimicrobial-coated CVCs.
Publication Types:
Comparative Study
Evaluation Studies
PMID: 17005806 [PubMed - indexed for MEDLINE]
12: Am J Infect Control. 2006 Aug;34(6):388-93.
Are antiseptic-coated central venous catheters effective in a real-world
setting?
Borschel DM, Chenoweth CE, Kaufman SR, Hyde KV, VanDerElzen KA, Raghunathan TE,
Collins CD, Saint S.
Department of Internal Medicine, University of Michigan, Ann Arbor, 48109-0376,
USA. dborsche@umich.edu
BACKGROUND: Catheter-related bloodstream infections are common, costly, and
morbid. Randomized controlled trials indicate that antiseptic-coated central
venous catheters reduce infection rates. OBJECTIVE: To assess the clinical and
economic effectiveness of antiseptic-coated catheters for critically ill
patients
in a real-world setting. METHODS: Central venous catheters coated with
chlorhexidine/silver-sulfadiazene were introduced in all patients requiring
central venous access in adult intensive care units at the University of
Michigan
Health System, a large, tertiary care teaching hospital. A pretest-posttest
cohort design measured the primary outcome of catheter-related bloodstream
infection rate, comparing the 2 years prior to the intervention with the 2 years
following the intervention. We also evaluated cost-effectiveness and changes in
vancomycin use. RESULTS: The intervention was associated with a 4% per month
relative reduction in the incidence of catheter-related bloodstream infection,
after controlling for the effects of time. Overall, a 35% relative risk
reduction
(P < .0003) in the catheter-related bloodstream infection rate occurred in the
posttest phase. The use of antiseptic-coated catheters reduced costs more than
$100,000 annually. Vancomycin use was less in units in which antiseptic
catheters
were used compared with wards in which these catheters were not used.
CONCLUSION:
Antiseptic-coated catheters appear to be clinically effective and economically
efficient in a real-world setting.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 16877109 [PubMed - indexed for MEDLINE]
8
13: Adv Chronic Kidney Dis. 2006 Jul;13(3):225-44.
Avoiding trouble down the line: the management and prevention of hemodialysis
catheter-related infections.
Lok CE.
Department of Medicine, Division of Nephrology, University Health NetworkToronto
General Hospital and University of Toronto, Toronto, Ontario, Canada.
charmaine.lok@uhn.on.ca
Over the last 2 decades, hemodialysis catheter use has increased. Annually,
approximately 30% of patients using a central venous catheter (CVC) experience a
septic or bacteremic episode and are subsequently at risk of its associated
long-term complications and mortality. Because of the serious clinical and
financial impact of hemodialysis catheter-related bacteremias (HCRIs),
standardized, validated definitions based on the hemodialysis patient population
are necessary in order to better diagnose, monitor, and report HCRI for patient
quality assurance and research purposes. The pathophysiology of HCRI involves a
complex interaction between a triad that consists of the host patient, the
infecting microorganism, and the vehicle catheter. Although the microorganism
contribution in the pathogenesis of HCRI is likely most important, certain
patient and catheter-related characteristics may be more amenable to
manipulation. The key to managing HCRI is on prophylaxis against the initial
microorganism catheter adherence and subsequent biofilm development. General and
specific prophylactic maneuvers directed at both an intravascular and
extraluminal route of microorganism entry are discussed including antibioticand
silver-impregnated catheters and dressings, subcutaneous access devices, and
topical prophylaxis at the exit site. In addition to systemic antibiotic use,
the
3 methods of HRCI treatment using catheter salvage, guidewire exchange, and
concurrent antibiotic lock are compared. The outcome and complications of HCRI
may be serious and highlight the importance of careful, continual infection
surveillance. Although the use of a multidisciplinary hemodialysis infection
control team is desirable, staffing education and physician feedback have been
shown to improve adherence to infection control guidelines and reduce HCRI.
Publication Types:
Review
PMID: 16815229 [PubMed - indexed for MEDLINE]
14: J Antimicrob Chemother. 2006 Aug;58(2):281-7. Epub 2006 Jun 6.
Use of chlorhexidine-impregnated dressing to prevent vascular and epidural
catheter colonization and infection: a meta-analysis.
Ho KM, Litton E.
Department of Intensive Care, Royal Perth Hospital Perth 6000, Western
Australia,
Australia. kwok.ho@health.wa.gov.au
OBJECTIVES: Vascular and epidural catheter-related infections cause significant
morbidities and mortality in hospitalized patients. This meta-analysis assessed
the effect of chlorhexidine-impregnated dressing on the risk of vascular and
epidural catheter bacterial colonization and infection. METHODS: Literature
search was based on MEDLINE (1966 to 1 November 2005), EMBASE and Cochrane
Controlled Trials Register (2005 issue 3) databases. Only randomized controlled
clinical trials comparing chlorhexidine-impregnated dressing with placebo or
9
povidine-iodine dressing were included in this meta-analysis. Two reviewers
reviewed and extracted the data independently. RESULTS: Eight studies assessing
a
single type of chlorhexidine-impregnated dressing were identified and subjected
to meta-analysis. The chlorhexidine-impregnated dressing reduced the risk of
epidural [3.6% versus 35%, odds ratio (OR) 0.07, 95% CI: 0.02-0.31, P=0.0005]
and
intravascular catheter or exit-site bacterial colonization (14.8% versus 26.9%,
OR 0.47, 95% CI: 0.34-0.65, P<0.00001) (overall 14.3% versus 27.2%, OR 0.40, 95%
CI: 0.26-0.61; P<0.0001). The use of chlorhexidine-impregnated dressing was
associated with a trend towards reduction in catheter-related bloodstream or CNS
infections (2.2% versus 3.8%, OR 0.58, 95% CI: 0.29-1.14, P=0.11). Local
cutaneous reactions to chlorhexidine-impregnated dressing were reported in 5.6%
of the patients in three studies (OR 8.17, 95% CI: 1.19-56.14, P=0.04), and 96%
of these reactions occurred in neonatal patients. The number needed to prevent
one episode of intravascular catheter-related bloodstream infection was 142 for
an average period of catheter in situ of 10 days and a change of dressing every
5
days. The cost of preventing one vascular catheter-related bloodstream infection
was estimated to be pound298 (US$532.5). CONCLUSIONS: Chlorhexidine-impregnated
dressing is effective in reducing vascular and epidural catheter bacterial
colonization and is also associated with a trend towards reduction in
catheter-related bloodstream or CNS infections. A large randomized controlled
trial is needed to confirm whether chlorhexidine-impregnated dressing is
cost-effective in preventing bacterial infection related to vascular and
epidural
catheters.
Publication Types:
Meta-Analysis
Review
PMID: 16757502 [PubMed - indexed for MEDLINE]
15: J Infect. 2007 Feb;54(2):146-50. Epub 2006 May 5.
Reduction of catheter-related colonisation by the use of a silver
zeolite-impregnated central vascular catheter in adult critical care.
Khare MD, Bukhari SS, Swann A, Spiers P, McLaren I, Myers J.
Department of Clinical Microbiology, University Hospitals of Leicester NHS
Trust,
Leicester LE1 5WW, UK.
Central vascular catheters (CVC) are used extensively in critical care for
monitoring and therapy. They can become colonised with viable micro-organisms
within 24 h of insertion, which can rapidly form biofilm. This colonisation is a
precursor of catheter-related bloodstream infections (CR-BSI), which are
associated with substantial morbidity, mortality, prolonged hospital stay and
increased cost. Antimicrobials have been incorporated into the bulk material of
CVC or applied to their surfaces as a coating in an attempt to reduce the
incidence of CVC colonisation and infection. This study examines the effect of a
silver zeolite-impregnated catheter on catheter-related colonisation and
infection in adult critical care patients. The study was conducted in adult
Intensive Care Units (ICU) at three acute hospitals over 14 months and involved
246 CVC insertions (122 silver-impregnated and 124 non-impregnated). CVC tip
colonisation was detected by the Maki Roll culture and CR-BSI by differential
time-to-positivity of blood cultures. Overall colonisation rate was
significantly
lower in the silver zeolite-impregnated CVC tips (58%) as compared with the
control CVC tips (73%) (p<0.025). In addition, there was a lower rate (34%) of
tip colonisation by coagulase negative staphylococci in the silver
10
zeolite-impregnated CVC tips as compared with the control CVC tips (47%)
(p<0.05). Four episodes of CR-BSI were detected in each arm by differential
time-to-positivity in a subset of patients. This study indicates that the silver
zeolite-impregnated catheter is superior to non-impregnated catheter in reducing
the rate of CVC colonisation but it showed no difference in the rates of CR-BSI
in the two arms. Larger prospective randomised control studies are required to
evaluate its role in the prevention of CR-BSI.
Publication Types:
Evaluation Studies
PMID: 16678904 [PubMed - indexed for MEDLINE]
16: Int Surg. 2005 Sep-Oct;90(4):219-22.
Prospective nonrandomized trial of silver impregnated cuff central lines.
Alderman RL, Sugarbaker PH.
Washington Cancer Institute, Washington, District of Columbia 20010, USA.
Central venous lines were used to administer total parenteral nutrition at our
institution. In an attempt to reduce line sepsis, silver impregnated cuff
central
lines (Hohn catheter) were adopted as standard of practice. Using a
comprehensive
morbidity and mortality database, 134 patients with Hohn catheters were compared
to 252 patients who had polypropylene central line. The incidence of central
line
sepsis was increased with Hohn catheters to 23 of 134 (17.2%). This compared to
8
of 252 (3.2%) patients with polypropylene catheters (P < 0.0001). Also, an
increased incidence of pulmonary embolism of 15 of 134 (11.2%) in patients with
Hohn catheters was observed as compared to 2 of 252 (0.8%) with a polypropylene
catheter (P < 0.0001). Insertion of Hohn catheters through the intrajugular vein
was judged to be more difficult than polypropylene catheters. This may cause
increased trauma to the vein resulting in a higher incidence of line infection
and pulmonary embolism.
Publication Types:
Comparative Study
PMID: 16548318 [PubMed - indexed for MEDLINE]
17: Crit Care Med. 2006 Mar;34(3):668-75.
Comment in:
Crit Care Med. 2006 Mar;34(3):905-7.
A prospective, randomized trial of rifampicin-minocycline-coated and
silver-platinum-carbon-impregnated central venous catheters.
Fraenkel D, Rickard C, Thomas P, Faoagali J, George N, Ware R.
Department of Intensive Care, Princess Alexandra Hospital, and School of
Population Health, University of Queensland, Australia.
OBJECTIVE: Central venous catheters are the predominant cause of nosocomial
bacteremia; however, the effectiveness of different antimicrobial central venous
catheters remains uncertain. We compared the infection rate of
silver-platinum-carbon (SPC)-impregnated catheters with rifampicin-minocycline
(RM)-coated catheters. DESIGN: A large, single-center, prospective randomized
study. SETTING: Twenty-two-bed adult general intensive care unit in a large
11
tertiary metropolitan hospital in Brisbane, Australia (2000-2001). PATIENTS:
Consecutive series of all central venous catheterizations in intensive care unit
patients. INTERVENTIONS: Randomization, concealment, and blinding were carefully
performed. Catheter insertion and care were performed according to published
guidelines. Blood cultures were taken at central venous catheter removal, and
catheter-tip cultures were performed by both roll-plate and sonication
techniques. Pulsed field gel electrophoresis was used to establish shared clonal
origin for matched isolates. MEASUREMENTS AND MAIN RESULTS: Central venous
catheter colonization and catheter-related bloodstream infection were determined
with a blinded technique using the evaluation of the extensive microbiological
and clinical data collected and a rigorous classification system. Six hundred
forty-six central venous catheters (RM 319, SPC 327) were inserted, and 574
(89%)
were microbiologically evaluable. Colonization rates were lower for the RM
catheters than SPC catheters (25 of 280, 8.9%; 43 of 294, 14.6%; p=.039). A
Kaplan-Meier analysis that included catheter time in situ did not quite achieve
statistical significance (p=.055). Catheter-related bloodstream infection was
infrequent for both catheter-types (RM 4, 1.4%; SPC 5, 1.7%). CONCLUSIONS: The
SPC catheter is a clinically effective antimicrobial catheter; however, the RM
catheter had a lower colonization rate. Both catheter types had low rates of
catheter-related bloodstream infection. These results indicate that future
studies will require similar rigorous methodology and thousands of central
venous
catheters to demonstrate differences in catheter-related bloodstream infection
rates.
Publication Types:
Comparative Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 16505651 [PubMed - indexed for MEDLINE]
18: Infect Control Hosp Epidemiol. 2006 Jan;27(1):23-7. Epub 2006 Jan 6.
Comment in:
Infect Control Hosp Epidemiol. 2006 Jan;27(1):3-7.
Disinfection of needleless catheter connectors and access ports with alcohol may
not prevent microbial entry: the promise of a novel antiseptic-barrier cap.
Menyhay SZ, Maki DG.
Menhay Medical, Fresno, California, USA.
BACKGROUND: Needleless valve connectors for vascular catheters are widely used
throughout the United States because they reduce the risk of biohazardous
injuries from needlesticks and exposure to bloodborne pathogens, such as human
immunodeficiency virus and hepatitis C virus. Patients with long-term central
venous catheters are at significant risk of acquiring catheter-related
bloodstream infections caused by microbes that gain access through the
connection
between the administration set and the catheter or an injection port. Most
healthcare practitioners wipe the membranous septum of the needleless connector
or the injection port with 70% alcohol before accessing it. We report a
simulation study of the efficacy of conventional alcohol disinfection before
access, compared with that of a novel antiseptic-barrier cap that, when threaded
onto a needleless luer-activated valved connector, allows a
chlorhexidine-impregnated sponge to come into continuous contact with the
membranous surface; after removal of the cap, there is no need to disinfect the
surface with alcohol before accessing it. METHODS: One hundred five commercial,
needleless luer-activated valved connectors, each accessible by a blunt
12
male-connector luer-lock attachment, were purchased from 3 manufacturers and
were
tested. The membranous septum of each test device was first heavily contaminated
with approximately 10(5) colony-forming units of Enterococcus faecalis and then
was allowed to dry for 24 hours. Fifteen of the contaminated devices were not
disinfected (positive controls), 30 were conventionally disinfected with a
commercial 70% alcohol pledget, and 60 had the antiseptic cap threaded onto the
connector and then removed after 10 minutes. The test connectors were then
accessed with a sterile syringe containing nutrient broth media, which was
injected, captured on the downstream side of the intraluminal fluid pathway, and
cultured quantitatively. RESULTS: All 15 control connectors (100%) showed
massive
transmission of microorganisms across the membranous septum (4,500-10,000
colony-forming units). Of the 30 connectors accessed after conventional
disinfection with 70% alcohol, 20 (67%) showed transmission of microorganisms
(442-25,000 colony-forming units). In contrast, of the 60 connectors cultured
after application of the novel antiseptic cap, only 1 (1.6%) showed any
transmission of microorganisms (P < .001). CONCLUSIONS: The findings of this
study show that, if the membranous septum of a needleless luer-activated
connector is heavily contaminated, conventional disinfection with 70% alcohol
does not reliably prevent entry of microorganisms. In contrast, the
antiseptic-barrier cap provided a high level of protection, even in the presence
of very heavy contamination. This novel technology deserves to be studied in a
clinical trial.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 16418982 [PubMed - indexed for MEDLINE]
19: J Hosp Infect. 2006 Feb;62(2):156-62. Epub 2005 Nov 22.
Efficacy of antiseptic-impregnated catheters on catheter colonization and
catheter-related bloodstream infections in patients in an intensive care unit.
Osma S, Kahveci SF, Kaya FN, Akalin H, Ozakin C, Yilmaz E, Kutlay O.
Department of Anaesthesiology and ICU, School of Medicine, Uludag University,
16059 Görükle, Bursa, Turkey.
This study was conducted to evaluate the impact of central venous catheters
impregnated with chlorhexidine and silver sulphadiazine on the incidence of
colonization and catheter-related bloodstream infection in critically ill
patients. One hundred and thirty-three patients requiring central venous
catheterization were chosen at random to receive either an antisepticimpregnated
triple-lumen catheter (N=64) or a standard triple-lumen catheter (N=69). The
mean
(SD) durations of catheterization for the antiseptic and standard catheters were
11.7 (5.8) days (median 10; range 3-29) and 8.9 (4.6) days (median 8.0; range
3-20), respectively (P=0.006). Fourteen (21.9%) of the antiseptic catheters and
14 (20.3%) of the standard catheters had been colonized at the time of removal
(P=0.834). Four cases (6.3%) of catheter-related bloodstream infection were
associated with antiseptic catheters and one case (1.4%) was associated with a
standard catheter (P=0.195). The catheter colonization rates were 18.7/1000
catheter-days for the antiseptic catheter group and 22.6/1000 catheter-days for
the standard catheter group (P=0.640). The catheter-related bloodstream
infection
rates were 5.3/1000 catheter-days for the antiseptic catheter group and 1.6/1000
catheter-days for the standard catheter group (P=0.452). In conclusion, our
results indicate that the use of antiseptic-impregnated central venous catheters
has no effect on the incidence of either catheter colonization or
catheter-related bloodstream infection in critically ill patients.
13
Publication Types:
Randomized Controlled Trial
PMID: 16307824 [PubMed - indexed for MEDLINE]
20: Anesth Analg. 2005 Dec;101(6):1778-84.
Central venous catheter colonization in critically ill patients: a prospective,
randomized, controlled study comparing standard with two antiseptic-impregnated
catheters.
Dünser MW, Mayr AJ, Hinterberger G, Flörl CL, Ulmer H, Schmid S, Friesenecker B,
Lorenz I, Hasibeder WR.
Division of General and Surgical Intensive Care Medicine, Department of
Anesthesia and Critical Care Medicine, Innsbruck Medical University,
Anichstrasse
35, 6020 Innsbruck, Austria. Martin.Duenser@uibk.ac.at
In this prospective, randomized, controlled, unblinded study, we compared
colonization rates of a standard, unimpregnated central venous catheter (CVC)
with rates for silver-coated and chlorhexidine-silversulfadiazine
(CH-SS)-impregnated CVC. Patient characteristics, CVC insertion site, indwelling
time, and colonization detected by semiquantitative and quantitative
microbiologic techniques were documented. Two-hundred-seventy-five critically
ill
patients were included into the study protocol. One-hundred-sixty standard, 160
silver (S)-coated, and 165 externally impregnated CH-SS CVC were inserted. There
was a significant difference in CVC colonization rates among study groups (P =
0.029). There was no difference in the colonization rate and the colonization
per
1000 catheter days between standard and S-coated (P = 0.564; P = 0.24) or
CH-SS-coated CVC (P= 0.795; P = 0.639). When comparing antiseptic CVC with each
other, colonization rates were significantly less with CH-SS-impregnated than
with S-coated CVC (16.9% versus 7.3%; P = 0.01; 18.2 versus 7.5 of 1000 catheter
days; P = 0.003; relative risk, 0.43; 95% confidence interval, 0.21-0.85).
Whereas standard and S-coated CVC were first colonized 2 and 3 days after
insertion, respectively, CH-SS CVC were first colonized only after 7 days. In
conclusion, antiseptic-impregnated CVC could not prevent catheter colonization
when compared with standard polyurethane catheters in a critical care setting
with infrequent catheter colonization rates and CVC left in place for >10 days.
Publication Types:
Comparative Study
Randomized Controlled Trial
PMID: 16301258 [PubMed - indexed for MEDLINE]
21: Ann Intern Med. 2005 Oct 18;143(8):570-80.
Summary for patients in:
Ann Intern Med. 2005 Oct 18;143(8):I36.
Effect of a second-generation venous catheter impregnated with chlorhexidine and
silver sulfadiazine on central catheter-related infections: a randomized,
controlled trial.
Rupp ME, Lisco SJ, Lipsett PA, Perl TM, Keating K, Civetta JM, Mermel LA, Lee D,
Dellinger EP, Donahoe M, Giles D, Pfaller MA, Maki DG, Sherertz R.
University of Nebraska Medical Center, Omaha, Nebraska, USA. merupp@unmc.edu
14
BACKGROUND: Central venous catheter-related infections are a significant medical
problem. Improved preventive measures are needed. OBJECTIVE: To ascertain 1)
effectiveness of a second-generation antiseptic-coated catheter in the
prevention
of microbial colonization and infection; 2) safety and tolerability of this
device; 3) microbiology of infected catheters; and 4) propensity for the
development of antiseptic resistance. DESIGN: Multicenter, randomized,
double-blind, controlled trial. SETTING: 9 university-affiliated medical
centers.
PATIENTS: 780 patients in intensive care units who required central venous
catheterization. INTERVENTION: Patients received either a standard catheter or a
catheter coated with chlorhexidine and silver sulfadiazine. MEASUREMENTS: The
authors assessed catheter colonization and catheter-related infection,
characterized microbes by molecular typing, and determined their susceptibility
to antiseptics. Patient tolerance of the catheter was monitored. RESULTS:
Patients with the 2 types of catheters had similar demographic features,
clinical
interventions, laboratory values, and risk factors for infection. Antiseptic
catheters were less likely to be colonized at the time of removal compared with
control catheters (13.3 vs. 24.1 colonized catheters per 1000 catheter-days; P <
0.01). The center-stratified Cox regression hazard ratio for colonization
controlling for sampling design and potentially confounding variables was 0.45
(95% CI, 0.25 to 0.78). The rate of definitive catheter-related bloodstream
infection was 1.24 per 1000 catheter-days (CI, 0.26 to 3.62 per 1000
catheter-days) for the control group versus 0.42 per 1000 catheter-days (CI,
0.01
to 2.34 per 1000 catheter-days) for the antiseptic catheter group (P = 0.6).
Coagulase-negative staphylococci and other gram-positive organisms were the most
frequent microbes to colonize catheters. Noninfectious adverse events were
similar in both groups. Antiseptic susceptibility was similar for microbes
recovered from either group. LIMITATIONS: The antiseptic catheter was not
compared with an antibiotic-coated catheter, and no conclusion can be made
regarding its effect on bloodstream infection. CONCLUSIONS: The secondgeneration
chlorhexidine-silver sulfadiazine catheter is well tolerated. Antiseptic coating
appears to reduce microbial colonization of the catheter compared with an
uncoated catheter.
Publication Types:
Clinical Trial
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 16230723 [PubMed - indexed for MEDLINE]
22: Ann Intern Med. 2005 Oct 18;143(8):I36.
Original report in:
Ann Intern Med. 2005 Oct 18;143(8):570-80.
Summaries for patients. Can antibiotic-coated catheters help decrease the
incidence of bloodstream infections in patients in the intensive care unit?
[No authors listed]
Publication Types:
Patient Education Handout
PMID: 16230719 [PubMed - indexed for MEDLINE]
23: Chest. 2005 Aug;128(2):489-95.
15
Risk of catheter-related bloodstream infection with peripherally inserted
central
venous catheters used in hospitalized patients.
Safdar N, Maki DG.
Section of Infectious Diseases, Department of Medicine, University of Wisconsin
Medical School, Madison, USA.
BACKGROUND: Peripherally inserted central venous catheters (PICCs) are now
widely
used for intermediate and long-term access in current-day health care,
especially
in the inpatient setting, where they are increasingly supplanting conventional
central venous catheters (CVCs) placed percutaneously into the internal jugular,
subclavian, or femoral veins. Data on the risk of PICC-related bloodstream
infection (BSI) with PICCs used in hospitalized patients are limited. STUDY
OBJECTIVES: To determine the risk of PICC-related BSI in hospitalized patients.
STUDY DESIGN: Prospective cohort study using data from two randomized trials
assessing the efficacy of chlorhexidine-impregnated sponge dressing and
chlorhexidine for cutaneous antisepsis. METHODS: PICCs inserted into the
antecubital vein in two randomized trials during from 1998 to 2000 were
prospectively studied; most patients were in an ICU. PICC-related BSI was
confirmed in each case by demonstrating concordance between isolates colonizing
the PICC at the time of removal and from blood cultures by restriction-fragment
DNA subtyping. RESULTS: Overall, 115 patients had 251 PICCs placed. Mean
duration
of catheterization was 11.3 days (total, 2,832 PICC-days); 42% of the patients
were in an ICU at some time, 62% had urinary catheters, and 49% had received
mechanical ventilation. Six PICC-related BSIs were identified (2.4%), four with
coagulase-negative staphylococcus, one with Staphylococcus aureus, and one with
Klebsiella pneumoniae, a rate of 2.1 per 1,000 catheter-days. CONCLUSION: This
prospective study shows that PICCs used in high-risk hospitalized patients are
associated with a rate of catheter-related BSI similar to conventional CVCs
placed in the internal jugular or subclavian veins (2 to 5 per 1,000
catheter-days), much higher than with PICCs used exclusively in the outpatient
setting (approximately 0.4 per 1,000 catheter-days), and higher than with cuffed
and tunneled Hickman-like CVCs (approximately 1 per 1,000 catheter-days). A
randomized trial of PICCs and conventional CVCs in hospitalized patients
requiring central access is needed. Our data raise the question of whether the
growing trend in many hospital hematology and oncology services to switch from
use of cuffed and tunneled CVCs to PICCs is justified, particularly since PICCs
are more vulnerable to thrombosis and dislodgment, and are less useful for
drawing blood specimens. Moreover, PICCs are not advisable in patients with
renal
failure and impending need for dialysis, in whom preservation of upper-extremity
veins is needed for fistula or graft implantation.
Publication Types:
Research Support, Non-U.S. Gov't
Review
PMID: 16100130 [PubMed - indexed for MEDLINE]
24: Pediatr Infect Dis J. 2005 Aug;24(8):676-9.
Chlorhexidine-impregnated dressing for prevention of colonization of central
venous catheters in infants and children: a randomized controlled study.
Levy I, Katz J, Solter E, Samra Z, Vidne B, Birk E, Ashkenazi S, Dagan O.
Department of Pediatric Infectious Diseases, Schneider Children's Medical Center
of Israel, Petah Tiqva, Israel. lavyguy@bezeqint.net
16
BACKGROUND: Infections of short term, nontunneled, intravascular catheters are
often caused by migration of organisms from the insertion site. The aim of this
study was to evaluate the effectiveness and safety of a chlorhexidine
gluconate-impregnated dressing for the reduction of central venous catheter
(CVC)
colonization and CVC-associated bloodstream infections in infants and children
after cardiac surgery. METHODS: This prospective, randomized, controlled study
was conducted in the pediatric cardiac intensive care unit of a tertiary care
pediatric medical center. Patients 0-18 years of age who were admitted to the
pediatric cardiac intensive care unit during a 14-month period and required a
CVC
for >48 hours were randomized to receive a transparent polyurethane insertion
site dressing (control group) or a chlorhexidine gluconate-impregnated sponge
(Biopatch) dressing covered by a transparent polyurethane dressing (study
group).
The main outcome measures were rates of bacterial colonization, rates of
CVC-associated bloodstream infections and adverse events. RESULTS: Seventy-one
patients were randomized to the control group and 74 to the study group. There
were no significant between group differences in age, sex, Pediatric Risk of
Mortality score or cardiac severity score. CVC colonization occurred in 21
control patients (29%) and 11 (14.8%) study patients (P = 0.0446; relative risk,
0.6166; 95% confidence interval, 0.3716-1.023). Bloodstream infection occurred
in
3 patients (4.2%) in the control group and 4 patients (5.4%) in the study group.
Local redness was noted in 1 control patient and 4 study group patients.
CONCLUSIONS: The chlorhexidine gluconate-impregnated sponge is safe and
significantly reduces the rates of CVC colonization in infants and children
after
cardiac surgery.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 16094219 [PubMed - indexed for MEDLINE]
25: Support Care Cancer. 2005 Dec;13(12):993-1000. Epub 2005 Apr 16.
Chlorhexidine and silver-sulfadiazine coated central venous catheters in
haematological patients--a double-blind, randomised, prospective, controlled
trial.
Ostendorf T, Meinhold A, Harter C, Salwender H, Egerer G, Geiss HK, Ho AD,
Goldschmidt H.
Department of Internal Medicine V, University of Heidelberg, Im Neuenheimer Feld
410, 69120, Heidelberg, Germany.
BACKGROUND: Central venous catheters (CVCs) are essential for the intensive care
of patients with haematological illness. Catheter-related infections (CRI) are
an
important problem in modern medicine, which may lead to life-threatening
situations, to prolonged hospitalisation and increased cost. In
immunocompromised
patients suffering from haemato-oncological diseases, CRI is a significant
factor
for adverse outcome. Several clinical studies have shown that CVCs coated with
antiseptics such as chlorhexidine and silver-sulfadiazine (CHSS) reduce the risk
of catheter-related bacteraemia. Most studies, however, were performed on
intensive care patients not suffering from chemotherapy-induced
immunosuppression. PATIENTS AND METHODS: A prospective double-blind, randomised,
controlled trial was performed to investigate the effectiveness of CHSS-coated
17
catheters in haemato-oncological patients. A total number of 184 catheters
(median duration of placement, 11 days) were inserted into 184 patients (male
115, female 69), of which 90 were antiseptically coated. After removal, all
catheters were investigated for bacterial growth. MAIN RESULTS: Catheters coated
with CHSS were effective in reducing the rate of significant bacterial growth on
either the tip or subcutaneous segment (26%) compared to control catheters
(49%).
The incidence of catheter colonisation was also significantly reduced (12%
coated
vs 33% uncoated). Data obtained show a significant reduction of catheter
colonisation in CHSS catheters. There was no significant difference in the
incidence of catheter-related bacteraemia (3% coated vs 7% uncoated). However,
due to the overall low rate of CRI, we could not observe a significant reduction
in the incidence of catheter-related bacteraemia. CONCLUSION: Our data show that
the use of CHSS catheters in patients with haematological malignancy reduces the
overall risk of catheter colonisation and CRI, although the incidence of
catheter-related bacteremia was similar in both groups.
Publication Types:
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 15834740 [PubMed - indexed for MEDLINE]
26: Ann Fr Anesth Reanim. 2005 Mar;24(3):291-3.
[Clinical use of antiseptic and antibiotic impregnated catheters]
[Article in French]
Lefrant JY.
Fédération d'anesthésie-douleur-urgence-réanimation, hôpital Caremeau, CHU,
place
du Professeur-Debré, 30029 Nîmes cedex 04 France. jean.yves.lefrant@chu-nimes.fr
In order to decrease the risks of colonisation and infection of central venous
catheters, their impregnation has been suggested using anti-infectious agents
(antiseptic, antibiotic, silver). Many methodological flaws and contradictory
results have been reported in the published trials. The use of impregnated
catheter should only be discussed when the issues of anatomic site and type of
insertion of the catheter have been adequately addressed.
Publication Types:
English Abstract
Review
PMID: 15792566 [PubMed - indexed for MEDLINE]
27: Am J Infect Control. 2004 Dec;32(8):486-8.
Susceptibility of coagulase-negative staphylococcal nosocomial bloodstream
isolates to the chlorhexidine/silver sulfadiazine-impregnated central venous
catheter.
Rosato AE, Tallent SM, Edmond MB, Bearman GM.
Department of Internal Medicine, School of Medicine, Virginia Commonwealth
University, Richmond, VA 23298, USA.
Publication Types:
Comparative Study
18
PMID: 15573055 [PubMed - indexed for MEDLINE]
28: Ann Hematol. 2005 Apr;84(4):258-62. Epub 2004 Nov 10.
Reduction of catheter-related infections in neutropenic patients: a prospective
controlled randomized trial using a chlorhexidine and silver
sulfadiazine-impregnated central venous catheter.
Jaeger K, Zenz S, Jüttner B, Ruschulte H, Kuse E, Heine J, Piepenbrock S, Ganser
A, Karthaus M.
Department of Anesthesiology, Hannover Medical School, Hannover, Germany.
Antiseptic coating of intravascular catheters may be an effective means of
decreasing catheter-related colonization and subsequent infection. The purpose
of
this study was to assess the efficacy of chlorhexidine and silver sulfadiazine
(CH-SS)-impregnated central venous catheters (CVCs) to prevent catheter-related
colonization and infection in patients with hematological malignancies who were
subjected to intensive chemotherapy and suffered from severe and sustained
neutropenia. Proven CVC-related bloodstream infection (BSI) was defined as the
isolation of the same species from peripheral blood culture and CVC tip (Maki
technique). This randomized, prospective clinical trial was carried out in 106
patients and compared catheter-related colonization and BSI using a
CH-SS-impregnated CVC (n=51) to a control arm using a standard uncoated
triple-lumen CVC (n=55). Patients were treated for acute leukemia (n=89),
non-Hodgkin's lymphoma (n=10), and multiple myeloma (n=7). Study groups were
balanced regarding to age, sex, underlying diseases, insertion site, and
duration
of neutropenia. The CVCs were in situ a mean of 14.3+/-8.2 days (mean+/-SD) in
the study group versus 16.6+/-9.7 days in the control arm. Catheter-related
colonization was observed less frequently in the study group (five vs nine
patients; p=0.035). CVC-related BSI were significantly less frequent in the
study
group (one vs eight patients; p=0.02). In summary, in patients with severe
neutropenia, CH-SS-impregnated CVCs yield a significant antibacterial effect
resulting in a significantly lower rate of catheter-related colonization as well
as CVC-related BSI.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 15549302 [PubMed - indexed for MEDLINE]
29: Infect Control Hosp Epidemiol. 2004 Aug;25(8):650-5.
Routine changing of intravenous administration sets does not reduce colonization
or infection in central venous catheters.
Rickard CM, Lipman J, Courtney M, Siversen R, Daley P.
Royal Brisbane Hospital, Brisbane, Australia.
OBJECTIVE: To determine the effect of routine intravenous (IV) administration
set
changes on central venous catheter (CVC) colonization and catheter-related
bacteremia. DESIGN: Prospective, randomized, controlled trial. SETTING:
Eighteen-bed intensive care unit (ICU) in a large metropolitan hospital.
PARTICIPANTS: Two hundred fifty-one patients with 404 chlorhexidine gluconate
and
silver sulfadiazine-coated multi-lumen CVCs. INTERVENTIONS: CVCs inserted in the
ICU and in situ on day 4 were randomized to have their IV administration sets
19
changed on day 4 (n = 203) or not at all (n = 201). Use of fluid containers and
blood product administration sets was limited to 24 hours. CVCs were removed
when
not required, infection was suspected, or in place on day 7. Catheter cultures
were performed on removal by blinded laboratory staff. Catheter-related
bacteremia was diagnosed by a blinded intensivist using strict definitions. Data
were collected regarding catheter duration, site, Acute Physiology and Chronic
Health Evaluation (APACHE) II score, patient age, diagnosis, hyperglycemia,
hypoalbuminemia, immune status, number of fluid containers and IV injections,
and
administration of propofol, blood, total parenteral nutrition, or lipid
infusion.
RESULTS: There were 10 colonized CVCs in the group receiving a set change and 19
in the group not receiving one. This difference was not statistically
significant
on Kaplan-Meier survival analysis. There were 3 cases of catheter-related
bacteremia per group. Logistic regression found that burns diagnosis and
increased ICU stay significantly predicted colonization. CONCLUSION: IV
administration sets can be used for 7 days in patients with short-term,
antiseptic-coated CVCs.
Publication Types:
Clinical Trial
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 15357156 [PubMed - indexed for MEDLINE]
30: Intensive Care Med. 2004 May;30(5):837-43. Epub 2004 Apr 2.
Prevention of intravascular catheter-related infection with newer
chlorhexidine-silver sulfadiazine-coated catheters: a randomized controlled
trial.
Brun-Buisson C, Doyon F, Sollet JP, Cochard JF, Cohen Y, Nitenberg G.
Réanimation Médicale, Hôpital Henri Mondor (AP-HP), Av du Maréchal de Lattre de
Tassigny, 94010 Créteil Cedex, France. christian.brun-buisson@hmn.ap-hopparis.fr
BACKGROUND: The indication of antiseptic-coated catheters remains debated.
OBJECTIVE: To test the ability of the new generation of chlorhexidine-silver and
sulfadiazine-coated catheters, with enhanced antiseptic coating, to reduce the
risk of central venous catheter (CVC)-related infection in ICU patients. DESIGN:
Multicentre randomized double-blind trial. PATIENTS AND SETTING: A total of 397
patients from 14 ICUs of university hospitals in France. INTERVENTION: Patients
were randomized to receive an antiseptic-coated catheter (ACC) or a standard
non-coated catheter (NCC). MEASUREMENTS: Incidence of CVC-related infection.
RESULTS: Of 367 patients having a successful catheter insertion, 363 were
analysed (175 NCC and 188 ACC). Patients had one (NCC=162, ACC=180) or more
(NCC=13, ACC=11) CVC inserted. The two groups were similar for insertion site
[subclavian (64 vs 69)] or jugular (36 vs 31%)], and type of catheters
(single-lumen 18 vs 18%; double-lumen 82 vs 82%), and mean (median) duration of
catheterisation [12.0+/-11.7 (9) vs 10.5+/-8.8 (8) days in the NCC and ACC
groups, respectively]. Significant colonisation of the catheter occurred in 23
(13.1%) and 7 (3.7%) patients, respectively, in the NCC and ACC groups (11 vs
3.6
per 1000 catheter-days; p=0.01); CVC-related infection (bloodstream infection)
occurred in 10 (5) and 4 (3) patients in the NCC and CC groups, respectively
(5.2
vs 2 per 1000 catheter days; p=0.10). CONCLUSIONS: In the context of a low
baseline infection rate, ACC were associated with a significant reduction of
catheter colonisation and a trend to reduction of infection episodes, but not of
20
bloodstream infection.
Publication Types:
Clinical Trial
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 15060765 [PubMed - indexed for MEDLINE]
31: Intensive Care Med. 2004 Apr;30(4):633-8. Epub 2004 Jan 13.
Evaluation of a triple-lumen central venous heparin-coated catheter versus a
catheter coated with chlorhexidine and silver sulfadiazine in critically ill
patients.
Carrasco MN, Bueno A, de las Cuevas C, Jimenez S, Salinas I, Sartorius A, Recio
T, Generelo M, Ruiz-Ocaña F.
Intensive Care Unit, Hospital Universitario de la Princesa, Diego de León 62,
28006 Madrid, Spain. ncarrasco.hlpr@salud.madrid.org
OBJECTIVE: To compare the incidence of catheter colonization and catheterrelated
bloodstream infections between heparin-coated catheters and those coated with a
synergistic combination of chlorhexidine and silver sulfadiazine. DESIGN:
Randomized, controlled clinical trial. SETTING: A 20-bed medical-surgical
intensive care unit. PATIENTS: A total of 180 patients requiring the insertion
of
a trilumen central venous catheter. INTERVENTIONS. Patients were randomized to
receive either a trilumen heparin or chlorhexidine and silver sulfadiazinecoated
catheter. MEASUREMENTS: Catheter colonization was defined by a semiquantitative
catheter tip culture yielding 15 or more colony-forming units or quantitative
culture of 1,000 or more colony-forming units/ml. Catheter-related bloodstream
infection as the isolation of the same microorganism from a peripheral blood
culture and catheter tip. RESULTS: A total of 260 catheters were cultured. Out
of
132 heparin-coated catheters, 29 were colonized and out of 128 chlorhexidine and
silver sulfadiazine-coated catheters, 13 were colonized ( p=0.03), relative risk
RR=2.16 (1.18-3.97). This represents an incidence of 23.5 and 11.5 episodes of
catheter colonization per 1,000 catheter-days, respectively ( p=0.0059), RR=2.04
(1.05-3.84). Microorganisms isolated in catheter colonization from heparincoated
catheters were gram-positive cocci 23, gram-negative bacilli 7, and Candida spp
4. In chlorhexidine and silver sulfadiazine-coated catheters were gram-positive
cocci 6 and gram-negative bacilli 11 ( p=0.009). The incidence of
catheter-related bloodstream infections per 1,000 catheter-days was 3.24 in
heparin-coated catheters and 2.6 in chlorhexidine and silver sulfadiazine-coated
catheters ( p=0.79), RR=1.22 (0.27-5.43). CONCLUSIONS: In critically ill
patients
the use of trilumen central venous catheters coated with chlorhexidine and
silver
sulfadiazine reduced the risk of catheter colonization due to prevention of
gram-positive cocci and Candida spp.
Publication Types:
Clinical Trial
Comparative Study
Randomized Controlled Trial
PMID: 14722639 [PubMed - indexed for MEDLINE]
21
32: Anaesth Intensive Care. 2003 Dec;31(6):697-8.
Anaphylaxis to chlorhexidine-impregnated central venous catheter.
Kluger M.
Publication Types:
Case Reports
Letter
PMID: 14719435 [PubMed - indexed for MEDLINE]
33: Intensive Care Med. 2004 Jan;30(1):62-7. Epub 2003 Nov 26.
The pathogenesis of catheter-related bloodstream infection with noncuffed
short-term central venous catheters.
Safdar N, Maki DG.
Section of Infectious Diseases, Department of Medicine, Medical School,
University of Wisconsin, Madison, WI 53792, USA.
OBJECTIVE: Short-term, noncuffed, percutaneously inserted central venous
catheters (CVCs) are widely used and cause more than 250,000 bloodstream
infections (BSIs) in hospitals each year in the United States. We report a
prospective study undertaken to determine the pathogenesis of CVC-related BSI.
DESIGN AND SETTING: Prospective cohort study in a university hospital 24-bed
medical-surgical intensive care unit. PATIENTS AND PARTICIPANTS: Patients
participating in two randomized trials during 1998-2000-one studying the
efficacy
of a 1% chlorhexidine-75% alcohol solution for cutaneous antisepsis and the
other
a novel chlorhexidine-impregnated sponge dressing-formed the study population;
CVC-related BSIs were considered to be extraluminally acquired if concordance
was
identified solely between isolates from catheter segments, skin, and blood
cultures and intraluminally acquired if concordance was demonstrated only
between
hub or infusate and blood culture isolates, as confirmed by DNA subtyping of
isolates from blood and catheter sites or infusate. RESULTS: Of 1,263 catheters
(6075 CVC days) prospectively studied, 35 (2.7%) caused BSI (5.9 per 1000 CVC
days); 27 were caused by coagulase-negative staphylococci. Overall, 45% of
infections were extraluminally acquired, 26% were intraluminally derived, and
the
mechanism of infection was indeterminate in 29%. In the pooled control groups of
the two trials, 25 CVC-related BSIs occurred (7.0 per 1000 CVC days), of which
60% of infections were extraluminally acquired, 12% were intraluminally derived
and 28% were indeterminate. In contrast, CVC-related BSIs in the treatment
groups
were most often intraluminally derived (60%, p=0.006). CONCLUSIONS: Most
catheter-related BSIs with short-term percutaneously inserted, noncuffed CVCs
were extraluminally acquired and derived from the cutaneous microflora.
Strategies achieving successful suppression of cutaneous colonization can
substantially reduce the risk of catheter-related BSI with short-term CVCs.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 14647886 [PubMed - indexed for MEDLINE]
34: Ther Apher Dial. 2003 Apr;7(2):225-31.
Long-term catheters for apheresis and dialysis with surface treatment with
22
infection resistance and low thrombogenicity.
Bambauer R, Mestres P, Schiel R, Bambauer S, Sioshansi P, Latza R.
Institute for Blood Purification, Homburg/Saar, Germany.
rolf.bambauer-praxis-homburg@t-online.de
Infection, thrombosis, and stenosis are among the most frequent complications
associated with blood-contacting catheters. These problems are usually related
to
surface properties of the base catheter material. Surface treatment processes,
such as ion implantation and ion beam assisted deposition (IBAD) and microdomain
structured surfaces, can be used to mitigate such complications. This study
evaluated silver coated and implanted large bore catheters used for
extracorporeal detoxification. In a 186 patient prospective study, 225 large
bore
catheters were inserted into the internal jugular or subclavian veins.
Eighty-five surface-treated catheters (Spi-Argent, Spire Corporation, Bedford,
MA, USA) and 28 catheters with surface treatment (Spi-Silicone, Spire
Corporation) were inserted in 90 patients. One hundred and twelve untreated
catheters placed in 96 patients served as controls, After removal, the catheters
were cultured for bacterial colonization using standard microbiologic assays.
They also were examined using a scanning electron microscope (SEM). Bacterial
colonization was observed in 8% of the treated catheter compared with 46.4% of
untreated catheters. The SEM investigations showed all treated catheters to
possess low thrombogenicity. Catheters with microdomain structured surfaces
showed same results in preliminary observation. The surface treatments of the
large bore catheters can be used to improve thrombus and infection resistance of
blood contacting catheters.
PMID: 12918948 [PubMed - indexed for MEDLINE]
35: J Antimicrob Chemother. 2003 Sep;52(3):389-96. Epub 2003 Aug 13.
Comparison of microbial adherence to antiseptic and antibiotic central venous
catheters using a novel agar subcutaneous infection model.
Gaonkar TA, Modak SM.
College of Physicians and Surgeons, Department of Surgery, 630 West 168th
Street,
New York, NY 10032, USA.
An agar subcutaneous infection model (agar model), which simulates the rat
subcutaneous infection model (rat model), was developed to assess the ability of
antimicrobial catheters to resist microbial colonization. The catheters were
implanted in the agar and rat models and the insertion sites were infected
immediately or on day 7, 14 or 21 post-implantation. The catheters implanted in
the agar model were transferred to fresh media one day before infection on day
7,
14 or 21. The efficacy of chlorhexidine and silver sulfadiazine impregnated (CS)
catheters, CS catheters with higher levels of chlorhexidine (CS+ catheters),
minocycline-rifampicin (MR) catheters and silver catheters against
Staphylococcus
aureus and rifampicin-resistant Staphylococcus epidermidis RIF-r2 was compared
in
the agar and rat models. No significant difference in the adherence or the drug
release was found between the in vitro and in vivo models. In both models, CS+
and MR catheters were effective against S. aureus even when infected on day 14,
whereas CS catheters were colonized when challenged on day 7. CS+ catheters were
effective against S. epidermidis RIF-r2, whereas MR catheters showed adherence
when infected on day 7. CS+ catheters prevented colonization of all the
organisms
23
including, Enterobacter aerogenes, Escherichia coli, Klebsiella pneumoniae,
Pseudomonas aeruginosa and Candida albicans in the agar model, whereas MR
catheters were effective only against S. aureus and S. epidermidis strains.
Silver catheters were ineffective against all the organisms. The agar model may
be used to predict the in vivo efficacy of antimicrobial catheters against
various pathogens.
Publication Types:
Comparative Study
PMID: 12917250 [PubMed - indexed for MEDLINE]
36: Chest. 2003 Jul;124(1):275-84.
New choices for central venous catheters: potential financial implications.
Shorr AF, Humphreys CW, Helman DL.
Pulmonary and Critical Care Medicine Service, Department of Medicine, Walter
Reed
Army Medical Center, Washington, DC, USA. afshorr@dnamail.com
OBJECTIVE: To determine the cost-effectiveness of the newer antiseptic and
antibiotic-impregnated central venous catheters (CVCs) relative to uncoated CVCs
and to each other. DESIGN: Decision model analysis of the cost and efficacy of
CVCs coated with either chlorhexidine silver sulfadiazine (CSS) or
rifampin-minocycline (RM) at preventing catheter-related bloodstream infections
(CRBSIs). The primary outcome is the incremental cost (or savings) to prevent
one
additional CRBSI. Model estimates are derived from prospective trials of the CSS
and RM CVCs and from other studies describing the costs of CRBSIs. Setting and
patients: Hypothetical cohort of 1,000 patients requiring placement of a CVC.
INTERVENTIONS: In the model, patients were managed with either an uncoated CVC,
CSS CVC, or RM CVC. Measurements and main results: The incremental
cost-effectiveness of the treated CVCs was calculated as the savings resulting
from CRBSIs averted less the additional costs of the newer devices. Sensitivity
analysis of the effect of the major clinical inputs was performed. For the base
case analysis, we assumed the incidence of CRBSIs was 3.3% with traditional
catheters and that the CSS and RM CVC conferred a relative risk reduction for
the
development of CRBSIs of 60% and 85%, respectively. Despite their significantly
higher cost than older catheters, both novel CVCs yield significant savings.
Employing either of the treated CVCs saves approximately $10,000 per CRBSI
prevented (relative to standard catheters). Comparing the RM CVC to the CSS CVC
revealed the RM product to be economically superior, saving nearly $9,600 per
CRBSI averted and $81 per patient in the cohort. For sensitivity analysis, we
adjusted all model variables by 50% individually and then simultaneously. This
demonstrated the model to be most sensitive to the cost of a CRBSI; however,
with
all inputs skewed by 50% against both the CSS CVC and the RM CVC, these devices
remained economically attractive. Under this scenario, use of either treated
device was less costly. CONCLUSIONS: Utilization of antiseptic and
antibiotic-impregnated CVCs represent an attractive alternative for the
prevention of CRBSIs and may lead to significant savings. Of the two newer,
coated devices, the RM CVC performs better financially. These observations hold
over a range of estimates for our model inputs.
Publication Types:
Clinical Trial
Controlled Clinical Trial
PMID: 12853534 [PubMed - indexed for MEDLINE]
24
37: J Hosp Infect. 2003 May;54(1):10-7.
Effect of central venous catheter type on infections: a prospective clinical
trial.
Richards B, Chaboyer W, Bladen T, Schluter PJ.
Intensive Care Unit, Gold Coast Hospital, Southport, Qld, Australia.
This study reports on a block clinical trial of two types of central venous
catheters (CVCS): antiseptic-impregnated catheters (AIC) and non-impregnated
catheters (non-AIC), on catheter tip colonization and bacteraemia. In total, 500
catheters were inserted in 390 patients over the 18 month study period, 260
(52.0%) AIC and 240 (48.0%) non-AIC. Of these, 460 (92.0%) tips (237 AIC and 223
non-AIC) were collected. While significantly fewer AIC, 14 (5.9%), than non-AIC,
30 (13.5%), catheters were colonized (P<0.01), there was no difference in the
rates of bacteraemias in the two groups (0.8% vs. 2.7%, respectively, P=0.16).
There were 6.87 (95% CI 3.38-14.26) and 16.92 (95% CI 10.61-27.12) colonized AIC
and non-AIC catheters, respectively, per 1000 catheter days, a difference that
was significant (P<0.01). However, no difference emerged between bacteraemias in
AIC and non-AIC catheters per 1000 catheter days measured at 0.98 (95% CI
0.24-5.54) and 3.38 (95% CI 1.29-9.34), respectively (P=0.10). Of the 444 CVCs
that were sited in the subclavian or jugular veins and had tips collected,
significantly more catheters were colonized in the jugular group, 19 (20%),
compared with the subclavian group, 24 (6.9%; P< or =0.01). Overall, the low
rates of colonization and bacteraemia may be explained by the population
studied,
the policies used and the employment of a clinical nurse dedicated to CVC
management.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 12767841 [PubMed - indexed for MEDLINE]
38: Intensive Care Med. 2003 Mar;29(3):403-9. Epub 2003 Feb 8.
The relationship between methodological trial quality and the effects of
impregnated central venous catheters.
Geffers C, Zuschneid I, Eckmanns T, Rüden H, Gastmeier P.
Department of Hospital Hygiene, Charité, Heubnerweg 6, 14059 Berlin, Germany.
christine.geffers@charite.de
OBJECTIVE: We assessed the methodological trial quality of individual randomized
controlled studies on chlorhexidine silver sulfadiazine impregnated catheters
and
the effect on catheter-related infection (CRI). DESIGN: Only the studies
identified in the Medline database from 1966 to December 2001 were considered,
abstracts being excluded. The outcome of this investigation centered on
bloodstream CRI. The trial quality of the 11 studies identified and published
(total 3,131 catheters) was assessed using a scoring system based on allocation,
patient selection, patient characteristics, blinding of the intervention and the
diagnosis of CRI (range 0-2 points, 10 points maximum). RESULTS: The mean
methodological quality score was 7.1 (range 5-9). The relative risk reduction
for
bloodstream CRI ranged from -0.14 to 1.0. No association between trial quality
and the impact of chlorhexidine silver sulfadiazine impregnated catheters on CRI
was found. The summary odds ratio for CRI was 0.69 (95% CI 0.46-1.03). Taking
only those studies with 2 points for diagnosis of CRI a summary odds ratio of
0.87 (95% CI 0.44-1.72) resulted, whereas studies with a diagnosis score of only
25
1 point led to a summary odds ratio of 0.60 (95% CI 0.35-1.02). CONCLUSIONS: The
quality of the studies seems to have had no influence on the outcome, according
to the results of this investigation, but the use of only a single quality score
may not be sufficient to investigate the prevention effect of impregnated
catheters.
Publication Types:
Meta-Analysis
Research Support, Non-U.S. Gov't
PMID: 12577150 [PubMed - indexed for MEDLINE]
39: Am J Infect Control. 2003 Feb;31(1):1-8.
Which antimicrobial impregnated central venous catheter should we use? Modeling
the costs and outcomes of antimicrobial catheter use.
Marciante KD, Veenstra DL, Lipsky BA, Saint S.
Pharmaceutical Outcomes Research and Policy Program, Department of Pharmacy,
University of Washington, Seattle WA 98195, USA.
BACKGROUND: Catheter-related bloodstream infections are costly and associated
with substantial morbidity and mortality. Trials suggest that central venous
catheters impregnated with minocycline/rifampin, although more expensive, are
clinically superior to chlorhexidine/silver sulfadiazine impregnated catheters.
It remains unclear whether minocycline/rifampin catheters are cost-effective for
all high-risk patients or only those requiring longer-term catheterization.
METHODS: We developed a series of decision models with patient-level clinical
trial data to determine whether minocycline/rifampin catheters are costeffective
for patients requiring various durations of catheterization. We calculated
incremental cost-effectiveness ratios for patients catheterized for durations
ranging from 1 to 25 days. RESULTS: The data were too sparse to estimate
cost-effectiveness for patients catheterized less than 8 days. The probability
that minocycline/rifampin catheters were cost-effective compared with
chlorhexidine/silver sulfadiazine catheters in patients catheterized for 8 days
was 91%. The probability that the minocycline/rifampin catheters in patients
catheterized 13 days or longer resulted in cost savings was more than 95%.
CONCLUSIONS: Our analysis suggests that central venous catheters coated with
minocycline/rifampin are cost-effective for patients catheterized for at least 1
week and lead to overall cost savings when patients are catheterized for 2 weeks
or longer. Policies for the use of antimicrobial catheters in high-risk patients
should reflect patients' expected duration of catheterization.
Publication Types:
Comparative Study
Research Support, Non-U.S. Gov't
PMID: 12548250 [PubMed - indexed for MEDLINE]
40: Intensive Care Med. 2003 Jan;29(1):139. Epub 2002 Nov 20.
Cost-effectiveness of an antiseptic-impregnated central venous catheter in the
ICU.
Frank U, Chojnacki T, Dettenkofer M, Daschner FD.
Publication Types:
Letter
PMID: 12528036 [PubMed - indexed for MEDLINE]
26
41: Infect Control Hosp Epidemiol. 2002 Dec;23(12):759-69.
Guidelines for the prevention of intravascular catheter-related infections.
O'Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur
H,
McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA;
Healthcare Infection Control Practices Advisory Committee.
Clinical Center, National Institutes of Health, Bethesda, Maryland, USA.
BACKGROUND: Although many catheter-related bloodstream infections (CRBSIs) are
preventable, measures to reduce these infections are not uniformly implemented.
OBJECTIVE: To update an existing evidenced-based guideline that promotes
strategies to prevent CRBSIs. DATA SOURCES: The MEDLINE database, conference
proceedings, and bibliographies of review articles and book chapters were
searched for relevant articles. STUDIES INCLUDED: Laboratory-based studies,
controlled clinical trials, prospective interventional trials, and epidemiologic
investigations. OUTCOME MEASURES: Reduction in CRBSI, catheter colonization, or
catheter-related infection. SYNTHESIS: The recommended preventive strategies
with
the strongest supportive evidence are education and training of healthcare
providers who insert and maintain catheters; maximal sterile barrier precautions
during central venous catheter insertion; use of a 2% chlorhexidine preparation
for skin antisepsis; no routine replacement of central venous catheters for
prevention of infection; and use of antiseptic/antibiotic-impregnated short-term
central venous catheters if the rate of infection is high despite adherence to
other strategies (ie, education and training, maximal sterile barrier
precautions, and 2% chlorhexidine for skin antisepsis). CONCLUSION: Successful
implementation of these evidence-based interventions can reduce the risk for
serious catheter-related infection.
Publication Types:
Guideline
Research Support, Non-U.S. Gov't
PMID: 12517020 [PubMed - indexed for MEDLINE]
42: Infect Control Hosp Epidemiol. 2002 Dec;23(12):748-56.
Prevention of bloodstream infections with central venous catheters treated with
anti-infective agents depends on catheter type and insertion time: evidence from
a meta-analysis.
Walder B, Pittet D, Tramèr MR.
Division of Surgical Intensive Care, University of Geneva Hospitals, Geneva,
Switzerland.
OBJECTIVE: To test the evidence that the risk of infection related to central
venous catheters (CVCs) is decreased by anti-infective coating or cuffing.
DESIGN: Systematic review of randomized, controlled trials comparing
anti-infective with inactive (control) CVCs. INTERVENTIONS: Average insertion
times were taken as a measurement of the length of insertion. Dichotomous data
were combined using a fixed effect model and expressed as odds ratio (OR) with
95% confidence interval (CI95). RESULTS: Two trials on antibiotic coating (343
CVCs) had an average insertion time of 6 days; the risk of BSI decreased from
5.1% with control to 0% with anti-infective catheters. There were no trials with
longer average insertion times. In three trials on silver collagen cuffs (422
CVCs), the average insertion time ranged from 5 to 8.2 days (median, 7 days);
the
risk of BSI was 5.6% with control and 3.2% with anti-infective catheters. In
27
another trial on silver collagen cuffs (101 CVCs), the average insertion time
was
38 days; the risk of BSI was 3.7% with control and 4.3% with anti-infective
catheters. In five trials on chlorhexidine-silver sulfadiazine coating (1,269
CVCs), the average insertion time ranged from 5.2 to 7.5 days (median, 6 days);
the risk of BSI decreased from 4.1% with control to 1.9% with anti-infective
catheters. In five additional trials on chlorhexidine-silver sulfadiazine
coating
(1,544 CVCs), the average insertion time ranged from 7.8 to 20 days (median, 12
days); the risk of BSI was 4.5% with control and 4.2% with anti-infective
catheters. CONCLUSIONS: Antibiotic and chlorhexidine-silver sulfadiazine
coatings
are anti-infective for short (approximately 1 week) insertion times. For longer
insertion times, there are no data on antibiotic coating, and there is evidence
of lack of effect for chlorhexidine-silver sulfadiazine coating. For
silver-impregnated collagen cuffs, there is evidence of lack of effect for both
short- and long-term insertion.
Publication Types:
Meta-Analysis
Research Support, Non-U.S. Gov't
PMID: 12517018 [PubMed - indexed for MEDLINE]
43: Am J Infect Control. 2002 Dec;30(8):476-89.
Guidelines for the prevention of intravascular catheter-related infections.
O'grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur
H,
McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA;
Healthcare Infection Control Practices Advisory Committee.
Clinical Center, National Institutes of Health, Bethesda, MD, USA.
BACKGROUND: Although many catheter-related bloodstream infections (CR-BSIs) are
preventable, measures to reduce these infections are not uniformly implemented.
OBJECTIVE: To update an existing evidenced-based guideline that promotes
strategies to prevent CR-BSIs.Data Sources: The MEDLINE database, conference
proceedings, and bibliographies of review articles and book chapters were
searched for relevant articles.Studies Included: Laboratory-based studies,
controlled clinical trials, prospective interventional trials, and
epidemiological investigations.Outcome Measures: Reduction in CR-BSI, catheter
colonization, or catheter-related infection. SYNTHESIS: The recommended
preventive strategies with the strongest supportive evidence are education and
training of healthcare providers who insert and maintain catheters; maximal
sterile barrier precautions during central venous catheter insertion; use of a
2%
chlorhexidine preparation for skin antisepsis; no routine replacement of central
venous catheters for prevention of infection; and use of antiseptic/antibiotic
impregnated short-term central venous catheters if the rate of infection is high
despite adherence to other strategies (i.e. education and training, maximal
sterile barrier precautions and 2% chlorhexidine for skin antisepsis).
CONCLUSION: Successful implementation of these evidence-based interventions can
reduce the risk for serious catheter-related infection.
Publication Types:
Guideline
Review
PMID: 12461511 [PubMed - indexed for MEDLINE]
44: Medicine (Baltimore). 2002 Nov;81(6):466-79.
28
A review of risk factors for catheter-related bloodstream infection caused by
percutaneously inserted, noncuffed central venous catheters: implications for
preventive strategies.
Safdar N, Kluger DM, Maki DG.
Department of Medicine, University of Wisconsin Medical School and University of
Wisconsin Hospitals and Clinics, Madison, 53792, USA.
Strategies for preventing central venous catheter (CVC)-related bloodstream
infection are most likely to be effective if guided by an understanding of the
risk factors associated with these infections. In this critical review of
published studies of risk factors for CVC-related bloodstream infection that
were
prospective and used multivariable techniques of data analysis or that were
randomized trials of a preventive measure, a significantly increased risk of
catheter-related bloodstream infection was associated with inexperience of the
operator and nurse-to-patient ratio in the intensive care unit, catheter
insertion with less than maximal sterile barriers, placement of a CVC in the
internal jugular or femoral vein rather than subclavian vein, placement in an
old
site by guidewire exchange, heavy colonization of the insertion site or
contamination of a catheter hub, and duration of CVC placement > 7 days.
Prospective studies or randomized trials of control measures focusing on these
risk factors have been shown to reduce risk significantly: formal training in
CVC
insertion and care, use of maximal sterile barriers at insertion, use of
chlorhexidine rather than povidone-iodine for cutaneous antisepsis, applying a
topical anti-infective cream or ointment or a chlorhexidine-impregnated dressing
to the insertion site, and the use of novel catheters with an anti-infective
surface or a contamination resistant hub. Better prospective studies of
sufficient size to address all potential risk factors, including insertion site
and hub colonization, insertion technique, and details of follow-up care, would
enhance our understanding of the pathogenesis of CVC-related bloodstream
infection and guide efforts to develop more effective strategies for prevention.
Publication Types:
Review
PMID: 12441903 [PubMed - indexed for MEDLINE]
45: Pediatrics. 2002 Nov;110(5):e51.
Guidelines for the prevention of intravascular catheter-related infections. The
Hospital Infection Control Practices Advisory Committee, Center for Disese
Control and Prevention, u.s.
O'Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur
H,
McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA.
National Institutes of Health, Department of Critical Care Medicine, Bethesda,
Maryland 20892, USA.
These guidelines have been developed for practitioners who insert catheters and
for persons responsible for surveillance and control of infections in hospital,
outpatient, and home health-care settings. This report was prepared by a working
group comprising members from professional organizations representing the
disciplines of critical care medicine, infectious diseases, health-care
infection
control, surgery, anesthesiology, interventional radiology, pulmonary medicine,
pediatric medicine, and nursing. The working group was led by the Society of
29
Critical Care Medicine (SCCM), in collaboration with the Infectious Disease
Society of America (IDSA), Society for Healthcare Epidemiology of America
(SHEA),
Surgical Infection Society (SIS), American College of Chest Physicians (ACCP),
American Thoracic Society (ATS), American Society of Critical Care
Anesthesiologists (ASCCA), Association for Professionals in Infection Control
and
Epidemiology (APIC), Infusion Nurses Society (INS), Oncology Nursing Society
(ONS), Society of Cardiovascular and Interventional Radiology (SCVIR), American
Academy of Pediatrics (AAP), and the Healthcare Infection Control Practices
Advisory Committee (HICPAC) of the Centers for Disease Control and Prevention
(CDC) and is intended to replace the Guideline for Prevention of Intravascular
Device-Related Infections published in 1996. These guidelines are intended to
provide evidence-based recommendations for preventing catheter-related
infections. Major areas of emphasis include 1) educating and training healthcare
providers who insert and maintain catheters; 2) using maximal sterile barrier
precautions during central venous catheter insertion; 3) using a 2%
chlorhexidine
preparation for skin antisepsis; 4) avoiding routine replacement of central
venous catheters as a strategy to prevent infection; and 5) using
antiseptic/antibiotic impregnated short-term central venous catheters if the
rate
of infection is high despite adherence to other strategies (ie, education and
training, maximal sterile barrier precautions, and 2% chlorhexidine for skin
antisepsis). These guidelines also identify performance indicators that can be
used locally by health-care institutions or organizations to monitor their
success in implementing these evidence-based recommendations.
Publication Types:
Guideline
Practice Guideline
PMID: 12415057 [PubMed - indexed for MEDLINE]
46: Curr Opin Crit Care. 2002 Oct;8(5):441-8.
Central line infections.
Lane RK, Matthay MA.
Department of Internal Medicine, Division of Pulmonary and Critical Care
Medicine, Yale University School of Medicine, New Haven, Connecticut, USA.
Central venous catheters are commonly used in the critical care setting.
Unfortunately, their use is often associated with complications, including fatal
infections. Making the diagnosis of central venous catheter infection can be
difficult. Additionally, resistance among the more common organisms that cause
catheter-related infection is increasing. However, our understanding of the
pathogenesis of catheter infection is improving through examination of biofilms.
Also, our ability to diagnose catheter-related infections more accurately is
improving with new techniques. There is new hope for ruling out catheter-related
infection before removal by several methods, including a rapid enzyme-linked
immunosorbent assay and the use of time differential for microbial growth
between
blood cultures obtained from a peripheral site and the catheter itself.
Prevention through the use of barrier techniques and antimicrobial-coated
catheters has been demonstrated to be of value in reducing catheter-related
infection with these devices.
Publication Types:
Research Support, U.S. Gov't, P.H.S.
Review
30
PMID: 12357113 [PubMed - indexed for MEDLINE]
47: MMWR Recomm Rep. 2002 Aug 9;51(RR-10):1-29.
Guidelines for the prevention of intravascular catheter-related infections.
Centers for Disease Control and Prevention.
O'Grady NP, Alexander M, Dellinger EP, Gerberding JL, Heard SO, Maki DG, Masur
H,
McCormick RD, Mermel LA, Pearson ML, Raad II, Randolph A, Weinstein RA.
National Institutes of Health, Bethesda, Maryland, USA.
These guidelines have been developed for practitioners who insert catheters and
for persons responsible for surveillance and control of infections in hospital,
outpatient, and home health-care settings. This report was prepared by a working
group comprising members from professional organizations representing the
disciplines of critical care medicine, infectious diseases, health-care
infection
control, surgery anesthesiology interventional radiology pulmonary medicine,
pediatric medicine, and nursing. The working group was led by the Society of
Critical Care Medicine (SCCM), in collaboration with the Infectious Disease
Society of America (IDSA), Society for Healthcare Epidemiology ofAmerica (SHEA),
Surgical Infection Society (SIS), American College of Chest Physicians (ACCP),
American Thoracic Society (ATS), American Society of Critical Care
Anesthesiologists (ASCCA), Association for Professionals in Infection Control
and
Epidemiology (APIC), Infusion Nurses Society (INS), Oncology Nursing Society
(ONS), Society of Cardiovascular and Interventional Radiology (SCVIR), American
Academy of Pediatrics (AAP), and the Healthcare Infection Control Practices
Advisory Committee (HICPAC) of the Centers for Disease Control and Prevention
(CDC) and is intended to replace the Guideline for Prevention of Intravascular
Device-Related Infections published in 1996 These guidelines are intended to
provide evidence-based recommendations for preventing catheter-related
infections. Major areas of emphasis include 1) educating and training healthcare
providers who insert and maintain catheters; 2) using maximal sterile barrier
precautions during central venous catheter insertion; 3) using a 2%
chlorhexidine
preparation for skin antisepsis; 4) avoiding routine replacement of central
venous catheters as a strategy to prevent infection; and 5) using
antiseptic/antibiotic impregnated short-term central venous catheters if the
rate
of infection is high despite adherence to other strategies (i.e., education and
training, maximal sterile barrier precautions, and 2% chlorhexidine for skin
antisepsis). These guidelines also identify performance indicators that can be
used locally by health-care institutions or organizations to monitor their
success in implementing these evidence-based recommendations.
Publication Types:
Guideline
Practice Guideline
PMID: 12233868 [PubMed - indexed for MEDLINE]
48: J Crit Care. 2002 Jun;17(2):114-21.
Applying the science to the prevention of catheter-related infections.
O'Grady NP.
Warren Magnusen Clinical Center, National Institutes of Health, Bethesda, MD
31
20892, USA.
BACKGROUND: Catheter-related bloodstream infection (CR-BSI) remains a leading
cause of nososcomial infection, despite the fact that many CR-BSIs are
preventable. Simple principles of infection control and the use of novel devices
to reduce these infections are not uniformly implemented. OBJECTIVE: To review
and summarize the evidence that promotes strategies to prevent CR-BSIs. DATA
SOURCES: The Medline database and bibliographies of review articles and book
chapters were searched for relevant articles. STUDIES INCLUDED: In vitro and in
vivo laboratory-based studies, controlled clinical trials, prospective
interventional trials, and epidemiologic investigations. OUTCOME MEASURES:
Reduction in CR-BSI, catheter colonization, tunnel infection, or local site
infection. SYNTHESIS: The recommended prevention strategies with strong
supportive evidence include educating and training of health care providers who
insert and maintain catheters; using full barrier precautions during central
venous catheter insertion; using a 2% chlorhexidine preparation for skin
antisepsis; eliminating the practice of scheduled replacement of central venous
catheters for prevention of infection; and using antiseptic/antibiotic
impregnated short-term central venous catheters. CONCLUSION: Simple
interventions
can reduce the risk for serious catheter-related infection. Health care provider
awareness and adherence to these prevention strategies is critical to reducing
the risk for CR-BSI, improving patient safety, and promoting quality health
care.
Copyright 2002, Elsevier Science (USA). All rights reserved.
Publication Types:
Review
PMID: 12096374 [PubMed - indexed for MEDLINE]
49: Eur J Clin Microbiol Infect Dis. 2002 May;21(5):379-84. Epub 2002 May 14.
In vitro evaluation of the antibacterial activity of three different central
venous catheters against gram-positive bacteria.
Yorganci K, Krepel C, Weigelt JA, Edmiston CE.
G.M.K. Bulvari 129/9 Koz Apt., 06530 Maltepe, Ankara, Turkey.
yorganci@hacettepe.edu.tr
The aim of this study was to evaluate the activity of three different catheters
against Staphylococcus aureus ATCC 29213 and the slime-producing Staphylococcus
epidermidis ATCC 35984 (RP62A). Three central venous catheters were evaluated:
one impregnated with silver sulfadiazine-chlorhexidine, one to which
minocycline/rifampin is bonded and a novel one into which silver, platinum and
carbon are incorporated. A nonantiseptic catheter was used as the control
catheter. One-centimeter trisected pieces of catheter were immersed in
phosphate-buffered saline (0.01 mol/l) with 0.25% dextrose and incubated. On
days
1, 3, 7, 14 and 21, a 1 ml standardized inoculum was added for 30 min and then
replaced with phosphate-buffered saline with 0.25% dextrose. One-third of the
samples were immediately sonicated and plated to determine bacterial adherence.
The remaining segments were incubated for 4 and 24 h to determine the
persistence
of bacterial adherence. Bacterial adherence to the catheters impregnated with
silver sulfadiazine-chlorhexidine was reduced 91-98% for the first 7 days.
Adherence of Staphylococcus aureus to catheters into which silver, platinum and
carbon are incorporated was reduced 70% on day 1 and 35% on day 3. Adherence to
minocycline/rifampin-bonded catheters was quite variable. There was an 85.699.8%
reduction in the persistence of bacterial adherence to the three catheters
compared to controls. Bacteriostatic and bactericidal studies indicated that the
32
effluents from the catheters impregnated with silver sulfadiazine-chlorhexidine
were bactericidal, while effluents from the minocycline/rifampin-bonded
catheters
were bacteriostatic. The antibacterial activity of the effluents from catheters
impregnated with silver sulfadiazine-chlorhexidine dissipated by day 7, while
the
activity of effluents from the minocycline/rifampin-bonded catheters continued
to
show activity at day 21. No measurable antibacterial activity was detected in
the
effluents of the catheters into which silver, platinum and carbon are
incorporated. These data suggest that catheters coated with
antibiotic/antibacterial agents and the novel catheters that incorporate
antiseptic agents have different activities against initial bacterial adherence.
All of them, however, effectively prevent bacterial colonization by grampositive
bacteria.
Publication Types:
Comparative Study
Evaluation Studies
Research Support, Non-U.S. Gov't
PMID: 12072923 [PubMed - indexed for MEDLINE]
50: Intensive Care Med. 2002 Apr;28(4):438-42. Epub 2002 Mar 15.
Activity of antibacterial impregnated central venous catheters against
Klebsiella
pneumoniae.
Yorganci K, Krepel C, Weigelt JA, Edmiston CE.
Hacettepe University, Faculty of Medicine, Department of General Surgery,
Ankara,
Turkey. yorganci@ada.net.tr
OBJECTIVE: Antibiotically coated or impregnated catheters are effective in
eliminating gram-positive bacteria from their surfaces. However, their activity
against gram-negative bacteria is not well known. The aim of this study was to
evaluate and compare the adherence, persistence and colonization of Klebsiella
pneumoniae on catheter surfaces and also to assess bacteriostatic and
bactericidal levels. DESIGN: Randomized, controlled, laboratory study. SETTING:
University surgical microbiology laboratory. SUBJECTIVE: Silver
sulfadiazine-chlorhexidine impregnated (SSC), minocycline and rifampin bonded
(M+R), silver, platinum and carbon incorporated (SP+C) and non-antiseptic
central
venous catheter segments. INTERVENTIONS: Catheter segments were immersed in 1 ml
of phosphate buffered saline (0.01 mol/l) with 0.25% dextrose (PBSD) and
incubated at 37 degrees C. The PBSD was replaced daily. Effluents were frozen at
-70 degrees C for subsequent determination of bacteriostatic and bactericidal
activity. On days 1,3,7,14 and 21 after initial immersion, 1 ml standardized
inoculum of Klebsiella pneumoniae was added to 90 tubes for a period of 30 min.
The inoculum was then replaced with PBSD. One third of the samples were
immediately sonicated and plated for the determination of bacterial adherence.
The remaining segments were incubated for 4 and 24 h, followed by the same
procedure to determine bacterial persistence and colonization with time. All
plates were read after 24 h of incubation. MEASUREMENTS AND RESULTS: There was a
significant reduction in initial bacterial adherence for SP+C catheters on all
days ( p<0.05). SSC catheters prevented initial bacterial adherence for the
first
7 days only ( p<0.05). SSC and SP+C catheters prevented bacterial persistence
and
33
further colonization on all days. However M+R catheters prevented bacterial
colonization for 3 days only. Effluent studies indicated that the impregnated
agents in catheter SSC were bactericidal compared to catheter M+R, which were
bacteriostatic to K. pneumoniae. No antibacterial activity was detected in the
effluents from catheter SP+C. CONCLUSIONS: SSC and SP+C catheters are effective
in eliminating K. pneumoniae from their surfaces for at least 21 days. M+R
catheters are less effective in eliminating bacterial adherence and colonization
may be due to their bacteriostatic property.
Publication Types:
Clinical Trial
Comparative Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 11967598 [PubMed - indexed for MEDLINE]
51: Clin Infect Dis. 2002 May 1;34(9):1232-42. Epub 2002 Apr 2.
The promise of novel technology for the prevention of intravascular
device-related bloodstream infection. I. Pathogenesis and short-term devices.
Crnich CJ, Maki DG.
Section of Infectious Diseases, Department of Medicine, University of Wisconsin
Medical School, Madison, WI, USA.
Intravascular devices (IVDs) are widely used for vascular access but are
associated with substantial risk of development of IVD-related bloodstream
infection (BSI). The development of novel technologies, which are based on an
understanding of pathogenesis, promises a quantum reduction in IVD-related
infections in an era of growing nursing shortages. Infections of short-term IVDs
(that is, those in place <10 days), including peripheral venous catheters,
noncuffed and nontunneled central venous catheters (CVCs), and arterial
catheters, derive mainly from microorganisms colonizing the skin around the
insertion site, which most often gain access extraluminally. More-effective
cutaneous antiseptics, such as chlorhexidine, a chlorhexidine-impregnated sponge
dressing, CVCs with an anti-infective coating, anti-infective CVC hubs, and
novel
needleless connectors, have all been shown to reduce the risk of IVD-related BSI
in prospective randomized trials. The challenge for the future will be to
identify new preventative technologies and to begin to adapt more widely those
technologies already shown to be efficacious and cost-effective.
Publication Types:
Research Support, Non-U.S. Gov't
Review
PMID: 11941550 [PubMed - indexed for MEDLINE]
52: J Chemother. 2001 Nov;13 Spec No 1(1):234-8.
The prevention of central venous catheter-related sepsis.
Elliott TS.
University Hospital Birmingham NHS Trust, UK.
tom.elliott@university-b.wmids.nhs.uk
Intravascular catheters continue to be a major source of sepsis which range from
localised inflammation at the site of insertion to septicaemia. There are two
main approaches which have been taken in an attempt to prevent these infections.
34
These can be divided into the patient and the catheter. Approaches for
prevention
with patients include improved aseptic techniques, appropriate choice of
antiseptic skin preparations, use of semi-occlusive dressings and cleaning
schedules when using the devices. Catheters have also been developed to reduce
the incidence of these infections. These include the production of polymers with
smooth, anti-adhesive coatings, eg Hydromer, and more recently the introduction
of devices which are either coated with antiseptics or antimicrobials. The
antimicrobial coatings include antibiotics such as rifampicin and doxycycline or
antiseptics, for example benzalkonium chloride or chlorhexidine. The efficacy of
these approaches will be reviewed based on both laboratory and clinical studies.
The treatment of intravascular catheter-related sepsis depends primarily on
establishing the diagnosis. When the diagnosis has been made treatment ranges
from the use of antimicrobials alone to removal of the device. More recent
approaches have included the use of antibiotic locks within the catheters.
Treatment schedules will also be reviewed.
Publication Types:
Review
PMID: 11936372 [PubMed - indexed for MEDLINE]
53: Rev Esp Anestesiol Reanim. 2002 Jan;49(1):17-33.
[Prophylaxis of infective complications of central venous catheters]
[Article in Spanish]
Gómez Luque A, Huertas Simonet N, Viciana Ramos MI, Moreno Palacios M, Hernández
Pardo PE.
Departamento de Farmacología, Facultad de Medicina de Málaga, Facultativo
Especialista de Area Servicio de Anestesiología, Reanimación y Terapéutica del
Dolor, Hospital Clínico Universitario de Málaga. jagomez@uma.es
Infections related to central venous cannulation present first-magnitude
problems
in recovery rooms and intensive care units. Catheter-related bloodstream
infection (CRBSI) is the most serious complication because of its high frequency
and a mortality rate that averages around 3%. Although infections arise for
various reasons, point-of-insertion contamination is the main cause when
catheters are implanted for periods of less than 10 days. Contaminating
microorganisms (especially Staphyloccocus epidermidis) find refuge from the
host's defenses in a biofilm that covers the catheter. Several factors
participate in the formation of this biofilm, such as catheter composition,
proteins of the host or type of microorganism. Biofilm bacteria are resistant to
both antibiotics and the host's own defenses (e.g. phagocytes and antibodies).
The microorganism can then begin to reproduce, possibly leading to bloodstream
infection. The measures designed to prevent this process include recommendations
for both catheter insertion and maintenance. Recent meta-analyses have led to
certain conclusions but no unanimity among authors. Thus, there is agreement on
the adoption of strict aseptic technique during catheter insertion, on the use
of
chlorhexidine as a skin antiseptic and on choice of the subclavian vein. Such
measures significantly decrease the frequency of CRBSI. Maintenance techniques
that have been shown to be effective are the use of connectors impregnated with
antiseptic, catheters impregnated with antiseptics or antibiotics, and permeable
dressings. Additionally, building an experienced infusion-therapy team to insert
and maintain central venous catheters has been shown to be one of the most
effective measures for preventing CRBSI.
Publication Types:
English Abstract
35
Meta-Analysis
PMID: 11898444 [PubMed - indexed for MEDLINE]
54: J Hosp Infect. 2002 Mar;50(3):202-6.
Contamination of central venous catheters in immunocompromised patients: a
comparison between two different types of central venous catheters.
Stoiser B, Kofler J, Staudinger T, Georgopoulos A, Lugauer S, Guggenbichler JP,
Burgmann H, Frass M.
Department of Internal Medicine I (Division of Infectious Diseases and
Chemotherapy), University of Vienna, Austria. brigitte.stoiser@akh-wien.ac.at
Catheters impregnated with silver have been proposed as a means of reducing
catheter-related infection. We therefore performed a prospective randomized
study
to compare a new silver-impregnated central venous catheter (CVC) with a
commercially available CVC in a cohort of immunocompromised patients. We studied
157 patients of whom 97 could be analysed. The median indwelling time in the
study group (SC) was 10.5 days and 11 days in the control group (CC). The
incidence of contamination in the SC group was 15.6 vs 24.6 in the CC group
referring to 1000 catheter days. In both groups, we found 6% of catheter-related
infections according to the definitions of a published scoring system. The
differences between the two groups were not significant. We conclude that the SC
decrease the incidence of catheter contamination and may have a positive effect
on the reduction of CVC-related infections. Copyright 2002 The Hospital
Infection
Society.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 11886196 [PubMed - indexed for MEDLINE]
55: Br J Anaesth. 2002 Feb;88(2):304-5; author reply 305.
Comment on:
Br J Anaesth. 2001 Aug;87(2):306-8.
Allergy to chlorhexidine-coated central venous catheters revisited.
Pittaway A, Ford S.
Publication Types:
Case Reports
Comment
Letter
PMID: 11878670 [PubMed - indexed for MEDLINE]
56: Cancer. 2002 Jan 1;94(1):245-51.
Catheter-related infection and thrombosis of the internal jugular vein in
hematologic-oncologic patients undergoing chemotherapy: a prospective comparison
of silver-coated and uncoated catheters.
Harter C, Salwender HJ, Bach A, Egerer G, Goldschmidt H, Ho AD.
Department of Internal Medicine V, University of Heidelberg, Heidelberg,
Germany.
36
Christoph.Harter@t-online.de
BACKGROUND: Catheter-related venous thrombosis is one of the most frequent
complications of central venous catheters (CVCs). This complication occurs in 440% of patients with hematologic malignancies receiving conventional
chemotherapy
after placement of CVCs. METHODS: The objective of this prospective study was to
assess whether a silver-coated CVC poses an additional risk in the development
of
catheter-related thrombosis in hematologic-oncologic patients. Patients were
randomized to receive either silver-coated polyurethane catheters (BactiGuard;
Metacot, Stockholm, Sweden) or uncoated standard polyurethane catheters
(Cavatheter, Fresenius AG, Bad Homburg, Germany) for central venous access.
Silver-coated catheters (n = 120) and standard catheters (n = 113) were inserted
into the jugular vein in 233 consecutive patients. Variables that may be
significant for the development of thrombosis were comparable in the two groups.
After removal of the CVC, the patency of both jugularian veins internal as well
as external was assessed with real-time ultrasound (Sonolayer-SAL-35A; Toshiba,
Tokyo, Japan). RESULTS: Four of 233 patients (1.5%) were found to have venous
thrombosis. Incomplete occlusion of the internal jugular vein occurred in 2
patients (0.75%, parietal thrombosis), and complete thrombosis, although
clinically silent, was found in 2 patients (0.75%). There was no difference
between patients with silver-coated and uncoated CVCs. CONCLUSIONS: The authors
concluded that this novel silver-coated CVC does not cause a higher rate of
central venous thrombosis compared with standard CVCs. The low overall incidence
of central venous thrombosis might be attributed to the routine application of
low-dose heparin in our patients during chemotherapeutic treatment. Copyright
2002 American Cancer Society.
Publication Types:
Clinical Trial
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
PMID: 11815983 [PubMed - indexed for MEDLINE]
57: J Chemother. 2001 Dec;13(6):595-606.
Efficacy of antiadhesive, antibiotic and antiseptic coatings in preventing
catheter-related infections: review.
Donelli G, Francolini I.
Laboratorio di Ultrastrutture, Istituto Superiore di Sanità, Rome, Italy.
donelli@iss.it
In recent years, central venous catheters (CVCs) are increasingly used in
clinical practice. However, complications such as local or systemic infections
are frequent for both temporary and indwelling vascular catheters. Annually, in
the United States of America there are more than 200,000 cases of nosocomial
bloodstream infections (BSIs), of which 90% are related to the use of an
intravascular device. These infections are associated with increased morbidity
and mortality, prolonged hospitalization and growing medical costs.
Technological
treatments of polymer surfaces including coating the catheter with antimicrobial
substances may be promising tools for prevention of catheter-associated
infections. A large number of surface-treated central venous catheters are now
commercially available. In this paper the features and the clinical efficacy of
different antimicrobial coatings are reviewed.
Publication Types:
Research Support, Non-U.S. Gov't
Review
37
PMID: 11806619 [PubMed - indexed for MEDLINE]
58: Pediatr Infect Dis J. 2002 Jan;21(1):63-4.
Antimicrobial-impregnated central venous catheters.
Schutze GE.
University of Arkansas for Medical Sciences, Arkansas Children's Hospital,
Little
Rock, AR, USA.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 11791103 [PubMed - indexed for MEDLINE]
59: Anaesth Intensive Care. 2001 Dec;29(6):600-3.
The effect of the biopatch, a chlorhexidine impregnated dressing, on bacterial
colonization of epidural catheter exit sites.
Mann TJ, Orlikowski CE, Gurrin LC, Keil AD.
Department of Anaesthesia, Women and Infants Research Foundation, King Edward
Memorial Hospital, Perth, Western Australia.
We performed a prospective, randomized study in 55 ASA I to 3 women undergoing
elective gynaecological surgery followed by postoperative epidural analgesia. We
compared the incidence of bacterial colonization at the epidural exit site
following catheter removal between a control group and an experimental group who
received a chlorhexidine impregnated dressing (Biopatch, Johnson and Johnson,
Arlington, TX, U.S.A.). Positive culture results were found in 11 of 27 (40.1%)
patients in the control group compared with one of 29 (3.4%) patients whose
epidural catheters were dressed with the Biopatch. We concluded that the
Biopatch
was effective in reducing bacterial colonization of the epidural catheter exit
site.
Publication Types:
Clinical Trial
Comparative Study
Randomized Controlled Trial
PMID: 11771602 [PubMed - indexed for MEDLINE]
60: Ann Pharmacother. 2001 Oct;35(10):1255-63.
Antimicrobial-coated/bonded and -impregnated intravascular catheters.
Pai MP, Pendland SL, Danziger LH.
College of Pharmacy, University of New Mexico, Albuquerque, USA.
OBJECTIVE: To review the literature regarding the prevention of catheter
colonization and catheter-related bloodstream infections (CRBIs) with the use of
antimicrobial-coated/bonded and -impregnated intravascular catheters. DATA
SOURCES: Primary and review English-language literature were identified using
MEDLINE (1966-September 2000) pertaining to the key terms antibiotic,
antimicrobial, antiseptic, silver, and bonded, coated, Impregnated catheters. In
addition, textbooks and relevant reference lists were reviewed. DATA EXTRACTION:
All articles identified through the data sources were evaluated. Information
38
deemed relevant to the objectives of the review was included. DATA SYNTHESIS:
Significant morbidity and mortality are associated with the development of
CRBIs.
Preventative measures such as modification of these catheters with antimicrobial
coating/bonding have produced varying results. Trials evaluating cefazolin,
teicoplanin, vancomycin, silver, and chlorhexidine-silver sulfadiazine (C-SS)
used for coated/bonded intravascular catheters have not demonstrated a
consistent
decrease in the incidence of CRBIs. However, a meta-analysis of trials
evaluating
C-SS intravascular catheters demonstrated a statistically significant reduction
in CRBIs. A larger reduction in CRBIs has been reported with minocyclinerifampin
(M-R) versus C-SS intravascular catheters. Use of the M-R and C-SS catheters may
result in a cost savings of $100 million and reduce as many as 12,000
CRBI-related deaths annually when used short term (<7 d). CONCLUSIONS: When used
for short-term catheterization, M-R catheters appear to be superior to the
currently available C-SS catheters at preventing CRBIs. Significant cost savings
and reduction in mortality can be anticipated with the use of M-R catheters.
Publication Types:
Review
PMID: 11675856 [PubMed - indexed for MEDLINE]
61: Curr Opin Clin Nutr Metab Care. 2001 May;4(3):211-8.
Comment in:
Curr Opin Clin Nutr Metab Care. 2001 May;4(3):197-200.
Evidence-based prevention of catheter infection during parenteral nutrition.
Attar A, Messing B.
Hepato-Gastroenterology Department and Nutritional Support Unit, Approved Centre
for HPN in adults for the Ile de France region, Lariboisière Hospital, Paris,
France.
Parenteral nutrition is a risk factor for catheter-related bloodstream
infection.
Here we reviewed strategies for the prevention of catheter-related infections,
which always must begin with the cornerstone of prevention: the strict adherence
to aseptic techniques. Most research has been interested in coated catheters.
From these results, it may be concluded that antibiotics or
antiseptic-impregnated catheters, like those with minocycline-rifampicin or
chlorhexidine/silver sulfadiazine, significantly reduce catheter-related blood
stream infections. Antibiotics or antiseptic-impregnated central venous
catheters
may even result in cost saving in intensive care units. Antiseptic or
antibiotic-lock techniques would also be of interest to prevent catheter-related
sepsis in high-risk patients who are receiving parenteral nutrition.
Publication Types:
Review
PMID: 11517355 [PubMed - indexed for MEDLINE]
62: Ann Acad Med Singapore. 2001 Jul;30(4):419-29.
Catheter-related infection: diagnosis, prevention and treatment.
Heard SO.
39
Department of Anesthesiology, Umass Memorial Medical Center, 55 Lake Avenue
North, Worcester, MA 01655, USA. stephen.heard@umassmed.edu
INTRODUCTION: Catheter infection continues to be a serious problem in critically
ill patients. This review will examine the incidence, epidemiology,
microbiology,
diagnosis, risk factors for and treatment of catheter-related bloodstream
infections. METHODS: Relevant articles were culled from a Medline search and
other review articles on catheter-related infection. Important abstracts
presented within the past year were included in the review if the data had not
been published in a peer-reviewed journal. RESULTS: Catheter-related bloodstream
infections (CRBSI) increase morbidity and the cost of care of patients. The
predominant organisms associated with CRBSI are coagulase negative
staphylococci,
enterococci and Staphylococcus aureus. Diagnosis usually requires catheter
removal and culture but newer techniques such as "differential time to
positivity" may permit diagnosis of CRBSI in situ. Reducing risk factors for
infection are important: education of house staff, use of the subclavian
insertion site, skin preparation with chlorhexidine solutions, use of maximum
barrier precautions during catheter insertion and catheter maintenance with
chlorhexidine sponges. If infection rates are still high after institution of
these measures, use of antiseptic or antibiotic-impregnated catheters should be
considered. Treatment of CRBSI in critically ill patients mandates catheter
removal and treatment with systemic antibiotics. CONCLUSIONS: The best treatment
for CRBSI is prevention. Ongoing studies are evaluating the effectiveness of
newer antiseptic catheters, the risk of developing antibiotic resistance when
using antibiotic-impregnated catheters and the contribution of multiple
interventions on the development of CRBSI.
Publication Types:
Review
PMID: 11503552 [PubMed - indexed for MEDLINE]
63: Br J Anaesth. 2001 Aug;87(2):306-8.
Comment in:
Br J Anaesth. 2001 Dec;87(6):940-1; author reply 941.
Feb;88(2):304-5; author reply 305.
Br J Anaesth. 2002
Two episodes of life-threatening anaphylaxis in the same patient to a
chlorhexidine-sulphadiazine-coated central venous catheter.
Stephens R, Mythen M, Kallis P, Davies DW, Egner W, Rickards A.
UCL Hospitals, The Middlesex Hospital, Mortimer Street, London W1N 8AA, UK.
Chlorhexidine allergy has been described in the literature, mainly in Japanese
individuals. Most reactions have been limited to the skin, mild in severity and
a
result of chlorhexidine containing solutions such as 'Savlon' (Novartis Consumer
Health, Horesham, UK). We describe what we believe is the first reported case of
anaphylaxis in a European patient to a chlorhexidine- sulphadiazine-coated
central venous catheter.
Publication Types:
Case Reports
PMID: 11493510 [PubMed - indexed for MEDLINE]
64: Pediatrics. 2001 Jun;107(6):1431-6.
Comment in:
40
Evid Based Nurs. 2002 Jul;5(3):73.
A randomized trial comparing povidone-iodine to a chlorhexidine
gluconate-impregnated dressing for prevention of central venous catheter
infections in neonates.
Garland JS, Alex CP, Mueller CD, Otten D, Shivpuri C, Harris MC, Naples M,
Pellegrini J, Buck RK, McAuliffe TL, Goldmann DA, Maki DG.
St. Joseph's Hospital, Milwaukee, WI 53210, USA. jsgarland@hotmail.com
Neonates who require a central venous catheter (CVC) for prolonged vascular
access experience high rates of catheter-related bloodstream infection (CRBSI).
PURPOSE: A multicenter randomized clinical trial was undertaken to ascertain the
efficacy of a novel chlorhexidine-impregnated dressing (Biopatch Antimicrobial
Dressing) on the CVC sites of neonates for the prevention of catheter tip
colonization, CRBSI, and bloodstream infection (BSI) without a source. Setting.
Six level III neonatal intensive care units. Patients Studied. Neonates admitted
to study units who would require a CVC for at least 48 hours. METHODS: Eligible
infants were randomized before catheter placement to 1 of the 2 catheter site
antisepsis regimens: 1) 10% povidone-iodine (PI) skin scrub, or 2) a 70% alcohol
scrub followed by placement of a chlorhexidine-impregnated disk over the
catheter
insertion site. A transparent polyurethane dressing (Bioclusive Transparent
Dressing) was used to cover the insertion site in both study groups. Primary
study outcomes evaluated were catheter tip colonization, CRBSI, and BSI without
an identified source. RESULTS: Seven hundred five neonates were enrolled in the
trial, 335 randomized to receive the chlorhexidine dressing and 370 to skin
disinfection with PI (controls). Neonates randomized to the antimicrobial
dressing group were less likely to have colonized CVC tips than control neonates
(15.0% vs 24.0%, relative risk [RR]: 0.6 95% confidence interval [CI]: 0.5-0.9).
Rates of CRBSI (3.8% vs 3.2%, RR: 1.2, CI: 0.5-2.7) and BSI without a source
(15.2% vs 14.3%, RR: 1.1, CI: 0.8-1.5) did not differ between the 2 groups.
Localized contact dermatitis from the antimicrobial dressing, requiring
crossover
into the PI treatment group, occurred in 15 (15.3%) of 98 exposed neonates
weighing </=1000 g. No neonates in the PI group developed contact dermatitis.
CONCLUSION: The novel chlorhexidine-impregnated dressing, replaced weekly, was
as
effective as cutaneous disinfection with 10% PI and redressing the site every 3
to 7 days for preventing CRBSI and BSI without a source in critically ill
neonates requiring prolonged central venous access. The risk of local contact
dermatitis under the chlorhexidine dressing limits its use in low birth weight
infants who require prolonged central access during the first 2 weeks of life.
Publication Types:
Clinical Trial
Multicenter Study
Randomized Controlled Trial
Research Support, Non-U.S. Gov't
Research Support, U.S. Gov't, P.H.S.
PMID: 11389271 [PubMed - indexed for MEDLINE]
65: J Antimicrob Chemother. 2001 May;47(5):589-98.
Comment in:
Aten Primaria. 2000 Nov 30;26(9):649-50.
In vitro evaluation of the risk of developing bacterial resistance to
antiseptics
and antibiotics used in medical devices.
41
Tambe SM, Sampath L, Modak SM.
Department of Surgery, College of Physicians and Surgeons of Columbia
University,
630 West 168th Street, BB 1734, New York, NY 10032, USA.
The risk of development of resistance in Staphylococcus epidermidis to the
antibiotics and antiseptics impregnated in central venous catheters was
evaluated. The culture was passaged 10-20 times through subinhibitory
concentrations of different antimicrobials, singly and in combination, and the
MIC of each antimicrobial before and after passage was compared. There was a 10to 16-fold increase in the MIC of the combination of minocycline and rifampicin,
while no significant increase in the MIC of minocycline alone was seen. The MIC
of rifampicin was 25,000-fold higher against strains passaged through rifampicin
alone (as compared with that for the original strain), while the increase was
only 80-fold when it was combined with minocycline for passage. There was no
substantial change in susceptibility to the antiseptic chlorhexidine when used
alone or in combination with either silver sulphadiazine or triclosan (the MIC
of
triclosan alone increased eight-fold). In time-kill studies, synergy was
observed
between chlorhexidine and both triclosan and silver sulphadiazine. Zone of
inhibition tests of catheters impregnated with minocycline and rifampicin showed
that their activity against rifampicin-resistant strains was lower than that
against the susceptible strain. On the other hand, the activity of the
antiseptic
(chlorhexidine and silver sulphadiazine) catheters against the
rifampicin-resistant and -susceptible strains was similar. Although this study
indicates that antibiotic catheters may be at a higher risk of being colonized
by
antibiotic-resistant bacteria, the implications of these results in clinical
settings need to be determined.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 11328769 [PubMed - indexed for MEDLINE]
66: Emerg Infect Dis. 2001 Mar-Apr;7(2):197-9.
New technologies to prevent intravascular catheter-related bloodstream
infections.
Mermel LA.
Brown University School of Medicine and Rhode Island Hospital, Providence, Rhode
Island, USA. lmermel@lifespan.org
Most intravascular catheter-related infections are associated with central
venous
catheters. Technologic advances shown to reduce the risk for these infections
include a catheter hub containing an iodinated alcohol solution, short-term
chlorhexidine-silver sulfadiazine- impregnated catheters,
minocycline-rifampin-impregnated catheters, and chlorhexidine- impregnated
sponge
dressings. Nontechnologic strategies for reducing risk include maximal barrier
precautions during catheter insertion, specialized nursing teams, continuing
quality improvement programs, and tunneling of short-term internal jugular
catheters.
Publication Types:
Review
42
PMID: 11294705 [PubMed - indexed for MEDLINE]
67: Diagn Microbiol Infect Dis. 2000 Sep;38(1):1-5.
Evaluation of antiseptic-impregnated central venous catheters for prevention of
catheter-related infection in intensive care unit patients.
Sheng WH, Ko WJ, Wang JT, Chang SC, Hsueh PR, Luh KT.
Department of Internal Medicine, Surgery and Laboratory Medicine, National
Taiwan
University Hospital, Taipei, Taiwan.
Central venous catheterization represents a significant medical advancement,
particularly in the treatment of critical ill. However, there is a high risk of
central venous catheters-related infection. A novel antiseptic central venous
catheter, made of polyurethane and impregnated with chlorhexidine and silver
sulfadiazine, was developed to reduce the risk of catheters-related infection.
In
this study, we did a randomized clinical study to determine the efficacy by
using
antiseptic catheters for the prevention of central venous catheters-related
infection in the intensive care units. A total of 204 patients with 235 central
venous catheters were studied at the surgical intensive care units at National
Taiwan University Hospital between November 1998 and June 1999. Participants
received either a standard triple-lumen polyurethane catheter or an antiseptic
catheter (Arrow International, Reading, Pennsylvania, USA). Both were
indistinguishable from each other. Compared to standard polyurethane catheters,
antiseptic catheters were less likely to be colonized by microorganisms when
they
were cultured at the removal (8.0 versus 20.0 colonized catheters per 100
catheters; relative risk 0.34 [95% CI, 0.15 to 0.74]; p<0.01). There was no
significant differences between both groups in catheter-related infections (0.9
versus 4.9 infections per 100 catheters; relative risk 0.17 [95% CI, 0.03 to
1.15]; p = 0.07). Gram-positive cocci and fungi were more likely to colonize in
the standard polyurethane catheters (p = 0.06 and 0.04, compared to antiseptic
catheters respectively). Two of our cases in the control group died directly due
to catheter-related candidemia. No adverse reactions such as hypersensitivity or
leukopenia were found in the antiseptic catheter group. Our study showed that
central venous catheters with antiseptic coating were safe and had less risk of
colonization of bacteria and fungi than standard catheters in the critically ill
patients.
Publication Types:
Clinical Trial
Randomized Controlled Trial
PMID: 11025176 [PubMed - indexed for MEDLINE]
68: J Biomed Mater Res. 2000 Sep;53(5):600-4.
Prevention of pin track infection in external fixation with silver coated pins:
clinical and microbiological results.
Massè A, Bruno A, Bosetti M, Biasibetti A, Cannas M, Gallinaro P.
Dept. of Orthopaedics, Traumatology and Occupational Medicine, University of
Torino, Italy. alessandro.masse@CTO.UNITO.it
Pin tract infection is a frequent complication of external fixation; according
to
literature its frequency ranges from 2-30%. The recent introduction of silver
coating of polymeric materials was found to decrease bacterial adhesion; its
43
clinical use with Foley catheters and central venous catheters led to
significant
results. To verify the ability of the same silver coating to decrease the
bacterial colonization on external fixation screws, a prospective randomized
study was carried out on 24 male patients; a total of 106 screws were implanted
in the lower limb to fix femoral or tibial diaphyseal fractures: 50 were coated
with silver and 56 were commercially available stainless steel screws. Although
the coated screws resulted in a lower rate of positive cultures (30.0%) than the
uncoated screws (42.9%), this difference was not statistically significant (p =
0.243). The clinical behavior of the coated screws did not differ from that of
the uncoated ones. Furthermore, the implant of silver-coated screws resulted in
a
significant increase in the silver serum level. These results led us to consider
it ethically unacceptable to continue this investigation. Copyright 2000 John
Wiley & Sons, Inc.
Publication Types:
Clinical Trial
Controlled Clinical Trial
PMID: 10984710 [PubMed - indexed for MEDLINE]
69: Infect Control Hosp Epidemiol. 2000 Jun;21(6):375-80.
The clinical and economic consequences of nosocomial central venous
catheter-related infection: are antimicrobial catheters useful?
Saint S, Veenstra DL, Lipsky BA.
Department of Medicine, University of Michigan Medical School, Ann Arbor
Veterans' Affairs Health Services Research and Development Service, USA.
Central venous catheters (CVCs) are essential for many hospitalized patients,
but
they are associated with important infectious complications. Recent studies have
indicated that CVCs coated with antimicrobial agents reduce the incidence of
catheter-related bloodstream infection (CR BSI). To estimate the clinical and
economic consequences of short-term central venous catheter-related infection
and
the potential usefulness of antimicrobial-coated catheters, we reviewed and
synthesized the available relevant literature. Statistical pooling was used to
estimate the incidence of both catheter colonization and CR BSI. The
attributable
mortality of CR BSI was also evaluated. In addition, the economic consequences
of
both local and systemic catheter-related infection was estimated from literature
reports that used micro-costing and other techniques. Among patients in whom
standard, noncoated CVCs are in place for an average of 8 days, 24.7% are
expected to develop catheter colonization (95% confidence interval [CI(95)],
22.0%-27.5%). Approximately 5.2% (CI(95), 3.9%-6.5%) will develop CR BSI. The
attributable mortality of CR BSI remains unclear, but recent studies are
consistent with a range from 4% to 20%. An episode of local catheter-related
infection leads to an additional cost of approximately $400, whereas the
additional cost of CR BSI ranges from approximately $6,005 to $9,738. Formal
economic analyses indicate that CVCs coated with antibacterial agents (such as
chlorhexidine-silver sulfadiazine or minocycline-rifampin) likely reduce
infectious complications, yielding economic advantages. In light of the
substantial clinical and economic burden of catheter-related infection, hospital
personnel should adopt proven cost-effective methods to reduce this common and
important nosocomial complication.
Publication Types:
Research Support, Non-U.S. Gov't
44
Review
PMID: 10879567 [PubMed - indexed for MEDLINE]
70: Crit Care Med. 2000 May;28(5):1376-82.
The safety of prolonging the use of central venous catheters: a prospective
analysis of the effects of using antiseptic-bonded catheters with daily site
care.
Norwood S, Wilkins HE 3rd, Vallina VL, Fernandez LG, McLarty JW.
East Texas Medical Center, Tyler, USA.
OBJECTIVE: To determine rates of catheter colonization and catheter-related
bloodstream infection (CRBSI) when antiseptic-bonded central venous catheters
(CVCs) and standardized daily site care are used with no predetermined interval
for removal. DESIGN: Prospective observational study. SETTING: Two major trauma
centers. PATIENTS: All trauma patients admitted to two major trauma centers that
received a CVC from May 1996 through May 1998. INTERVENTIONS: None. MEASUREMENTS
AND MAIN RESULTS: Catheters were semiquantitatively cultured to identify
bacterial colonization and CRBSI. Monitored variables included total catheter
days, anatomical site of catheter insertion, and area in hospital of catheter
insertion. CVC tips and intracutaneous segments were semiquantitatively
cultured.
A total of 460 (92%) of 501 catheters placed in 324 trauma patients were
evaluable, representing 95.5% of all catheter days during the study period.
Rates
of catheter colonization and CRBSI were 5% (5/1000 catheter days) and 1.5%
(1.511000 catheter days), respectively. Subclavian catheters were in place
longer
than femoral or internal jugular catheters (p < .0001), but the colonization
rate
was significantly lower (p = .03; relative risk, 0.34; 95% confidence interval,
0.15-0.77). No differences in CRBSI rates among anatomical sites or between
catheters used < or =14 days and those used >14 days were identified.
CONCLUSION:
Femoral and internal jugular antiseptic-bonded CVCs develop bacterial
colonization earlier than subclavian CVCs. Subclavian antiseptic-bonded CVCs
combined with standardized daily site care may be safely used >14 days in trauma
patients.
Publication Types:
Comparative Study
PMID: 10834681 [PubMed - indexed for MEDLINE]
71: Crit Care Med. 2000 Feb;28(2):366-70.
Evaluation of an antiseptic triple-lumen catheter in an intensive care unit.
Hanley EM, Veeder A, Smith T, Drusano G, Currie E, Venezia RA.
Department of Epidemiology, Albany Medical Center Hospital, New York 12208, USA.
OBJECTIVE: To evaluate a decrease in catheter-related bloodstream infection rate
in patients with antiseptic triple-lumen catheters in an intensive care unit.
DATA SOURCES: Retrospective review of surveillance records, patient medical
records, laboratory and microbiological reports, and antibiotic administration
records. STUDY SELECTION: Patients admitted to the intensive care unit with
triple-lumen catheters. DATA EXTRACTION: A subset of one entry per patient was
extracted from 2 yrs of primary bloodstream infection surveillance data. Data
collection included risk factors, laboratory and microbiological data, and
45
insertion sites and dates of all intravascular catheters present during
triple-lumen catheterization. DATA SYNTHESIS: The catheter-related bloodstream
infection rate was 5.4 and 11.3 per 1000 catheter days in antiseptic and
nonantiseptic triple-lumen catheter groups, respectively (p = .06). By
multivariate analysis using a Cox Proportional Hazards Model, the antiseptic
triple-lumen catheters were associated with a significant reduction in
catheter-related bloodstream infection (p = .03). Model expansion to include
intrajugular site was significant by a likelihood ratio test [2(log likelihood
diff) = 4.26 P<.05 chi2(1)] CONCLUSIONS: The use of antiseptic triple-lumen
catheters may substantially reduce catheter-related bloodstream infections in an
intensive care population and may be subsequently associated with a decrease in
length of stay.
Publication Types:
Research Support, Non-U.S. Gov't
PMID: 10708168 [PubMed - indexed for MEDLINE]
72: Ann Intern Med. 2000 Mar 7;132(5):391-402.
Erratum in:
Ann Intern Med 2000 Sep 5;133(5):5.
Comment in:
ACP J Club. 2000 Nov-Dec;133(3):96.
Prevention of intravascular catheter-related infections.
Mermel LA.
Division of Infectious Diseases, Rhode Island Hospital and Brown University
School of Medicine, Providence 02903, USA. lmermel@lifespan.org
PURPOSE: To review the literature on prevention of intravascular catheterrelated
infections. DATA SOURCES: The MEDLINE database, conference proceedings, and
bibliographies of review articles and book chapters were searched for relevant
articles. Primary authors were contacted directly if data were incomplete. STUDY
SELECTION: Studies met the following criteria unless otherwise stated: Trials
were prospective and randomized; catheters were inserted into new sites, not
into
old sites over guidewires; catheter cultures were done by using semiquantitative
or quantitative methods; and, for prospective studies, catheter-related
bloodstream infection was confirmed by microbial growth from percutaneously
drawn
blood cultures that matched catheter cultures. DATA EXTRACTION: Data on
population, methods, preventive strategy, and outcome (measured as
catheter-related bloodstream infections) were gathered. The quality of the data
was graded by using preestablished criteria. DATA SYNTHESIS: The recommended
preventive strategies with the strongest supportive evidence are full barrier
precautions during central venous catheter insertion; subcutaneous tunneling
short-term catheters inserted in the internal jugular or femoral veins when
catheters are not used for drawing blood; contamination shields for pulmonary
artery catheters; povidone-iodine ointment applied to insertion sites of
hemodialysis catheters; specialized nursing teams caring for patients with
short-term peripheral venous catheters, especially at institutions with a high
incidence of catheter-related infection; no routine replacement of central
venous
catheters; antiseptic chamberfilled hub or hub-protective antiseptic sponge for
central venous catheters; and use of chlorhexidine-silver
sulfadiazine-impregnated or minocycline-rifampin-impregnated short-term central
venous catheters if the rate of infection is high despite adherence to other
46
strategies that do not incorporate antimicrobial agents (for example, maximal
barrier precautions). CONCLUSIONS: Simple interventions can reduce the risk for
serious catheter-related infection. Adequately powered randomized trials are
needed.
Publication Types:
Meta-Analysis
PMID: 10691590 [PubMed - indexed for MEDLINE]
73: J Hosp Infect. 2000 Feb;44(2):141-5.
Measurement of ultrasonic-induced chlorhexidine liberation: correlation of the
activity of chlorhexidine-silver-sulfadiazine-impregnated catheters to agar roll
technique and broth culture.
Schierholz JM, Bach A, Fleck C, Beuth J, König D, Pulverer G.
Institute of Medical Microbiology and Hygiene, University of Cologne,
Goldenfelsstr. 19-21, 50935 Cologne, Germany.
The diagnosis of intravascular catheter-related infections continues to be a
challenge to both the clinician and the microbiologist. To assess the antiseptic
effects of silver-sulfadiazine-chlorhexidine-impregnated central venous
catheters
(SSC) on catheter culture systems, segments of fresh antiseptic- and non
antiseptic-impregnated catheters as well as extracted catheters following five
days of immersion in PBS were sonicated. The chlorhexidine liberated from the
catheter material by ultrasonication was measured by HPLC. Fresh
antiseptic-impregnated catheter segments rolled on seeded agar plates produced
inhibition zones unlike catheters which had been extracted for >five days in
phosphate buffered saline (PBS). Scanning electron microscopy (SEM) revealed
that
chlorhexidine-silversulfadiazine crystals were located in the superficial
catheter matrix. Direct contact of superficially located drug particles with
seeded agar plates probably caused the inhibition of bacterial growth. The study
suggests that antiseptic compounds readily elute from fresh catheters during
solid medium-based culturing processes and ultrasonication. The addition of
inhibitors of silversulfadiazine-chlorhexidine to media may be prudent
especially
when culturing antimicrobial loaded catheters removed after short inwelling
times. Copyright 2000 The Hospital Infection Society.
Publication Types:
In Vitro
PMID: 10662565 [PubMed - indexed for MEDLINE]
47