10 - Springer Static Content Server
advertisement

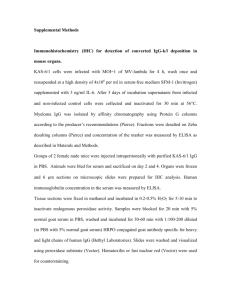
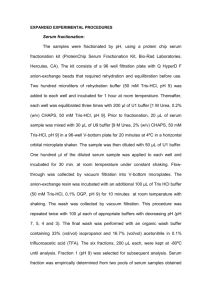
1 Supplementary Materials Radiotherapy The gross tumor volume (GTV) was defined as all macroscopically identifiable tumor determined by CT scan, EUS, esophagogram, and PET scan. The clinical target volume (CTV) was defined as 4 cm proximal and distal as well as 0.5 cm lateral beyond GTV. The CTV included the supraclavicular nodes for upper-third primaries and celiac nodes for distal-third primaries. The planning target volume (PTV) was defined as the CTV plus 0.5-cm margins. A 0.5-cm margin around the spinal cord was added for the planning organ-at-risk volume. Inverse intensity-modulated radiation therapy (IMRT) plans were generated using a commercial treatment planning system (Pinnavle3, v9.0, ADAC Laboratories, Milpitas, CA). The CTV was irradiated with a total dose of 40 Gy at 2 Gy per fraction. The treatment was delivered with 6- and/or 10-MV photons using 3–5 beam fields (median 4 beams). The typical beam orientation was similar to the conventional four-beam arrangement with anteroposterior, posteroanterior, and two posterior oblique fields. The goals of inverse IMRT planning were to ensure that ≧95% of the PTV received the prescribed dose while keeping the exposure of normal structures within normally acceptable tolerances. 2 Proximity ligation assay (PLA) Probe pairs were made for each of the 15 protein markers by attaching goat or rabbit antibodies specific for each protein to complementary oligonucleotides using a Solulink Antibody-Oligonucleotide All-In-One Conjugation Kit. These probes were divided into two panels. Each of the individual probes and the probe panels were validated in a pilot study using either anti-goat or anti-rabbit antibodies as a pseudo-antigen. Multiplex PLA was performed on 158 frozen serum samples. Samples were thawed and mixed in a 1:1 ratio with buffer (Olink AB) and incubated for 10 minutes at room temperature. Two μL of either of the probe panels was mixed with 2 μL of the buffered serum sample and incubated for 2 hours at 37°C to allow the probes to bind to the analytes. Ligation was achieved by incubating 120 μL of reaction mixture with the 4 μL probed samples for 15 minutes at 30°C to dilute and separate any free probes. To stop the ligation, 2 μL of uracil-DNA excision mix (Epicentre) was added and incubated for 15 minutes at room temperature. Preamplification of bar-coded amplicons required mixing 25 μL of stopped ligation reaction mixture with 25 μL of pooled PCR mix (Platinum Taq kit, Invitrogen). After 13 cycles at 95°C for 30 seconds and a 4-minute extension at 60°C, the preamplification products were diluted 10-fold in TE. For each of the 3 15 proteins assayed, a separate qPCR reaction was run in a 384-well plate with 2 μL of diluted preamplication product sample, 5 μL of iTaq mix (iTaq SYBR Green Supermix with ROX, Bio-Rad), 2 μL qPCR primer mix, and 1 μL water. Real-time qPCR was performed with a sample volume of 10 μL per well for 40 cycles at 95°C for 15 seconds and 60°C for 1 minute. To ensure standardization of values for each biomarker investigated, all 158 samples were simultaneously probed and evaluated on a single 384-well plate with a PBS-BSA blank well. Cycle threshold (Ct) values resulting from qPCR were converted into estimated number of starting amplicons, or PLA units, by calculating 10(-0.301 × Ct+11.439) as previously reported 10. Enzyme-linked immunosorbent assay (ELISA) The serum biomarker concentration was measured with a commercially available human protein sandwich enzyme immunoassay kit with two mouse monoclonal antihuman antibodies (R&D Systems, Inc., Minneapolis, MN, USA). All serum samples from patients and standards were incubated in microplate wells coated with the first mouse monoclonal anti-human biomarker antibody. After washing, a second antihuman biomarker antibody labeled with peroxidase (HRP) was added for subsequent incubation. The reaction 4 between HRP and substrate (hydrogen peroxide and tetramethylbenzidine) resulted in color development and the intensities were measured with a microplate reader at an absorbance of 450 nm. Concentrations of serum biomarkers were determined against a standard curve. 5 Supplementary Table F factor and the significance (p value) by two-way analysis of variance (ANOVA) for the association of 15 serum biomarkers' pre-chemoradiotherapy (CCRT), post-CCRT, and pre-/post-CCRT changes of proximity ligation assay (PLA) data with pathological response. Biomarker Time factor (Pre- Response factor Interaction of Time versus (CR versus factor and Response Post-CCRT) microscopic factor F factor (p value) residual, versus macroscopic residual) Axl 3.0 (0.09) 0.43 (0.65) 0.66 (0.52) BMP2/4 2.37 (0.13) 0.40 (0.67) 0.40 (0.67) EGFR 3.53 (0.06) 0.53 (0.59) 0.81 (0.45) FAM84B 9.37 (0.003) 0.85 (0.43) 0.80 (0.45) Gas6 1.44 (0.23) 0.39 (0.68) 0.99 (0.38) Her2 4.26 (0.04) 0.39 (0.68) 0.35 (0.71) IGFBP3 0.13 (0.72) 0.69 (0.51) 0.32 (0.73) MMP1 0.18 (0.67) 0.70 (0.50) 2.55 (0.09) MMP13 2.68 (0.11) 0.20 (0.82) 1.06 (0.35) 6 OPN 0.15 (0.70) 2.15 (0.12) 0.14 (0.87) PDGFR-α 0.001 (0.97) 0.70 (0.50) 0.89 (0.42) Periostin 10.26 (0.002) 1.95 (0.15) 0.62 (0.54) SPARC 0.07 (0.79) 2.72 (0.07) 1.21 (0.30) TGF-β1 9.7 (0.003) 5.07 (0.009) 0.97 (0.38) VEGF-A 2.09 (0.15) 0.65 (0.53) 1.98 (0.15)