Bronchiolitis - Navy Emergency Medicine
advertisement

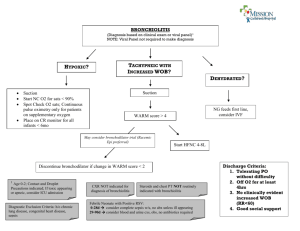
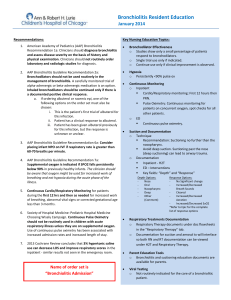
ED Management of Bronchiolitis Bronchiolitis1 ABCs, Monitors, Oxygen2 Yes Respiratory Failure?3 IV/IO, Sepsis W/U,3 Abx,4 RSI, ABG, CXR, RSV EIA,5 PICU No Respiratory Distress?6 No Yes Yes Improved after Albuterol neb?7 Yes Albuterol nebs PRN Meet D/C criteria?8 No D/C home,9 F/U 24 hrs Ancillary studies,10 Admit11 No Yes Improved after racemic epi neb?12 Racemic epi nebs PRN No Ancillary studies,10 Admit11 Notes: 1 Bronchiolitis = virally induced cause of acute bronchiolar inflammation associated with airway obstruction & clinical findings of fever, rhinitis, tachypnea, expiratory wheezing, cough, rales, use of accessory muscles, apnea, dyspnea, nasal flaring, and retractions. 2 Give 100% oxygen via non-rebreather mask for SaO2 consistently < 91% (RA). Wean for SaO2 consistently > 94%. 3 Respiratory failure=apnea; Risk factors for severe disease: age < 6 wks; 1 Guideline for ED Management of Bronchiolitis 3 4 5 6 7 8 9 10 prematurity (< 36 wks GA); complicated congenital heart disease (esp. pulmonary HTN); chronic lung disease of prematurity; cystic fibrosis; American Indian/ Alaskan Native; immunosuppression; multiple congenital anomalies; CP; metabolic disease Sepsis W/U includes: CBC/diff; bld cx; cath UA/urine cx; LP (CSF gm stain/cx/protein/ glucose/cell count/consider HSV or enteroviral PCR); CXR (AP/Lat) for respiratory signs/sx (tachypnea, retractions, focal auscultatory findings, SaO2 < 97% (RA); stool cx for stool blood/PMNs; consider rapid viral studies (Influenza A & B) IV Abx (suggested empiric therapy): a. Suspected sepsis/fever without source: (1) Age < 28 days: Ampicillin 50 mg/kg/dose IV Q12H (< 1 wk) or 50 mg/kg/dose IV Q6H (> 1 wk) + Cefotaxime 50 mg/kg/dose IV Q12H (< 1 wk) or 50 mg/kg/dose IV Q8H (> 1 wk) OR + Gentamycin 2.5 mg/kg/dose IV Q12H (< 1 wk) or 2.5 mg/kg/dose IV Q8H (> 1 wk); consider antiviral treatment if suspect HSV. (2) Age 29-60 days: Ampicillin 50 mg/kg/dose IV Q6H + Cefotaxime 60 mg/ kg/dose IV Q8H (3) Age > 60 days: Ceftriaxone 50 mg/dose IV/IM b. Signs of bacterial meningitis: (1) Age < 28 days: see suggested abx for FWOS (3) Age 29-60 days: Vancomycin 15 mg/kg/dose + cephalosporin (either Cefotaxime 50 mg/kg/dose or Ceftriaxone 100 mg/kg/dose) (note: add Ampicillin 50-100 mg/kg/dose if suspect Listeria) (3) Age > 60 days: Vancomycin 15 mg/kg/dose + cephalosporin (either Cefotaxime 50 mg/kg/dose or Ceftriaxone 100 mg/kg/dose RSV EIA= rapid test for respiratory syncytial virus, which is responsible for 70% of cases of bronchiolitis (80-100% in winter months). Respiratory distress= RR > 70; retractions; SaO2 < 94% (RA); altered mental status; grunting Consider trial of nebulized 0.5% albuterol (0.15 mg/kg in 3 mL NSS) for most patients. Avoid further albuterol if patient shows no improvement. Repeat PRN if albuterol-responsive. Discharge criteria: nontoxic; RR < 70; SaO2 > 94% (RA); adequate PO; caretaker able to clear airway with suctioning Home management: albuterol via aerochamber/mask if albuterol responsive; saline nose drops/bulb suction before feedings and PRN upper respiratory congestion; small frequent feedings; good follow-up Ancillary studies: a. RSV EIA: avoid in uncomplicated cases; obtain by 2 mL nasal wash ONLY in patients with need of admission (cohorting), severe disease, presentation early/late in season, age < 2 mos with respiratory sx + fever, immunization with Synagis (Palivizamab), or immunocompromise b. CBC/blood cx/urine cx: obtain in pts with severe disease or age < 2 mos with fever c. CXR: avoid in uncomplicated cases; obtain in patients with severe disease, 2 Guideline for ED Management of Bronchiolitis underlying cardiac and/or pulmonary disease, or unclear diagnosis d. ABG: obtain in patients with severe disease 11 Admit for: apnea/respiratory failure; severe respiratory distress; dehydration; bacterial superinfection; pneumothorax/pneumomediastinum 12 Nebulized 2.25% racemic epinephrine (.05 mL/kg up to 0.5 mL in 3 mL NSS) may be more effective than albuterol. References: Schuh S, Canny G, Reisman JJ, et al. Nebulized albuterol in acute bronchiolitis. J Pediatr 1990;117:633-7 Bisgaard H, Munck SL, Nielsen JP, et al. Inhaled budesonide for treatment of recurrent wheezing in early childhood. Lancet 1990;336:649-51 Springer C, Bar-Yishay E, Uwayyed K, et al. Corticosteroids do not affect the clinical or physiological status of infants with bronchiolitis. Pediatr Pulmonol 1990; 9:181-5 Shaw KN, Bell LM, Sherman NH. Outpatient assessment of infants with bronchiolitis. Am J Dis Child 1991;145:151-5 [Predictors of severe disease: ill or toxic appearance; RR > 70; SaO2 < 95% (single best predictor); atelectasis on CXR; GA < 34 wks; & age < 3 mos.] Klassen TP, Rowe PC, Sutcliffe T, et al. Randomized trial of salbutamol in acute bronchiolitis. J Pediatr 1991;118:807-11 Noble V, Ruggins NR, Everard ML, et al. Inhaled budesonide for chronic wheezing under 18 months of age. Arch Dis Child 1992;67:285-8 Kristjansson S, Lodrup Carlsen KC, Wennergren G, et al. Nebulized racemic adrenaline in the treatment of acute bronchiolitis in infants and toddlers. Arch Dis Child 1993;69:650-4 Sanchez I, De Koster J, Powell RE et al: Effect of racemic epinephrine and salbutamol on clinical score and pulmonary mechanics in infants with bronchiolitis. J Pediatr 1993;122:145-51 (or 123:491-2) [Racemic epinephrine 0.1 mg/kg was superior to a nebulized beta2-agonist in improving clinical score in patients with bronchiolitis.] Tepper RS, Rosenberg D, Eigen H, et al. Bronchodilator responsiveness in infants with bronchiolitis. Pediatr Pulmonol 1994;17:81-5 Gadomski AM, Lichenstein R, Horton L, et al. Efficacy of albuterol in the management of bronchiolitis. Pediatrics 1994;93:907-912 3 Guideline for ED Management of Bronchiolitis [Bronchodilators may improve the clinical appearance of a child through a general stimulatory effect rather than by improving respiratory function.] Menon K, Sutcliffe T, Klassen TP: A randomized trial comparing the efficacy of epinephrine with salbutamol in the treatment of acute bronchiolitis. J Pediatr 1995;126:1004-7 [3 mL of nebulized L-epinephrine (1:1000) is more effective than a nebulized beta2agonist in improving SaO2 and reducing hospitalization.] Martinez FD, Wright AL, Taussig LM, et al. Asthma and wheezing in the first six years of life. N Engl J Med 1995;332:133-8 [The majority of infants with wheezing have transient conditions associated with diminished airway function at birth and do not have increased risks of asthma or allergies later in life. In a substantial minority of infants, however, wheezing episodes are probably related to a predisposition to asthma.] Reijonen T, Korppi M, Pitkakangas S, et al. The clinical efficacy of nebulized racemic epinephrine and albuterol in acute bronchiolitis. Arch Pediatr Adolesc Med 1995;149:686-92 Hammer J, Numa A, Newth CJL: Albuterol responsiveness in infants with respiratory failure caused by respiratory syncytial virus infection. J Pediatr 1995;127:485-90 [There is a subset of patients with acute bronchiolitis who benefit from inhaled albuterol; it should be discontinued if a beneficial response cannot be observed.] Stick SM, Burton PR, Clough JB, et al. The effects of inhaled beclomethasone diproprionate on lung function and histamine responsiveness in recurrently wheezy infants. Arch Dis Child 1995;73:327-32 Davies HD, Matlow A, Petric M, et al. Prospective comparative study of viral, bacterial and atypical organisms identified in pneumonia and bronchiolitis in hospitalized Canadian infants. Pediatr Infect Dis 1996;15:371-5 American Academy of Pediatrics Committee on Infectious Diseases. Reassessment of indications for ribavirin therapy in respiratory syncytial virus infection. Pediatrics 1996;97:137-40 Randolph AG, Wang EE. Ribavirin for respiratory syncytial virus lower respiratory tract infection. A systematic overview. Arch Pediatr Adolesc Med 1996;150:942-7 Roosevelt G, Sheehan K, Grupp-Phelan J et al: Dexamethasone in bronchiolitis: a randomized controlled trial. Lancet 1996;348:292-5 [IM dexamethasone did not reduce symptoms of bronchiolitis better than placebo.] 4 Guideline for ED Management of Bronchiolitis Kellner JD, Ohlsson A, Gadomski AM, et al. Efficacy of bronchodilator therapy in bronchiolitis. A meta-analysis. Arch Pediatr Adolesc Med 1996;150:1166-72 Reijonen T, Korppi M, Kuikka L, et al. Anti-inflammatory therapy reduces wheezing after bronchiolitis. Arch Pediatr Adolesc Med 1996;150:512-7 De Boeck K, Van der Aa N, Van Lierde S et al: Respiratory syncytial virus bronchiolitis: a double-blind dexamethasone efficacy study. J Pediatr 1997;131: 919-21 [There is no benefit from IV dexamethasone in acute RSV bronchiolitis.] Flores G, Horwitz RI: Efficacy of beta sub 2-agonists in bronchiolitis: A reappraisal and meta-analysis. Pediatrics 1997;100:233-9 [A review of 8 clinical trials, 5 RCTs & 251 children, in outpatients showed no evidence that bronchodilators significantly improve SaO2 or, compared to placebo, reduce admission rates.] Klassen TP, Sutcliffe T, Watters LK et al: Dexamethasone in salbutamol-treated inpatients with acute bronchiolitis: a randomized, controlled trial. J Pediatr 1997;130:191-6 [PO dexamethasone does not affect the course of bronchiolitis in hospitalized patients treated with a nebulized beta2-agonist.] Kuppermann N, Bank DE, Walton EA et al: Risks for bacteremia and urinary tract infections in young febrile children with bronchiolitis. Arch Pediatr Adolesc Med 1997;151:1207-14 [Previously healthy febrile children with bronchiolitis are unlikely to have bacteremia or UTI; routine cultures of blood and urine in these patients are unnecessary.] Antonow JA, Hansen K, McKinstry CA, et al. Sepsis evaluations in hospitalized infants with bronchiolitis. Pediatr Infect Dis J 1998;17:231-6 Adcock PM, Sanders CL, Marshall GS: Standardizing the care of bronchiolitis. Arch Pediatr Adolesc Med 1998;152:739-44 [General practice guidelines for patients admitted with bronchiolitis.] Andrade MA, Hoberman A, Glustein J, Paradise JL, Wald ER: Acute otitis media in children with bronchiolitis. Pediatrics 1998;101:617-9 [62% of 42 patients with bronchiolitis were also diagnosed with bacterial AOM by middle ear aspirate.] Dobson JV, Stephens-Groff SM, McMahon SR et al: The use of albuterol in hospitalized infants with bronchiolitis. Pediatrics 1998;101:361-8 [Nebulized albuterol does not improve SaO2 or decrease hospital LOS in bronchiolitis.] Hollman G, Shen G, Zeng L, Yngsdal-Krenz R, Perloff W, Zimmerman J, Strauss 5 Guideline for ED Management of Bronchiolitis R: Helium-oxygen improves clinical asthma scores in children with acute bronchiolitis. Crit Care Med 1998;26:1731-6 [Heliox improves respiratory status in non-intubated patients with RSV bronchiolitis.] Richter H, Seddon P: Early nebulized budesonide in the treatment of bronchiolitis and prevention of postbronchiolitic wheezing. J Pediatr 1998;132:849-53 [A 6 week course of nebulized steroid did not reduce symptoms of acute bronchiolitis or prevent post-bronchiolitic wheezing.] Berger I, Argaman Z, Schwartz SB, et al. Efficacy of corticosteroids in acute bronchiolitis: Short-term and long-term follow-up. Pediatr Pulmonol 1998;26:162-6 Kneyber MCJ, Brandenburg AH, deGroot R, et al. Risk factors for respiratory syncytial virus associated apnoea. Eur J Pediatr 1998;157:331-5 Greenes DS, Harper MB. Low risk of bacteremia in febrile children with recognizable viral syndromes. Pediatr Infect Dis J 1999;18:258-61 Antovow JA, Byington CL. Use of respiratory syncytial virus testing could safely eliminate many sepsis evaluations. Arch Pediatr Adolesc Med 1999;153:1310 Meissner HC, Welliver RC, Chartrand SA, et al. Pediatr Infect Dis J 1999;18:223231 [Factors which increase risk of acquiring RSV infection: maternal education < grade 12; daycare; school age siblings; lack of breast-feeding; > 2 individuals sharing a bedroom; multiple births; passive smoke exposure; birth within 6 mos before onset of RSV season.] Fox GF, Everard ML, Marsh MJ, et al. Randomized controlled trial of budesonide for the prevention of post-bronchiolitic wheezing. Arch Dis Child 1999;80:343-7 Karron RA et al. J Infect Dis 1999;180:41-49 [Risk factors for severe disease: age < 6 wks; prematurity (< 36 wks GA); complicated congenital heart disease (especially pulmonary HTN); chronic lung disease of prematurity; cystic fibrosis; American Indian/Alaska Native; underlying immunosuppression; & multiple congenital anomalies/CP/metabolic disease.] Bulow SM, Nir M, Levin E. Prednisolone treatment for respiratory syncytial virus infection: a randomized controlled trial of 147 infants. Pediatrics 1999;104:77 Barr FE, Patel NR, Newth CJL. The pharmacologic mechanism by which inhaled epinephrine reduces airway obstruction in respiratory syncytial virus-associated bronchiolitis. J Pediatr 2000;136:699-700 Cade A, Brownlee KG, Conway, SP. Randomised placebo-controlled trial of nebulised corticosteroids in acute respiratory syncytial viral bronchiolitis. Arch Dis Child 2000;82:126-130 6 Guideline for ED Management of Bronchiolitis Kajosaari M, Syvanen P, Forars M, et al. Inhaled corticosteroids during and after respiratory syncytial virus-bronchiolitis may decrease subsequent asthma. Pediatr Allergy Immunol 2000;11:198-202 Van Woensel JB, Kimpen JL, Sprikkelman AB, et al. Long-term effects of prednisolone in the acute phase of bronchiolitis caused by respiratory syncytial virus. Pediatr Pulmonol 2000;30:92-6 Goebel J, Estrada B, Quinonez J, et al. Prednisolone plus albuterol versus albuterol alone in mild to moderate bronchiolitis. Clin Pediatr 2000;39:213-20 Garrison M, Christakis D, Harvey E, et al. Systemic corticosteroids in infant bronchiolitis: A meta-analysis. Pediatrics 2000;105:e44 [A systemic review of 6 RCTs, 347 children, of the effect of systemic corticosteroids on the course of bronchiolitis suggest a statistically significant improvement in clinical symptoms, LOS, and duration of symptoms. However the evidence is difficult to interpret because some of the RCTs did not exclude children with a history of wheezing who may have asthma, a condition likely to respond to corticosteroids. The clinical relevance of the changes in SaO2 in the RCTs are unclear, and the clinical significance of the effect size is unclear. Furthermore, 8 RCTs with more than twice the number of people, all of which except 1 did not find a benefit of corticosteroids, were not included in the meta-analysis. The 1 RCT which found a benefit only observed a transient improvement in clinical score at one timepoint.] Lodrup Carlsen KC, Carlsen KH. Inhaled nebulized adrenaline improves lung function in infants with acute bronchiolitis. Resp Med 2000;94:709-14 Bertrand P, Aranibar H, Castro E, et al. Efficacy of nebulized epinephrine versus salbutamol in hospitalized infants with bronchiolitis. Pediatr Pulmonol 2001;31: 284-8 Schuh S, Coates AL, Binnie R, et al. Efficacy of oral dexamethasone in outpatients with acute bronchiolitis. J Pediatr 2002;140:27-32 [In a RCT of infants in the ED with first-time wheezing, Respiratory Disease Assessment Instrument > 6, and treated with dexamethasone 1 mg/kg or placebo, fewer infants in the dexamethasone group had a poor Respiratory Assessment Change Score and hospitalization compared to placebo. However the evidence is difficult to interpret because the RCT did not exclude children with a history or family hx of atopy; hence some of the first-time wheezers may have had asthma, a condition likely to respond to corticosteroids.] Wainwright C, Altamirano L, Cheney M, et al. A multicenter, randomized, doubleblind, controlled trial of nebulized epinephrine in infants with acute bronchiolitis. N Engl J Med 2003;349:27-35 [In a RCT comparing nebulized single-isomer epinephrine with placebo in 194 infants 7 Guideline for ED Management of Bronchiolitis admitted to 4 hospitals in Australia with a clinical diagnosis of bronchiolitis, use of nebulized epinephrine did not significantly reduce hospital LOS or time until ready for discharge. Among infants requiring supplemental O2 and IV fluids, the time until ready for discharge was significantly longer in the epinephrine group than the placebo group (P=.02). The need for supplemental O2 at admission had the greatest influence on severity of illness score and strongly predicted hospital LOS and time until ready for discharge.] Hartling L, Wiebe N, Russell K, et al. A meta-analysis of randomized controlled trials evaluating the efficacy of epinephrine for the treatment of acute viral bronchiolitis. Arch Pediatr Adolesc Med 2003;157:957-964 [Among outpatients, results favored epinephrine compared with placebo for clinical score at 60 min, SaO2 at 30 min, RR at 30 min, and compared with albuterol sulfate (salbutamol) for SaO2 at 60 min, HR at 90 min, RR at 60 min, and improvement. Among inpatients, results favored epinephrine compared with placebo for clinical score at 60 min, and compared with salbutamol for RR at 30 min. Epinephrine may be favorable compared with placebo and albuterol for short-term use among outpatients; however there is insufficient evidence to support the use of epinephrine among inpatients.] 8 Guideline for ED Management of Bronchiolitis