One -time surgery for SUI and pelvic organ prolapse (POP)
advertisement
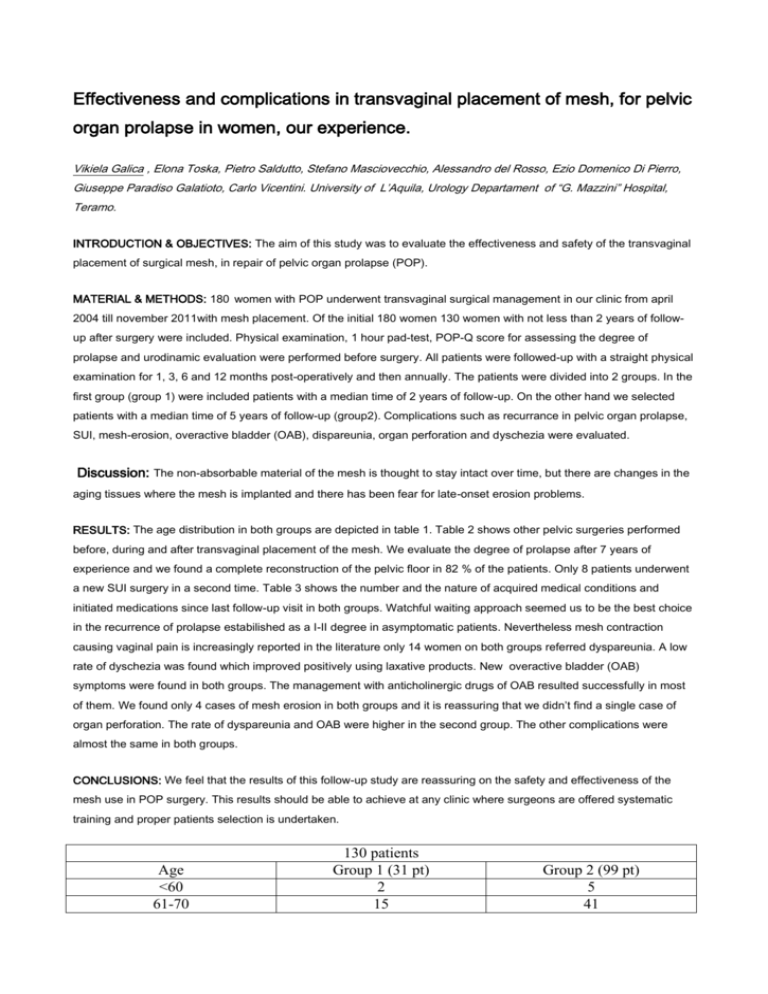
Effectiveness and complications in transvaginal placement of mesh, for pelvic organ prolapse in women, our experience. Vikiela Galica , Elona Toska, Pietro Saldutto, Stefano Masciovecchio, Alessandro del Rosso, Ezio Domenico Di Pierro, Giuseppe Paradiso Galatioto, Carlo Vicentini. University of L’Aquila, Urology Departament of “G. Mazzini” Hospital, Teramo. INTRODUCTION & OBJECTIVES: The aim of this study was to evaluate the effectiveness and safety of the transvaginal placement of surgical mesh, in repair of pelvic organ prolapse (POP). MATERIAL & METHODS: 180 women with POP underwent transvaginal surgical management in our clinic from april 2004 till november 2011with mesh placement. Of the initial 180 women 130 women with not less than 2 years of followup after surgery were included. Physical examination, 1 hour pad-test, POP-Q score for assessing the degree of prolapse and urodinamic evaluation were performed before surgery. All patients were followed-up with a straight physical examination for 1, 3, 6 and 12 months post-operatively and then annually. The patients were divided into 2 groups. In the first group (group 1) were included patients with a median time of 2 years of follow-up. On the other hand we selected patients with a median time of 5 years of follow-up (group2). Complications such as recurrance in pelvic organ prolapse, SUI, mesh-erosion, overactive bladder (OAB), dispareunia, organ perforation and dyschezia were evaluated. Discussion: The non-absorbable material of the mesh is thought to stay intact over time, but there are changes in the aging tissues where the mesh is implanted and there has been fear for late-onset erosion problems. RESULTS: The age distribution in both groups are depicted in table 1. Table 2 shows other pelvic surgeries performed before, during and after transvaginal placement of the mesh. We evaluate the degree of prolapse after 7 years of experience and we found a complete reconstruction of the pelvic floor in 82 % of the patients. Only 8 patients underwent a new SUI surgery in a second time. Table 3 shows the number and the nature of acquired medical conditions and initiated medications since last follow-up visit in both groups. Watchful waiting approach seemed us to be the best choice in the recurrence of prolapse estabilished as a I-II degree in asymptomatic patients. Nevertheless mesh contraction causing vaginal pain is increasingly reported in the literature only 14 women on both groups referred dyspareunia. A low rate of dyschezia was found which improved positively using laxative products. New overactive bladder (OAB) symptoms were found in both groups. The management with anticholinergic drugs of OAB resulted successfully in most of them. We found only 4 cases of mesh erosion in both groups and it is reassuring that we didn’t find a single case of organ perforation. The rate of dyspareunia and OAB were higher in the second group. The other complications were almost the same in both groups. CONCLUSIONS: We feel that the results of this follow-up study are reassuring on the safety and effectiveness of the mesh use in POP surgery. This results should be able to achieve at any clinic where surgeons are offered systematic training and proper patients selection is undertaken. Age <60 61-70 130 patients Group 1 (31 pt) 2 15 Group 2 (99 pt) 5 41 71-80 81-90 Type of surgery 12 1 Table 1. Group 1 Previous 9 Hysterectomy Concomitant 4 Secondly 2 Perioneoplasty Concomitant 14 SUI surgery Secondly 2 New surgery for 2 Recurrent prolapse prolapse Waiting 4 Table 2. Type of surgery improved in both groups of patients. 47 6 Group 2 38 28 2 28 6 6 19 130 patients Group 1 No pt (%) Group 2 No pt (%) Treatment SUI 5 (5%) 1 (3%) Waiting OAB 12 (!2%) 2 (6%) anticholinergic Prolapse actually 19 (19%) 4 (12%) Watchful waiting Dyschezia 4 (4%) 1 (3%) Laxative therapy Dyspareunia 12 (12%) 2 (6%) Pelvic rehabilitation Erosion 3 (3%) 1 (3%) Estrogen local therapy Organ perforation 0 0 Table 3. Follow-up data after last visit and medical treatment improved.