Headache presentations - The Student Health Association
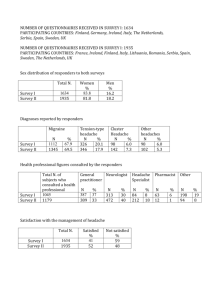
advertisement

The diagnosis and investigation of adult headache presentations in primary care David Kernick General Practitioner St Thomas Health Centre Cowick Street Exeter Address for correspondence: St Thomas Health Centre Cowick Street Exeter su1838@eclipse.co.uk Case A twenty-one year old female presents with a recent history of a severe headache that lasted four hours. She had to take to her bed and felt nauseated. Her mother had migraine at this age. Her father had died suddenly in his forties but she was unaware of the cause of death. Over the next six months she had three similar but less severe attacks that responded to simple analgesia and domperidone. The GP diagnosed migraine and shortly afterwards she moved away from the practice. 1 Background In a three-month period, 70% of the adult population will have headache.1 3% of GPs consultations are for headache and 4% of headache consultations will result in a referral to secondary care.2 Invariably there will be an underlying concern for patient and practitioner that there is a serious underlying cause and in particular a brain tumour. The two major classifications of headache are primary where there is no identifiable underlying disorder and secondary, where an underlying cause can be identified. (Table 1 shows the main sub headings of these groups.) Some will present as medical emergencies. Others will not be life threatening but have a major impact on quality of life. In many cases a diagnostic threshold will not be reached and careful observation is required until a diagnosis can be made. Table 2 shows an estimate of the incidence of important presentations in primary care.3 4 5 Table 1 in here Table 2 in here This article addresses two questions: firstly, what clinical features increase diagnostic accuracy; secondly, who needs further investigation? Unfortunately, the evidence base on which to base these answers is limited. Studies are characterised by small sample sizes, a wide range of estimates, retrospective recall bias and specialist centre focus. Diagnosing headache in primary care The primary headaches Migraine Migraine is the most likely cause for headache presentations in primary care3 but one third will be incorrectly diagnosed6. A number of simple screening questions have been developed that have high sensitivity and specificity when compared with the 2 formal International Headache Society criterion. For example, recurrent headaches that interfere with function, lasting at least 4 hours with no new headache in past 6 months7. A pooled analysis identified five relevant features that are shown in table 3 8 . Table 3 in here Cluster headache Cluster headache affects 0.1% of the population and is invariably misdiagnosed or inappropriately treated. The cluster attack is predominately unilateral, peri-orbital, excruciatingly painful, occurs in short bursts over a period of time (the cluster period) and is associated with peri-orbital or nasal autonomic features. 90% of attacks occur daily for 6-8 weeks with spontaneous resolution once or twice a year. In view of the paucity of data in cluster headache, it is recommended that all new cases of cluster headache are imaged. This can be relaxed for presentations of established disease. Tension type headache Tension type headache is poorly understood. The headache is usually dull, occipital and bilateral. It has been suggested that in many cases tension type headache is part of a migraine spectrum and based on similar neural mechanisms. Some other less common primary headaches are shown in table 4 Table 4 in here Subarachnoid haemorrhage The incidence of subarachnoid haemorrhage (SAH) is 10 per 100,000 persons per year. 50% will not survive and one third of survivors need life long care9 10 11 . A missed diagnosis is the most common cause of neurological litigation12. Risk factors include smoking, excess alcohol consumption, hypertension, a positive family history, polycystic kidney disease and connective tissue disorders. The following features are more frequent in SAH: occipital location, nausea, neck stiffness, impaired consciousness. The most common presentation is a “thunderclap headache” that reaches maximum intensity within 10 seconds and lasts for a few hours. 12% of such patients have a SAH rising to 25% if examination is abnormal. The term “sentinel” headache or “warning bleed” is misleading as it simply represents a small subarachnoid haemorrhage that was not identified at the time. The “worst headache 3 ever” which may not be a thunderclap presentation is always cause for concern. 12% of these patients with a normal neurological examination will have a subarachnoid haemorrhage10. Meningitis In developed countries, the annual incidence of bacterial meningitis is 3 per 100,000 and viral meningitis 11 per 100,000. Risk factors include diabetes, otitis media, alcohol abuse, pneumonia and sinusitis13. Physical examination has sensitivities that are clinically useful14 15: Fever - 85% (CI 78%-91%) Neck stiffness - 70% (CI 58%-82%). Alteration in mental status - 67% (52%-82%). Jolt accentuation of headache - sensitivity of 97%, specificity 60%, positive likelihood ratio 2.4. The evidence for other signs of meningeal irritation is conflicting. Kernig’s sign (extension of the knee with a hip flex at 90° elicits resistance or pain in the lower back or posterior thigh) and Brudzinski sign (passive neck flexion in a supine patient results in flexion of the knees and hips) have low sensitivity but high specificity. In summary, the absence of all three signs of fever, neck stiffness and altered mental state virtually eliminate the diagnosis of meningitis. Jolt accentuation is a useful manoeuvre to confirm a positive diagnosis. Temporal arteritis Temporal arteritis is a generalised vasculopathy affecting medium and large arteries with an incidence of 10 per 100,000 per year. It should be considered in any patient older than 50 years with headache. Visual impairment due to involvement of the ophthalmic artery is the main concern and may present as the first symptom. The headache can mimic the features of other primary headaches although the headache gradually worsens with time. Other features include jaw claudication and constitutional symptoms of anorexia, weight loss, fever, malaise and depression. A raised erythrocyte sedimentation rate (ESR) can be a useful laboratory indicator. However a raised ESR is a non-specific finding, while studies of biopsy proven arteritis demonstrate normal ESRs in between 4 5% and 30% of cases16. A review of all clinical studies17 found positive likelihood ratios of: Jaw claudication 4.2 (CI 2.8-6.2). Dyploplia 3.4 (CI 1.3-8.6). Temporal artery beading 4.6 (CI 1.1 -18.4), prominence 4.3 (CI 2.1 – 8.9) and tenderness 2.6 (CI 1.9 – 3.7). The absence of any temporal artery abnormality gave a negative likelihood ratio of 0.53 (CI 0.38-0.75). Primary Brain Tumour The incidence of primary brain tumours is 6-10/100000 population/year of which 72% will present above the age of 5018. 2% to 16% of tumours will present with isolated headache and 0.09%(CI 0.08-0.10) of headache presentations in primary care will be due to a primary tumour19. A review of the literature found the following features associated with headache that gave important likelihood ratios8: Abnormal findings on neurological examination - 5.3 (CI 2.4-12) Headache aggravated by exertion or Valsalva like manoeuvre - 2.3 (CI 1.43.8) Headache with vomiting - 1.8 (CI 1.2-2.6) Other important secondary headaches are shown in table 5. Table 5 in here Practical guidance for the practitioner on who to investigate Due to limited data in the area, guidance is based largely on expert opinion combined with available evidence. For example, referral guidelines have been issued by The British Association for the Study of Headache and NICE (see article web site – web tables 1 and 2). For the practitioner, other inputs on the decision to investigate include medico-legal case law, organisational factors, service availability and the expectations of practitioner and patient and the way they handle risk.20 5 The following features of the headache or features associated with it should alert the physician to a possible serious underlying cause and the need for further investigation. Thunderclap headache. Neck stiffness and fever. Alteration in mental status. Papilloedema. Abnormal findings on neurological examination. Vomiting. Aggravation with exertion or Valsalva manoeuvre. Temporal artery abnormalities. Jolt accentuation. New isolated headache where a diagnosis has not emerged after eight weeks. Headaches that have been present for some time but have changed significantly. New headache in a patient over 50. Conclusion to the case. A year later the GP received a letter from a solicitor specialising in medical negligence. The patient had been found dead in bed and post-mortem demonstrated a ruptured cerebral aneurysm. GPs are sometimes in a dilemma. Not all first presentations of headache can or should be investigated. However, presentations of “first ever headache” should be managed cautiously particularly when severe. TABLES Main primary headaches - Migraine - Tension - Cluster type headache headache and other trigeminal autonomic cephalalgias Main secondary headaches - Headache attributed to head or neck trauma. - Headache attributed to cranial or cervical vascular disorder. 6 - Headache attributed to non-vascular intracranial disorder. - Headache attributed to a substance or its withdrawal. - Headache attributed to infection - Headache attributed to disorder homeostasis - Headache or facial pain attributed to disorder of cranium, neck, eyes, nose, sinus, teeth, mouth or other facial or cranial structures. - Headache - Cranial attributed to psychiatric disorder. neuralgias and central causes of facial pain. Table 1. Main categories of primary and secondary headache.21 (A full classification can be found at www.i-h-s.org ). Diagnosis Incidence Migraine 73% Other primary headache 23% (predominantly tension type) Sub-arachnoid haemorrhage 0.05% Meningitis 0.02% Temporal arteritis 0.02% Primary tumour 0.09% Table 2. Estimates of the incidence of some important headache presentations in primary care. Pulsatile quality of headache. Duration of 4-72 hours, Unilateral location nausea or vomiting. Disabling intensity. Positive likelihood ratios were: 24 (CI 1.5-388) for four or more features. 3.5 (CI 1.3-9.2) for three features. 0.41 (CI 0.32-0.52) for one or two features. 7 Table 3. Features that indicate migraine and their likelihood ratios Headache type Features Paroxysmal hemicrania Similar to cluster headache but pain is shorter lasting and more frequent characterised by an absolute response to adequate doses of Indomethacin. Primary stabbing headache Short stabs or jabs lasting up to a few seconds and recurring frequently. Predominantly felt in distribution of the first division of the trigeminal nerve. Hypnic headache Dull headache that always awakens patient from sleep often at a similar time, and occurs at no other time Hemicrania continua Persistent unilateral pain of moderate intensity but with severe exacerbations. Autonomic features during an exacerbation. Characterised by an absolute response to Indomethacin Table 4. Some less common primary headaches Comments Diagnosis Secondary brain tumours Brain metastases occur in 20-40% of patients with cancer. Lung (43% of secondary tumours) and breast (8% of 8 secondary tumours) are the predominant primary locations. Non-progressive space-occupying Occur with similar frequency to primary lesions. E.g. cysts, arterio-venous tumours but their contribution to malformations and aneurysms. headache is less certain Cerebral venous sinus thrombosis. Risk factor for venous thrombosis often present. Idiopathic Intracranial Hypertension Daily headache with papilloedema in 90% and features of raised intracranial pressure (morning worsening, Valsalva worsening) and otological symptoms (pulsatile tinnitus). Patients usually obese. The headache is often throbbing and can resemble daily migrainous symptoms. Spontaneous Intracranial Hypotension Daily headache worsened within 15 minutes of upright posture and resolved by recumbent posture. Often follows minor head trauma. Headache is often absent on wakening and worsens though the day whilst erect. Dissection of carotid or Vertebrobasilar artery Pain can be head, neck or face. Neurological features may be minimal, absent or fluctuating. Always examine for a horners syndrome in patients with neck pain ( horners syndrome may indicate a dissection of carotid artery Hypertensive encephalopathy Blood pressure mandatory in all headache presentations Carbon monoxide poisoning Ask about headache in other family members and type of heating. Acute angle closure glaucoma Periorbital pain, visual disturbance 9 (particularly halo), can be nausea or vomiting. Table 5. Other causes of secondary headache needing urgent investigation FOR WEBSITE Search Strategy Articles in MedLine were searched using the following MESH terms: Subarachnoid tumour AND review (literature) Temporal arteritis AND review (literature) Meningitis AND headache Brain tumour AND review (literature) Web Table 1 - Headache presentations suggesting urgent assessment as suggested by The British Association for the Study of Headache (www.bash.org.uk) - Thunderclap - Associated - Headache headache (intense headache with abrupt or “explosive” onset) with other signs or symptoms with atypical aura (duration >1 hour, or including motor weakness) - New onset headache in a patient older than 50 years - New onset headache in a patient younger than 10 years - Progressive headache, worsening over weeks - Headache associated with postural change - Headache markedly worse with wakening, straining or coughing - New onset headache in a patient with a history of cancer or HIV infection Web Table 2 - Headache presentations suggesting urgent assessment as suggested by NICE (www.nice.org.uk)_ 10 Headaches of recent onset accompanied by features suggestive of raised intracranial pressure (for example, vomiting, drowsiness, postural related headache with pulse synchronous tinnitus) or other focal or non-focal neurological symptoms (for example, blackout, change in personality or memory) - an urgent referral should be made. Unexplained headaches of recent onset present for at least one month but not accompanied by features suggestive of raised intracranial pressure - discussion with a local specialist or referral (usually non-urgent) should be considered. A new qualitatively different unexplained headache that becomes progressively severe an urgent referral should be made. Reassessment and re-examination is required if the patient does not progress according to expectations. References 1 Boardman H, Thomas E, Croft PR, Millson DS, Epidemiology of headache in an English district. Cephalalgia 2003;23:129-37. 2 Latinovic R, Gulliford M, Ridsdale L. Headache and migraine in primary care: consultation, prescription and referral rates in a large population. J Neurol Neurosurg Psychiatry 2006;77:385-387. 3 Tepper S, Dahlof C, Dowson A, Newman L, Mansbach H, Jones M, et al. Prevalence and diagnosis of migraine in patients consulting their physician 11 with a complaint of headache: data from the Landmark Study. Headache 2004;44:856-864. 4 Watson D. Ominous headache in primary care: myth or reality? Headache Care 2004;1(1):17-18. 5 General Practitioner Workload. Royal College of General Practice. London 2004. 6 Lipton RB, Scher A, Steiner T, Bigal M, Kolodner K,Liberman J et Al. Patterns of health care utilization for migraine in England and in the United States. Neurology 2003;60:441-448. 7 Martin V, Penzien D, Houle T. The predicted value of abbreviated migraine diagnostic criteria. Headache 2005;45:1102-12. 8 Detsky M, McDonald D, Baerlocher M, Tomlinson G, McCory D, Booth C. Does this patient with headache have a migraine or need neuro imaging? JAMA 2006;296:1274-1283. 9 Hop J, Rinkel G, Algra A, Van Gign J. Case fatality rates and functional outcome after subarachnoid haemorrhage: a systematic review. Stroke 1997;28:660-4. 10 Suarez J, Tarr R, Selman W. Aneurysmal subarachnoid haemorrhage. N Eng J Med 2006;354(4):387-396. 11 Al-Shahi R, White P, Davenport R, Lindsay K. Subarachnoid haemorrhage. BMJ 2006; 333(7561):235-40. 12 Edlow J, Kaplan L. Avoiding pitfalls in a diagnosis of subarachnoid haemorrhage. N Engl J Med. 2000;342(1):29-36. 13 Durand M, Calderwood S, Webber D. Acute bacterial meningitis in adults: a review of 493 episodes. N Engl J of Med 1993;328:21-28. 14 Attia J, Hatala R, Cook D, Wong J. Does this adult patient have acute meningitis? JAMA 1999;282:175-181. 15 Uchihara T, Tsukagoshi H. Jolt accentuation of headache: the most sensitive sign of CSF pleocytosis. Headache 1991;31:167-71. 16 Zweegman S, Makkink B, Stehouwer C. Giant cell arteritis with normal erythrocyte sedimentation rate: case report and review of the literature. JAMA 2002;287:92-101. 17 Smetana G, Shmerling R. Does this patient have temporal arteritis? Neth J Med 1993;42:128-31. 12 18 Counsell C, Grant R. Incidence studies of primary and secondary intracranial tumours: a systematic review of their methodology and results. J NeuroOncol 1998;37:241-50. 19 Hamilton W, Kernick D. Clinical features of primary brain tumours: a casecontrol study using electronic primary care records. Br J Gen Pract. 2007;57(542):695-9. 20 Morgan M, Jenkions L, Ridsdale L. Patient pressure for referral for headache. BJGP 2007;57:29-35. 21 International classification of headache disorders, 2nd edition. Cephalalgia 2004;Volume 24. supplement 1. 13