Neuroscience 18b – Depression and Anxiety
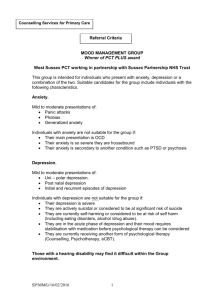
advertisement
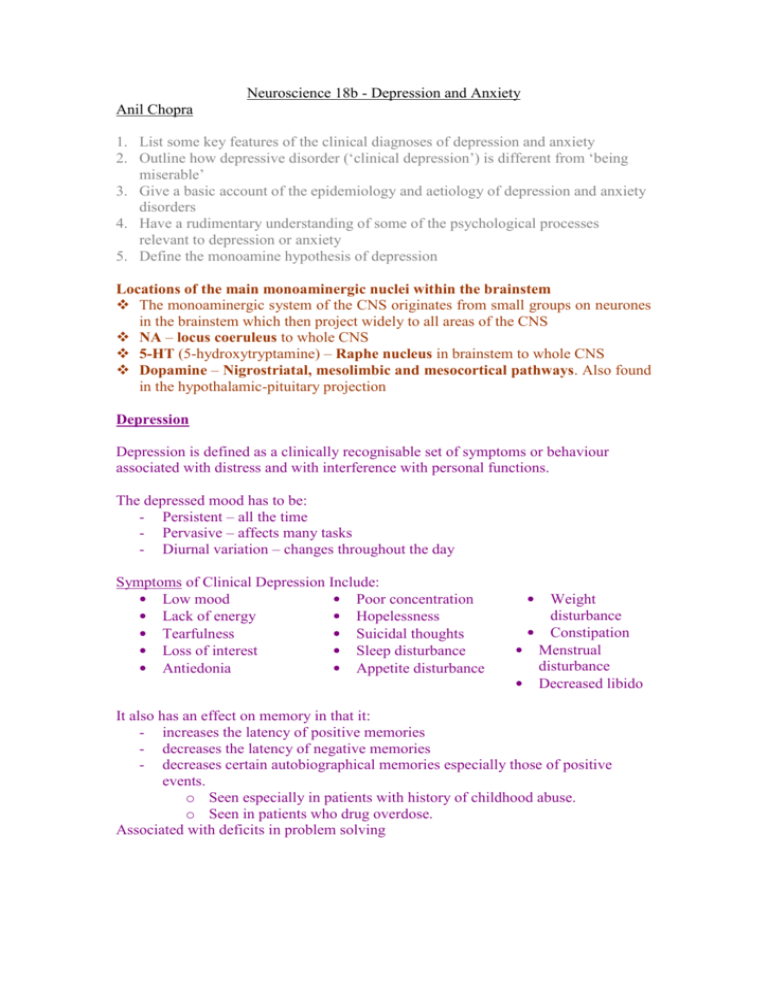
Neuroscience 18b - Depression and Anxiety Anil Chopra 1. List some key features of the clinical diagnoses of depression and anxiety 2. Outline how depressive disorder (‘clinical depression’) is different from ‘being miserable’ 3. Give a basic account of the epidemiology and aetiology of depression and anxiety disorders 4. Have a rudimentary understanding of some of the psychological processes relevant to depression or anxiety 5. Define the monoamine hypothesis of depression Locations of the main monoaminergic nuclei within the brainstem The monoaminergic system of the CNS originates from small groups on neurones in the brainstem which then project widely to all areas of the CNS NA – locus coeruleus to whole CNS 5-HT (5-hydroxytryptamine) – Raphe nucleus in brainstem to whole CNS Dopamine – Nigrostriatal, mesolimbic and mesocortical pathways. Also found in the hypothalamic-pituitary projection Depression Depression is defined as a clinically recognisable set of symptoms or behaviour associated with distress and with interference with personal functions. The depressed mood has to be: - Persistent – all the time - Pervasive – affects many tasks - Diurnal variation – changes throughout the day Symptoms of Clinical Depression Include: • Low mood • Poor concentration • Lack of energy • Hopelessness • Tearfulness • Suicidal thoughts • Loss of interest • Sleep disturbance • Antiedonia • Appetite disturbance • Weight disturbance • Constipation • Menstrual disturbance • Decreased libido It also has an effect on memory in that it: - increases the latency of positive memories - decreases the latency of negative memories - decreases certain autobiographical memories especially those of positive events. o Seen especially in patients with history of childhood abuse. o Seen in patients who drug overdose. Associated with deficits in problem solving The manifestation of depression is thought to be a cognitive process with a number of different causes: Genetic – family history Developmental o Emotional deprivation o Maternal separation o Parental discord and childhood abuse Neuroticism Situational factors o Loss events o Chronic difficulties e.g. money/housing o Lack of social support 70% of suicides have a history of depression and 15% of depressed people commit suicide. Recognition of is incredibly important clinically because it causes great distress and suffering not only to the patient but all those connected with him/her. It increases the burden of illness, reduces quality of life, reduces healing and is associated with a substantially increased suicide rate. - Rate of depressives = 3% - Rate of those who self harm = 0.3% - Rate of those who commit suicide = 0.03%. Epidemiology Lifetime risk 5-10% Risk to 1º relatives Sex ratio (F:M) Average age of onset 15% 2:1 27 yrs Unipolar illness – characterised by mood swings in the same direction with a relatively late onset. Reactive depression is suffered by 3-4 % of the population during their lifetime. It occurs due to stressful life events and shows non-familial suffering. Endogenous depression (1% of the population) is unrelated to external depression and shows a familial pattern. Drug treatment is via a trial method (different drugs and drug classes are tried until one is found that works with side effects that do not outweigh the beneficial effects). Bipolar illness (manic depression) – characterised by oscillating depression and mania. It is less common with a relatively early onset and strong familial pattern. The best drug for treatment is lithium. The monoamine hypothesis of depression This was first described by Schildkraut. It states that depression results from a functional deficit of the central monoaminergic transmission, and that mania results from a functional excess of monoaminergic transmission. Pharmacological evidence in some cases supports the theory (e.g. TCAs) and in others does not (e.g. cocaine, amphetamine), and biochemical evidence is inconsistent. Even though the general conclusions remain firm, they delayed onset of the clinical effect of drugs indicates that the adaptive changes may be more important (e.g. down-regulation of - and 2adrenoceptors). Anxiety Anxiety is a physiological state characterized by cognitive, somatic, emotional, and behavioral components. These components combine to create the feelings that we typically recognize as fear, apprehension, or worry. Symptoms Anxious rumination – negative thought Autonomic arousal o Palpitations o Sweating o Diarrhoea o Nausea Hyper vigilance o Poor concentration o Irritability o Insomnia Disorders of Anxiety PHOBIC ANXIETY DISORDERS – characterised by onset as a result of a particular stimulus/ circumstance. These circumstances tend to be avoided and anticipatory anxiety when the circumstance is expected. o Social phobia o Agoraphobia o Specific phobias PANIC DISORDER – regular attacks of anxiety without a particular stimulus. Symptoms often include: o Palpitations o Chest pain o Hyperventilation o Depersonalisation/derealisation o Fears e.g. ‘going mad’, losing control GENERALIZED ANXIETY DISORDER - characterized by excessive, uncontrollable and often irrational worry about everyday things, which is disproportionate to the actual source of worry.