Medical History - dermatology naples
advertisement

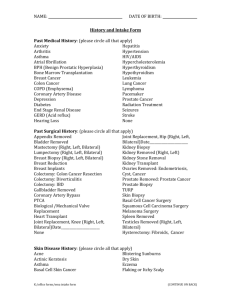
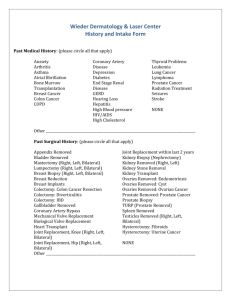
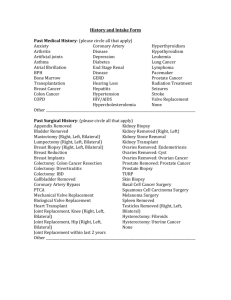
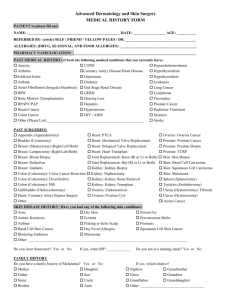
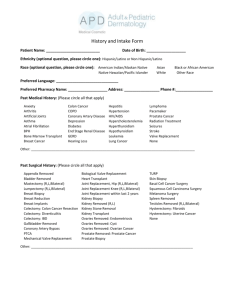
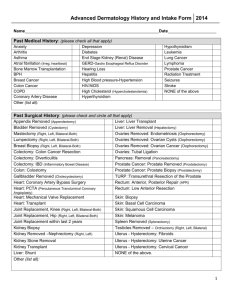
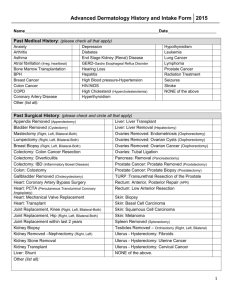
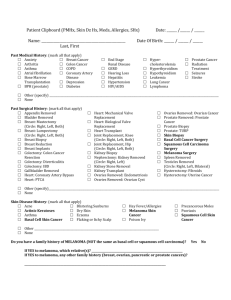
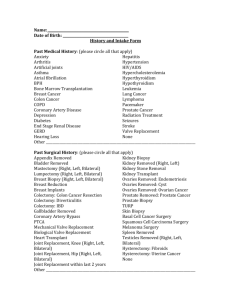
History and Intake Form Todays Date _______________________________ Patient Name _______________________________________________________________________________________ (Last) (First) (Middle Initial) Date of Birth _______________________________ (Month) (Day) (Year) Reason for todays visit: _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ Past Medical History: (please circle all that apply) Anxiety Arthritis Asthma Atrial fibrillation Bone Marrow Transplantation Breast Cancer Colon Cancer COPD Coronary Artery Disease Depression Diabetes End Stage Renal Disease GERD Hearing Loss Hepatitis If Yes, What Type? ______ Current/Past Treatment? _____________ High Blood pressure HIV/AIDS High Cholesterol Thyroid Problems Leukemia Lung Cancer Lymphoma Prostate Cancer Radiation Treatment Seizures Stroke NONE Other _________________________________________________________________________________________ Past Surgical History: (please circle all that apply) Appendix Removed Bladder Removed Mastectomy (Right, Left, Bilateral) Lumpectomy (Right, Left, Bilateral) Breast Biopsy (Right, Left, Bilateral) Breast Reduction Breast Implants Colectomy: Colon Cancer Resection Colectomy: Diverticulitis Colectomy: IBD Gallbladder Removed Coronary Artery Bypass Patient Name _______________________________________________________________________ (Last) (First) (Middle Initial) Mechanical Valve Replacement Biological Valve Replacement Heart Transplant Joint Replacement If yes, what joint(s)? _______________________ what year(s)? _______________________ Kidney Biopsy (Nephrectomy) Kidney Removed (Right, Left) Kidney Stone Removal Kidney Transplant Ovaries Removed: Endometriosis Ovaries Removed: Cyst Ovaries Removed: Ovarian Cancer Prostate Removed: Prostate Cancer Prostate Biopsy TURP (Prostate Removal) Spleen Removed Testicles Removed (Right, Left, Bilateral) Hysterectomy: Fibroids Hysterectomy: Uterine Cancer NONE Other _________________________________________________________________________________________ Personal Skin Disease History: (please circle all that apply) If Circled, Please specify Location and Treatment Basal Cell Skin Cancer Squamous Cell Skin Cancer Melanoma Dysplastic/Abnormal Moles Actinic Keratoses (PreCancers) Location(s) Treatment(s) _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ _____________________________ (Blue Light Treatment /Efudex (Fluorouracil) Carac/Aldara/Liquid Nitrogen) (Excision/Mohs/Radiation) Acne Asthma Blistering Sunburns Dry Skin Flaking or Itchy Scalp Eczema Hay Fever/Allergies Psoriasis Poison Ivy Other ________________________________________________________________________________________ Do you wear Sunscreen? Yes If yes, what SPF? ___________ Do you tan in a tanning salon? No Yes-Current Use Yes-Past Use No 2 Patient Name _______________________________________________________________________ (Last) (First) (Middle Initial) Do you have a family history of Melanoma? Yes No If yes, which relative(s)? ____________________________________________________________________________ Medications: (Please enter all current medications) _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ _________________________________________________________________________________ Allergies: (Please enter all allergies and the reaction you have to each medication, ex: Penicillin, Rash as child) _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ _________________________________________________________________________________ Social History: (Please circle all that apply) Cigarette Smoking: Currently Smokes Former Smoker If yes, What year did you quit? _________ Never smoked Alcohol Use: None Less than 1 drink per day 1-2 drinks per day 3 or more drinks per day Occupation ________________________________ Other Medical History _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ _________________________________________________________________________________________________________ Preferred Language: _____________________________ Race:________________________ Ethnic Group:___________________________ Preferred Pharmacy Name: _____________________________ Phone#: _______________________________ City or Zip code:____________________ 3 Patient Name _______________________________________________________________________ (Last) (First) (Middle Initial) Review of Systems: (Please check yes or no for the following) Symptom Immunosuppression Problems with Healing Problems with Bleeding Problems with Scarring Rash Hay Fever Fever/Chills Night Sweats Unintentional Weight Loss Abdominal Pain Joint Pain Headaches Cough Shortness of Breath Depression Anxiety Yes No ALERTS: (please circle all that apply) Allergy to Lidocaine Rapid heart beat with epinephrine Defibrillator Artificial joint replacement in past 7 years Require antibiotics prior to a surgical procedure If Yes, What Antibiotic __________________ History of MRSA Blood thinners Allergy to adhesive Allergy to topical antibiotics Artificial heart valve Pacemaker Are you pregnant or currently trying to get pregnant? 4