Post-Surgical Health Post Surgical Health Care Expenditures and p
advertisement
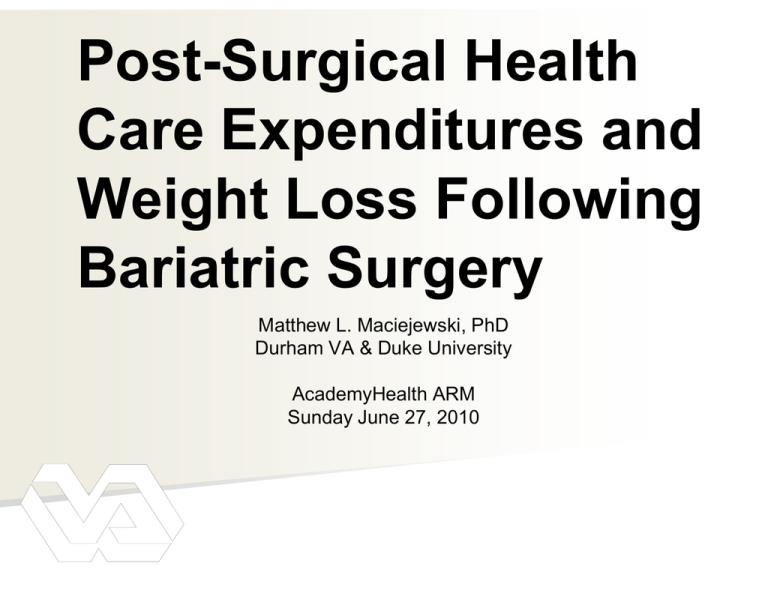
Post Surgical Health Post-Surgical Care Expenditures p and Weight g Loss Following g Bariatric Surgery g y Matthew L. Maciejewski, PhD Durham VA & Duke University AcademyHealth ARM Sunday June 27, 2010 Acknowledgements g Collaborators Maren Olsen, Leila Kahwati, Valerie Smith, Andrew Kavee: VA David Arterburn: Group Health Cooperative William Henderson: University of Colorado Edward Livingston: UT-Southwestern Funding F di VA HSR&D Bariatric Surgery Evidence Base for Bariatric Surgery •Most effective treatment for weight loss, comorbidity reduction, reduction and improved QoL •Low mortality (30-day: 0.28%, 1 yr: 1%) Bariatric surgery increased in 10 years •Medicare M di covered d starting t ti in i 2005 Increasing Surgical Volume Davis, Slish, 2006; Encinosa, Bernard, 2005; Santry, Gillen, Lauderdale, 2005; Thomson, 2007 What We Know and Current Research Question •From prior work, we found… •Mortality rate at one year: 3.4% (Arch Surg 2009) •Higher if BMI≥ 50 or greater overall disease burden •Post-surgical discontinuation rates of lipid-lowering (40%) & diabetes Rx (52%) at 1 yr (under review) •Research Question •Examine a e whether e e p pre-surgical e su g ca and a d post-surgical pos su g ca health ea ca care eu utilization a o a and d expenditures differ •Examine whether post-surgical expenditures vary by weight loss Veterans Health Administration in 2009 •Largest vertically and horizontally integrated health care system in US •153 hospitals in each of the 50 states, District of Columbia and Puerto Rico •900+ outpatient clinics & 135 nursing homes •47 residential rehabilitation treatment centers •108 comprehensive home-care programs •7.9 million enrollees, 5.5 million unique users, and 60 million outpatient visits •Annual budget g of $48 billion in 2010 •Divided into 21 regional networks National Surgical Quality I Improvement t Program P (NSQIP) •VA VA Initiative I iti ti to t Monitor, M it Compare C and d p Surgical g Q Quality y Improve •Founded in 1994 •Trained surgical clinical nurses extract data on major surgical procedures using standardized protocol •Demographics Demographics, pre-op pre op comorbidities & labs •30-day post-op complications & mortality Study Design and Data •Study Design •Retrospective cohort of surgical cases from 12 VA bariatric surgical centers •Identified by CPT codes •Sensitivity: y 99.2%, Specificity: p y 99.9% •Administrative and clinical data •VA utilization/cost: OPC, PTF, HERC Average Cost •Longitudinal L it di l weight: i ht C Corporate t D Data t W Warehouse h •Covariates: Pre/post, age, gender, race, ASA, baseline BMI, smoking status, marital status, taking of diabetes or lipid-lowering Rx, DCG score Economic Outcomes Type of Care Utilization Expenditures Primary Care Visits √ Specialty Care Visits √ Mental Health Visits √ Medications 30‐dayy equivalents q √ Inpatient # admissions, LOS √ Total Outpatient √ O Overall ll √ Descriptive Statistics Demographic and Preoperative Characteristics Age Male (%) C Caucasian i (%) Non-Caucasian (%) Married (%) P i l or Never Previously N Married M i d (%) BMI Super Obese (BMI ≥ 50) (%) DCG ASA physical status classification 4 (%) Smoker within year prior to surgery (%) Laparoscopic Procedure (%) Patients with 3 pre-surgical, 3 post-surgical years of data (%) Patients with 3 pre-surgical, 2 post-surgical years of data (%) Patients with 3 pre pre-surgical, surgical, 1 post post-surgical surgical years of data (%) Patients with 2 pre-surgical, 3 post-surgical years of data (%) Patients with 2 pre-surgical, 2 post-surgical years of data (%) pre-surgical, g , 1 ppost-surgical g years y of data (%) ( ) Patients with 2 p Patients with 1 pre-surgical, 3 post-surgical years of data (%) Patients with 1 pre-surgical, 2 post-surgical years of data (%) Patients with 1 pre-surgical, 1 post-surgical years of data (%) Surgical Cases (n = 846) 51.3 (8.2) 73.0 77.5 16.3 52.5 47 3 47.3 48.5 (7.7) 35.9 0 76 (1.04) 0.76 (1 04) 7.1 13.6 24 7 24.7 61.1 15.5 3.4 14.1 1.4 0.6 3.4 0.4 0.1 Utilization Results Utilization significantly lower post-surgery Utilization significantly higher post-surgery Utilization similar pre- & post-surgery Expenditure Results Expenditures significantly lower post-surgery Expenditures significantly higher post-surgery Expenditures similar pre- & post-surgery Specification for Weight Change & Expenditures •Specification in prior analysis (6 years) Costt = f(Demog, Hlth, pre/post, time, pre*time) •Modified specification to examine impact of weight change on expenditures at one year Cost1 = f(Wgt 1, Demog, Hlth, post time) Post-Surgical Expenditures and Weight Change at 1 Year Expe enditures (u unadjusted)) $16,000 T t l OP Costs Total C t IP Costs C t T t l Costs Total C t $12 000 $12,000 $8,000 $4,000 $0 1 2 3 T til off % Weight Tertile W i ht Change Ch (1 (1stt ttertile=most til t weight i ht loss) l ) Sample = 385 Limitations •May not generalize beyond veterans in 2000-2006 seen at 12 bariatric surgery centers t •May generalize male Medicare/Medicaid cases •Non-VA •Non VA utilization & expenditures not included •Current analysis satisfies VA payer perspective •Cannot address social perspective Conclusion •No reduction in total VA expenditures three years after surgery for older male p patients •Longer term follow-up might find reductions •These results differ from prior studies •Post-surgical P t i l expenditures dit influenced i fl d by b baseline b li weight i ht and d amountt off weight i ht loss •Post-surgical expenditures at one year highest for those with greatest weight loss Questions? VA Response to Obesity Managing Overweight/Obese Veterans Everywhere ((MOVE!)) started 2005-2006 •Multidisciplinary, evidence-based, stepped-care, primary care based program for identifying & primary-care intervening with overweight and obese patients •Population-based approach to ID at risk patients by screening all PC patients using BMI •In 2007, bariatric surgery became 5th and final level of MOVE! intervention for patients who don’t success in prior less intensive levels