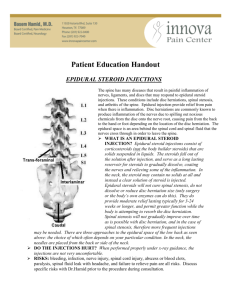
What is an epidural steroid injection
advertisement
The Ajax Pain Clinic Magdi Gaid MD ChB FRCPC Kirit Patel MD FRCPC Kevin Smith MD FRCPC 95 Bayly Street West, # 402 Ajax, ON L1S 7K8 T 905 427-3900 F 905 427-7090 Epidural Steroid Injections (ESIs) Overview Epidural steroid injection (ESI) is a non-surgical treatment that can help relieve pain in the neck, arm, low back and leg (sciatica) caused by irritation of the spinal nerves. ESIs are performed to relieve pain caused by spinal stenosis, spondylosis or disc herniation. The epidural injection delivers a long-lasting steroid and often an anesthetic agent to the irritated and inflamed spinal nerve(s). Medicines are delivered to the nerve through the epidural space - that is the area between the protective covering of the spinal cord and backbones. The effects of ESIs are usually temporary and vary. Pain relief may last for 1 week or up to 1 year. The goal is to reduce pain so that patients may resume their normal activities and, in some cases, continue a physical therapy program. What is an epidural steroid injection? This injection includes both a long-lasting steroid cortisone called a corticosteroid (e.g. depomedrol, triamcinolone) and an anesthetic (e.g. bupivicaine, lidocaine). The drugs are delivered into the epidural space of the spine, which is the area between the protective covering (dura) of the spinal cord and vertebrae (back bones). ESIs can relieve symptoms caused by inflammation and pressure on the spinal nerves. Corticosteroids can reduce inflammation and can be effective when delivered directly into the site of the painful part of the neck or back. Who is a candidate for ESI? Patients with pain in the neck, arm, low back or leg (sciatica) may benefit from ESI. Specifically, those with the following conditions: Spinal stenosis: a narrowing of the spinal canal and nerve root canal that causes back and leg pain. Spondylosis: a weakness or fracture between the upper and lower facets of a vertebra. If the damaged vertebra slips forward (spondylolisthesis), it can compress the nerve roots, causing pain. Herniated disc: the gel-like center of an intervertebral disc ruptures and releases inflammatory proteins. Pain results when the proteins contact a nearby nerve causing inflammation. ESIs have proven helpful for some patients in the treatment of the above painful inflammatory conditions. ESIs can also help to determine whether surgery might be beneficial for pain associated with a herniated disc. When symptoms interfere with rehabilitative exercises, epidurals can ease the pain enough so that patients can continue their rehabilitation. ESIs should not be performed on people who have an infection or those with bleeding problems. Extra care should be taken in performing ESIs on people with pregnancy, diabetes, hypertension, heart disease or renal failure due to the possibility of short-term aggravation of these conditions. ESIs may not be performed on patients whose pain is from a tumour or infection, and if suspected, an MRI scan should be done prior to the injection to rule out these conditions. Who performs ESIs? In Canada, the vast majority of ESIs are performed by Anesthesiologists. What happens before treatment? If you are taking aspirin you may need to stop taking it 7 days before the ESI. Other blood thinners such as Plavix and Ticlid need to be stopped for 14 days before injection. Coumadin (warfarin) needs to be stopped 10 days before injection. Discuss any medications with one of the Pain Clinic doctors. Make arrangements to have someone drive you home from your ESI appointment. What happens during treatment? The goal is to inject the medication as close to the pain site as possible. The right type of injection for you depends on your condition and which procedure will likely produce the best results and the least discomfort or side effects. The entire procedure usually takes less than 15 minutes. The injection is usually performed in the outpatient Ambulatory Care Unit (ACU) on the ground floor of the Ajax Hospital. You will be awake for the injection. Sedatives to lessen anxiety may be available for exceptional circumstances; this must be arranged at the time of booking the injection and will lengthen your stay in hospital. You will either be sitting or lying on your side for the injection. Your blood pressure and pulse will be taken before and after the procedure. After the initial temporary burning sensation from local anesthetic applied in the skin, the injection is usually not painful. Some mild discomfort, often described as deep pressure, may occur during injection of the medication. Occasionally your leg pain may temporarily be reproduced during the injection. What happens after treatment? Most patients may walk within 10 minutes after the procedure. After being monitored for a short time, you can usually leave the hospital. Although you may feel better the same day, take it easy for 24 to 36 hours after the injection to allow the anti-inflammatory benefits to take effect. You may find your pain is aggravated for 1 or 2 days after the injection, followed by a gradual improvement, especially in the leg pain if present. Most patients can resume normal activities and/or participate in their physical therapy program within a few days after the ESI. Localized soreness is usually relieved within 24 hours by using ice, reducing strenuous activities and taking a mild analgesic and/or anti-inflammatory such as ibuprofen. Patients are advised to reduce work schedule and activities for 48 hours following the procedure to help healing. Call the Ajax Pain Clinic if any of the following occur: fever > 38.5 celsius, shortness of breath, bowel or bladder incontinence, severe headache, increased pain lasting over 1 week, increased weakness or numbness, sign of infection at the needle site (red, warm, tender, swollen, drainage). If you cannot contact us, see your family doctor immediately, GO TO THE NEAREST EMERGENCY ROOM or dial 911. however, there are few risks associated with ESIs and they tend to be rare. Risks may include: Infection. Minor infections occur in 1% to 2% of all injections. Severe injections are rare, occurring on 0.1% to 0.01% of injections. Bleeding. Bleeding is a rare complication and is more common for patients with underlying bleeding disorders. Nerve damage. While extremely rare, nerve damage can occur from direct trauma from the needle, or secondarily from infection or bleeding. Arachnoiditis, or inflammation of the lining if the dural sac, may rarely cause worse pain. Dural puncture (“wet tap”). A dural puncture occurs in 0.5% of injections. It may cause a post-dural puncture headache, also called a spinal headache, that usually gets better within a week. If this occurs, leave us a message at the office, drink plenty of caffeinated fluids (coffee, tea, colas) and use pain killers as required. Although uncommon, if you are unable to manage at home an epidural blood patch may be necessary to alleviate the headache. What are the results? About 50% of patients experience significant pain relief. If you don’t notice any such benefit, discuss additional injections with the doctor. You will be booked for 3 consecutive injections, each 3 to 6 weeks apart. The need for each subsequent injection will be reassessed at the time of the booked appointment. You will be given a follow-up appointment for approximately 3 months after the final injection to determine overall effectiveness of the treatments and to plan the next steps. The benefits of ESIs tend to be temporary. Some patients experience pain relief for as little as 1 week and others for up to 1 year. Most importantly, patients may experience enough relief to get moving again, resuming normal activities and/or continuing a physical therapy program. What are the side effects? In addition to risks from the injection, there are also potential risks and side effects from the medication injected. These side effects tend to be uncommon and temporary unless injections are repeated often for several months. Patients who are being treated for chronic conditions (e.g. heart disease, poorly controlled diabetes, rheumatoid arthritis, or those who cannot temporarily discontinue anti-clotting medications) should consult their personal physician for a risk assessment. Risks and side effects may include: High blood sugar High blood pressure Transient flushing A transient decrease in immunity Water retention, swelling and weight gain Rarely stomach ulcers, severe arthritis of the hips (avascular necrosis), cataracts, increased appetite Transient numbness and mild muscle weakness usually resolve within 8 hours in the affected extremity (similar to the facial numbness experienced after dental work) What are the risks? As with all invasive medical procedures, there are potential risks associated with ESIs. Generally, Links for further information www.spine-health.com www.reddinganesthesia.com/ESB.htm Avoid lifting objects more than 20 pounds or active sports until advised otherwise. Swimming tends to help you feel better and strengthens core muscle groups.