Chlorine: Guidance for Health Care Providers

Virginia Department of Health
Chlorine: Overview for Healthcare Providers
Agent
Chlorine
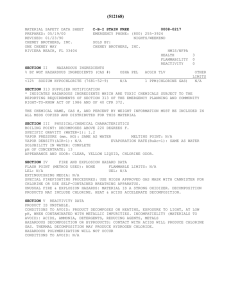
CAS number: 7782-50-5 UN number: 1017
Physical
Characteristics
Contamination/
Decontamination
Yellowish green gas with bleach-like, sharp, burning odor
Odor detection: 0.2 – 3.5 ppm; mild symptoms: 1-3 ppm; lowest reported lethal level: >430 ppm
Immediately Dangerous to Life or Health (IDLH): 10 ppm
Potential Sources
Chlorine is one of the most common industrial chemicals used in manufacturing and is transported in large tanker cars by rail and highway. It is often shipped as a liquid but readily becomes a gas when released from its container. Commonly used for disinfecting water. Chlorine comes in other forms such as sodium hypochlorite (bleach).
Route of Exposure
Most common route of exposure is by inhalation. Injury can also occur from skin contact.
Contamination: Patients with gas exposure are unlikely to have secondary contamination and pose little risk of causing harm to healthcare providers. Liquid products, such as industrial-strength chlorine bleach, can off-gas from contaminated clothing, hair and skin. Patients contaminated with liquid product pose a risk of releasing chlorine gas into the breathing space of healthcare providers. Decontamination: Decontaminate outside of hospital. Clothing removal and copious water rinse are adequate to decontaminate an exposure to liquid product. After decontamination, standard precautions are adequate for handling patients. NOTE: a chlorine (bleach) odor may persist on the patient’s skin despite adequate decontamination.
Risk Indicators
Cause of Death
Latency
Clinical manifestations
Laboratory tests/
Sample collection
Radiography
Treatment
Precautions/
Disposition
Notification
Extent of injury depends on the concentration and duration of exposure. Chlorine exposure may exacerbate underlying chronic diseases. Those with reactive airways disease, chronic pulmonary diseases, or cardiovascular disease are more susceptible to smaller exposures and may have serious effects.
Deaths are due to respiratory compromise or cardiovascular effects from respiratory compromise.
Extremely high concentrations (especially in enclosed space) can result in asphyxiation.
Most exposures result in immediate irritant symptoms. Mild symptoms typically resolve within a few hours. Delayed pulmonary edema has developed hours after exposure in patients with persistent or severe symptoms at the time of exposure.
INHALATION EXPOSURE causes IRRITANT GAS effects
ENT: Burning eyes, nose and throat
Respiratory: Cough, chest pain (burning sensation), shortness of breath, wheezing, hypoxemia, tachypnea, hemoptysis, delayed pulmonary edema
SKIN: Gas exposure can cause irritation of skin. Direct skin contact with high concentrations or prolonged duration causes corrosive burns. Serious skin injuries are likely to have associated inhalational injury.
Confirmatory diagnostic testing: None. On-scene environmental monitoring may provide the best evidence of the presence of chlorine.
Monitor clinical effects and complications: CXR, ABG, oxygen saturation, peak flow as indicated.
CXR findings are not specific for chlorine but may confirm the presence of acute lung injury.
Supportive Care: Fresh air, humidified oxygen, and bronchodilators. Aerosolized sodium bicarbonate has sometimes been used as a therapy but with unproven benefit.
Antidotes: None
Pitfall: Not recognizing patients at risk for progressive lung injury.
Those with significant signs of toxicity shortly after exposure may improve but exhibit persistent symptoms and several hours later have a worsening condition with noncardiogenic pulmonary edema.
Disposition: Asymptomatic patients and those who experienced only minor symptoms that resolve within 1-2 hours may be released.
All chemical exposures should be reported to the regional poison center at 1-800-222-1222.
Outbreaks and unusual occurrences are reportable to your local health department. If this is a suspected emergency then report the incident to the local 911 center.
For more information, refer to : Virginia Department of Health, www.vdh.virginia.gov/EPR/Agents.asp
and the Centers for Disease Control and
Prevention, www.bt.cdc.gov
or www.atsdr.cdc.gov/MHMI/mmg172.html
Updated 07/19/2004