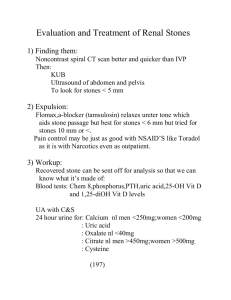
of kidney stones
advertisement

NEPHROLITHIASIS Pablo Quintero Pinzon August, 2005 Introduction: Nephrolithiasis is a common disorder that causes significant cost to society. It is estimated that between 5-15% of people will at some time in their life develop a kidney stone. The yearly cost of kidney stones, attributed to surgical extraction, fragmentation, and loss of productivity tops $2 billion per year! Nephrolithiaisis is more common in men than women and less common in people of African and Asian descent. The decision of when to evaluate of patients is stylistic, with some physicians deferring metabolic w/u until the second episode of nephrolithiasis. Clinical Presentation: Classically, kidney stones present with “renal colic.” The onset of the pain is usually acute and is described as loin to groin, retracing the path of the stone down the urinary tract to the bladder. The pain starts in the flank and curves anteriorly, radiating to the groin. Nausea and vomiting are associated with this pain. As the stone approached the ureterovesical junction (interface between the ureter and the bladder), urinary frequency and dysuria become more prominent. Once the stone has passed to the bladder, the described symptoms resolve and are followed by localized pain with passage through the urethra. Though usually not clinically significant in regards to blood loss, patients are often very distressed by the associated hematuria that accompanies the traumatic passage of kidney stones through the urinary tract. Obstruction by a stone can also predispose to urinary tract infections and pyelonephritis. Diagnosis: Radiology is often used to identify the presence of a stone in the correct clinical setting. Calcium stones and calcium complexed struvite stones are radiodense. Urate and cystine stones are not. Intravenous pyelogram had been the dx procedure of choice. However, concerns over the renal side-effects of IV contrast have prompted the use of non-contrast-enhanced helical CT scan as the gold standard. CT can detect both the stone (radiodense or radiolucent) and the urinary tract obstruction. Ultrasound is the test of choice for patients who should avoid radiation i.e pregnant women. It is very sensitive for the dx of urinary tract obstruction but it may miss small stones and ureteral stones. Retrograde pyelography is also an option that spares IV contrast, but the procedure is invasive and is usually done in the context of a cystoscopy. Acute Management of Acute Nephrolithiasis: The mainstay of acute management does not focus on the etiology of the kidney stone, but rather promotion of passage and analgesia. NSAIDS such as IV/IM ketorolac as well as opiods are acutely utilized to reduce the intense pain associated with the passage of stones. Hydration and swift radiologic estimation of kidney stone size and location complete the triad of emergency management. Asymptomatic stones less than 5mm are not treated Ureteral stones less than 5mm in diameter tend to pass spontaneously and usually do not require urologic intervention if resolved in 2-3 days. Ureteral stones greater than 7mm rarely pass spontaneously. Stones in the ureter below the pelvic brim that have arrested are usually removed by cystoscopy or with extracorporeal shock-wave lithotripsy (ESWL). Stones that arrest in the proximal ureter require cystoscopic intervention to push the stone back up to the renal pelvis. After this procedure ESWL may be used to fragment the stone. Stones that cannot be pushed to the pelvis require placement of bypass stent to decompress the obstruction and ESWL is used to fractionate the stone in its ureteral location. Intrarenal stones between 5mm and 2 cm are best treated with ESWL. Intrarenal stones greater than 2cm or stones larger than 1 cm in the lower pole of the kidney are best treated by percutanous nephrolithotomy. Lithotripsy failures should undergo percutaneous nephrolithotomy. Beth Israel Deaconess Medical Center Interns’ Report Ureterolithotomy is used as a last resort if all other approaches fail. Cystine stones are resistant to ESWL and often require percutaneous nephrolithotomy. Reviewed literature recommends that captured stones be sent for chemical analysis. Urgent urology consult if urosepsis, acute renal failure, anuria, and/or unyielding pain, nausea, or vomiting. Types of Kidney Stones: 35% pure calcium oxalate 40% calcium oxalate with hydroxyapatite or carbonate apatite 1% brushite (CaHPO4 2H2O) 8% struvite (magnesium ammonium phosphate) 8% urate stones 2% cystine Rarely ammonium urate, xanthine, drugs (indinavir, etc.) Prevention of Recurrence: OUTPATIENT W ORK UP: Analysis of the stone is the first step in identifying reversible or treatable causes of nephrolithiasis. After 2-3 weeks have passed after the episode of renal colic, a battery of urine and blood tests are recommended. It is important that these tests are ordered after the patient has been enjoying his or her normal diet to identify obvious abnormalities. Among these tests is a 24 hour urine collection that is done first with the patient’s normal diet. A repeat urine collection is done after a one week long 400mg/day calcium diet and again after a “calcium challenge test.” The following data should be gathered on these collected urines:volume, pH, calcium, magnesium, potassium, sodium, ammonia, urine urea nitrogen, creatinine, cystine, oxalate, citrate. Blood samples should also be acquired to check electrolytes, calcium, magnesium, and phosphorous. Some sources recommend ordering parathyroid hormone and calcitriol with the initial battery of tests, while others base this recommendation on calcium and phosphate findings on initial labs. These tests identify the most common causes or renal stones, but another category is not identified: renal stones that are secondary to faulty intrinsic inhibitors of stone formation. Several proteins inhibit crystal formation and may be defective in stone formers. These include TammHorsfall (inhibits aggregation of calcium oxalate unless it self-aggregates because of a defect), nephrocalcin (inhibits calcium oxalate crystal growth), and uropontin (another inhibitor of calcium oxalate growth). CRYSTAL ETIOLOGY / PATHOPHYSIOLOGY AND TREATMENT: Dehydration is an easily addressable cause of kidney stones. Though unstudied, the goal of high fluid intake seems to decrease occurrence of all stones. Calcium-handling defects causing hypercalcuria: Commonest stones contain calcium, so a defect often occurs that causes hypercalcuria. The mechanisms include increased intestinal absorption, decreased renal absorption of calcium, excessive bone reabsorption, combination of the above. Most people have a daily excretion of calcium around 4mg/kg/day when consuming 1 g of calcium per day. Lower calcium intake should be mirrored in lower urinary excretion. Sodium intake also affects calcium absorption, with increased dietary sodium promoting increased calcuria. Calcium handling defects causing nephrolithiasis include primary hyperparathyroidism, sarcoidosis, idiopathic hypercalcuria, malignant neoplasms, secondary hyperparathyroidism (renal-leak theory), and excess vitamin D. Newer data indicates that patients with calcium nephrolithiasis are also at risk of decreased bone density due to their defect in calcium handling. To summarize hypercalcuria: Absorptive hypercalcuria type I: Calcium stones with normal serum calcium and phosphate, hypercalcuria (>200mg/d) with restriction of calcium (400mg/d) and sodium (100meq/d), normal or low PTH, exaggerated calcuria after 1 g calcium challenge (>0.2 mg u Ca/mg u creatinine), normal fasting urinary calcium (<0.11mg/dL GFR) Beth Israel Deaconess Medical Center Interns’ Report Absorptive hypercalcuria type II: Same as above except for normal urinary calcium levels on restricted calcium and sodium diet. Absorptive hypercalcuria type III: Same as type I except with hypophosphatemia Renal hypercalcuria: Normal serum phosphate and calcium, hypercalcuria on restriction, fasting calcium wasting, high PTH. Other idiopathic hypercalcuria: Same as renal hypercalcuria except with normal PTH. Primary hyperparathyroidism: Hypercalcemia, hypophosphatemia, high PTH, hypercalcuria, abnormal parathyroid tissue. Treatments include: 2-3 L of urine output per day Treatment of hyperparathyroidism or other non-idiopathic cause Normal Calcium diedt and reduced sodium diets. Thiazide diuretics: Cause volume contraction leading to increased absorption of calcium in proximal tubule and decreased calcuria. Directly stimulate calcium absorption distally. Retained renal calcium temporarily decreases intestinal absorption. Potassium phosphate Sodium cellulose phosphate (calcium binder) not frequently used because of reflex hyperoxaluria and bone loss. Hyperoxaluria as cause of calcium oxalate stones: Normal people excrete 20-40 mg of oxalate per day. Excess ingestion of high oxalate foods may be the isolated cause of hyperoxaluria. These foods include spinach, rhubarb, Swiss chard, beets, cocoa, peppers, wheat germ, peanuts, okra, pecans, chocolate, and lime peel. If dietary excess is not the cause hyperoxaluria it is divided into enteric and primary. Enteric: Patients with inflammatory bowel disease, history of resections, and history of jejunoileal bypass are predisposed to this by incomplete absorption of bile salts and fatty acids leading to a detergent action on the colon, increasing non-selective colonic permeability to multiple substances including oxalate. These detergents also bind calcium and magnesium, freeing up more oxalate for colonic absorption. This increased absorption leads to increased urinary oxalate, supersaturation, and ultimately stone formation. Treatment is high fluid intake, low fat diet, calcium supplements, magnesium supplements, and cholestyramine. Primary hyperoxaluria: Genetic defects in liver enzymes leading to high oxalate and often early onset nephrolithiasis, nephrocalcinosis, and renal failure. One variety of this condition may respond to pyridoxine. High urine output, thiazides, and potassium phosphate may also help. Hypocitraturia as cause of calcium stones: Distal Renal Tubular Acidosis (RTA), chronic diarrheal illnesses, and idiopathic hypocitraturia may decrease the amount of citrate in the urine. Citrate functions to bind calcium, competing with oxalate. Therapy is potassium citrate, a therapy that replaces the lost alkali in these two syndromes. Sodium citrate expands volume and decreases proximal tubular calcium reabsorption, so it is not used. Hyperuricosuria as cause of calcium stones: Allopurinol has been shown to decrease formation of calcium oxalate stones. This observation has prompted the theory that heteronucleation may occur with a seed uric acid crystal providing a nidus for calcium crystal formation. Low purine diets, allopurinol, and urinary alkalinization may all be used. Uric Acid Stones: Acid urine promotes formation of urate stones. Alkalinization with potassium citrate may help avoid precipitation of urate, but this is difficult to maintain around the clock. Allopurinol is a reasonable therapy since alkalinization is difficult to maintain. Beth Israel Deaconess Medical Center Interns’ Report Struvite Stones: Also known as magnesium ammonium phosphate stones or “triple phosphate stones.” These stones are caused by bacterial superinfection with urease producing organisms such as Klebsiella, Proteus, Enterococci, and Pseudomonas. E.Coli infection does not cause struvite stones. These stones can often grow to be very large (staghorn calculi) and may not pass. The approach to these patients should be to remove the stone and treat the infection. ESWL or percutaneous nephrostolithotomy are used. The stone should be seen as an infected foreign body until it passes or is removed. Cystine Stones: These stones are very rare and are caused by an inherited defect in amino acid transport leading to high levels of cystine in the urine. Rarely high urine output alone is enough to avoid cystine crystals, but often the amount of urine necessary to dilute the cystine load is unattainable (greater than 4L qd). In this case chelating agents penicillamine, tiopronin or captopril can be used. These stones often do not respond to ESWL. Bibliography Coe, FL et al. The pathogenesis and treatment of kidney stones. NEJM. 1992. Vol 327. No 16:1141-51. Hruska, K. Renal Calculi (nephrolithiasis). Goldman: Cecil Textbook of Medicine. 21 st ed. 623627. Levy, FL et al. Ambulatory Evaluation of Nephrolithiasis: An Update of a 1980 Protocol. Amer J of Med. 1995. 98: 50-59. Beth Israel Deaconess Medical Center Interns’ Report