Adolescent-Psychiatry
advertisement
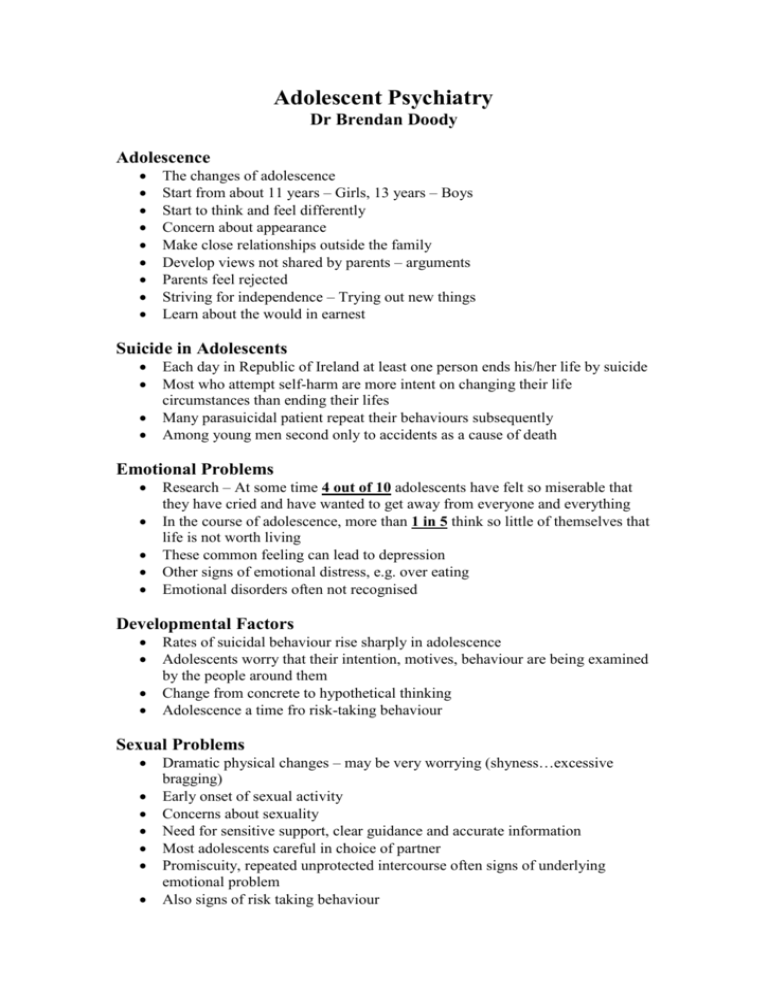
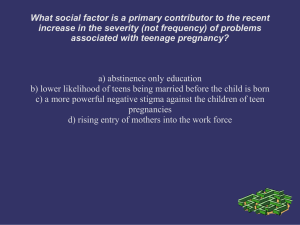
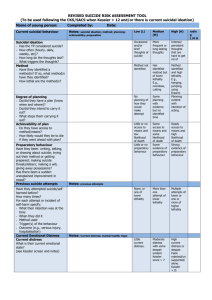
Adolescent Psychiatry Dr Brendan Doody Adolescence The changes of adolescence Start from about 11 years – Girls, 13 years – Boys Start to think and feel differently Concern about appearance Make close relationships outside the family Develop views not shared by parents – arguments Parents feel rejected Striving for independence – Trying out new things Learn about the would in earnest Suicide in Adolescents Each day in Republic of Ireland at least one person ends his/her life by suicide Most who attempt self-harm are more intent on changing their life circumstances than ending their lifes Many parasuicidal patient repeat their behaviours subsequently Among young men second only to accidents as a cause of death Emotional Problems Research – At some time 4 out of 10 adolescents have felt so miserable that they have cried and have wanted to get away from everyone and everything In the course of adolescence, more than 1 in 5 think so little of themselves that life is not worth living These common feeling can lead to depression Other signs of emotional distress, e.g. over eating Emotional disorders often not recognised Developmental Factors Rates of suicidal behaviour rise sharply in adolescence Adolescents worry that their intention, motives, behaviour are being examined by the people around them Change from concrete to hypothetical thinking Adolescence a time fro risk-taking behaviour Sexual Problems Dramatic physical changes – may be very worrying (shyness…excessive bragging) Early onset of sexual activity Concerns about sexuality Need for sensitive support, clear guidance and accurate information Most adolescents careful in choice of partner Promiscuity, repeated unprotected intercourse often signs of underlying emotional problem Also signs of risk taking behaviour Behaviour Problems Teenagers and parents complain about each other’s behaviour Parents fear a loss of control or influence While wanting some structure and boundaries, resent restriction on their growing freedom and ability to decide for themselves Disagreements common, part of the young person’s struggle to establish a separate identity May get to point where parents have lost control Do parents know where their children are? School Problems Refusal to go to school – difficulties separating Children who truant from school Emotional problems often affect school work Pressure to do well may come from parents or teache5rs, but usually adolescent themselves want to do well and push themselves Excessive nagging can be counter-productive Eating Problems Being fat is a common cause of unhappiness Often made fun of, become depressed and grow to dislike themselves Many adolescents diet, particularly girls Very few develop serious eating disorders Anorexia or Bulimia More likely in those who take up serious dieting, have low self-esteem, are under stress and have been over-weight as a child Drugs, Solvents and Alcohol Most teenagers never use drugs or inhale solvents Most that do never go beyond experimenting Alcohol that drug that causes the most problems When serious, sudden changes in behaviour ?possibility of drug use How to Cope Anxiety experienced by parents is more than matched by the periods of uncertainty, turmoil and unhappiness experienced by the adolescent Most difficulties not serious or long-term Parents continue to play a crucial role Provide a Secure Base The need for rules Adults – a source of advice, sympathy and comfort Don’t expect gratitude Sources of help Suicide and Metal Illness 90% of those who end their lives by suicide are suffering from mental illness, most commonly depression Alcohol is an increasingly important factor Precipitating Factors Inter-personal argument in preceding 72 hours Bereavement, Break-up or relationship etc Cultural issues Suicide and education Recognising and Responding to Suicidal Behaviour The expression of suicidal thoughts or intentions should never be ignored Most people have given warning signs Temporary nature of suicidal ideation, especially in the young Impulsivity is a central feature of adolescent suicidal behaviour – Access to methods Commonest way of recognising – the individual disclosing his distress or intention How to enquire about suicide Ability to listen, and elicit such thoughts Time and sympathy are essential Questions about the future can elicit hidden self-destructive impulses Expressions of failure or hopelessness Person says there is no future, death the only solution If person has considered methods or made plans, a serious situation Depression in Childhood and Adolescence Uses of the term “Depression” o A mood – Sad and miserable o Syndrome – clustering of moods and types of behaviour (6-8% of 12 to 16 year olds o Disorder – Handicapping, particular symptoms, characteristic course an response to treatment (1-2% of 12 to 16 year olds) Definition Individual suffers from depressed mood, loss of interest and enjoyment, reduced energy (duration of 2 weeks) Other common symptoms include o Reduced concentration and attention o Reduced self-esteem and self-confidence o Ideas of guild and unworthiness o Bleak and pessimistic view of the future o Ideas or acts of elf-harm or suicide o Disturbed sleep o Weight loss or gain Causation-risk factors Personal factors in the child Temperament, educational difficulties, chronic physical condition, genetic Family factors Parental mental illness, marital disharmony, tense atmosphere in the home, child-rearing practices, abuse, social circumstances Outside the family E.g. bullying at school TRIGGERING FACTOR Treatment Psychological Supportive therapy Cognitive-behavioural therapy Family therapy Biological Anti-depressants