About The Center for Living Donation at the Recanati /Miller
advertisement

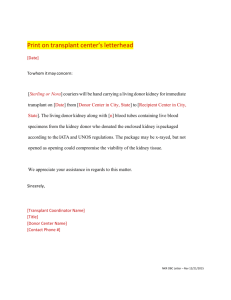
Living Donor Kidney Transplant at Mount Sinai Medical Center What Every Living Donor Needs to Know! The Center for Living Donations • One Gustave Levy Place • Box 1104 • New York, NY • 10029 • 212-659-8351 1 About The Center for Living Donation at the Recanati /Miller Transplant Institute (RMTI) Mount Sinai Medical Center is known internationally for its innovation in research, education and clinical care. The RMTI at Mount Sinai Medical Center is one of the nation’s leading academic transplant centers providing comprehensive care to those with end stage organ failure. Our transplant program began in 1967, as one of the first transplant programs in the northeast. We have performed pancreas transplant since 1994 and performed our first laparoscopic kidney transplant in 1996. Our clinical expertise in care of patients with end stage renal disease and with kidney transplantation is insurmountable. RMTI researchers are working independently and collaboratively to improve organ preservation, reduce rejection, minimize surgical complications and improve long term survival of transplant recipients. Calling on our many years of experience, we continue to provide lifelong partnerships with our patients, their families and referring physicians. Our mission is to provide exemplarity medical and surgical care in a compassionate and individualized setting, a hallmark of the RMTI. In 2010, The RMTI created The Center for Living Donation. The focus is solely to provide quality care to living organ donors pre and post donation in a patient friendly environment. This innovative center is the first of its kind providing expertise in the medical, surgical and psychological health to people considering living donation and to those who have donated the gift of life. Our Mission: To provide quality health care to potential and actual live organ donors in an environment focused on wellness through the latest medical advances, comprehensive evaluation, support and education, before, during and after donation. 2 Revised August 2011| Mount Sinai Medical Center Donating one of your kidneys to another person can be a priceless gift, but it must not be undertaken without serious thought. We recommend you begin the evaluation with an open mind and listen carefully to all the members of the living donor team, read this guidebook and research being a living donor carefully. Discuss live donation with people close to you as well. This is a completely voluntary procedure and at no point should you feel coerced or obligated to undergo surgery. Living donation will not provide any benefit to you except the knowledge that you have tried to save a life. Occasionally the evaluation process may uncover an illness that you may not have known about. The most significant benefit to the recipient is that they will live longer with a functioning kidney than being on dialysis. Additionally, he or she can be transplanted in a controlled situation prior to the development of life threatening complications of end stage renal disease. The outcome of the living donor kidney transplant is not guaranteed. Its benefit is the timing of the operation, which is likely significantly sooner than waiting for a deceased donor. Living Donor Team The living donor team that will perform a comprehensive evaluation is called the DAT (Donor Advocate Team) The living donor team is comprised of many people who will evaluate and educate you about the process. They include: · · · · · · · Nephrologist Registered Nurse or Nurse Practitioner Independent Donor Advocate Social Worker Financial Coordinator Nutritionist Live Donor Program Administrative Assistants Donor surgeon Many members of the DAT team are part of the RMTI transplant institute, but do not care for transplant recipients. Some members such as the independent donor advocate social worker are employed by the hospital and primary role is to evaluate and advocate for you. You may speak to your advocate about any and all concerns at any point during or after your evaluation. None of our team members receive financial gain from participating in the DAT. 3 At times you may feel overwhelmed with the information you are receiving from the team members, or you may get tired of repeating your story multiple times but each member plays a critical role in the evaluation process and has important information for you to consider prior to making your decision about donation. How to Start the Process: 1. 2. Telephone screening is performed by a member of the DAT and a “Potential Living Donor Health Questionnaire” is completed and reviewed by the transplant coordinator Potential Donors are encouraged to attend an educational class on live kidney donation 3. Donor criteria for living kidney donation includes: a. Compatible blood type or compatible paired exchange b. Body Mass Index < 35 c. Age 18 or greater d. Absence of chronic illness that could be affected by removal of kidney e. Absence of uncontrolled high blood pressure f. Absence of diabetes g. Absence of infectious disease or cancer h. Absence of family history of genetic kidney disease i. Absence of severe active psychiatric disorders j. Absence of current or recent history of alcohol or substance abuse k. No evidence of coercion or payment 4. An interested potential living donor without obvious contraindications to donation will sign consent to begin evaluation and be scheduled for a comprehensive donor evaluation by the DAT team. The Donor Evaluation: The comprehensive donor evaluation consists of: Donor education class Blood type, HLA typing and cross match to recipient Comprehensive laboratory examination Urinalysis 24 hour urine for protein and creatinine 4 Revised August 2011| Mount Sinai Medical Center Electrocardiogram Chest x-ray Psychosocial assessment by a social worker Kidney ultrasound MRA of abdomen with IV contrast Cardiac stress test and echocardiography (recommended over the age of 50) All women should have a Pap smear within 3 years prior to donating Women over the age of 40 should have a mammogram 2 hours oral glucose tolerance test (recommended for BMI over 30 or strong family history of diabetes) Additional tests will be ordered based on the donor’s age and past medical history. Depending on your age you will need cancer screening based on Cancer Screening Protocols as per American Cancer Society Guidelines based on age and sex (many can be done locally) Compatibility Below is a table of what blood types are compatible. Positive and negative are not important for the consideration of kidney donation. Recipient Donor A A or O B B or O AB A or B or O or AB O O Kidney Paired Exchange Program Kidney paired donation is a system that matches live kidney donors who are not compatible with another pair that is compatible. For instance a donor whose blood type is B cannot donate to his family who is A but then exchanges a kidney with a family whose donor is A and recipient is B. (see Figure) This can be done with two pairs or with large chains of donors who are matched through a computer system. 5 Being Informed To Make the Right Decision for YOU You will be asked to give consent on multiple occasions. The first time is when you begin the evaluation and finally when you ultimately decide to undergo surgery. It is the role of the donor team to make sure that all potential donors are fully informed of the risks involved and given ample time to make the right decision for themselves. Listen carefully to the donor team and their description of the surgery, recovery and risks involved. Take the opportunity to attend the educational workshops available and speak with someone who has gone through the process. Knowledge is power and will help you regardless of your decision. All donors must be: · · · · · Competent Willing to donate Free of coercion Medically and psychosocially stable Fully informed of the risks, benefits and alternatives to living donation To ensure that you completely understand the process and risk, the transplant center will present its experience and program statistics so that you can make an informed choice about donation at this center. Payment for Organs is Illegal The sale or purchase of human organs is a federal crime and it is unlawful for any person to knowingly acquire, receive or otherwise transfer any human organ for valuable consideration for use in human transplantation. 6 Revised August 2011| Mount Sinai Medical Center Additionally, if any money was given or will be given in exchange for an organ, that person may be subject to criminal prosecution; any insurance coverage may no longer apply and the donor will become personally responsible for all the health care costs associated with the donation, and that persons private health information will be available to law enforcement agencies. The Donor Operation The standard surgical procedure to remove your kidney is called a Laparoscopic Donor Nephrectomy. The decision of which kidney to remove will be based on the size and other anatomical considerations addressed by our multidisciplinary team. Before the surgery you will be medicated with general anesthesia, the surgeon will place two to four small holes in your abdomen for a camera and surgical instruments, and one incision will be made to remove your kidney. The surgeon may use that same incision to introduce one hand during the procedure. The abdomen will then be stitched closed. A small tube will be inserted into a vein for fluids and medications and a urinary tube will be inserted in the bladder after the surgery to measure the urine output. The typical hospital stay is 2 days. Currently, the surgical team at RMTI is offering a modified surgical approach by performing all of the surgeries laparoscopically. This approach will shorten the healing time and reduce the time you will need to be hospitalized. We encourage you to discuss this with your surgeon at the time of your surgical evaluation. The Scar: The scar from a laparoscopic donor nephrectomy consists of two to four small scars where the ports were inserted and a small incision to remove the kidney 7 The Recovery A donor is typically hospitalized for 1-2- days after the nephrectomy and is unable to return to work for 2-4 weeks. The first day after surgery you will be very sore, nauseated, and slightly groggy. You may experience pain and some nausea as you are switched from IV to oral pain medication and encouraged to walk a little. You should take the medication at least twice a day. Now is not the time to be tough, you need this medication. By the time you go home from the hospital you start to feel yourself again. You are allowed to eat and your bowel function will start to return. Following discharge, you will be given a prescription for oral pain medicine to take as needed, and you can expect to be moderately fatigued for several weeks. You must not lift greater that 20 lbs. for 4 weeks. Otherwise, you are encouraged to slowly resume normal activity at your own pace, making sure that you walk daily and stay active. Most donors will be out of work for a few weeks but not feel 100% normal for up to 3-4 months. Once you return home, if you develop a fever or have drainage from your incision you should call the transplant office and speak to your nurse of doctor. You should shower daily, wash your incision with soap and water, and pat dry. You should eat a normal, healthy, well-rounded diet to improve healing. The transplant center will follow you closely as you recuperate. You will be seen two weeks after discharge to assess your condition and check your blood tests. Additionally, at 6 weeks, six months, one year and annually for 2-5 years we ask that you return to see us for a checkup. The United Network for Organ Sharing(UNOS) requires that we follow you for two years. The transplant team strongly encourages you to comply with follow up recommendations. If you feel ill and need additional follow up, you are encouraged to call the center. 8 Revised August 2011| Mount Sinai Medical Center It is also important for you to keep your primary care physician aware of your progress and see him or her annually for a check up as well. You should provide the donor team the information about your primary care physician so that we may send your reports to your doctor so he or she is fully informed of your care. Risk of Live Kidney Donation Removing a kidney from a healthy person involves risk. The risk of being a living kidney donor comes from studies of previous donors at individual transplant programs and from follow-up reports that centers send to UNOS. Transplant centers must immediately report adverse outcomes and the deaths of any living donors to UNOS. Based on currently available information the short-term risks are relatively low, and can include: Risks associated with anesthesia. Conversion from laparoscopic to open surgery (less than 1% of cases). The most common complication is typically and ileus in which your stomach is slow to awaken from anesthesia and you experience abdominal distension and bloating limiting dietary intake in 4% of patients. Surgical complications such as pain, infection, blood loss, blood clots and the need for a blood transfusion. Although very rare, blood transfusions might carry the risk for the Human Immunodeficiency Virus (HIV), Hepatitis C Virus infection. Death- the risk of dying from living donor surgery is 0.04% (1 death for every 2,500 living donors). As with any surgery there can be unknown risks associated with the surgical procedure. Currently, information on long-term health and psychological outcomes of living donors shows: The lifetime risk of end stage kidney disease and the lifetime need for dialysis or to receive a kidney transplant is between 1 per 1000-2000 (0.1 to 0.5%) The risk may be higher if the potential donor is African American. Between January, 1996, and February, 2008 throughout the entire United States, there were 172 kidney Transplant candidates identified to be previous living kidney donors. The median time from donation to listing was 19 years. The risk for the future development of conditions that may affect kidney function is not known for each individual. It is possible that a donor may later develop diabetes, decreased kidney function, a new kidney disease or kidney stones. 9 One recent Canadian study did not find any increase in cardiovascular risk for kidney donors up to 10 years after donation. Recent studies from Canada, Norway and the University of Minnesota showed a slight increased risk (16% compared to 11%) of high blood pressure in donors. Previous kidney donors who become pregnant have an increased risk (5% compared to 2%) for preclampsia (a condition in pregnancy characterized by a sharp rise in blood pressure leakage of large amounts of the protein in to the urine) Understanding Organ Allocation in the United States Since all potential recipients of living donors are also listed with UNOS (The United Network for Organ Sharing), if for some reason living donation does not go forward the recipient will be eligible for a deceased donor. In addition if the recipients name comes up for an organ prior to the living donor surgery, deceased donation would take precedence. Organ allocation is maintained by UNOS, a nonprofit charitable organization that operates the Organ Procurement and Transplantation Network (OPTN) under federal contract. On an ongoing basis, the OPTN/UNOS continuously evaluates new advances and research and adapts these into new organ transplant policies to better serve patients awaiting transplants. To learn more about Kidney Organ allocation, read the brochure Questions and Answers for Transplant candidates about kidney transplant or go online to www.UNOS.org. Preparing to be a Donor Plan Ahead: Peace of mind during your hospital stay and recovery will be enhanced by planning ahead. It is recommended that you consider making the following advanced directives and legal arrangements: Appoint a Health Care Proxy: Did you know that it is possible to carry out your wishes for medical care even if you cannot answer for yourself? By choosing a person(s) to represent you and to act on your behalf, you will always remain in control of your medical care. Transplant Social Workers will educate you further on appointing a Health Care Proxy. We require you to complete a Health Care Proxy a requirement for surgery to take place. Without a health care proxy the medical team must turn to your next of kin. For instance, an unmarried adult’s next of kin is his or her parent. A separated patient’s next of kin is the spouse. Make a living will: A living will specifically says what procedures you want or do not want if you are not able to make your own medical decisions. 10 Revised August 2011| Mount Sinai Medical Center Appoint a Power of Attorney: Compelling business and legal matters often require patients’ attention during hospitalization and recovery. By choosing someone to conduct your affairs, you can reduce stress on you and your family. Create a Joint Bank Account: A family member who has joint access to your bank account will be able to pay bills, deposit and withdraw funds. Accommodations: Your family may be comforted by being able to stay nearby when you are hospitalized. TLC: The Transplant Living Center may be available to provide affordable housing away from home. There are also a variety of hotels nearby. A complete list of hotels can be provided to you by your Transplant Social Worker Speak to someone who has donated No one knows what it is like to be a donor except someone who has done this before. It is strongly encouraged that you speak to a prior donor so you can have first hand knowledge as to what should be expected; what questions to ask and how to really prepare yourself for the surgery. The Donor team can help you with this. When you go Home Discharge Planning: Transplant Social Workers will work with you and the Medical team to coordinate a safe and appropriate discharge plan when you are well enough to leave the hospital. On the day of discharge from the hospital, you and your family will receive written instructions on how to provide care for you at home including telephone numbers you can access 24 hours a day to speak with a doctor on call. Typically, after a hospital stay of 1-2 days, you will not require any special nursing care at home. You will be advised to eat a normal diet, to walk around several times a day and to get plenty of rest. You will be unable to drive for a few weeks following discharge. You will be required to return to the Transplant Practice for a check-up often within the first year and then annually. PSYCHOSOCIAL IMPACT OF DONATION: Many issues may affect donors and their families from the psychosocial standpoint and should be addressed before a decision to donate is made. Your social worker will be available to discuss and of your concerns. Since scars from surgery are inevitable, potential donors are strongly advised to evaluate whether scarring will negatively affect their body image and lifestyle. Some donors worry about the possibility that the donated kidney might be rejected by the recipient. If that occurs, 11 the recipient would be relisted for another kidney from a deceased donor. In that case, your donation would not be useful to the recipient or anyone else. It is also important to consider how you might feel if the recipient died during or after the surgery. Due to your emotional relationship with the recipient, are you able to accept that possibility as a risk? You might have to manage not only your own recovery from major surgery; but also deal with a grief reaction, not only yours, but that of the recipient’s family as well. Another concern facing donors is that the disease that caused the recipient’s kidney to fail will recur in the donated kidney. Preparing Your Family for Donation: Ideally, family members will accompany you to kidney transplant education seminars given throughout the year. There, they too, will become familiar with the members of the team who will assist you throughout your medical journey. In some families, donors may experience fierce objections to the idea of donation, often from a significant other. It is helpful that family members who object to donation be given the opportunity for the donor team to answer their questions and to discuss their objections. Your social worker and psychiatrist often meet with family members individually. Ask your family to create a separate team of caregivers for you, the donor, and the recipient. As inpatients, both of you will find comfort in knowing that the other has caregivers devoted to them alone. Make sure that family members know how important it is to help with your transportation to and from the hospital when you are unable to drive. Special focus on young children is advisable. Your social worker will provide you and your children with help on age-appropriate explanations about your hospitalization. Pediatric recipients and their siblings have access to the Child Life Program where specialists will prepare children for surgery from a psychological point of view. Other donors and caregivers who have completed surgery and recovery are always available to provide you and your family with telephone or email support. Financial Considerations for Donation: Medical expenses associated with donation are borne by the recipient’s health insurance provider. Donors are responsible for out-of-pocket expenses that may include some of the following: parking, transportation costs, telephone, television, possible living expenses after discharge such as hotels, childcare, and medical expenses after the first year. 12 Revised August 2011| Mount Sinai Medical Center Due to surgery, donors are advised that health and life insurance companies may increase raise their rates or even deny coverage. Donors are strongly advised to discuss donation with insurance providers in advance of donation. Although families are allowed assist donors with their out-of-pocket expenses, Federal law prohibits receipt of money or other compensation for a donated organ. Donors are strongly advised to discuss possible donation with your employer in order to investigate benefits and to develop a financial plan for your hospitalization and recovery. Some employers oppose voluntary medical leave and donors should be advised that they may face not only a possible loss of employment; but also, donation may impact future employment, especially where heavy lifting is required. Disability Insurance: In New York State there is short-term disability insurance for most full time workers that provides modest replacement income while you are unable to work. New York State ShortTerm Disability Insurance (filed through the NYS Workers’ Compenstion Board) is accessed by submission of forms filled out by you and your doctor. A way to obtain a pamphlet and form and to see if you are eligible is to call 1-800-353-3092 or 718-802-6964. The human resources department at your job may also have forms. Some employers have a private short-term disability insurance policy that you can/should access instead of filing through the New York State Workers’ Compensation. This would get coordinated by the employer’s human resource department. This short-term policy usually asks for the same kind of information as the State. Another long-term benefit is Supplemental Security Income. It is granted to low-income disabled or elderly persons without a work record or whose income from SSDI is not sufficient. Thus, SSI supplements social security benefits. The definition of disability has the same rigorous standard as for the Social Security Disability program discussed above. Applications are made at your Social Security Office. Family Medical Leave Act (FMLA): Federal legislation allows for workers in public or private enterprises of at least 50 employees to be awarded 12 weeks per year of unpaid time off taken all at once or day by day. The leave is granted due to an illness or disability of the employee or a family member. For example, once FMLA is granted, a family member would be eligible to assist you during your hospitalization, recuperation and follow-up medical appointments. The employer would be required to maintain health insurance benefits during the unpaid leave. Use of the Internet: 13 While the Internet can be a valuable resource for medical information, donors are advised to use the Internet with awareness that sometimes the facts about donation may be sensationalized and distorted. Please contact your donor team with any questions or concerns. UNOS has developed and excellent website for those considering living donation and you are encouraged to review it at www.UNOS.org. Additionally The American Society for Transplant Surgeons has videos on live donation at www.ASTS.org. Education and Support: Please ask your social worker for a list of educational and support groups you may wish to attend to prepare for your transplant and to cope with your recovery afterwards. RESOURCES: American Society for Transplant Surgeons at www.ASTS.org. Disability Claims: New York State 718-802-6964 National Kidney Foundation: www.kidney.org for information on living donors) or 1-800-6229010 Tobacco Cessation Clinics: 212-939-6000 United Network of Organ Sharing: 1-888-894-6361, www.unos.org/patient 14 Revised August 2011| Mount Sinai Medical Center