FRESH Tools for Effective School Health First Edition 2004 http
advertisement

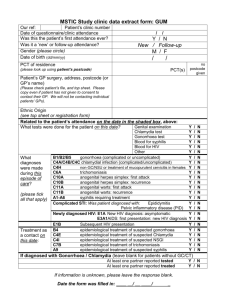
STI Facts Description of tool: The information in this tool was adapted by UNESCO Division for the Promotion of Quality Education from the following organization’s website: National Center for HIV, STD and TB Prevention, Division of Sexually Transmitted Diseases. http://www.cdc.gov/nchstp/dstd/Disease_Info.htm This information or activity supports Core Component #3 of the FRESH framework for effective school health: skills-based health education. It will have a greater impact if it is reinforced by activities in the other three components of the framework. FRESH Tools for Effective School Health http://www.fresh.org/ First Edition 2004 STI Facts1 I. Chlamydia What is chlamydia? Chlamydia is a common sexually transmitted infection (STI) caused by Chlamydia trachomatis, a bacterium, which can damage a woman's reproductive organs. Because symptoms of chlamydia are mild or absent, serious complications that cause irreversible damage, including infertility, can occur "silently" before a woman ever recognizes a problem. How do people get chlamydia? Chlamydia can be transmitted during vaginal, anal, or oral sex. Chlamydia can also be passed from an infected mother to her newborn during vaginal childbirth. How common is chlamydia? Not including HIV/AIDS, chlamydia is one of the four most common sexually transmitted infections. (The others are gonococcal infections, syphilis and trichomoniasis.) WHO estimates (1996) that 89 million people worldwide are infected with chlamydia per year. What are the symptoms of chlamydia? Chlamydia is known as a "silent" disease because three quarters of infected women and half of infected men have no symptoms. The infection is frequently not diagnosed or treated until complications develop. In women, the bacteria initially attack the cervix (opening to the uterus) and the urethra (urine canal). The few women with symptoms might have an abnormal vaginal discharge or a burning sensation when urinating. When the infection spreads from the cervix to the fallopian tubes, some women still have no signs or symptoms; others have lower abdominal pain, low back pain, nausea, fever, pain during intercourse, and bleeding between menstrual periods. Whenever the infection spreads past the cervix into the upper reproductive system, permanent and irreversible damage can occur. Men with signs or symptoms might have a discharge from the penis and a burning sensation when urinating. Men might also have burning and itching around the opening of the penis or pain and swelling in the testicles, or both. How soon after exposure do symptoms appear? If symptoms do occur, they usually appear within 1 to 3 weeks of exposure. How is chlamydia diagnosed? There are two kinds of laboratory tests to diagnose chlamydia. One involves collecting a specimen from an infected site (cervix or penis) to detect the bacterium directly. Another test that is becoming widely available can accurately detect chlamydia bacteria in a urine sample. A Pap test is not a test for chlamydia; it is a test for abnormal cervical cells. 1 Who is at risk for chlamydia? Sexually active men and women can be exposed to chlamydia bacteria during sexual contact with an infected person. The more sex partners a person has, the greater the risk of chlamydia infection. Babies are at risk of acquiring a chlamydial infection from their infected mother. Sexually active teenagers and young women are especially susceptible to chlamydia bacteria because of the characteristics of the cells that form the lining of the cervical canal. What is the treatment for chlamydia? Chlamydia can be easily treated and cured with antibiotics. A single dose of azithromycin or a week of doxycycline (twice daily) are the most commonly used treatments. All sex partners must also be treated. What complications can result from untreated chlamydia? If untreated, chlamydia infection can progress to serious reproductive and other health problems with both short-term and long-term consequences. Like the disease itself, the damage that chlamydia causes is often "silent." Untreated chlamydia in men typically causes urethral infection. Infection sometimes spreads to the epididymis (a tube that carries sperm from the testis), causing pain, fever, and, potentially, infertility. In women, the chlamydia bacteria often infect the cells of the cervix. If not treated, the infection can spread into the uterus or fallopian tubes (egg canals) and cause an infection called pelvic inflammatory disease (PID). This happens in up to 40% of women with untreated chlamydia. PID can cause permanent damage to the fallopian tubes, uterus, and tissues surrounding the ovaries. This damage can lead to chronic pelvic pain, infertility, and potentially fatal ectopic pregnancy (pregnancy outside the uterus). In pregnant women, there is some evidence that chlamydia infections can lead to premature delivery. Babies who are born when their mothers are infected can get chlamydial infections in their eyes and respiratory tracts. Chlamydia is a leading cause of early infant pneumonia and conjunctivitis (pinkeye) in newborns. Compared to women who do not have chlamydia, women infected with chlamydia may also have higher risk of acquiring HIV infection from an infected partner. Chlamydia can cause proctitis (an infection of the lining of the rectum) in persons having receptive anal intercourse. The bacterium also can be found in the throats of women and men having oral sex with an infected male partner. How can chlamydia be prevented? Safe sexual behaviour and seeking proper health care can help keep people from becoming infected or re-infected with chlamydia and from experiencing chlamydia complications. Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. 2 Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from chlamydia and other STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. However, condoms do not provide complete protection from all STIs. Sores and lesions of other STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Get a screening test for STIs. If you are young, sexually active, and do not use condoms correctly every time you have sex, you should be screened for chlamydia at least once a year. It has been shown that screening and treatment of women with chlamydia infection of the cervix reduces the likelihood of PID. All pregnant women should have a screening test for chlamydia. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Though there are often no symptoms of chlamydia, especially during the initial phase of the infection, any genital signs or symptoms such as unusual discharge, burning during urination, pain during intercourse, sores or a rash, should be a signal to stop having sex and consult a health care provider immediately. If you are told you have chlamydia, notify all your sex partners immediately. If you are told you have chlamydia or any other STI and receive drug treatment, you should notify all of your recent sex partners so that they can see a health care provider and be treated. A sex partner needs treatment even if (s)he has no symptoms. This will reduce the risk that your partners will develop serious complications from chlamydia and reduce your risk of becoming re-infected. Do not have sex until both you and your sex partner complete your chlamydia drug treatment. II. Genital Herpes What is genital herpes? Herpes is a sexually transmitted infection (STI) caused by the herpes simplex viruses type 1 (HSV -1) and type 2 (HSV-2). Most individuals have no or only minimal signs or symptoms from HSV-1 or HSV-2 infection. When signs do occur, they typically appear as one or more blisters on or around the genitals or rectum. The blisters break, leaving tender ulcers (sores) that may take two to four weeks to heal the first time they occur. Typically, another outbreak can appear weeks or months after the first, but it almost always is less severe and shorter than the first episode. Although the infection can stay in the body indefinitely, the number of outbreaks tends to go down over a period of years. How is genital herpes spread? HSV-1 and HSV-2 can be found and released from the sores that the viruses cause, but they also are released between episodes from skin that does not appear to be broken or to have a sore. A person almost always gets HSV-2 infection during sexual contact with someone who has a genital HSV-2 infection. HSV-1 causes infections of the mouth and lips, so-called 3 "fever blisters." A person can get HSV-1 by coming into contact with the saliva of an infected person. HSV-1 infection of the genitals almost always is caused by oral-genital sexual contact with a person who has the oral HSV-1 infection. How common is genital herpes? HSV-2 infection is more common in women than in men. This may be due to male-to-female transmission being more efficient than female-to-male transmission. Is genital herpes serious? HSV-2 usually produces only mild symptoms or signs or no symptoms at all. However, HSV2 can cause recurrent painful genital sores in many adults, and HSV-2 infection can be severe in people with suppressed immune systems. Regardless of severity of symptoms, genital herpes frequently causes psychological distress in people who know they are infected. In addition, HSV-2 can cause potentially fatal infections in infants if the mother is shedding virus at the time of delivery. It is important that women avoid contracting herpes during pregnancy because a first episode during pregnancy causes a greater risk of transmission to the newborn. If a woman has active genital herpes at delivery, a caesarean delivery is usually performed. HSV-2 may play an important role in the heterosexual spread of HIV, the virus that causes AIDS. Herpes can make people more susceptible to HIV infection, and it can make HIVinfected individuals more infectious. What happens when someone is infected with genital herpes? Most people infected with HSV-2 are not aware of their infection. However, if signs and symptoms occur during the first episode, they can be quite pronounced. The first episode usually occurs within two weeks after the virus is transmitted, and the sores typically heal within two to four weeks. Other signs and symptoms during the primary episode may include a second crop of sores, or flu-like symptoms, including fever and swollen glands. However, most individuals with HSV-2 infection may never have sores, or they may have very mild signs that they don't even notice or that they mistake for insect bites or a rash. Most people diagnosed with a first episode of genital herpes can expect to have several symptomatic recurrences a year (typically four or five). These recurrences usually are most noticeable within the first year following the first episode. How is genital herpes diagnosed? The signs and symptoms associated with HSV-2 can vary greatly. Health care providers can diagnose genital herpes by visual inspection if the outbreak is typical, and by taking a sample from the sore(s). HSV infections can be difficult to diagnose between outbreaks. Blood tests which detect HSV-1 or HSV-2 infection may be helpful, although the results are not always clear cut. Is there a cure for herpes? There is no treatment that can cure herpes, but antiviral medications can shorten and prevent outbreaks during the period of time the person takes the medication. 4 How can people protect themselves against infection? Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. Remember, however, that condoms do not provide complete protection from all STIs. The herpes sore(s) may be outside of the area covered by the condom, or not visible to the naked eye. In either case, viral shedding may occur and the infection may be passed from one person to another. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex and consult a health care provider immediately. If you are told you have genital herpes, notify all your sex partners immediately. If you are told you have genital herpes or any other STI and receive treatment, you should notify all of your recent sex partners so they can also see a health care provider and be evaluated for STIs. If either you or your partner have genital herpes, it is best to abstain from sex when symptoms or signs of an outbreak are present. III. Genital HPV Infection What is genital HPV infection? Genital HPV infection is a sexually transmitted infection (STI) that is caused by human papillomavirus (HPV). Human papillomavirus, or HPV, is the name of a group of viruses that includes more than 100 different strains or types. Over 30 of these are sexually transmitted, and they can infect the genital area, like the skin of the penis, vulva, labia, or anus, or the tissues covering the vagina and cervix. Some of these viruses are considered "high-risk" types and may cause abnormal Pap smears and cancer of the cervix, anus, and penis. Others are "low-risk," and they may cause mild Pap smear abnormalities and genital warts. Genital warts are single or multiple growths or bumps that appear in the genital area, and sometimes form a cauliflower-like shape. 5 How do people get genital HPV infections? The types of HPV that infect the genital area are spread primarily through sexual contact. Most HPV infections have no signs or symptoms; therefore, most infected persons are completely unaware they are infected, yet they can transmit the virus to a sex partner. Rarely, pregnant women can pass HPV to their baby during vaginal delivery. A newborn that is exposed to HPV during delivery can develop warts in the larynx (voice box). What are the signs and symptoms of genital HPV infection? Most people who have a genital HPV infection do not know they are infected. The virus lives in the skin or mucus membranes and usually causes no symptoms. Other people get visible genital warts. What are genital warts? These usually appear as soft, moist, pink or red swellings. They can be raised or flat, single or multiple, small or large. Some cluster together forming a cauliflower-like shape. They can appear on the vulva, in or around the vagina or anus, on the cervix, and on the penis, scrotum, groin, or thigh. Warts can appear within several weeks after sexual contact with an infected person, or they can take months to appear. Genital warts are diagnosed by inspection. Visible genital warts can be removed, but no treatment is better than another, and no single treatment is ideal for all cases. Who is at risk for genital HPV infection? Anyone who has sex is at risk for genital HPV infection. How is genital HPV infection diagnosed? Most women are diagnosed with HPV on the basis of abnormal Pap smears. Pap smears are the primary screening tool for cervical cancer or pre-cancerous conditions, many of which are cell changes related to HPV. Confirming HPV requires a more sophisticated and expensive test. Is there a cure for HPV? There is no "cure" for HPV, although the infection usually goes away on its own. Cancerrelated types are more likely to persist. What is the connection between HPV infection and cervical cancer? All types of HPV can cause mild Pap smear abnormalities that do not have serious consequences. Approximately 10 of the 30 identified genital HPV types can lead, in rare cases, to development of cervical cancer. Research has shown that for most (90%) women, cervical HPV infection becomes undetectable within two years; only a small proportion have persistent infection. Persistent infection with certain types of HPV is the key risk factor for cervical cancer. A Pap smear can detect pre-cancerous and cancerous cells on the cervix. Frequent Pap smears and careful medical follow-up, with treatment if necessary, can help ensure that precancerous cells in the cervix caused by HPV infection do not develop into life-threatening cervical cancer. 6 How can genital HPV infection be prevented? Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has sores or unusual growths in the genital area or the anus. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. Remember, however, that condoms do not provide complete protection from all STIs. The causative agent for many STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Get a screening test for STIs. Sexually active women should have a regular Pap smear to screen for cervical cancer or other pre-cancerous conditions. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex, and consult a health care provider immediately. If you are told you have HPV, notify all your sex partners immediately. If you are told you have HPV or any other STI and receive treatment, you should notify all of your recent sex partners so they can see a health care provider and be evaluated for STIs. Sexual activity should not resume until all sex partners have been examined and, if necessary treated. IV. Gonorrhoea What is gonorrhoea? Gonorrhoea is a common sexually transmitted infection (STI). What causes gonorrhoea? Gonorrhoea is caused by Neisseria gonorrhoeae, a bacterium that can grow and multiply easily in mucous membranes of the body. Gonorrhoea bacteria can grow in the warm, moist areas of the reproductive tract, including the cervix (opening to the womb), uterus (womb), and fallopian tubes (egg canals) in women, and in the urethra (urine canal) in women and men. The bacteria can also grow in the mouth, throat, and anus. 7 How do people get gonorrhoea? Gonorrhoea is spread through sexual contact (vaginal, oral, or anal). This includes penis-tovagina, penis-to-mouth, penis-to-anus, mouth-to-vagina, and mouth-to-anus contact. Ejaculation does not have to occur for gonorrhoea to be transmitted or acquired. Gonorrhoea can also be spread from mother to child during birth. Gonorrhoea infection can spread to other unlikely parts of the body. For example, a person can get an eye infection after touching infected genitals and then the eyes. Individuals who have had gonorrhoea and received treatment may get infected again if they have sexual contact with persons infected with gonorrhoea. How common is gonorrhoea? Gonorrhoea is a very common infectious disease. What are the signs and symptoms of gonorrhoea? When initially infected, the majority of men have some signs or symptoms. Symptoms and signs include a burning sensation when urinating and a yellowish white discharge from the penis. Sometimes men with gonorrhoea get painful or swollen testicles. In women, the early symptoms of gonorrhoea are often mild, and many women who are infected have no symptoms at all. Even when a woman has symptoms, they can be so nonspecific as to be mistaken for a bladder or vaginal infection. The initial symptoms and signs in women include a painful or burning sensation when urinating and a vaginal discharge that is yellow or occasionally bloody. Women with no or mild gonorrhoea symptoms are still at risk of developing serious complications from the infection. Untreated gonorrhoea in women can develop into pelvic inflammatory disease (PID). Symptoms of rectal infection include discharge, anal itching, soreness, bleeding, and sometimes painful bowel movements. Infections in the throat cause few symptoms. When do symptoms appear? In males, symptoms usually appear 2 to 5 days after infection, but it can take as long as 30 days for symptoms to begin. Regardless of symptoms, once a person is infected with gonorrhoea, he or she can spread the infection to others if condoms or other protective barriers are not used during sex. How is gonorrhea diagnosed? Several laboratory tests are available to diagnose gonorrhoea. A health care provider can obtain a sample of fluid from the infected mucus membrane (cervix, urethra, rectum, or throat) and send the specimen to a laboratory for analysis. Gonorrhoea that is present in the male or female genital tract can be diagnosed in a laboratory by using a urine specimen from an infected person. A quick laboratory test for gonorrhoea that can be done in the clinic or doctor’s office is a Gram stain. The Gram stain allows the doctor to see the gonorrhoea bacteria under a microscope. This test works better for men than for women. Who is at risk for gonorrhoea? Any sexually active person can be infected with gonorrhoea. 8 What is the treatment for gonorrhoea? Many of the currently used antibiotics can successfully cure gonorrhoea in adolescents and adults. Penicillin is a common antibiotic that is no longer used to treat gonorrhoea, because many strains of the gonorrhoea bacterium have become resistant to penicillin. Because many people with gonorrhoea also have chlamydia, antibiotics for both infections are usually given together. Persons with gonorrhoea should also be screened for other STIs. It is important to take all of the medication prescribed to cure gonorrhoea, even if the symptoms or signs stop before all the medication is gone. Although medication will stop the infection, it will not repair any permanent damage done by the disease. Persons who have had gonorrhoea and have been treated can also get the disease again if they have sexual contact with an infected person. What are the complications of gonorrhoea? Untreated gonorrhoea can cause serious and permanent problems in both women and men. In women, gonorrhoea is a common cause of pelvic inflammatory disease (PID). Women with PID do not necessarily have symptoms or signs. When symptoms or signs are present, they can be very severe and can include strong abdominal pain and fever. PID can lead to internal abscesses (pus pockets that are hard to cure), long-lasting pelvic pain, and infertility. PID can cause infertility or damage the fallopian tubes (egg canals) enough to increase the risk of ectopic pregnancy. Ectopic pregnancy is a life-threatening condition in which a fertilized egg grows outside the uterus, usually in a fallopian tube. In men, gonorrhoea can cause epididymitis, a painful condition of the testicles that can lead to infertility if left untreated. Without prompt treatment, gonorrhoea can also affect the prostate and can lead to scarring inside the urethra, making urination difficult. Gonorrhoea can spread to the blood or joints. This condition can be life threatening. Also, persons with gonorrhoea can more easily contract HIV, the virus that causes AIDS. Persons with HIV infection and gonorrhoea are more likely than persons with HIV infection alone to transmit HIV to someone else. How does gonorrhoea affect a pregnant woman and her baby? If a pregnant woman has gonorrhoea, she may give the infection to her infant as the baby passes through the birth canal during delivery. This can cause blindness, joint infection, or a life-threatening blood infection in the baby. Treatment of gonorrhoea as soon as it is detected in pregnant women will lessen the risk of these complications. Pregnant women should consult a health care provider for appropriate medications. How can gonorrhoea be prevented? Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. 9 However, condoms do not provide complete protection from all STIs. Sores and lesions of other STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Get a screening test for STIs. Persons who are young, sexually active, and who do not use condoms correctly every time they have sex should be screened for gonorrhoea and other STIs. Screening and treatment of women with gonorrhoea or chlamydia infection of the cervix reduces the likelihood of PID. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex and consult a health care provider immediately. If you are told you have gonorrhoea, notify all your sex partners immediately. If you are told you have gonorrhoea or any other STI and receive treatment, you should notify all of your recent sex partners so they can also be evaluated by a health care provider. This will reduce the risk that your partners will develop serious complications from gonorrhoea and will reduce your own risk of becoming re-infected. Sexual activity should not resume until all sex partners have been examined and, if necessary treated. V. Syphilis What is syphilis? Syphilis is a complex sexually transmitted infection (STI) caused by the bacterium Treponema pallidum. It has often been called "the great imitator" because so many of the signs and symptoms are indistinguishable from those of other infections. How is syphilis spread? Syphilis is passed from person to person through direct contact with a syphilis sore. Sores occur mainly on the external genitals, vagina, anus, or in the rectum. Sores also can occur on the lips and in the mouth. Transmission of the organism occurs during vaginal, anal, or oral sex. Pregnant women can pass the infection to the babies they are carrying. Syphilis cannot be spread by toilet seats, door knobs, swimming pools, hot tubs, bath tubs, shared clothing, or eating utensils. Washing the genitals, urinating, or douching after sex does not prevent STIs, including syphilis. What are the signs and symptoms in adults? Primary Stage The time between infection with syphilis and the start of the first symptom can range from 10-90 days (average 21 days). The primary stage of syphilis is usually marked by 10 the appearance of a single sore (called a chancre), but there may be multiple sores. The chancre is usually firm, round, small, and painless. It appears at the spot where syphilis entered the body. The chancre lasts 3-6 weeks, and it will heal on its own. If adequate treatment is not administered, the infection progresses to the secondary stage. Secondary Stage The second stage starts when one or more areas of the skin break into a rash that usually does not itch. Rashes can appear as the chancre is fading or can be delayed for weeks. The rash often appears as rough, red or reddish brown spots both on the palms of the hands and on the bottoms of the feet. The rash also may also appear on other parts of the body with different characteristics, some of which resemble other diseases. Sometimes the rashes are so faint that they are not noticed. Even without treatment, rashes clear up on their own. In addition to rashes, second-stage symptoms can include fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches, and tiredness. A person can easily pass the infection to sex partners when primary or secondary stage signs or symptoms are present. Late Syphilis The latent (hidden) stage of syphilis begins when the secondary symptoms disappear. Without treatment, the infected person still has syphilis even though there are no signs or symptoms. It remains in the body, and it may begin to damage the internal organs, including the brain, nerves, eyes, heart, blood vessels, liver, bones, and joints. This internal damage may show up many years later in the late or tertiary stage of syphilis. Late stage signs and symptoms include not being able to coordinate muscle movements, paralysis, numbness, gradual blindness and dementia. This damage may be serious enough to cause death. Can a newborn get syphilis? Depending on how long a pregnant woman has been infected, she has a good chance of having a stillbirth (syphilitic stillbirth) or of giving birth to a baby who dies shortly after birth. If not treated immediately, an infected baby may be born without symptoms but could develop them within a few weeks. These signs and symptoms can be very serious. Untreated babies may become developmentally delayed, have seizures, or die. How is syphilis diagnosed? A health care provider can diagnose syphilis by using dark field microscopy to examine material from infectious sores. If syphilis bacteria are present in the sore, they will show up with a characteristic appearance. A blood test is another way to determine whether someone has syphilis. Shortly after infection occurs, the body produces syphilis antibodies that can be detected by an accurate, safe and inexpensive blood test. A low level of antibodies will stay in the blood for months or years even after the infection has been successfully treated. Because untreated syphilis in a pregnant woman can infect and possibly kill her developing baby, every pregnant woman should have a blood test for syphilis. How common is syphilis? Not including HIV/AIDS, syphilis is one of the four most common sexually-transmitted infections. (The others are gonococcal infections, chlamydial infections and trichomoniasis.) WHO estimates (1996) that 12 million people worldwide are infected with syphilis per year. 11 What is the link between syphilis and HIV? While the health problems caused by syphilis in adults and newborns are serious in their own right, it is now known that the genital sores caused by syphilis in adults also make it easier to transmit and acquire HIV infection sexually. There is a 2- to 5-fold increased risk of acquiring HIV infection when syphilis is present. Is there a cure for syphilis? Yes! A single dose of penicillin, an antibiotic, will cure a person who has had syphilis for less than a year. Larger doses are needed to cure someone who has had it for longer than a year. For people who are allergic to penicillin, other antibiotics are available to treat syphilis. There are no home remedies or over-the-counter drugs that will cure syphilis. Penicillin treatment will kill the syphilis bacterium and prevent further damage, but it will not repair any damage already done. Persons who receive syphilis treatment must abstain from sexual contact with new partners until the syphilis sores are completely healed. Persons with syphilis must notify their sex partners so that they also can be tested, and, if necessary, receive treatment. Will syphilis recur? Having had syphilis does not protect a person from getting it again. Antibodies are produced as a person reacts to the infection, and, after treatment, these antibodies may offer partial protection from getting infected again, if exposed right away. Even though there may be a short period of protection, the antibody levels naturally decrease in the blood, and people become susceptible to syphilis infection again if they are sexually exposed to syphilis sores. How can people protect themselves against infection? Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. However, condoms do not provide complete protection from all STIs. Sores and lesions caused by syphilis or other STIs on infected men and women may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Get a screening test for STIs. Because syphilis sores can be hidden in the vagina, rectum, or mouth, it may not be obvious that a sex partner has syphilis. Only lab tests can confirm whether someone has syphilis. 12 If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex and consult a health care provider immediately. If you are told you have syphilis, notify all your sex partners immediately. If you are told you have syphilis or any other STI and receive treatment, you should notify all of your recent sex partners so they can also be evaluated by a health care provider. Sexual activity should not resume until all sex partners have been examined and, if necessary treated. VI. Bacterial Vaginosis (BV) What is bacterial vaginosis? Bacterial vaginosis (BV) is the most common vaginal infection in women of childbearing age, and it is sometimes accompanied by discharge, odour, pain, itching, or burning. What causes bacterial vaginosis? The cause of BV is not fully understood. BV is associated with an imbalance in the bacteria that are normally found in a woman's vagina. The vagina normally contains mostly "good" bacteria, and fewer "harmful" bacteria. BV develops when there is a change in the environment of the vagina that causes an increase in harmful bacteria. How do women get bacterial vaginosis? Not much is known about how women get BV. Women who have a new sex partner or who have had multiple sex partners are more likely to develop BV. Women who have never had sexual intercourse are rarely affected. It is not clear what role sexual activity plays in the development of BV, and there are many unanswered questions about the role that harmful bacteria play in causing BV. Women do not get BV from toilet seats, bedding, swimming pools, or from touching objects around them. How common is bacterial vaginosis? Scientific studies suggest that BV is common in women of reproductive age. What are the signs and symptoms of bacterial vaginosis? Women with BV often have an abnormal vaginal discharge with an unpleasant odour. Some women report a strong fish-like odour, especially after intercourse. The discharge is usually white or grey; it can be thin. Women with BV may also have burning during urination or itching around the outside of the vagina, or both. Some women with BV report no signs or symptoms at all. How is bacterial vaginosis diagnosed? A health care provider must examine the vagina for signs of BV (e.g., discharge) and perform laboratory tests on a sample of vaginal fluid to look for bacteria associated with BV. 13 Who is at risk for bacterial vaginosis? Any woman can get BV. However, some activities or behaviours can upset the normal balance of bacteria in the vagina and put women at increased risk: Having a new sex partner or multiple sex partners Douching Using an intrauterine device (IUD) for contraception. Pregnant women are at increased risk for complications of BV. What are the complications of bacterial vaginosis? In most cases, BV causes no complications. But there are some serious risks from BV: Pregnant women with BV more often have babies who are born early or with low birth weight. The bacteria that cause BV can sometimes infect the uterus (womb) and fallopian tubes (egg canals). This type of infection is called pelvic inflammatory disease (PID). PID can cause infertility or damage the fallopian tubes enough to increase the future risk of ectopic pregnancy and infertility. Ectopic pregnancy is a life-threatening condition in which a fertilized egg grows outside the uterus, usually in a fallopian tube. BV can increase a woman's susceptibility to HIV infection if she is exposed to the virus. Having BV increases the chances that an HIV-infected woman can pass HIV to her sex partner. BV can increase a woman's susceptibility to other STIs, such as chlamydia and gonorrhoea. Who should be treated for bacterial vaginosis? Although BV will sometimes clear up without treatment, all women with symptoms of BV should be treated to avoid such complications as PID. Treatment is especially important for pregnant women. All pregnant women, regardless of symptoms, who have ever had a premature delivery or low birth weight baby should be considered for a BV examination and be treated when necessary. All pregnant women who have symptoms of BV should be checked and treated. Male partners generally do not need to be treated. However, BV may spread between female sex partners. What is the treatment for bacterial vaginosis? BV is treatable with anti-microbial medicines prescribed by a health care provider. Two different medicines are recommended as treatment for BV: metronidazole or clindamycin. Either can be used with non-pregnant or with pregnant women, but the recommended dosages differ. Women with BV who are HIV-positive should receive the same treatment as those who are HIV-negative. BV can recur after treatment. How can bacterial vaginosis be prevented? BV is not completely understood by scientists, and the best ways to prevent it are unknown. However, enough is known to show that BV is associated with having a new sex partner or having multiple sex partners. It is seldom found in women who have never had intercourse. Some basic prevention steps can help reduce the risk of upsetting the natural balance in the vagina and developing BV: Limit the number of sex partners, and do not go back and forth between partners. 14 Practice sexual abstinence, or limit sexual contact to one partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from BV and other STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. However, condoms do not provide complete protection from all STIs. Sores and lesions of other STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Do not douche. If you think you are infected, avoid sexual contact, and see a health care provider immediately. Any unusual discharge, sore, or rash, especially in the genital area, should be a signal to stop having sex and consult a health care provider immediately. Use all of the medicine prescribed for treatment of BV, even if the signs and symptoms go away. VII. Trichomoniasis What is trichomoniasis? Trichomoniasis is a common sexually transmitted infection (STI) that affects both women and men, although symptoms are more common in women. What causes trichomoniasis? Trichomoniasis is caused by the single-celled protozoan parasite Trichomonas vaginalis. The vagina is the most common site of infection in women, and the urethra is the most common site of infection in men. How do people get trichomoniasis? Trichomoniasis is a sexually transmitted infection that is spread through penis-to-vagina intercourse or vulva-to-vulva contact with an infected partner. Women can acquire the disease from infected men or women, whereas men usually contract it only from infected women. How common is trichomoniasis? Not including HIV/AIDS, trichomoniasis is the most common curable STI in the world today. WHO estimates (1996) that 170 million people worldwide are infected with trichomoniasis per year. 15 What are the signs and symptoms of trichomoniasis? Most men with trichomoniasis do not have signs or symptoms. Men with symptoms may have an irritation inside the penis, mild discharge, or slight burning after urination or ejaculation. Many women do have signs or symptoms of infection. In these women, trichomoniasis causes a frothy, yellow-green vaginal discharge with a strong odour. The infection may also cause discomfort during intercourse and urination. Irritation and itching of the female genital area and, in rare cases, lower abdominal pain can also occur. When do symptoms appear? Symptoms usually appear within 5 to 28 days of exposure in women. What are the complications of trichomoniasis? Trichomoniasis in pregnant women may cause premature rupture of the membranes and pre-term delivery. The genital inflammation caused by trichomoniasis might also increase a woman's risk of acquiring HIV infection if she is exposed to HIV. Trichomoniasis in a woman who is also infected with HIV can increase the chances of transmitting HIV infection to a sex partner. How is trichomoniasis diagnosed? To diagnose trichomoniasis, a health care provider must perform a physical examination and laboratory test. In women, a pelvic examination can reveal small red ulcerations on the vaginal wall or cervix. Laboratory tests are performed on a sample of vaginal fluid or urethral fluid to look for the disease-causing parasite. The parasite is harder to detect in men than in women. Who is at risk for trichomoniasis? Any sexually active person can be infected with trichomoniasis. What is the treatment for trichomoniasis? Trichomoniasis can usually be cured with the prescription drug metronidazole given by mouth in a single dose. The symptoms of trichomoniasis in infected men may disappear within a few weeks without treatment. However, an infected man, even a man who has never had symptoms or whose symptoms have stopped, can continue to infect a female partner until he has been treated. Therefore, both partners should be treated at the same time to eliminate the parasite. Persons being treated for trichomoniasis should avoid sex until they and their sex partners complete treatment and have no symptoms. Metronidazole can be used by pregnant women. How can trichomoniasis be prevented? Limit the number of sex partners, and do not go back and forth between partners. Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting 16 sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. However, condoms do not provide complete protection from all STIs. Sores and lesions caused by other STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex and consult a health care provider immediately. If you are told you have trichomoniasis, notify all your sex partners immediately. If you are told you have trichomoniasis or any other STI and receive treatment, you should notify all of your recent sex partners so they can also be evaluated by a health care provider. Sexual activity should not resume until all sex partners have been examined and, if necessary treated. VIII. Pelvic Inflammatory Disease (PID) What is PID? Pelvic inflammatory disease (PID) is a general term that refers to infection of the fallopian tubes (tubes that carry eggs from the ovary to the womb) and of other internal reproductive organs in women. It is a common and serious complication of some sexually transmitted infections (STIs). Inside the lower abdominal cavity, PID can damage the fallopian tubes and tissues in and near the uterus and ovaries. Untreated PID can lead to serious consequences including infertility, ectopic pregnancy, abscess formation, and chronic pelvic pain. How common is PID? Each year in the United States, more than 1 million women experience an episode of acute PID. More than 100,000 women become infertile each year as a result of PID, and a large proportion of the ectopic pregnancies occurring every year are due to the consequences of PID. More than 150 women die from this infection every year. What causes PID? PID occurs when bacteria move upward from a woman's vagina or cervix into the internal reproductive organs. Sexually active women in their childbearing years are most at risk. Many different organisms can cause PID, but most cases are associated with gonorrhoea and chlamydia, two very common bacterial STIs. It is estimated that 10% to 80% of women with either of these STIs will develop symptomatic PID. 17 What are the symptoms of PID? Symptoms of PID vary from none to severe. Particularly when it is caused by chlamydial infection, PID may produce only mild symptoms or no symptoms at all, even while it is seriously damaging the internal reproductive organs. Because of the vague symptoms, PID goes unrecognized both by women and by their health care providers about two thirds of the time. Women who do have symptoms of PID most commonly have lower abdominal pain. Other signs and symptoms include fever, unusual vaginal discharge that may have a foul odour, painful intercourse, painful urination, irregular menstrual bleeding, and pain in the right upper abdomen (rare). What are the complications of PID? Early and complete treatment can help prevent complications of PID. Without treatment, PID can cause permanent damage to the female internal reproductive organs. Infection-causing bacteria can silently invade the fallopian tubes, causing normal tissue to turn into scar tissue. Scar tissue blocks or interrupts the normal movement of eggs into the uterus. If the fallopian tubes are totally blocked by scar tissue, an egg will not be fertilized by sperm or move to the uterus to develop into a baby. Totally blocked fallopian tubes cause a woman to be infertile. Infertility can also occur if the fallopian tubes are partially blocked or even slightly damaged. About one in five women with PID become infertile. If a woman has multiple episodes of PID, her chances of becoming infertile are increased. In addition, a partially blocked or slightly damaged fallopian tube may cause a fertilized egg to get stuck in the tube. This fertilized egg may begin to grow in the tube as if it were in the womb. This is an ectopic pregnancy, which is a pregnancy in the fallopian tube or elsewhere outside the uterus. As it grows, an ectopic pregnancy can rupture the fallopian tube and cause severe pain, internal bleeding, and even death. Scarring in the fallopian tubes and other pelvic structures can also cause chronic pelvic pain (pain that lasts for months or even years). Women with repeated episodes of PID are more likely than women with a single episode to suffer infertility, ectopic pregnancy, or chronic pelvic pain. How is PID diagnosed? PID is difficult to diagnose because the symptoms are often subtle and mild. Many episodes of PID go undetected because the woman or her health care provider fails to recognize the implications of mild or non-specific symptoms. Because there are no precise tests for PID, a diagnosis is usually based on clinical findings. If symptoms such as lower abdominal pain are present, a health care provider should perform a physical examination to determine the nature and location of the pain and check for fever, abnormal vaginal or cervical discharge, and for evidence of gonorrhoea or chlamydia infection. If the findings suggest PID, treatment is necessary. If more information is necessary, the health care provider may order other tests to identify the infection-causing organism or to distinguish between PID and other problems with similar symptoms. A pelvic ultrasound is a procedure that may be helpful in evaluating someone for PID. An ultrasound can view the pelvic area to see whether the fallopian tubes are enlarged or whether an abscess is present. In some cases, a laparoscopy may be necessary to confirm the diagnosis. A laparoscopy is a minor surgical procedure in which a thin, flexible tube with a lighted end (laparoscope) is inserted through a small incision in the lower abdomen. This procedure enables the doctor to view the internal pelvic organs and to take specimens for laboratory studies, if needed. 18 What is the treatment for PID? PID can be cured with antibiotics. If women have pelvic pain and other symptoms caused by PID, it is critical that they seek care immediately. Prompt antibiotic treatment can prevent severe damage to pelvic organs. The longer women delay treatment for PID, the more likely they are to be infertile or to have an ectopic pregnancy in the future because of damage to the tubes. However, antibiotic treatment does not reverse any damage that has already occurred to the reproductive organs. Because of the difficulty in identifying organisms infecting the internal reproductive organs and because more than one organism may be responsible for an episode of PID, PID is usually treated with at least two antibiotics that are effective against a wide range of infectious agents. These antibiotics can be given by mouth or by vein. The symptoms may go away before the infection is cured. Even if symptoms do go away, women should finish taking all of the medicine. This will help prevent the infection from returning. Women on treatment for PID should be re-evaluated by their health care provider two to three days after starting treatment to be sure the antibiotics are working to cure the infection. In addition, women's sex partners should be treated to decrease the risk of re-infection, even if the partners have no symptoms. Many women with PID have sex partners who have no symptoms, although their sex partners may be infected with the organisms that can cause PID. About one fourth of women with suspected PID must be hospitalized. Hospitalization may be recommended if the woman is severely ill (e.g., high fever) or pregnant; if she cannot take oral medication and needs intravenous antibiotics; if the diagnosis is uncertain; or in some cases, if she is infected with HIV (human immunodeficiency virus, the virus that causes AIDS). If symptoms continue or if an abscess does not resolve, surgery may be needed. Complications of PID, such as chronic pelvic pain and scarring are difficult to treat but are sometimes improved with surgery. Who is at risk for PID? Women with STIs--especially gonorrhoea and chlamydia--are at increased risk for developing PID. A prior episode of PID increases the risk of another episode because the body's defences are often damaged during the initial bout of infection. Sexually active women under age 25 are more likely to develop PID than are women older than 25. The more sex partners a woman has, the greater her risk of developing PID. Also, a woman whose partner has more than one sex partner is at greater risk of getting PID, because of the potential for more exposures to infectious agents. Women who douche have a higher risk of developing PID compared with women who do not. Women who have an intrauterine device (IUD) inserted may have a slightly increased risk of PID compared with women using other contraceptives or no contraceptive at all. However, this risk is greatly reduced in women being screened and treated for any infections before an IUD is inserted. In addition, mutual monogamy is encouraged for women who choose to use this form of contraception to decrease the risk of getting PID. How can PID be prevented? The main cause of PID is an untreated STI. Women can protect themselves from PID by taking action to prevent STIs or by getting early treatment if they do get an STI: Limit the number of sex partners, and do not go back and forth between partners. 19 Practice sexual abstinence, or limit sexual contact to one uninfected partner. Do not have sex with anyone who has genital sores. Use condoms correctly every time with every sex act. Persons who engage in sexual behaviours that can place them at risk for STIs should use latex condoms every time they have sex. A condom put on the penis before starting sex and worn until the penis is withdrawn can help protect both the male and the female partner from STIs. When a male condom cannot be used appropriately, sex partners should consider using a female condom. However, condoms do not provide complete protection from all STIs. Sores and lesions caused by various STIs may be present in areas not covered by the condom, and transmission of the infection to a new person may thus still occur. Common methods of birth control such as the oral contraceptive pill or the contraceptive shot or implant do not give women protection from STIs. Women who use these methods should also use condoms every time they have sex to prevent STIs. Get a screening test for STIs. Persons who are young, sexually active, and who do not use condoms correctly every time they have sex should be screened for STIs. Screening and treatment of women with chlamydia or gonorrhoea infection of the cervix reduces the likelihood of PID. If you think you have an STI, avoid sexual contact, and see a health care provider immediately. Any genital symptoms such as an unusual sore, rash, discharge with odour, burning during urination, or bleeding between cycles could mean infection with an STI. If you have any of these symptoms, stop having sex and consult a health care provider immediately. Treating STIs early can prevent PID. If you are told you have an STI, notify all your sex partners immediately. If you are told you have an STI and receive treatment, you should notify all of your recent sex partners so they can also be evaluated by a health care provider. Sexual activity should not resume until all sex partners have been examined and, if necessary treated. 1 Adapted from: National Center for HIV, STD and TB Prevention, Division of Sexually Transmitted Diseases. http://www.cdc.gov/nchstp/dstd/Disease_Info.htm 20