Repro19-MaleHistoII
advertisement
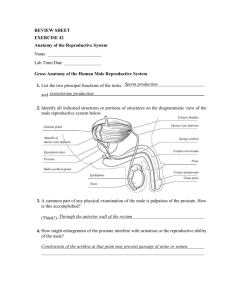
Repro #19 Tues, 4/01/2003, 11am Dr. Cammarata Saira Momin Page 1 of 6 Checked by Dr. Cammarata Male Reproductive Histology II Hormonal control of male reproductive function --The structure and endocrine function of the interstitial cells are controlled by LH (also from gonadotroph). --Testosterone (in adenohypophysis and hypothalamus) is required to maintain spermatogenesis. It therefore, exerts a positive control on Sertoli (and germ) cells. Excessive testosterone acts as a feedback inhibitor to regulate LH production and secretion by acting on the pituitary gland and hypothalamus. --The primary target cell for FSH is the Sertoli cell, stimulating protein synthesis (FSH is from gonadotroph in anterior pituitary; also makes LH) --Sertoli cells respond to FSH by secreting androgen binding protein (to bind testosterone in system, keeping it active) --Inhibin is a feedback inhibitor (to gonadotroph) which regulates FSH secretion from the pituitary gland. -GnRH is secreted from the hypothalamus and activates the Gonadotrophs in the pituitary -believed sertoli feedback on Leydig cells, unclear as to why I. Male Genital Ducts Route of sperm from the lumen of S.T.(not on its own motility; must mature at the epididymis) to mediastina to efferent ductules to vas deferens (penetrate prostate) and empties through urethra (prostate gland encircles urethra) A. Tubuli Recti (i.e. straight tubule) 1. At the apex of each lobule, the component seminiferous tubules join to form a straight tubule 2. Each short tubule is straight, short and devoid of convolutions 3. At the junction of the seminiferous tubule the spermatogenic cells disappear and only Sertoli cells remain a. these form a simple columnar epithelium to cuboidal b. epithelial cells rests on a basal lamina surrounded by loose connective tissue, devoid of smooth muscle cells (late spermatid to lumen of S.T. at rete testis) B. Rete Testis 1. The straight tubules course to the dense connective tissue of the Repro #19 Tues, 4/01/2003, 11am Page 2 of 6 mediastinum where they enter a network of anastomosing channels the rete testis 2. Appear as irregular spaces lined by simple cuboidal epithelium to Low columnar 3. Passage of spermatozoa through the tubuli recti and the rete testis is rapid, since in sections spermatozoa are only rarely seen C. Ductuli Efferentes (efferent ductules) - leave testis in tunica albuginea (look for hill, bump, scallops) 1. In the superior portion of the posterior border of the testis some 10-15 spirally wound ductules arise from the rete testis and emerge on the surface of the testis 2. Ductules are bound by connective tissue and each is surrounded by a thin layer of circularly arranged smooth muscle fibers a. each ductule is 6-8 cm long and 0.05 mm in diameter 3. Lined mostly by a simple columnar epithelium which rests on thin basal lamina a. lumen of the ductule is irregular in outline owing to the varying height of the epithelial cell b. groups of tall columnar cells alternate with groups of much shorter cells c. many of the taller columnar cells have motile cilia which beat helping to transport spermatozoa to the epididymis d. non-ciliated shorter cells appear to be absorptive resorbs fluid at S.T. and therefore pulls sperm with it from S.T. to efferent ductules D. Ductus Epididymides (look for defined boundary around the circular lumen) -10-12 efferent ductules merge into the epididymis - head, midsection, tail 1. This duct is surrounded by connective tissue and is highly tortuous 2. Lined with a pseudostratified epithelium (ciliated columnar cells) (has stereocilia which is made up of microtubules for resorption, therefore not true cilia which is for motility) a. tall columnar cells or principal cells (i) in the caput they are very tall but gradually become lower in successive segments and may be cuboidal in the cauda (ii) surface of these cells contains a tuft of very long, non-motile, stereocilia b. basal Cells: small round or pyramidal elements lodged between the bases of the columnar cells (i) Function is obscure 3. Smooth muscle surrounding the epididymis increases gradually from caput to the cauda Repro #19 Tues, 4/01/2003, 11am Page 3 of 6 a. distal part of the cauda has three-layered muscle coat (epididymis has more smooth muscle surrounding it than efferent ductules) 4. Functions of epididymis a. resorption of fluids; over 90% of the fluid leaving the testis is reabsorbed in the efferent ductules and epididymis b. site of maturation of sperm (late spermatid becomes mature sperm; sperm cells achieve motility in epididymis) c. site of storage of sperm (especially cauda) d. site of phagocytosis of defective sperm (epididymis cells recognize destroy defective sperm to decrease birth defects) e. secretion E. Ductus Deferens (looks like the ureter but ureter has transitional epith.) 1. The epididymis straightens out at its termination and becomes continuous with the ductus deferens which continues to the prostate urethra 2. Ascends from the scrotum through the "spermatic cord" toward the urethra a. prior to its termination the duct dilates and enlarges into the ampulla 3. Epithelium is pseudostratified columnar and many of the tall cells bear stereocilia a. delicate basal lamina; thin lamina propria with elastic fibers b. mucosa rises into longitudinal folds; stellate pattern 4. Muscle coat is thick and is composed of three distinct layers of smooth muscle a. inner - thin, longitudinally arranged b. middle - large, circularly arranged c. outer - large, longitudinally arranged d. fibrous adventitia surrounds the muscle coat -Ampulla >lumen of the duct is wider and the mucosa is much more folded >the ampulla receives the duct of the seminal vesicle and then forms the short ejaculatory duct (pierces the prostate) which, in turn, empties into prostatic portion of urethra F. Spermatic Cord 1. Enclosed by cremaster muscle 2. Cord contains a. ductus deferens b. spermatic artery c. pampiniform plexus d. nerves Repro #19 Tues, 4/01/2003, 11am Page 4 of 6 3. Countercurrent exchange may cool blood going to testes (vas deferens has pampiniform plexus and arteries which is important b/c blood to the testis must be cooler than rest of the body) II. Auxiliary Genital Glands A. Seminal Vesicles (paired, pierce prostate also; no thick connective tissure like rete testis and rete testis has simple cuboidal) 1.Each vesicle is a tortuous, elongated diverticulum off the ductus deferens a. consists of a (1) external connective tissue adventitia, (2) smooth muscle coat, and (3) highly folded mucosa b. secondary and tertiary folding patterns (helps carry sperm) 2.Epithelium is variable showing pseudostratified columnar to regular columnar but may be simple columnar a. epithelium depends upon hormonal support (i.e. testosterone) 3.It is an exocrine gland whose secretion is a major component of semen a. contains prostaglandins, fructose, lipid, and flavins b. fructose is energy source for spermatozoa c. flavins - yellow pigments that fluoresce B. Prostate provides food to ejaculatory duct to keep semen liquified (look for calcified glycoproteins which inc. with age) 1. Surrounds the urethra at its origin from the bladder 2. It is an aggregate of 30-50 small compound tubuloalveolar glands that drain into the prostatic urethra a. drained by 15-30 small excretory ducts 3. Small glands (periurethral) lie in the mucosa and these are surrounded by submucosal glands 4. Main or principal glands line peripherally and constitute the bulk of the gland a. main glands are embedded in an abundant, dense stroma which is continuous with a fibroelastic capsule 5. Secretory alveoli and tubules are very irregular and vary greatly in size and form a. branch frequently and both alveoli and tubules have wide lumina b. no distinct basal lamina and epithelium is simple columnar or pseudostratified c. Cytoplasm contains numerous secretory granules and lipid droplets 6. Secretion is a thin, colorless fluid which is slightly acid (pH 6.5) Repro #19 Tues, 4/01/2003, 11am Page 5 of 6 a. can contain corpora amylacea; i.e., condensations of the secretion which may become calcified b. proteolytic enzymes c. zinc, citric acid and acid phosphatase occur in high concentrations 7. Benign nodular hyperplasia - hypertrophy of both stroma and glandular components (occurs in the central zone of the prostate-more immediately wrapped around urethra; difficulty urinating; correct with surgery) 8. Carcinoma of the prostate (2nd /3rd highest cause of male death) a. AcPase levels in blood increase occurs in the peripheral zone; PSA (Prostate Specific Antigen) inc. with circulating antibodies; metastatic plasia; should feel smooth bumps/nodules; if hard, means potential problem arising b. “d” class carcinoma; if at this phase, less than 5 years to live; metastatic cells have broken through thick fibroelastic capsule c. used to treat with orchidectomy and lots of E2 (prostate requires lots of testosterone) C.Bulbourethral Glands or Cowper's Glands (inf. To prostate) 1. Paired bodies, lying in connective tissue behind the membranous urethra 2. Each is a compound tubuloalveolar gland whose duct enters the posterior portion of the membranous urethra 3. Epithelium is usually simple columnar a. secretion is clear, viscid, and mucoid b. probably secretion serves to lubricate urethra III.Penis A.Introduction 1.The penis is formed of three cylindrical bodies of cavernous or erectile tissue a. paired corpora cavernosa penis and the b. unpaired corpus cavernosum urethrae (corpus spongiosum) (both surrounded by tunica albuginea of the testis) B.Erectile Tissue 1.The erectile tissue of the corpora cavernosa is a vast spongelike system of irregular vascular spaces lined by endothelium and fed by efferent arteries and drained by efferent veins a..in the flaccid condition the cavernous spaces contain very little blood and appear as irregular clefts b. in erection they become engorged with blood and become large cavities Repro #19 Tues, 4/01/2003, 11am Page 6 of 6 2.Trabeculae separate vascular spaces a. trabeculae contain connective tissue and smooth muscle b. helicine arteries run into the cavernous spaces (blood goes here and drains directly into venous spaces, fills with blood as long as there is an arousal; when arousal is lost, anastomosis is not maintained) 3.Each of the cavernous bodies is surrounded by a thick (1mm) resistant fibrous capsule, the tunica albuginea a. consists of collagenous and elastic fibrous network 4.The skin covering the penis is thin and is provided with an abundant subcutaneous layer containing smooth muscles 5.Mechanism of erection: deep artery diverted to helicine arteries C.Male Urethra - has 3 divisions 1. Prostatic urethra a. surrounded by prostate b. lined by transitional epithelium c. receives ejaculatory ducts 2. Membranous urethra a. short, extends from prostate to bulb of corpus spongiosum b. lined by stratified or pseudostratified columnar epithelium 3. Penile urethra a. Passes through corpus spongiosum b. glands of Littre are present c. lined by stratified or pseudostratified columnar except at fossa navicularis where epithelium is stratified squamous Know: Function and visual sertoli Germ cell line and development Structure and conduction of sperm from S.T. to penis Bulbourethral gland not on the practical Know difference btwn. Rete testis and seminal vesicle of written and practical