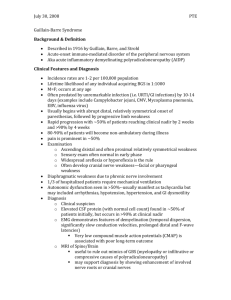
GBS Guidelines
advertisement
Guidelines for Prevention of Neonatal Group B Streptococcal Infection Purpose of Policy: Intrapartum antibiotic prophylaxis (IAP) to prevent neonatal Group B Streptococcal (GBS) disease has reduced the incidence of invasive early-onset GBS infections in newborns by 70%. The revised 2002 CDC guidelines for the prevention of GBS disease are based upon universal screening for GBS in all pregnant women. Scope of Policy: Nurses, LIP with OB privileges, residents Policy/guideline: I. Screening: Screen every (see exceptions*) pregnant woman for GBS with vaginal and rectal culture at 35-37 weeks gestation. If the pt is PCN allergic, request sensitivities on culture. Review culture results. If a GBS culture is positive during the current pregnancy, regardless of EGA obtained, the patient is treated as GBS positive. If a GBS culture is negative, and was obtained > 5 weeks prior, re-screen for GBS. (* Do NOT screen at 35-37 weeks patients who: ○ GBS bacteriuria in present pregnancy ○ Previous infant affected by invasive GBS disease These patients will automatically receive prophylaxis at delivery) II. Intrapartum Prophylaxis Indicated: Previous infant with invasive GBS disease GBS bacteriuria during current pregnancy Positive GBS screening culture during current pregnancy (unless delivered by cesarean section, in the absence of labor or ruptured membranes). Unknown GBS status (culture not done, incomplete, or results unknown) AND any of the following: ○ Delivery at < 37 weeks’ gestation. (*see below) ○ Amniotic membrane rupture ≥ 18 hours ○ Intrapartum temperature > 100.4 0 F (≥ 38.4 C tympanic) ○ Intrapartum NAAT** + for GBS (**Nucleic acid amplification test =rapid test for GBS; soon to be available on L&D) If chorioamnionitis is suspected, use broad spectrum antibiotic also active against GBS. *● Give IAP when diagnosis of preterm labor is made at <37 wks and continue until delivery or until labor is arrested and tocolytic therapy is discontinued. ● PPROM > 34.0 weeks: Deliver. Give IAP unless GBS culture was negative ● PPROM <34.0 weeks : a) If laboring and + GBS/unknown GBS treat with appropriate regimen below b) If not laboring and GBS known/unknown: latency ATBs (total = 7 days) 1) Amp 2 g IVPB then 1 g IVPB Q 6 X 48 hours and Erythro 250 mg IVPB Q 6 X 48 hours then 2) Amoxicillin 250 mg Q 8 X 5 days and Erythro 333 mg Q 8 X 5 days c) Obtain GBS culture results and treat accordingly when labor begins. If culture is negative and labor occurs > 5 weeks from result, re-screen patient III. Intrapartum Prophylaxis NOT Indicated: Current pregnancy is documented to be GBS negative even if previous pregnancy screened GBS positive. Planned cesarean delivery performed in the absence of labor or membrane rupture (regardless of maternal GBS culture status). Negative vaginal and rectal GBS screening culture in late gestation during the current pregnancy, regardless of intrapartum risk factors. Regimens for IAP prophylaxis: IV. 1. PCN G, 5 million units IV initial dose, then 2.5 million units IV every 4 hours until delivery. 2. If PCN allergic AND NOT at high risk for anaphylaxis: Cefazolin, 2g IV initial dose, then 1g IV every 8 hours until delivery. 3. If PCN allergic AND at high risk for anaphylaxis, GBS susceptible to both Clindamycin and Erythromycin: Clindamycin, 900 mg IV every 8 hours until delivery (Use of Erthromycin no longer recommended even if sensitive) 4. If PCN allergic AND at high risk for anaphylaxis, GBS sensitivities unknown, OR GBS resistant to either Clindamycin or Erythromycin: Vancomycin, 1 g IV every 12 hours until delivery V. Initiation of IAP Prophylaxis: 1. Antibiotics for IAP should be entered by the provider with admission orders. 2. IAP antibiotics will be started by the nurse when: a. regular CTXs established (Q 5 min or less) b. ROM at any point in the labor process c. as otherwise ordered in PCOSS (e.g. Start IAP on admission for Hx rapid labor) VI. Management of Newborns Exposed to IAP: 1. If a woman is considered to have chorioamnionitis (maternal temp>38 AND two of the following; maternal WBC>15, maternal tachycardia>100, fetal tachycardia>160, uterine tenderness and foul odor of amniotic fluid) The newborn should have diagnostic evaluation and may receive empiric antibiotic therapy. Consultation with obstetric provider is important to determine neonatal management. a. Level 1 Code Pink should be called for all deliveries to women with chorioamnionitis 2. Adequate GBS intrapartum antibiotic prophylaxis is >4 hours of PCN, ampicillin or cefazolin before delivery. All other agents are considered inadequate for neonatal management 3. Well appearing infants of any gestational age whose mother received adequate intrapartum prophylaxis should be observed for >48 hours. No routine diagnostic testing is recommended. 4. Infants born to mothers with an indication of GBS prophylaxis who received inadequate or no treatment, if the infant is; a. Either <37 weeks gestational age or rupture of membranes > 18 hours prior to delivery, it is recommended that newborn should undergo limited evaluation and observation for > 48 hours i. Newborn’s pediatrician (appropriate private Pediatrician or Mac Peds team for Interim/RAP patients) must be contacted by L&D nurse to decide on course of action. Nurse should note conversation in infant chart. ii. Mac Peds team needs to be called as phlebotomy for any private Pediatrician’s newborn requiring venipuncture for laboratory tests. iii. Maternal screens including GBS status are to be reviewed by accepting Mac 3/5 nurse as well as review of action taken for newborns born to mother receiving inadequate IAP. If L&D nurse did not contact Pediatrician, Mac 3/5 nurse must do so b. If the infant is well appearing and > 37weeks and rupture of membranes < 18 hours prior to delivery no routine diagnostic evaluation is recommended. The infant should be observed for 48 hours. Reference: Verani J, McGee L, SchragS.Prevention of Perinatal Group B Streptococcal Disease; revised guidelines from CDC 2010 References: Schrag S, Gorwitz R, Fultz-Butts K, Schuchat A. Prevention of perinatal Group B Streptococcal disease: revised guidelines from CDC. MMWR 2002;51:1-21. Revised and Approved 02/16/11 MacDonald Quality Council Approved MFM division 8/28/2009 Approved Perinatal Collaborative 7 2009 Approved CQPS 8 2009 Located on the S/Drive Machouse/OB Guidelines/GBS Prophylaxis